Abstract
Objective:
Since April 1, 2008, patients aged ≥65 years presenting with a hip fracture at Ziekenhuisgroep Twente, Almelo (ZGT-A), The Netherlands, have been admitted to the geriatric fracture center (GFC) and treated according to the multidisciplinary treatment approach. The objective of this study was to evaluate how implementation of the treatment approach has influenced the quality of care given to older patients with hip fracture.
Design:
Prospective cohort study with historical control group.
Method:
Two groups of patients with hip fracture were compared, 1 group was treated according to the new multidisciplinary treatment approach in 2009-2010, and the other group received the usual treatment in 2007-2008. The number of readmissions within 30 days after discharge was compared, and an analysis was carried out regarding the number of complications, the number of consultations with various specialists and with the geriatrician, and the duration of hospital stay.
Results:
In all, 140 patients from 2009 to 2010 group and 90 patients from 2007 to 2008 group were included. In 2009-2010 group, the number of readmissions within 30 days dropped by 11 percentage points (P = .001). The incidence of the number of complications decreased with a median of 1 compared with 2007-2008 (P = .017) group. Delirium was diagnosed to be 6 percentage points more frequent. The median number of consultations with various specialists per patient decreased by 1 percentage point as a result of geriatrician cotreatment (P = .002). The median duration of hospital stay was 1 day shorter than that in 2007-2008 group.
Conclusion:
The use of the multidisciplinary treatment approach led to a significant reduction in the number of readmissions within 30 days after discharge. It appears to be associated with improved short-term treatment outcomes for older patients with a hip fracture.
Keywords: hip fracture, elderly, multidisciplinary treatment, clinical pathway, geriatrician
Introduction
Hip fractures in an older patient represent a significant problem for both the patient and the health care system. In absolute terms, the incidence of hip fractures is rising in many Western countries due to the increase in aging populations and longer life expectancy.1 In the Netherlands, between 2000 and 2004, an average of 17 000 patients were admitted per year with a hip fracture. Based on demographic changes, the absolute number of hip fractures is expected to rise by 40.4% between 2005 and 2025.2,3
The effects of a hip fracture are serious: 25% of patients die within the first year of the hip fracture and the risk of dying from the effects of a hip fracture rises with age.4 Age-related aspects such as comorbidity and polypharmacy complicate the treatment, as a result of which there are considerable risks of developing serious complications and loss of function in elderly patients.5,6 Furthermore, treatment is often associated with high costs.7,8 The need for greater focus on this patient group was highlighted in the recently published Royal Dutch Medical Association (KNMG) viewpoint entitled Sound Medical Care for Vulnerable Elderly, in which recommendations were made to optimize primary and secondary care.9 In the present study, we investigated whether the multidisciplinary treatment concept developed at Ziekenhuisgroep Twente, Almelo (ZGT-A), for older patients with hip fracture who often require complex treatment had a favorable effect on the course of the condition.
Usual Treatment
Until April 2008, at ZGT-A, elderly patients with a hip fracture were given usual treatment, characterized by low treatment urgency at the emergency department (ED), consultation with several specialists in case of comorbidity, and consultation with a geriatrician only in cases of severe postoperative confusion. There were no standard clinical pathways, nor was there a multidisciplinary treatment plan with a proactive approach to prevent/limit complications. The patients were admitted to various surgical wards to spread the care burden between the nursing staff.
Models of Care
The inadequacies of usual treatment for this group of patients have been highlighted in international publications since the 1990s.10–12 Various treatment concepts have been described, adding geriatric expertise (both medical and nursing) to the surgical treatment or, in a few cases, making logistical changes to optimize the treatment. The multidisciplinary treatment concept, of the Geriatric Fracture Centre (GFC) at ZGT-A, is based on the treatment principles of a clinic in Rochester, New York.13,14 The GFC in Almelo goes a step further: the multidisciplinairy treatment concept is used from admission through to the outpatient clinic.
The Multidisciplinary Treatment Concept: The GFC
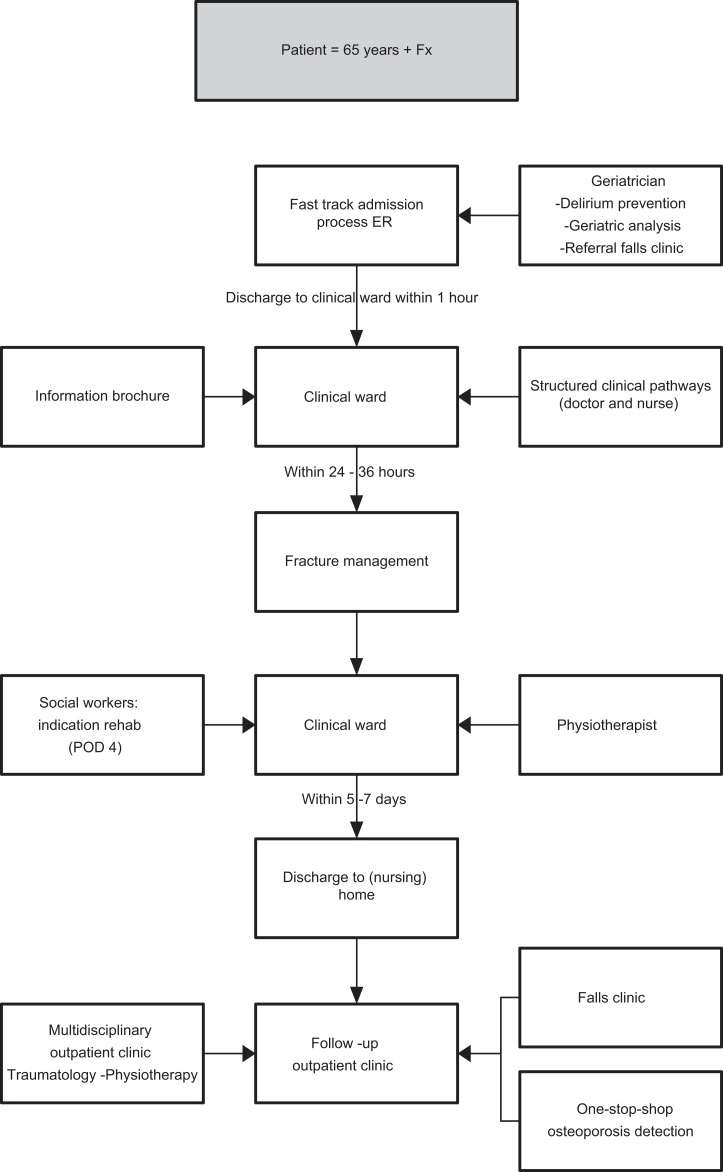
The multidisciplinary treatment concept of the GFC was developed in 2008 and is characterized by intensive comanagement by the geriatrician and the use of multidisciplinary clinical pathways starting at the ED (Figure 1). The clinical geriatrician is a medical specialist who cares for the elderly patients. As a holistic professional, he treats problems in elderly patients with mixed somatic, psychological, and social fields. The emphasis is on maintenance or improving the functioning and quality of life. Their training consists of 2 years of internal medicine, 2 years of geriatric somatic, and 1 year of mental health care/elderly psychiatry. Addition to the expertise of the geriatrician clinical pathways plays an important role in the GFC.
Figure 1.
Flowchart for the treatment of the older patient with a hip fracture.
A clinical pathway is a multidisciplinary management tool based on evidence-based practice for a specific group of patients, in which the different interventions by the professionals involved in the patient care are defined, optimized, and sequenced; outcomes are tied to specific interventions.15–17 As well as focusing on trauma surgery, these pathways describe age-related and geriatric aspects such as estimating the risk of developing delirium,18,19 paying attention to comorbidity, scoring preoperative and postoperative mobility, nutritional status upon admission, prevention of falls, and osteoporosis care.
Using a fast-track procedure at the ED, the aim is to have the patient admitted to the GFC nursing ward within 1 hour of arrival. In the ED, the geriatrician is called by the ED physician. Depending on the medical condition of the patient, he is visiting the patient on the ED, or he gives recommendations by telephone and visiting the patient preoperatievely on the nursing ward. One of the standardized procedures on the ED is blood testing. The test results are used by the geriatrician and the trauma surgeon for further treatment, for example, osteoporosis detection and deficiencies, causes of falls, and malnutrition. Fracture management is planned as soon as possible within 24 to 36 hours. This nursing ward of the GFC is divided into the fields of geriatrics and traumatology and has 12 trauma surgery beds specifically intended for the older patient, thus maximizing paramedical, medical, and nursing expertise. The ward nurses play an important role in early detection of issues such as the first signs of delirium and problems with activities of daily living. A trauma surgery nurse practitioner ensures the process is adhered to and acts as the case manager for individual patients. Daily ward visits under the supervision of the trauma surgeon and in consultation with the geriatrician emphasize the importance of preventing complications. The geriatrician visits the patients daily on the ward and gives recommendations to the nurse practitioner or ward doctor. Preoperative and postoperative pain relief is carried out according to protocol by the department of anesthesiology. There is a multidisciplinary meeting twice a week. Within 5 to 7 days, the patients are ready for discharge.
The clinical pathways are also used in the trauma surgery follow-up treatment and takes place at the multidisciplinary osteophysiotrauma outpatients’ clinic, where the focus is on fall assessment, osteoporosis case finding, and treatment and maintaining function. The follow-up appointments are standardized and scheduled at 2 weeks, 6 weeks, and 3 months after surgery. For research and policy-related purposes, data are registered in the GFC research center.
Research Questions
During recent years, there have been a few international studies regarding the effects of geriatric comanagement of older patients with a hip fracture.11,12,20,21 The aim of our study was to investigate how effective the ZGT-A multidisciplinary treatment concept is and what effect it has on the quality of care.
The hypothesis of this study was that the use of a multidisciplinary treatment concept would lead to a reduction in the number of readmissions within 30 days after discharge. In addition, we investigated the effect on the number of complications and analyzed the number of consultations with other specialists and with the geriatrician. We assumed that the patient flow (ie, logistics) through the care pathway would improve compared with the previous usual approach for older patients with hip fracture.
Patients and Methods
Patients
Two groups of patients aged ≥65 years with a hip fracture were studied. For the usual treatment group, the period selected was from April 1, 2007, to March 03, 2008; and for the multidisciplinary treatment concept group, the same period was selected in 2009-2010. Both patient groups were admitted via the ED and hospitalized for treatment by the trauma surgeon at ZGT-A. The patients from the control group were identified retrospectively using the electronic hospital information system, by entering the International Classification of Diseases, Ninth Revision treatment code for hip fracture (820).22 Patients with a pathological hip fracture or a periprosthetic fracture or those who received a total hip replacement were excluded. This resulted in 230 patients who could be included for this study.
Data Collection
Prior to the study, we performed a power analysis for the primary outcome. Based upon the proportion of patients being readmitted, the power to detect the observed difference is 87%. We used prospective collected data from the GFC research center for the group 2009 to 2010. We took a random sample from the patient records of the control group and concluded that the information recorded was of sufficient quality to allow the research questions to be answered. A single investigator used a search protocol and a list of definitions for the various parameters and collected the required data from the medical and nursing records and the electronic hospital system.
Primary Outcome
The primary outcome measure was readmission within 30 days after discharge and was defined as the number of patients who required readmission for any specialty within 30 days following discharge from the ZGT-A.
Secondary Outcomes
The following secondary parameters were analyzed: the flow of patients through the treatment process (ie, the logistics) in terms time spent at the ED following arrival in minutes, the time to surgery following admission in hours, and the discharge destination. We analyzed the number of consultations per patient with other specialists and the number of geriatrician consultations and finally the number of complications per patient. The most common complications after hip fracture were predefined as well as additional tests and treatment.23
Statistical Analysis
In this study, descriptive statistics were used. Differences between the groups were analyzed using the chi-square test or Fisher exact test in the case of categorical variables, and in the case of continuous variables, the independent t test for normally distributed variables and the Mann-Whitney U test for nonnormally distributed variables were used. Statistical analyses were carried out using the Statistical Package for the Social Sciences version 16 (SPSS).
Results
There were no significant differences between the 2 groups in terms of patient characteristics (Table 1), nor did the surgical techniques and implants undergo any important changes during the study periods. However, the difference in age reached the borderline significance.
Table 1.
Characteristics of Hip Fracture Patients Aged ≥65 Years Who were Treated at ZGT-A According to the Usual Method During the Period From April 2007 Through March 2008, and Those Patients Who were Treated According to the Multidisciplinary Approach in the Period From April 2009 Through March 2010
| Year | 2007-2008 (n = 90) | 2009-2010 (n = 140) | P value |
|---|---|---|---|
| Sex, n (%) | |||
| Men | 24 (27%) | 45 (32%) | .376 |
| Women | 66 (73%) | 95 (68%) | |
| Age in years, mean (SD) | 82.4 (7.6) | 80.5 (7.4) | .064 |
| Dementia, n (%)a | 18 (20%) | 29 (21%) | .900 |
| Prefracture living | |||
| Home/with home care | 56 (62%) | 83 (59%) | .660 |
| Home for the elderly individuals | 19 (21%) | 38 (27%) | .300 |
| Long-stay nursing home and psychogeriatrics | 14 (16%) | 17 (12%) | .460 |
| Other/hospice | 1 (1%) | 3 (2%) | 1.000 |
| Fracture type, n (%) | .459 | ||
| Femoral neck fracture | 47 (52%) | 73 (52%) | |
| Pertrochanteric femur fracture | 37 (41%) | 60 (42%) | |
| Subtrochanteric femur fracture | 6 (7%) | 7 (5%) | |
| ASA classification, n (%)a | |||
| I | 3 (3%) | 4 (3%) | .601 |
| II | 31 (34%) | 49 (35%) | |
| III | 39 (43%) | 69 (49%) | |
| IV | 18 (18%) | 15 (11%) | |
| V | 1 (1%) | 3 (2%) | |
Abbreviations: ASA, American Society of Anesthesiologists; I, healthy patient; V, moribund patient.
a Dementia, at time of admission with known diagnosis.
Patient Flow Times, Duration of Hospital Stay, and Discharge Destination
There were no differences in the duration of stay in the ED between the 2 groups. There was no difference in terms of time to surgery between the groups. In 2009-2010, 12 percentage points fewer people were discharged home, in other words 25% compared with 37% in 2007-2008. In 2009-2010, 11 percentage points more people were admitted to a nursing home for rehabilitation. The median duration of bed occupancy was 1 day less than that in 2007-2008 (Table 2).
Table 2.
Effect of Multidisciplinary Treatment of Hip Fracture Patients Aged ≥65 Years (2009-2010 Group) Compared With Usual Treatment (2007-2008 Group)
| Patient flow times, duration of hospitalization, and discharge destination | |||
|---|---|---|---|
| Year | 2007-2008 (n = 90) | 2009-2010 (n = 140) | P value |
| Duration of stay in ED in minutes | |||
| Mean | 95 (52) | 92 (44) | .663 |
| Min-max | 5-278 | 13-221 | |
| Time to surgery within 48 hours, n (%) | 84 (93%) | 133 (95%) | 1.000 |
| Length of stay in days, median (IQR) | 12 (6-20) | 11 (7-18) | .547 |
| Discharge destination, n (%) | .231 | ||
| Home/with home care | 33 (37%) | 35 (25%) | |
| Home for the elderly | 9 (10%) | 14 (10%) | |
| Rehabilitation bed in nursing home | 26 (29%) | 56 (40%) | |
| Long-stay nursing home and psychogeriatrics | 11 (12%) | 24 (17%) | |
| Other/hospice | 11 (12%) | 11 (8%) | |
Abbreviations: ED, emergency department; IQR, interquartile range.
Consultations With Other Specialists and With the Geriatrician
In the 2007-2008 control group, the most frequently consulted specialists were those of internal medicine, cardiology, urology, and pulmonology (Table 3). In the control group, preoperative geriatric consultation tended to be an exception rather than the rule and occurred in case of patients with severe confusion. In 2007-2008, geriatric consultation took place postoperatively in 33% of the patients due to severe delirium and behavioral problems. Geriatrician comanagement significantly reduced the number of consulted specialists per patient in the 2009-2010 intervention group (P = .002). This effect was particularly visible in the reduction in the number of consultations with the internal medicine specialist (14 percentage points less), the pulmonologist (7 percentage points less), the urologist (7 percentage points less), and other specialists (9 percentage points less). Finally, in 2009-2010, the cardiologist was consulted 4 percentage points more frequently than in 2007-2008.
Table 3.
Effect of Multidisciplinary Treatment of Hip Fracture Patients ≥Aged 65 Years(2009-2010 Group) Compared With Usual Treatment (2007-2008 Group)
| The number of consultations with various specialists and with the geriatrician | |||
|---|---|---|---|
| Year | 2007-2008 (n = 90) | 2009-2010 (n = 140) | P value |
| Consulted specialist, n (%) | |||
| Cardiologist | 20 (22%) | 37 (26%) | .471 |
| Internist | 19 (21%) | 10 (7%) | .002 |
| Pulmonologist | 10 (11%) | 5 (4%) | .024 |
| Urologist | 14 (16%) | 13 (9%) | .150 |
| Other specialists | 20 (22%) | 18 (13%) | .061 |
| Number of consultations per patient, median (interquartile range) | 1 (0-1) | 0 (0-1) | .002 |
| Geriatrician, n (%) | |||
| Preoperative consultation | 4 (4%) | 124 (89%) | <.001 |
| Postoperative consultation | 30 (33%) | 136 (97%) | <.001 |
Complications
Table 4 summarizes the most common postoperative complications following a hip fracture.23 With geriatrician cotreatment, postoperative delirium was diagnosed 6 percentage points more frequently in 2009-2010 (P = .421). However, the incidence of postoperative complications decreased in this group compared with 2007-2008, with a significant reduction of 1 relative to the median (P = .017). This was mainly observed in urinary tract infections, urinary retention, heart failure, deep wound infection, death, and other complications. During the clinical period, 4 percentage points fewer patients died compared with 2007-2008 (P = .244).
Table 4.
Effect of Multidisciplinary Treatment of Hip Fracture Patients Aged ≥65 Years (2009-2010 Group) Compared With Usual Treatment (2007-2008 Group)
| Complications during hospitalization | |||
|---|---|---|---|
| Year, n | 2007-2008 (n = 90) | 2009-2010 (n = 140) | P value |
| Complications, n (%)a | |||
| Deliriumb | 30 (33%) | 54 (39%) | .421 |
| Mild | |||
| Urinary tract infectionc | 14 (16%) | 9 (6%) | .024 |
| Urinary retentiond | 9 (10%) | 4 (3%) | .022 |
| Superficial wound infectione | 12 (13%) | 14 (10%) | .436 |
| Serious | |||
| Pneumoniaf | 11 (12%) | 13 (9%) | .477 |
| Heart failureg | 15 (17%) | 16 (11%) | .256 |
| Myocardial infarctionh | 2 (2%) | 2 (1%) | .653 |
| Osteosynthesis failurei | 4 (4%) | 3 (2%) | .437 |
| Deep wound infectionj | 3 (3%) | 0 | .059 |
| Deathk | 8 (9%) | 7 (5%) | .244 |
| Otherl | 31 (34%) | 33 (24%) | .073 |
| Total number of complications per patient excluding delirium, median (IQR) | 1 (0-2) | 0 (0-1) | .017 |
Abbreviations: IQR, interquartile range; CXR, chest x-ray
a Several concomitant complications were observed in a number of patients.
b Delirium Observation Screening Scale: score above 3, geriatrician diagnosis confirmed in medical record.
c Urine sediment with positive WBC and nitrite, started antibiotics.
d Retention of 500 mL or more confirmed with bladder scan.
e Diffuse redness, serous fluid leakage, and no fever.
f Clinical presentation, diagnosis confirmed on CXR, started antibiotics.
g Clinical presentation, diagnosis confirmed on CXR, started diuretics.
h Eelectrocardiogram abnormalities suspicious for ischemia and elevated cardiac troponin level.
i Diagnosis confirmed on XR, need for revision.
j Worse than superficial, need for revision.
k Established by physician, date, and time in medical record.
l Renal failure, hypervolemia, electrolyte abnormalities, anemia, nerve injury, and pressure sore.
Readmissions Rate Within 30 Days After Discharge
The study revealed that, in 2009-2010, the number of readmissions within 30 days after discharge decreased significantly from 12% to 1% (P = <.001), with no patient deaths during readmission (Table 5).
Table 5.
Effect of Multidisciplinary Treatment of Hip Fracture Patients Aged Older Than or Equal to 65 Years (2009-2010 Group) Compared With Usual Treatment (2007-2008 Group)
| Readmissions within 30 days after discharge | |||
|---|---|---|---|
| Year, n | 2007-2008 (n = 90) | 2009-2010 (n = 140) | P value |
| Readmission within 30 days, n (%) | 11 (12%) | 1 (1%) | <.001 |
| Death during readmission, n (%) | 2 (2%) | 0 | .152 |
Discussion
The GFC was designed to optimize the treatment of older patients with hip fractures, making use of a multidisciplinary treatment approach and trauma-specific care pathways. In this study, we investigated the effect of the concept on the number of 30-day readmissions, the development of complications, the number of consultations with other specialists, and geriatrician comanagement, as well as the logistics of the treatment process. Our study found that there were fewer readmissions and a decreasing trend in mortality. There were significantly fewer postoperative complications, with the exception of postoperative delirium. In addition, geriatrician cotreatment allowed a significant reduction in the number of consulted specialists per patient.
Various international studies have described the benefits of similar initiatives in terms of a reduction in complications, mortality, and the number of readmissions within 30 days. 12–14,16,20,21,24–26 A comparison is difficult because of the different types of study designs, the outcome measures, and health care systems.
In our study, postoperative delirium was diagnosed more frequently in 2009-2010. Early recognition of delirium in its various forms through geriatric expertise within the various disciplines would have contributed to this change.27–31 In comparison, the records of the control group only described signs of hyperactive delirium. The definition of delirium was a clinical diagnosis of the geriatrician. The seemingly high rate may be explained by the strict monitoring of early signs of delirium. By implementing a proactive approach, we were able to avoid the need to consult the geriatrician due to postoperative delirium; in the 2007-2008 group, 33% of our patients needed special attention because of postoperative delirium. The incidence of postoperative delirium in older patients with a hip fracture ranges from 20% to 65%.32–34 The etiology of delirium is multifactorial and is associated with loss of function and a higher mortality.18,35,36 Observation using the Delirium Observation Screening Scale is a standard part of the treatment and care pathways within the GFC.27,33 Research has demonstrated the importance of monitoring for delirium: 70% of patients with delirium will otherwise not be identified.32,35,36 Thus, recognition is key in delirium treatment.18,36 At ZGT-A, detection of high-risk patients starts at the ED, with geriatric evaluation and daily assessment of the multidisciplinary team. Prompt transfer to the nursing ward allows the patient to be treated in a calmer environment with nursing interventions to limit delirium as far as possible. Beside special attention for delirium, early geriatrician comanagement focuses also on treatment of comorbidity, prevention and treatment of complications, reduction in medication in the case of polypharmacy, and analysis of fall issues and advice regarding the follow-up institution.10,20,21,24
In this model of treatment comanaged care, starting already at the ED plays an important role. This comanaged care had several advantages. For instance, early treatment by a geriatrician led to fewer consultations from specialties other than cardiology. In severe cardiac pathology, consultation by the cardiologist was still needed preoperatively. Also, there were fewer complications in the postoperative course. It might be that early identification and treatment of situations leading to complications play a role. In addition, the geriatric treatment was also focused on preventing further loss of function in the elderly patients. To improve standardization of the comanaged treatment, geriatric issues were predefined in clinical pathways.13–17 However, in this study, it was not possible to determine how much of the model’s success is due to the standardization of care with the use of clinical pathways or due to the expertise of the geriatrician and the multidisciplinary team.
In the 2009-2010 intervention group, the duration of hospitalization decreased by only 1 day compared with the control group, despite the fact that the 2009-2010 group had a less complicated course of recovery. Our clinical pathway reports revealed that, from both a surgical and geriatric point of view, the patients were ready for discharge after approximately 7 days. However, in the 2009-2010 group, more patients had to go to a rehabilitation center and fewer patients went directly to their own home. This slight decrease is possibly due to the judgment of the geriatrician after assessing the patient’s resilience that more patients need rehabilitation. The flow of patients to rehab beds in nursing homes is still not optimized in our setting and will be addressed in the future. There is always a shortage of available rehab beds in the nursing homes, which might explain the fact that the length of hospital stay was not reduced significantly. Risk factors predicting difficulties with discharge to own home are age ≥85, chronic systemic diseases, dementia, and walking disability before injury.26,40 It is possible that in addition to a less complicated course, discharge destination plays a role in the observed decrease in the number of readmissions within 30 days after discharge by having closer observation on the subset of patients who are more “at risk.”
The lack of sufficient rehabilitation beds is leading to a longer length of stay in the hospital. In our study, almost half of the length of stay in the hospital was due to the fact that the patient was waiting for a rehabilitation bed. Since 58% of the treatment costs of hip fracture consist of hospitalization,37 it seems likely that the treatment costs of a hip fracture can be reduced if the outflow to rehabilitation beds could be improved. With the results of this study it would be possible to achieve a further reduction in costs of treatment.38,39 This was not the focus of our study, but financial analysis of this model seems to be desirable.
Our study focused on the practical situation; health care institutions and health care professionals are, no doubt, aware of the complexity of the care needed in this category of patients. It seems justified to conclude that a proactive approach and geriatric expertise brought about favorable effects on the treatment outcomes during the clinical period (up to 30 days after discharge) in hip fracture patients aged ≥65 years. We notice that it will be important to address more long-term outcomes to assess whether the short-term benefits persist and that larger studies are necessary to support our findings.
We have identified the following critical success factors in the implementation of the multidisciplinary treatment concept for older patients with hip fracture: initiating a multidisciplinary collaboration with the department of geriatrics, developing, implementing, and maintaining paramedical, medical, and nursing clinical pathways, and seeking approval for the financing of this care from the hospital management. As a result of the outcomes of this study, as of January 1, 2010, all older patients at ZGT-A, regardless of the type of fracture, are now treated according to the multidisciplinary treatment approach with comanagement by the geriatrician. Recently, the KNMG published recommendations for primary and secondary care providers to optimize the care for older patients upon clinical admission.9 In the light of the results of the present study, this may contribute to the initiatives to further improve the care given to older (trauma) patients.
Study Limitations
This study had some important limitations. When interpreting the study results, it is important to take into account the nonrandomized prospective design with a historical control group and small patient populations of this study, with possible selection and information bias. The use of validated testing (ie, confusion assessment method [CAM], Charlson Comorbidity Index, and Barthel score) would have helped to better define the patient characteristics and validate results. Furthermore, this study focuses on in-hospital and short-term outcomes of care. It will be important to evaluate more long-term outcomes, such as functional status and location of residence at 12 months. Data collection on long-term outcomes is currently underway.
Cost-effectiveness of multidisciplinary treatment concept with geriatric cotreatment was not analyzed in our study. This is an interesting aspect of health care innovation also seen in the light of increasing costs of health and aging. Although it is a nonrandomized study with small patient populations, the outcomes can help guide further research into multidisciplinary treatment concepts, multidisciplinary care, and initiatives to optimize care for vulnerable older patients.
Conclusion
Using the GFC multidisciplinary treatment approach to treat hip fracture patients aged ≥65 years, the number of readmissions within 30 days after discharge decreased significantly. In this study, there were significantly fewer complications in the 2009-2010 population, with the exception of delirium. In addition, fewer patients died during hospitalization and readmission. Finally, geriatric comanagement led to a significant reduction in the number of consultations with other specialists per patient. Future large-scale randomized studies are needed to confirm these results.
Acknowledgments
Job van der Palen (clinical epidemiologist) provided the statistical analyses for this manuscript. Peter Dubbeld and Bob van Deelen (clinical geriatricians) were involved in the clinical activities at the GFC.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The GFC was set up with financial support from the ZGT Innovation fund. The GFC is supported with a donation from Synthes Nederland BV.
References
- 1. Cooper C, Cole ZA, Holroyd CR, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22(5):1277–1288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lanting LC, Stam C, den Hertog PC, Brugmans MJP. Whats the Incidence and Mortality Rate of Proximal Femur Fractures?: Bilthoven, The Netherlands: National Institute for Public Health; 2006 [Google Scholar]
- 3. Van der Klift M, Burger H, de Laet CEDH, Pols HAP, Poos MJJC, Gijsen R. Osteoporosis; Does It Increase or Decrease? Bilthoven, The Netherlands: National Institute for Public Health http://www.nationaalkompas.nl/NationaalKompasVolksgezondheid\Gezondheidenziekte/Ziektenenaandoeningen/Bewegingsstelselenbindweefsel/Osteoporose Accessed June 24, 2009 [Google Scholar]
- 4. Saltzherr TP, Borghans HJ, Bakker RH, Go PM. Proximal femur fractures in the elderly in the Netherlands during the period 1991-2004: incidence, mortality, length of hospital stay and an estimate of the care capacity needed in the future. Ned Tijdschr Geneeskd. 2006;150(47):2599–2604 [PubMed] [Google Scholar]
- 5. De Luise C, Brimacombe M, Pedersen L, Sorensen HT. Comorbidity and mortality following hip fracture: a population-based cohort study. Aging Clin Exp Res. 2008;20(5):412–418 [DOI] [PubMed] [Google Scholar]
- 6. Abrahamsen van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2010;20(10):1633–1650 [DOI] [PubMed] [Google Scholar]
- 7. Lanting LC, Stam C, den Hertog PC, Brugmans MJP. What’s the Burden of Health Care? Bilthoven, The Netherlands: National Institute for Public Health; Kosten van Ziekten 2005 http://www.kostenvanziekten.nl, versie 1.1. Accessed June 26, 2008 [Google Scholar]
- 8. Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service-a literature review comparing different models. Osteoporos Int. 2010;21(suppl 4):S637–S646 Review [DOI] [PubMed] [Google Scholar]
- 9. KNMG Sound medical care for vulnerable elderly. Utrecht: KNMG; 2010. http://knmg.artsennet.nl/Publicaties/KNMGpublicatie/Sterke-medische-zorg-voor-kwetsbare-ouderen-1.htm [Google Scholar]
- 10. Handoll HH, Cameron ID, Mak JC, Finnegan TP. Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures (Cochrane review). Coch Database Syst Rev. 2009;(4):CD007125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beaupre LA, Jones AC, Saunders LD, Johnston DWC, Buckingham J, Majumdar SR. Best practices for elderly hip fracture patients. A systematic overview of the evidence. J Gen Intern Med. 2005;20(11):1019–1025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Giusti A, Barone A, Razzano M, Pizzonia M, Pioli G. Optimal setting and care organization in the management of older adults with hip fracture. Eur J Phys Rehabil Med. 2011;47(2):281–296 [PubMed] [Google Scholar]
- 13. Friedman SM, Mendelson DA, Kates SL, McCann RM. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56(7):1349–1356 [DOI] [PubMed] [Google Scholar]
- 14. Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–1717 [DOI] [PubMed] [Google Scholar]
- 15. Dutch Institute for Healthcare Improvement CBO http://www.nkp.be/english/index.html Utrecht, The Netherlands: CBO; 2008 [Google Scholar]
- 16. Antonelli-Incalzi R, Gemma A, Capparella O. Orthogeriatric unit: a thinking process and a working model. Aging Clin Exp Res. 2008;20(2):109–112 [DOI] [PubMed] [Google Scholar]
- 17. Lau TW, Leung F, Siu D, Wong G, Luk KD. Geriatric hip fracture clinical pathway: the Hong Kong experience. Osteoporos Int. 2010;21(suppl 4):S627–S636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kalisvaart KJ, Vreeswijk R, de Jonghe JFM, van der Ploeg T, van Gool WA, Eikelenboom P. Risk factors and prediction of postoperative delirium in elderly hip-surgery patients: implementation and validation of a medical risk factor model. J Am Geriatr Soc. 2006;54(5):817–822 [DOI] [PubMed] [Google Scholar]
- 19. Vochteloo AJ, Moerman S, Borger van der Burg BL, et al. Delirium risk screening and haloperidol prophylaxis program in hip fracture patients is a helpful tool in identifying high-risk patients, but does not reduce the incidence of delirium. BMC Geriatr. 2011;11:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vidan M, Serra J, Moreno C, Riquelme G. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized controlled trial. J Am Geriatr Soc. 2005;53(9):1476–1482 [DOI] [PubMed] [Google Scholar]
- 21. Barone A, Giusti A, Pizzionia M, Razzano M, Palummeri E, Pioli G. A comprehensive geriatric intervention reduces short-and long-term mortality in older people with hip fracture. J Am Geriatr Soc. 2006;54(7):1145–1147 [DOI] [PubMed] [Google Scholar]
- 22. World Health Organization International Classification of Diseases (ICD), version 2007 [Google Scholar]
- 23. Booij LHDJ, Knape JTA, Linden CJ van der, Schneider AJ. Peri-operative care. In: Principles and Practice. 2002 [Google Scholar]
- 24. Adunsky A, Arad M, Levi R, Blankstein A. Five-year experience with the ‘Sheba’model of comprehensive orthogeriatric care for elderly hip fracture patients. Disabil Rehabil. 2005;27(18-19):1123–1127 [DOI] [PubMed] [Google Scholar]
- 25. Fallon WF, Rader E, Zyzanski S, Mancuso C, Martin B, Breedlove L. Geriatric outcomes are improved by a geriatric trauma consultation. J Trauma. 2006;61(5):1040–1046 [DOI] [PubMed] [Google Scholar]
- 26. Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PM, Budge MM. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20(3):172–178 [DOI] [PubMed] [Google Scholar]
- 27. Steis MR, Fick DM. Are nurses recognizing delirium? A systematic review. J Gerontol Nurs. 2008;34(9):40–48 [DOI] [PubMed] [Google Scholar]
- 28. Joshi S. Current concepts in the management of delirium. Mo Med. 2007;104(1):58–62 [PubMed] [Google Scholar]
- 29. Sieber FE. Postoperative delirium in the elderly surgical patient. Anesthesiol Clin. 2009;27(3):451–464 [DOI] [PubMed] [Google Scholar]
- 30. Saxena S, Lawley D. Delirium in the elderly: a clinical review. Postgrad Med J. 2009;85(1006):405–413 [DOI] [PubMed] [Google Scholar]
- 31. Gillis AJ, MacDonald B. Unmasking delirium. Can Nurse. 2006;102(9):18–24 [PubMed] [Google Scholar]
- 32. Santana Santos F, Wahlund LO, Varli F, Tadeu Velasco I, Eriksdotter Jonhagen M. Incidence, clinical features and subtypes of delirium in elderly patients treated for hip fractures. Dement Geriatr Cogn Disord. 2005;20(4):231–237 [DOI] [PubMed] [Google Scholar]
- 33. Lutz A, Heymann A, Radtke FM, Spies CD. If delirium is not monitored it will often not detected. Anasthesiol Intensivmed Notfallmed Schmerzther. 2010;45:106–111 [DOI] [PubMed] [Google Scholar]
- 34. Kuehn BM. Delirium often not recognized or treated despite serious long-term consequences. JAMA. 2010;304(4):389–390 [DOI] [PubMed] [Google Scholar]
- 35. Moraga AV, Rodiguez-Pascual C. Accurate diagnosis of delirium in elderly patients. Curr Opin Psychiatry. 2007;20(3):262–267 [DOI] [PubMed] [Google Scholar]
- 36. Pae CU, Marks DM, Han C, Patkar AA, Masand P. Delirium: underrecognized and undertreated. Curr Treat Options Neurol. 2008;10(5):386–395 [DOI] [PubMed] [Google Scholar]
- 37. Roos MJJC, Smit JM, Groen J, Kommer GJ, Slobbe LCJ. Costs of Illness in the Netherlands. Bilthoven, The Netherlands: National Institute for Public Health and the Environment (RIVM). Rapportnr.270751019 [Google Scholar]
- 38. Kates SL, Mendelson DA, Friedman SM. The value of an organized fracture program for the elderly: early results. J Orthop Trauma. 2011;25(4):233–237 [DOI] [PubMed] [Google Scholar]
- 39. Kates SL, Blake D, Bingham KW, Kates OS, Mendelson DA, Friedman SM. Geriatr Orthop Surg Rehabil. 2010;1(1):15–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hagino T, Ochiai S, Sato E, Watanabe Y, Senga S, Haro H. Prognostic prediction in patients with hip fracture: risk factors predicting difficulties with discharge to own home. J Orthop Trauma. 2011;12(2):77–80 [DOI] [PMC free article] [PubMed] [Google Scholar]