Abstract
Background: The use of telemonitoring of patients with chronic illness in their homes is growing. Current literature does not describe what types of patient problems are addressed by nurses in these programs and what actions are taken in response to identified problems. This study defined and analyzed patient problems and nursing actions delivered in a telemonitoring program focused on chronic disease management. Subjects and Methods: Data were drawn from a clinical trial that evaluated telemonitoring in patients with comorbid diabetes and hypertension. Using study patient records, patient problems and nursing actions were coded using an inductive approach. Results: In total, 2,336 actions were coded for 68 and 65 participants in two intervention groups. The most frequent reasons for contact were reporting information to the primary care provider and lifestyle information related to diabetes and hypertension (e.g., diet, smoking cessation, foot care, and social contacts). The most frequent mode of contact was the study sending a letter to a participant. Conclusions: Detailed descriptions of interventions delivered facilitate analysis of the unique contributions of nurses in the expanding market of telemonitoring, enable identification of the appropriate number and combination of interventions needed to improve outcomes, and make possible more systematic translation of findings to practice. Furthermore, this information can inform calculation of appropriate panel sizes for care managers and the competencies needed to provide this care.
Key words: telemedicine, nursing interventions, telehealth, diabetes, hypertension
Introduction
Telemonitoring of patients in their homes can be incorporated into a variety of care management programs, and its use for chronic disease management is growing rapidly. Telemonitoring technologies used in the home include Web-based applications, videophones, messaging devices, devices that record and transmit vital sign data only, and telephone calls, including interactive voice response. Although several studies have evaluated the effectiveness of telemonitoring in chronic disease care management, results have been mixed.1 Two systematic reviews of telemonitoring in patients with diabetes mellitus (DM) found mixed effects on glycemic control.2,3 Although all of the studies in these two reviews included transmission of blood glucose (BG) values, contact with healthcare professionals varied from telephone communication only, routine clinic visits, or use of e-mail contact only; some studies only evaluated transmission of BG values. A recent Cochrane review4 of 25 studies evaluating structured telephone support, telemonitoring, or both in outpatients with heart failure found that telemonitoring reduced all-cause mortality and that both structured telephone support and telemonitoring reduced heart failure–related hospitalizations. In contrast, in the largest multisite clinical trial to date, in 1,643 patients with heart failure, telemonitoring had no statistically significant effect on outcomes.5 However, Chaudhry et al.5 did not report what variances occurred or the specific interventions provided in response to variances.6
When care management is part of the design of a telemonitoring program, it is typically delivered by nurses. Nursing interventions can be either direct or indirect. Direct interventions include treatments performed during interactions with patients, whereas indirect interventions are typically performed away from the patient but on behalf of the patient.7 Nurses also perform non–patient care tasks.8 Inadequate descriptions of interventions in published reports prevent a thorough assessment of the reliability and validity of the intervention and hinder future research and translation of the intervention to practice.9
To date, there have been few published description of “what nurses do” in telemonitoring programs. Because the numbers of these programs are growing and they are associated with significant costs, it is important to describe what is actually delivered within the program. The purpose of this study was to define and categorize what types of patient problems are addressed by nurses in these programs and what interventions are taken in response to identified problems. The data reported here are drawn from a clinical trial that evaluated nurse care management and telemonitoring in patients with comorbid DM and hypertension (HTN), and an analysis of nursing interventions provided to patients enrolled in the trial is reported.
Subjects and Methods
The primary study findings have been published elsewhere.10 In brief, the study was a single-center, randomized, controlled clinical trial that evaluated use of a messaging device and compared two monitoring intensity levels and usual care in patients with comorbid DM and HTN. Primary outcome measures were hemoglobin A1c and systolic blood pressure (SBP). The local institutional review board and Veterans Affairs (VA) Research Committee approved the study prior to data collection. Data were collected from patients enrolled for care at a VA Medical Center outpatient clinic. Participants were randomized to three groups: usual care group, low-intensity group, and high-intensity group.
The study intervention combined close surveillance via telemonitoring using a commercially available messaging device (Viterion 100 telehealth monitor; Bayer-Panasonic, Tarrytown, NY) and nurse care management over a 6-month time period. Participants in the low-intensity group were instructed to measure blood pressure (BP) daily, measure BG as directed by their physician, and answer two questions each day using the telemonitoring device. One question was “Have you taken all your medications as prescribed?” The second question was rotated daily and focused on diet, exercise, foot care, or medication side effects. All questions used yes/no or multiple choice responses. Participants responded by pressing buttons to answer questions and transmitting BP and BG using the device.
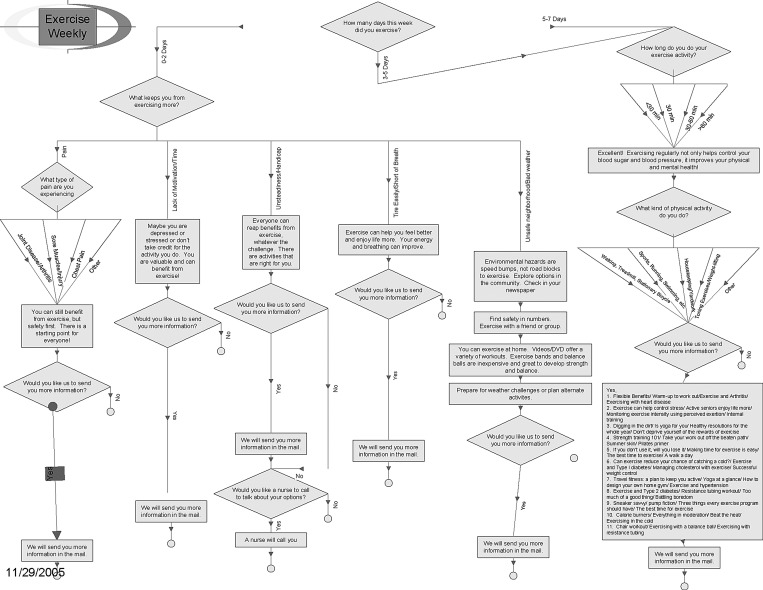
The high-intensity group received a more intensive intervention. The study team (nurses, a physician, and a certified diabetes educator) developed a branching disease management algorithm based on DM and HTN guidelines from the VA, American Diabetes Association, and American Heart Association. The algorithm was programmed into the device and provided information or asked the patient questions about diet, exercise, smoking cessation, foot care, managing sick days, medications, weight management, preventive care, and behavior modification and lifestyle adjustments (Figure 1 shows an example of an algorithm for one topic). A schedule was established so that subjects received both a standard set of information and questions each day and a rotation of questions and educational “tips” on each topic throughout the 6-month intervention. Participants responded by pressing buttons to answer questions and read content on the device screen. Participants in the high-intensity group were also instructed to measure and upload BP daily and BG as directed by their physician.
Fig. 1.
Sample algorithm: exercise.
Trended data on BP and BG and responses to questions by participants in both groups were viewed via a secure Web site by the study nurses. Triggers that prompted nurses to contact patients included patient-entered BP and BG values and responses to questions. Patients in both groups then received appropriate feedback depending on how they answered the device prompt. In order to standardize responses, study nurses used a Triage Scale11 to determine the immediacy of response needed by patients. The Triage Scale was scored on a 0–4 scale. Scores of 0 indicated the patient needed education and information, typically delivered via letter. A score of 1 indicated a somewhat problematic situation where the nurse should intervene as needed. One example is BP or BG trends (higher or lower toward out of range) where the nurse would follow up with a letter and assess further as needed. Scores of 2 indicated an important problem that needed intervention within 1 week. Examples include patient report of not taking medications, follow-up on lab results, or fluctuating BP; in this case the nurse would contact patient by phone to gather information, assess, and make recommendations and/or notify the primary care provider via e-mail message. Scores of 3 indicated a significant problem that needed intervention within 24–48 h. Examples include reported dizziness, questions about medications, or new reddened areas of skin. Follow-up actions by the nurse included contacting the patient by phone to gather information, assess, and make recommendations, notifying the primary care provider via e-mail message, and/or contacting the patient by phone again within 48 h for reassessment and adjustment of the treatment plan. Finally, scores of 4 indicated an urgent problem that needed intervention as soon as possible. Examples include high or low BG or BP readings reported. Follow-up actions included contacting the patient via phone to gather information, assess, and make recommendations, notifying the primary care provider via page or phone call followed by e-mail message, and/or contacting the patient by phone again the next day for reassessment and adjustment of the treatment plan.
As described above, patient follow-up was conducted by telephone, mailing a letter to patients, or using the device to send an advice message. On occasion, if the patient was at the medical center for a clinic appointment, study nurses met with the participant in person. Standardized letters were developed for the study (e.g., diet education), but telephone calls and advice messages were tailored to the patient's particular need. Thus, although the content delivery was standardized across patients via the algorithms programmed into the messaging device, and we used a structured approach in responding to patient-reported data by using the Triage Scale, the study nurses had some latitude in responding to patient needs and tailoring approaches to individual patients.
At the conclusion of the main study, intervention subjects (low- and high-intensity) experienced decreased hemoglobin A1c during the 6-month intervention period compared with the control group, but 6 months after the intervention was withdrawn the intervention groups were comparable with the control group. For SBP the high-intensity subjects had a significant decrease in SBP compared with the other two groups at 6 months, and this pattern was maintained at 12 months. Medication adherence improved over time for all groups, but there were no differences among the three groups.
Data Analysis
We used an inductive approach to identify the patient problems and activities of the nurse as part of the overall intervention strategy. The study nurses kept track of each patient-related activity with intervention patients in a paper-based record. We extracted this information to a spreadsheet for analysis. The study's Principal Investigator and two study nurses independently reviewed the data and subsequently developed an initial list of codes to categorize each nurse activity. One nurse then coded a set of 70 activities using the code list. This coding was reviewed and discussed among the study team until consensus was reached on the final coding schema. One nurse then coded all of the data using the final code list except for the level of severity, which had been coded by the study nurses during the study using the Triage Scale. Each activity was coded for the reason for the activity, who was contacted (patient, primary care physician, other, or study nurse), mode of communication (i.e., whether the contact was conducted by telephone, letter, using the device to send an advice message, or other), and level of severity using the response Triage Scale. Each intervention was analyzed using descriptive statistics by group (low- and high-intensity). The frequency of each intervention was compared between the low- and high-intensity groups using chi-squared analysis.
Results
In total, 2,336 activities were coded for 68 low-intensity and 65 high-intensity patients. On average, there were 17.2 (±8.1) activities for each low-intensity patient and 18 (±8.3) activities for each high-intensity patient over the 6-month intervention period (high-intensity median was 17 activities, and low-intensity median was 16.5 activities). Number of activities per patient ranged from 1 to 45 in the high-intensity patients and from 6 to 45 in the low-intensity patients.
Overall, the most frequent activity by the nurses was reporting information to the primary care provider (17%), followed by providing lifestyle information to the patient related to DM and HTN (e.g., diet, smoking cessation, foot care [14%], and social contacts with the patient [14%]). The 14 activities from the inductive analysis were then categorized according to whether each was for direct patient care (47.9% of all activities) (Table 1), indirect patient care (35.7% of all activities) (Table 2), and non–patient care (16.3% of all activities) (Table 3). The percentages in Tables 1–3 indicate the relative frequency of each activity within that category of intervention.
Table 1.
Direct Care Interventions (n=1,121)
| |
HIGH-INTENSITY (N=570) |
LOW INTENSITY (N=551) |
||
|---|---|---|---|---|
| PROBLEMS/INTERVENTIONS | NUMBER | % | NUMBER | % |
| Provided lifestyle or health information (DM- or HTN-related) | 190 | 33% | 134 | 24% |
| Provided emotional support/words of encouragement | 94 | 16% | 114 | 21% |
| Addressed clinical issue | ||||
| BG | 81 | 14% | 101 | 18% |
| BP | 78 | 14% | 86 | 16% |
| Not BP or BG | 38 | 7% | 37 | 7% |
| Combined BP and BG | 19 | 3% | 23 | 4% |
| Medication adjustments or issues | 62 | 11% | 53 | 10% |
| Provided lifestyle or health information (not DM or HTN) | 8 | 1% | 3 | 1% |
BG, blood glucose; BP, blood pressure; DM, diabetes mellitus; HTN, hypertension.
Table 2.
Indirect Care Interventions (n=834)
| |
HIGH-INTENSITY (N=413) |
LOW-INTENSITY (N=421) |
||
|---|---|---|---|---|
| PROBLEMS/INTERVENTIONS | NUMBER | % | NUMBER | % |
| Report to primary care provider | 205 | 50% | 194 | 46% |
| Social contacts | 146 | 35% | 170 | 40% |
| System issues: medication refills, strip refills, clinic appointment reminders, troubleshooting BG meter | 62 | 15% | 57 | 14% |
BG, blood glucose.
Table 3.
Non–patient Care Interventions (n=381)
| |
HIGH-INTENSITY (N=381) |
LOW-INTENSITY (N=414) |
||
|---|---|---|---|---|
| PROBLEMS/INTERVENTIONS | NUMBER | % | NUMBER | % |
| Device-related (not working, reminders to enter data) | 149 | 39% | 153 | 37% |
| False alarm | 24 | 6% | 23 | 6% |
| Other | 12 | 3% | 20 | 5% |
Each activity was then compared between the low- and high-intensity groups using chi-squared testing. The frequency of “providing lifestyle or health information related to DM or HTN” (Table 1) was used significantly more frequently in the high-intensity group (chi-squared=10.64; odds ratio, 1.5; 95% confidence interval, 1.2–2.0; p=0.001). There were no significant differences between the low- and high-intensity groups on any other intervention category.
Using the Triage Scale, each activity was initiated based on the level of severity of the patient problem. Slightly under half (49%) of all activity were educational in nature, with 6% being significant or urgent. The most frequent recipient of contact was study nurses contacting patients (68% of all contacts), followed by study nurses contacting the patient's primary care provider (21%) and “others” (5%), including specialist physicians, other nurse care managers, pharmacists, the diabetes educator, and patient family members. Over the 6-month intervention period, study nurses were contacted 124 times (68 times in the high-intensity group and 56 in low-intensity group).
The most frequent mode of contact used was the study sending a letter to a participant (33%). Study nurses could also send information with an advice message via the messaging device to patients (31% of all contacts). Slightly less frequently, telephone calls (27%) and other modes of contact were used (11%), including e-mail contact (this was prior to secure messaging implementation in the VA).
Discussion
Evaluating nursing activities during telemonitoring in patients with comorbid DM and HTN, we found the most frequent type of activity was for direct patient care (41%), and most of this was providing lifestyle information related to DM and HTN, emotional support, addressing clinical issues about BP or BG, and medication management. Most contacts were not urgent and were handled by advice messaging via the telemonitoring device or letter. Patients in the high-intensity group had significant and sustained improvements in SBP and were significantly more likely to receive BP- and BG-related lifestyle counseling and information from the nurses.
As noted in the Introduction, telemonitoring programs vary in design and implementation. Thus, it can be difficult to ascertain the mechanism of effect in successful programs or what is missing in ineffective programs.12 Although there is a growing literature on nurse care management and telemonitoring, the content and dose of nursing interventions delivered during studies are rarely described. Frequently the proposed intervention is described in detail, but published results typically report frequency of patient data uploads and clinician time for data review13,14 rather than specific nursing interventions. Some briefly report topics addressed during patient contacts, such as addressing medication side effects and adherence, self-monitoring, and psychological problems.15,16 In a study that used pharmacist–nurse teams to improve BP in patients with DM, there was a significant reduction in SBP. The authors speculated the effect was due to lifestyle adjustment or improved adherence but did not collect data on these factors.17 Our study evaluated the amount of direct and indirect care provided by the nurse and found that a key nursing intervention—provision of DM- or HTN-related lifestyle and health information—was significantly higher in patients who improved and sustained SBP improvements.
For clinical programs that have adopted telemonitoring, a frequent question is how many telemonitoring patients should be assigned to the care manager? Several factors determine panel size, including the specifics of the program design, patient factors such as acuity and adherence to the plan of care, and the skill level of the care manager. Nursing workload has been conceptualized as a combination of nursing intensity and non–patient care activities. Nursing intensity includes both nurse and patient factors, including the condition of the patient, severity of illness, amount of direct and indirect care needed from the nurse, and the time to carry out nursing interventions.8 There are a few published reports describing the amount of time needed to deliver remote care per patient.13–15 In a study of depression care management delivered via telephone, initial assessments took up to 95 min, with almost an hour spent on each follow-up call; panel size ranged from 143 to 165 patients.18 Because depression care is different from diabetes management, it is likely time estimates would vary significantly from these estimates. A time–motion study in a home spirometry telemonitoring program19 found only 34% of time was spent on direct care, with the rest spent on indirect care and administrative tasks. Without specific information on the frequency and type of interventions used in programs and how long each one takes on average, panel size is difficult to calculate.
Limitations
This study has several limitations. Data were collected as part of a larger research study with dedicated study nurses; thus findings may differ if this analysis was conducted in clinical practice. Although we captured interventions delivered by the study nurses, we did not collect data on interventions that may have been delivered by the patients' primary nurse care manager or primary care physician (either through routine care or in response to messages from the study nurses). Because the primary objective of the parent study was to evaluate the efficacy of the telemonitoring program, we did not collect time spent on each activity provided by the study nurses. We assessed the frequency of each intervention but did not assess the extent to which they were clustered within individual patients.
Conclusions
Currently published literature describing trials of telemonitoring programs does not provide sufficient detail on individual program components to enable identification of the appropriate number and combination of interventions needed to improve outcomes or translate findings to practice. Descriptions of interventions delivered need to include details about the active components of the intervention, the quantity of each active element, the number of times each active element was delivered, and the duration of the program.20,21 This information would enable a more accurate estimate of the workload requirements in telemonitoring programs, including level of staff needed relative to patient needs and time to deliver interventions in order to inform calculations of appropriate panel sizes for care managers and the competencies needed to provide this care.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
This study is registered with the title “Effectiveness of Home-Based Health Messaging for Patients with Hypertension and Diabetes” at www.ClinicalTrials.gov with trial identification number NCT00119054.
Acknowledgments
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (grant number NRI 03-312).
Disclosure Statement
No competing financial interests exist.
References
- 1.Hersh W. Hickam DH. Severance SM. Dana TL. Krages KP. Helfand M. Diagnosis, access and outcomes: Update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(Suppl 2):3–31. doi: 10.1258/135763306778393117. [DOI] [PubMed] [Google Scholar]
- 2.Pare G. Jaana M. Sicotte C. Systematic review of home telemonitoring for chronic diseases: The evidence base. J Am Med Inform Assoc. 2007;14:269–277. doi: 10.1197/jamia.M2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farmer A. Gibson OJ. Tarassenko L. Neil A. A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med. 2005;22:1372–1378. doi: 10.1111/j.1464-5491.2005.01627.x. [DOI] [PubMed] [Google Scholar]
- 4.Inglis SC. Clark RA. McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2009;(1):1. doi: 10.1002/14651858.CD007228.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhry SI. Mattera JA. Curtis JP, et al. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai AS. Stevenson LW. Connecting the circle from home to heart-failure disease management. N Engl J Med. 2010;363:2364–2367. doi: 10.1056/NEJMe1011769. [DOI] [PubMed] [Google Scholar]
- 7.Bulechek G, editor; Butcher H, editor; Dochterman J, editor. Nursing interventions classification. 5th. St. Louis: Mosby Elsevier; 2008. [Google Scholar]
- 8.Morris R. MacNeela P. Scott A. Treacy P. Hyde A. Reconsidering the conceptualization of nursing workload: Literature review. J Adv Nurs. 2007;57:463–471. doi: 10.1111/j.1365-2648.2006.04134.x. [DOI] [PubMed] [Google Scholar]
- 9.Conn VS. Groves PS. Protecting the power of interventions through proper reporting. Nurs Outlook. 2011;59:318–325. doi: 10.1016/j.outlook.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wakefield BJ. Holman JE. Ray A, et al. Effectiveness of home telehealth in comorbid diabetes and hypertension: A randomized, controlled trial. Telemed J E Health. 2011;17:254–261. doi: 10.1089/tmj.2010.0176. [DOI] [PubMed] [Google Scholar]
- 11.Piette JD. Moving diabetes management from clinic to community: Development of a prototype based on automated voice messaging. Diabetes Educ. 1997;23:672–680. doi: 10.1177/014572179702300607. [DOI] [PubMed] [Google Scholar]
- 12.Norman GJ. Answering the “what works?” question in health behavior change. Am J Prev Med. 2008;34:449–450. doi: 10.1016/j.amepre.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montori VM. Helgemoe PK. Gyatt GH, et al. Telecare for patients with type I diabetes and inadequate glycemic control. Diabetes Care. 2004;27:1088–1094. doi: 10.2337/diacare.27.5.1088. [DOI] [PubMed] [Google Scholar]
- 14.Piette JD. Weinberger M. McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: A randomized, controlled trial. Med Care. 2000;38:218–230. doi: 10.1097/00005650-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Piette JD. Weinberger M. McPhee SJ. Mah CA. Kraemer FB. Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? Am J Med. 2000;108:20–27. doi: 10.1016/s0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- 16.Piette JD. Weinberger M. Kraemer FB. McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: A randomized controlled trial. Diabetes Care. 2001;24:202–208. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 17.McLean DL. McAlister FA. Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: Study of Cardiovascular Risk Intervention by Pharmacists—Hypertension (SCRIP-HTN) Arch Intern Med. 2008;168:2355–2361. doi: 10.1001/archinte.168.21.2355. [DOI] [PubMed] [Google Scholar]
- 18.Liu CF. Fortney J. Vivell S, et al. Time allocation and caseload capacity in telephone depression care management. Am J Manag Care. 2007;13:652–660. [PubMed] [Google Scholar]
- 19.Cady R. Finkelstein S. Lindgren B, et al. Exploring the translational impact of a home telemonitoring intervention using time-motion study. Telemed J E Health. 2010;16:576–584. doi: 10.1089/tmj.2009.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manojlovich M. Sidani S. Nurse dose: What's in a concept? Res Nurs Health. 2008;31:310–319. doi: 10.1002/nur.20265. [DOI] [PubMed] [Google Scholar]
- 21.Wakefield B. Boren S. Groves P. Conn V. Heart failure care management programs: A review of study interventions and meta-analysis of outcomes. J Cardiovasc Nurs. 2013;28:8–19. doi: 10.1097/JCN.0b013e318239f9e1. [DOI] [PubMed] [Google Scholar]