Abstract
Objective.
Description of the prevalence of vertebral fractures in a fracture and osteoporosis outpatient clinic (FO-Clinic) and evaluation of the value of spinal radiographs by screening on osteoporosis.
Design.
Retrospective data collection, description, and analysis.
Methods.
All patients admitted to the FO-Clinic during the period of December 2005 until October 2006 were enrolled in this study. At the FO-Clinic spinal radiographs were obtained and bone mineral density (BMD) was measured by Dual energy X-ray-Absorptiometry (DXA).
Results.
During the study period, a total of 176 patients were screened at our FO-Clinic. In 41.5% of these patients, a vertebral fracture was diagnosed. There appeared to be an indication for anti-osteoporotic medication in 95 of the 176 patients. Of these 95 patients, 77% could be identified by spinal radiographs. Moreover, only 36% of all patients with a vertebral fracture did suffer from osteoporosis.
Conclusion.
The prevalence of vertebral fractures in patients screened at an FO-Clinic is high and spinal radiographs can identify up to 77% of patients in which anti-osteoporotic medication should be considered. However, fracture risk is not only dependent on bone quality but also on bone density. Therefore, the preferred method of screening on osteoporosis is DXA with vertebral fracture assessment and, if necessary, spinal radiographs. If DXA is not available, spinal radiographs might be used as a first step in osteoporosis screening.
Keywords: osteoporosis, dual energy x-ray absorptiometry, bone mineral density, vertebral fracture, spinal radiograph
Introduction
Osteoporosis is a major health problem of which the clinical manifestation is a fragility fracture.1–3 Fragility fractures result in a significant impact on quality of life, morbidity, and mortality.4 When patients with a fragility fracture are treated with anti-osteoporotic medication, it is possible to achieve a 40% reduction in subsequent fragility fractures.5,6 Most subsequent fragility fractures (up to 60%) occur in the first year after the initial fracture.7,8 Therefore, treatment should be started as soon as possible after the initial fracture.
The main indication for initiating anti-osteoporotic medication is osteoporosis. Patients older than 50 years who present with a low energy fracture to the emergency room are at increased risk of osteoporosis and should be screened on osteoporosis.9 At our hospital, this is done at the Fracture and Osteoporosis outpatient Clinic (FO-Clinic). At this FO-Clinic, among other things, bone mineral density (BMD) is measured with dual energy x-ray absorptiometry (DXA) of the hip and spine. The advantage of DXA in screening on osteoporosis is that treatment thresholds are established and follow-up measurements by repeated DXA are possible to evaluate the effect of anti-osteoporotic therapy.10–12 A general disadvantage of DXA is that it is still not available in every clinic and interpretation of DXA can be difficult in patients with arthrosis or other skeletal deformities, which happens to occur especially in the older aged patient group.13
Another reason for initiating anti-osteoporotic treatment, independent on the BMD, is an (a)-symptomatic vertebral fracture, which increases the risk of a subsequent fragility fracture at least 4-fold.4,14–19 Vertebral fractures are the most common fragility fractures in patients ≥50 years with a prevalence of up to 50%.20,21 But, although the prevalence of vertebral fractures is high, only one third of these fractures is clinically recognized.19,20 Spinal radiographs might therefore be helpful in deciding whether or not anti-osteoporotic medication should be initiated.
This study was designed to establish the prevalence of vertebral fractures in patients screened at an FO-Clinic in the Netherlands. Our goal was to determine whether or not spinal radiographs can be used as a first step in screening on osteoporosis.
Materials and Methods
Study design
This study is a retrospective data collection study conducted in a nonacademic teaching hospital.
Patient Selection
All patients admitted to the FO-Clinic during the period of December 2005 until October 2006 were enrolled in this study. Patients were screened at the FO-Clinic when they were ≥50 years and admitted to the hospital with a low energy fracture. Patients were excluded from further screening at the FO-Clinic when no informed consent was obtained or in the case of dementia or a pathologic fracture.
Data Collection
At the FO-Clinic, a standard questionnaire and physical examination was done. Furthermore, patients were sent for an x-ray from the fourth thoracic vertebra down to the fourth lumbar vertebra. Vertebrae were graded using the semiquantative method described by Genant, which is a visual inspection of the vertebral column without direct vertebral measurement.22 This was done by 2 different radiologists, followed by a consensus reading. Genant described in his original article that from grade 1 (approximately a reduction in anterior, middle, and/or posterior height ≥20%), a vertebra can be considered to be fractured.22 In our study, in all vertebrae graded ≥1 using the method described by Genant, the anterior, middle, and posterior height were really measured. If the reduction was indeed ≥20%, this vertebra was considered to be fractured.
The BMD was measured in all patients using DXA (Hologic Discovery A; Hologic, Massachusetts, VS and GE Lunar, Madison, Wisconsin). The DXA was obtained from the left hip and from the first till fourth lumbar vertebra unless contraindicated. The DXA was expressed as a T-score, which is the standard deviation (SD) in BMD compared with the peak BMD of young adults.23,24 Both the T-score of hip and spine were stored in our database. As osteoporosis is considered to be a systemic disease, the lowest of these 2 T-scores was used for further analysis in this study. Therefore, a patient with a spine T-score of −1.9 SD and a hip T-score of −2.6 SD was considered to be osteoporotic. Scanning time on the DXA took about 20 minutes and the machine was calibrated automatically on a daily basis using a phantom.
Classification of patients
Patients were classified into 4 groups. First patients were classified based on the existence of a vertebral fracture on the radiographs. Then patients were further classified based on their BMD (Table 1). In this study, the definition of manifest osteoporosis (T-score ≤ −2 SD) was used instead of the definition of osteoporosis recommended by the World Health Organization (WHO) because the WHO defines patients with a T-score ≤−2.5 SD as osteoporotic and patients with a T-score ≤ −2.5 SD plus a fracture as severe osteoporotic.25 As all patients at the FO-Clinic per definition had a fracture, the definition of manifest osteoporosis is more suitable to the patient group screened at an FO-Clinic and recommended by the most recent Dutch guideline on osteoporosis.9
Table 1.
Distribution of vertebral fractures and bone mineral density among patients screened at the FO-Clinic.
| Vertebral Fracture on X-ray | 73 patients | Group 1: Osteoporosis | 26 patients |
| Group 2: No osteoporosis | 47 patients | ||
| No Vertebral Fracture on x-ray | 103 patients | Group 3: Osteoporosis | 22 patients |
| Group 4: No osteoporosis | 81 patients |
Statistical Analysis
Statistical analysis was performed using SPSS software program (version 15.1 for Windows XP, SPSS, Chicago, Illinois). The normally distributed variables are expressed as mean and SD. For comparison of age, body mass index, and gender with the different groups of patients, crosstabulation were performed with chi-square test and analysis of variance as appropriate. The level of significance was set at P < .05.
Results
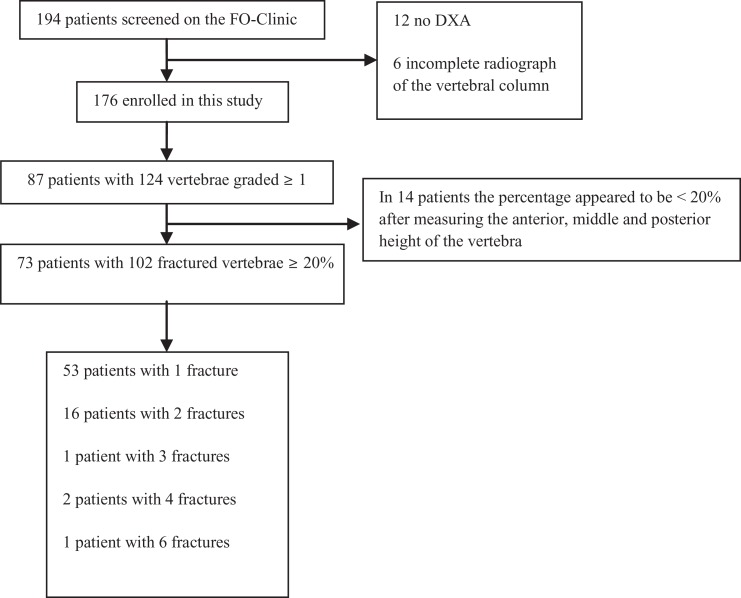
In the 10-month study period, a total of 194 fracture patients were screened on osteoporosis at our FO-Clinic. For unknown reasons, in 12 patients, DXA was not performed and in 6 patients, spinal radiographs were not obtained. Thus, the final study population comprised 176 patients (Figure 1). The general patient characteristics of the 176 patients are expressed in Table 2.
Figure 1.
Flowchart of the inclusion of patients in this study
Table 2.
General patient characteristics of patients admitted to the FO-Clinic.
| General patient characteristics | |
| Men:women | 36:140 |
| Height, mean (SD), cm | 168 (8.7) |
| Weight, mean (SD), kg | 79 (12.7) |
| Body mass index, mean (SD), kg/m2 | 28 (4.4) |
| Age, mean (SD), years | 67 (9.5) |
| Fracture localization | |
| Tibia/fibula/patella | 33 |
| Radius/ulna | 56 |
| Hand/foot | 36 |
| Humerus | 25 |
| Femur/pelvis | 8 |
| vertebrae | 13 |
| Clavicula/scapula | 2 |
| Rib | 3 |
Abbreviation: SD, standard deviation.
In 87 patients, 124 vertebrae were graded ≥1 using the semiquantative method described by Genant. In 73 patients, at least 1 vertebra was indeed fractured (reduction in height ≥20%) after measuring the anterior, middle, and posterior height. Thus, a vertebral fracture was diagnosed in 41.5% of all patients (73 of 176). Only 13 of these 73 patients were referred to the FO-clinic because of a clinical symptomatic vertebral fracture (Table 2). The incidence of symptomatic vertebral fractures at our FO-Clinic is therefore 17.8% and the incidence of a-symptomatic vertebral fractures is 82.2%.
The BMD was in 48 patients (27%) in the osteoporotic range, in 67 patients (38%) in the osteopenic range, and 61 patients (35%) had a normal BMD. As can be seen in Table 1, anti-osteoporotic medication can be considered in 95 of the 176 patients. In 47 (50%) patients, this is because of a vertebral fracture, in 22 (23%) patients because of osteoporosis, and in 26 (27%) patients because of both a vertebral fracture and osteoporosis. This means that it is possible to identify 77% of all patients in which anti-osteoporotic medication can be considered by obtaining a simple spinal radiograph. An interesting result of this study is that only 36% (26 of 73) of the patients with a vertebral fracture did suffer from osteoporosis (Table 1). Therefore, 47 patients did suffer from a vertebral fracture but no osteoporosis. It appeared that the age, body mass index, or gender in these 47 patients was not significantly different from the other patients.
In 137 patients, it was known which medication was prescribed prior to screening at the FO-Clinic. It appeared that 10% of these patients were already on anti-osteoporotic medication. The reason why these patients were already treated was not recorded.
Discussion
Vertebral fractures are frequently diagnosed in patients screened at an FO-Clinic. We found a prevalence of vertebral fractures of over 40% in our study population. One fifth of these fractures appeared to be symptomatic, which is comparable to the literature.19–21 Another important finding of this study is that only 36% of all patients with a vertebral fracture did suffer from osteoporosis. As vertebral fractures in patients older than 50 years can be considered a reason for initiating anti-osteoporotic treatment irrespective of their BMD, assessment of the spinal column is important in order not to withheld patients adequate treatment.4,18–20 When both vertebral fractures and osteoporosis are considered a reason to initiate anti-osteoporotic medication, spinal radiographs can already identify 77% of all patients who will benefit from this medication. On the other hand, 23% of the patients with an indication for anti-osteoporotic medication did not have a vertebral fracture and cannot be identified with spinal radiographs. Spinal radiographs might thus serve as a first step in screening on osteoporosis. Of all patients screened at the FO-Clinic, 10% were already on anti-osteoporotic medication. The value of obtaining spinal radiographs in patients who are already on osteoporotic medication is questionable, although the kind of medication might be changed in the presence of recurrent vertebral fractures.26
It is important to realize that bone strength and therefore fracture risk can be described as the integration of BMD and bone quality. In a previous study, it has been stated that DXA represents BMD and spinal radiographs can represent a test for bone quality.19 Although a vertebral fracture is probably not the best test for bone quality, it is true that vertebral fractures should be considered a reason for initiating anti-osteoporotic therapy. However, BMD measurement remains also important in this decision. Both modalities do have their own advantages. The most important advantage of BMD measurements is that follow-up measurements are possible to evaluate the effect of medication. A great advantage of spinal radiographs is that it can be obtained very easily and will identify more than 40% of all patients in which treatment can already be initiated. This latter is important as most subsequent fragility fractures occur in the first months after the initial fracture.7,8 In our opinion, a combination of BMD measurement and assessment of the spinal column is therefore the best way in screening patients at an FO-Clinic.
A relatively new aspect of DXA scanners is the possibility of morphometry or instant vertebral fracture assessment (VFA). This combines measurement of BMD and assessment of the spinal column at levels where vertebral fractures are most common (below the fourth thoracic vertebra).27 The VFA allows manual or automatic placement of markers at the anterior, middle, and posterior height of the vertebra to calculate ratios.28 The VFA has been compared with spinal radiographs in previous studies. The sensitivity and specificity in diagnosing ≥grade 2 deformity (according to the classification by Genant) with VFA is good, with a lower dose of ionizing irradiation and greater patient convenience.29–31 The VFA is therefore suitable as a first step in screening the vertebral column.9 If a ≥grade 2 vertebral deformity is detected, which happens to be the case in 57% of patients, conventional radiographs do not have to be obtained and these patients can be classified as having a vertebral fracture.9,32 If a grade 1 deformity is detected on VFA, spinal radiographs should be obtained to exclude vertebral fractures.9,29
Conclusion
At most FO-Clinics, the cornerstone in deciding whether or not anti-osteoporotic medication has to be prescribed is BMD measurement using DXA. However, vertebral fractures should also be considered a reason to initiate anti-osteoporotic medication and the prevalence of vertebral fractures in patients screened at an FO-Clinic is high (41.5%). The ideal screening method at an FO-Clinic is probably DXA with VFA. However, if DXA is not available or the waiting list for DXA is long, spinal radiographs can be used as a first step in osteoporosis screening.
Acknowledgments
The authors would like to thank Mrs I. ter Beek and Mrs A. Maathuis, specialized trained nurses of the FO-Clinic, for their work at the FO-Clinic.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article.
References
- 1. Cooper C. Epidemiology of osteoporosis. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 1999;9(suppl 2):S2–S8 [DOI] [PubMed] [Google Scholar]
- 2. Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 1997;7(5):407–413 [DOI] [PubMed] [Google Scholar]
- 3. Keen RW. Burden of osteoporosis and fractures. Curr Osteoporos Rep. 2003;1(2):66–70 [DOI] [PubMed] [Google Scholar]
- 4. Netelenbos JC, Lems WF, Geusens PP, et al. Spine radiographs to improve the identification of women at high risk for fractures. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA.2009;20(8):1347–1352 [DOI] [PubMed] [Google Scholar]
- 5. Hegeman JH, Oskam J, van der Palen J, Ten Duis HJ, Vierhout PA. The distal radial fracture in elderly women and the bone mineral density of the lumbar spine and hip. J Hand Surg Br. 2004;29(5):473–476 [DOI] [PubMed] [Google Scholar]
- 6. Nakamura T, Liu JL, Morii H, et al. Effect of raloxifene on clinical fractures in Asian women with postmenopausal osteoporosis. J Bone Miner Metab. 2006;24(5):414–418 [DOI] [PubMed] [Google Scholar]
- 7. Johnell O, Kanis JA, Oden A, et al. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004;15(3):175–179 [DOI] [PubMed] [Google Scholar]
- 8. van Helden S, Cals J, Kessels F, Brink P, Dinant GJ, Geusens P. Risk of new clinical fractures within 2 years following a fracture. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2006;17(3):348–354 [DOI] [PubMed] [Google Scholar]
- 9. Institute for Quality in Public Healthcare CBO 2011 Osteoporosis, third revised guideline. Utrecht, the Netherlands http://www.cbo.nl/Downloads/1385/OsteoporoseRichtlijn%202011.pdf
- 10. Eastell R. Treatment of postmenopausal osteoporosis. New Eng J Med. 1998;338(11):736–746 [DOI] [PubMed] [Google Scholar]
- 11. Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312(7041):1254–1259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stone KL, Seeley DG, Lui LY, et al. BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res. 2003;18(11):1947–1954 [DOI] [PubMed] [Google Scholar]
- 13.Osteoporose Stichting, author. http://www.osteoporosestichting.nl Accessed March 20, 2006.
- 14. Delmas PD, Genant HK, Crans GG, et al. Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone. 2003;33(4):522–532 [DOI] [PubMed] [Google Scholar]
- 15. Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15(4):721–739 [DOI] [PubMed] [Google Scholar]
- 16. Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285(3):320–323 [DOI] [PubMed] [Google Scholar]
- 17. Melton LJ, 3rd, Atkinson EJ, Cooper C, O'Fallon WM, Riggs BL. Vertebral fractures predict subsequent fractures. Osteoporos Int. 1999;10(3):214–221 [DOI] [PubMed] [Google Scholar]
- 18. Pongchaiyakul C, Nguyen ND, Jones G, Center JR, Eisman JA, Nguyen TV. Asymptomatic vertebral deformity as a major risk factor for subsequent fractures and mortality: a long-term prospective study. J Bone Miner Res. 2005;20(8):1349–1355 [DOI] [PubMed] [Google Scholar]
- 19. Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH. Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int. 2007;18(6):761–770 [DOI] [PubMed] [Google Scholar]
- 20. Cauley JA, Hochberg MC, Lui LY, et al. Long-term risk of incident vertebral fractures. JAMA. 2007;298(23):2761–2767 [DOI] [PubMed] [Google Scholar]
- 21. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–1767 [DOI] [PubMed] [Google Scholar]
- 22. Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8(9):1137–1148 [DOI] [PubMed] [Google Scholar]
- 23. Kullenberg R. Reference database for dual X-ray and laser Calscan bone densitometer. J Clin Densitom. 2003;6(4):367–372 [DOI] [PubMed] [Google Scholar]
- 24. World Health Organization Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. 1994;843:1–12 [PubMed] [Google Scholar]
- 25. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis Report of a WHO Study Group. World Health Organization Technical Report Series. 1994;843:1–129 [PubMed] [Google Scholar]
- 26. Neer RM, Arnaud CD, Zanchetta JR, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. New Engl J Med. 2001;344(19):1434–1441 [DOI] [PubMed] [Google Scholar]
- 27. Chapurlat RD, Duboeuf F, Marion-Audibert HO, Kalpakcioglu B, Mitlak BH, Delmas PD. Effectiveness of instant vertebral assessment to detect prevalent vertebral fracture. Osteoporos Int. 2006;17(8):1189–1195 [DOI] [PubMed] [Google Scholar]
- 28. Lewiecki EM, Laster AJ. Clinical review: clinical applications of vertebral fracture assessment by dual-energy x-ray absorptiometry. J Clin Endocrinol Metab. 2006;91(11):4215–4222 [DOI] [PubMed] [Google Scholar]
- 29. Fuerst T, Wu C, Genant HK, et al. Evaluation of vertebral fracture assessment by dual X-ray absorptiometry in a multicenter setting. Osteoporos Int. 2009;20(7):1199–1205 [DOI] [PubMed] [Google Scholar]
- 30. Lewiecki EM. Bone densitometry and vertebral fracture assessment. Curr Osteoporos Rep. 2010;8(3):123–130 [DOI] [PubMed] [Google Scholar]
- 31. Schousboe JT, Debold CR. Reliability and accuracy of vertebral fracture assessment with densitometry compared to radiography in clinical practice. Osteoporos Int. 2006;17(2):281–289 [DOI] [PubMed] [Google Scholar]
- 32. Dumitrescu B, van Helden S, ten Broeke R, et al. Evaluation of patients with a recent clinical fracture and osteoporosis, a multidisciplinary approach. BMC Musculoskelet Disord. 2008;9:109. [DOI] [PMC free article] [PubMed] [Google Scholar]