Abstract
Acetabular fractures in the elderly individuals are increasing in prevalence. Although there is evidence in the literature that acetabular fractures in elderly patients sustained as a result of low-energy mechanisms can be well treated by nonoperative management, open reduction and internal fixation, or even acute arthroplasty, almost no literature exists that may appropriately guide the treatment of elderly acetabular fractures that occur as a result of high-energy mechanisms. In spite of this lack of evidence, specific principles for providing the best care in adult trauma patients may reasonably be adopted. These principles include aggressive resuscitation and medical optimization; surgical care that focuses on a patient’s survival but does not sacrifice skeletal stability; and early mobilization. Best practices that guide the care of hip fracture patients, such as a team approach to care, the use of protocols to guide treatment, and the timing of surgery to occur as soon as is safely possible also should be employed to guide care in patients who have sustained acetabular fractures. Opportunity exists to better study these higher energy fractures and to, thereby, affect outcomes in patients who have sustained them.
Keywords: acetabular fracture, elderly trauma, high-energy injuries, geriatric
Introduction
As the elderly population in the United States is increasing, the incidence of acetabular fractures is rising as well. Already, the elderly population has become the fastest growing subset of those affected by acetabular trauma.1 While numerous studies have found that acetabular fractures sustained by young adults are managed with success,2–4 the comorbidities, bone quality, and fracture patterns of the elderly patients make acetabular fractures in this population more challenging to manage.5–8 In spite of the increasing prevalence of these fractures in the elderly individuals, there is a paucity of literature on elderly individuals who have sustained acetabular fractures as a result of high-energy trauma.
Two recent epidemiological studies on fractures of the pelvic ring describe trends indicating that orthopedic surgeons are operatively treating more pelvic and acetabular fractures in patients of age 65 and older.9,10 The increase in prevalence of acetabular trauma is not matched by an increase in tolerance of these injuries in the elderly individuals, particularly if they are the result of high-energy trauma. Patients over the age of 65 do not tolerate polytrauma as well as younger patients.11 Taylor et al, in a retrospective study of 26 237 trauma patients admitted for blunt trauma to 24 different trauma centers, found that older patients had significantly higher mortality rates than their younger counterparts after trauma at every level of severity as defined by Injury Severity Score (ISS).
It is clear from the current literature that outcomes for elderly patients treated after acetabular fractures remain less than satisfying.5,6,12 Early studies followed patients who had undergone nonoperative management of their acetabular fractures and noted inadequacy of reduction.5,13 Improvements in existing surgical techniques and approaches have been tested, but outcomes are still poorer when compared with younger patients.2–4 To date, there has been no published study dedicated to the management of severely injured elderly patients with acetabular fractures.
The purpose of this article is to review and summarize the relevant literature with respect to high-energy acetabular fractures in elderly patients and provide the knowledge we have gained from our institutional experience treating these injuries. The need for improved care of elderly patients with acetabular fractures, and particularly those who present after high-energy trauma is evident, and will be underscored in this article. This review will not address specific technical explanations of surgical interventions that can be accessed in many major texts and manuscripts on the subject of acetabular fractures.
Fracture Patterns
Identification of acetabular fractures in elderly patients can be difficult and requires greater vigilance than in younger populations.14 Judet x-ray views for the elderly population may be insufficient to detect acetabular fractures due to decreased bone quality and fracture pattern complexity. Computed tomography (CT) scans may provide more important information and are better at determining accuracy of reduction.15
Acetabular fracture patterns in the elderly population have a very different distribution than those that occur in younger people.16 The most common acetabular fractures in younger patients are posterior wall and transverse patterns. In the elderly individuals, both column and anterior column fractures are far more prevalent (Table 1).
Table 1.
Classification of Fracture Patterns Based on 1309 Displaced Acetabular Fractures, According to Age and Percentage.a
| Pattern | <60 Years (%) | >60 Years (%) | P Value |
|---|---|---|---|
| Elementary | 29.1 | 37.0 | .02 |
| Posterior wall | 14.7 | 13.2 | .62 |
| Posterior column | 2.4 | 0.4 | .2 |
| Anterior wall | 0.3 | 3.4 | .001 |
| Anterior column | 7.2 | 19.2 | <.001 |
| Transverse | 4.6 | 0.9 | .01 |
| Associated | 69.6 | 63.0 | .03 |
| T-shaped | 12.9 | 10.2 | .3 |
| Posterior column and posterior wall | 2.9 | 3.4 | .84 |
| Transverse and posterior wall | 18.2 | 8.1 | <.001 |
| Anterior and posterior hemitransverse | 7.6 | 14.9 | <.001 |
| Associated both column | 27.9 | 26.4 | .7 |
| Unknownb | 1.3 | 0.0 | <.001 |
| Total involving AC/AW displacement (AC, AW, AHT, ABC) | 43.0 | 63.8 | <.001 |
Abbreviations: AC, anterior column; AW, anterior wall; AHT, anterior with posterior hemitransverse; ABC, associated both columns.
a Reprinted with permission from Ferguson et al (Table IV).16
b Unknown represents the 14 patients recorded in the database, who did not have a pattern classification recorded or in whom the data could not be abstracted from the medical records or radiographs.
An understanding of the fracture pattern will help guide surgeons toward more appropriate management options. Patients who sustain fractures with greater than 20 mm of displacement have typically done poorly after nonoperative management,17 and operative management should be considered for these patients. Furthermore, acetabular fractures with severe central or superior dome impaction,18 displaced and impacted subchondral bone of the medial roof (“gull sign”),19 posterior wall fractures with hip dislocation,20 or those fractures with damage to the femoral head have historically done poorly with open reduction and internal fixation (ORIF) and may have more favorable outcomes with acute total hip arthroplasty (THA) in patients able to withstand the surgical insult.
Perioperative Management
Blunt trauma in the elderly individuals is a particularly challenging problem. Grossman et al reported each 1-year increase in age beyond 65 years of age increased the odds of an elderly patient dying following trauma by 6.8%.21
The general management of elderly patients (presenting after high-energy trauma) is similar to the triage, resuscitation, and general care of younger patients. However, as a result of compromised ability to generate an adrenergic response, lower physiologic reserve, associated comorbidities, and interplay of preexisting medications, the care of elderly trauma patients is more challenging. Special consideration should be paid to hemodynamic stability, as Magnussen et al reported that age may be an independent factor associated with bleeding in acetabular factures.22 And, because the elderly patients may not have the cardiac capacity needed to respond to blunt trauma injury, aggressive cardiac and hemodynamic treatment have been shown to enhance survival.23 These treatments help avoid death in the elderly patients that appear “hemodynamically stable” in the emergency department but progress quickly to cardiovascular collapse. Immediate foley insertion in geriatric patients may help with monitoring resuscitation from the hour of admission, even if injuries seem modest.
Appropriate resuscitation of elderly patients can be difficult because their vital signs are often unreliable. A retrospective review by Heffernan et al compared 2194 geriatric patients (>65) versus 2081 younger patients (17-35) who presented after blunt trauma with similar ISS scores.24 In this study, mortality increased considerably in the elderly patients with heart rates greater than 90 beats/min, and systolic blood pressure greater than 100 mm Hg, while similar increases in mortality were not seen in the younger patients. The authors advocated changing parameters that dictate aggressive resuscitation so that there is greater sensitivity to minor variations in vital signs during the assessment and optimization of elderly trauma victims.
An interdisciplinary team approach to elderly patients who present after trauma is paramount. Ceder et al described a decreased hospital stay for patients over the age of 50 following hip fracture after implementation of a program that stressed early operation with early mobilization and consisted of multidisciplinary care.25 Zuckerman et al noted following initiation of such a multidisciplinary program, elderly hip fracture patients had fewer complications, fewer intensive care unit transfers, and significantly improved ambulatory status when compared with the age-matched patients who had not been enrolled in such a program.26 The researchers also noted fewer discharges to nursing homes in the multidisciplinary program cohort. Recently, Kates et al has demonstrated the benefits of a protocol-driven fracture program for 193 patients over the age of 60 that presented with hip fracture.27 Not only did patients in the program demonstrate lower mortality, decreased length of stay and fewer complications than published national averages but the cost of care was 66.7% of the national average. Although, most of the literature published on the benefits of a “team” approach for elderly patients have been based on hip fracture outcomes, it is reasonable to expect that the importance of collaborative medicine would be even more vital in the setting of severe or polytrauma.
Surgical Timing
Zuckerman et al reported that a surgical delay of more than 2 days after hospital admission doubled the risk of the patient dying before the end of the first postoperative year for geriatric patients with a hip fracture.28 Conversely, another study analyzing hip fracture mortality reported that patients with 3 or more comorbid conditions who were operated on within 24 hours after injury had poorer survival rate than those who underwent surgery after 24 hours of hospital admission.29
The timing of surgical treatment for acetabular fracture following high-energy trauma requires at least as much thoughtful consideration as for hip fractures. It is influenced by fracture pattern and approach, availability of blood products, and optimal resuscitation of the patient. Elderly patients may have low compensatory reserve, become coagulopathic faster, are prone to tearing of venous structures, and are more vulnerable to cardiac and pulmonary events. The ilioinguinal approach is used for the more common anterior column and both column fracture patterns in the elderly individuals.30 Blood loss tends to be greater due to the size of the incision, the delicate, friable deep pelvic veins, the difficulty of access for reduction clamps applied to bones with low bone density, as well as the presence of corona mortise vessels. In light of this risk of significant blood loss, the availability of cell saver and blood must be insured prior to proceeding to surgery.
Nonoperative Treatment
Due to the frequent concomitant, multiple comorbidities and baseline function, nonoperative management may be the best option in some geriatric patients; however a futilistic outlook must not be taken. Indeed, many elderly acetabular fracture patients can expect satisfactory if not good or excellent outcomes. Furthermore, traction is no longer the preferred method of managing geriatric acetabular fractures; rather, a nonoperative approach with mobilization, even if bed to chair, may prevent bed sores, pneumonia, thrombosis, deconditioning, and a loss of independence, albeit at the expense of a less satisfactory reduction. Historically, traction and nonweight bearing for 6 to 12 weeks were the preferred methods of treatment of acetabular fractures in frail and low-demand individuals. Tile suggested that in older patients with osteoporotic bone, surgical treatment may not be suitable.31
Unfortunately, however, elderly patients have generally not attained satisfactory outcomes following nonoperative management. Spencer retrospectively reviewed 25 patients over the age of 65 managed nonoperatively and found that 7 (30%) out of 23 survivors had unacceptable results.5 These poor outcomes may be secondary to one or all of the following 3 factors: traction is unlikely to accomplish adequate correction because typical deformities in acetabular fractures include rotational as well as translational elements.32 Ligamentotaxis is not effective in achieving satisfactory realignment of displaced fragments or columns.13,17 Complications of nonoperative care derive from prolonged recumbency. Although there is little data regarding acetabular fractures, patients with hip fracture who poorly mobilize are more likely to develop pulmonary compromise and deterioration.25,33
Nonoperative treatment is indicated in minimally displaced, stable acetabular fractures, and in patients who are nonambulatory. Hesp et al retrospectively followed 55 patients and concluded that no optimal result can be expected using conservative treatment with posterior column or acetabular roof fractures.13 In this series, 79% of patients had moderate to bad results (Merle de’ Aubigne and Postel classification) when these fracture patterns were involved. Sen et al reported on a subgroup of 14 patients with acetabular fractures displaced greater than 20 mm who were treated nonoperativley.17 Reducibility was very poor, as only 2 (14.3%) of the 14 achieved good reduction on follow-up x-ray imaging. It should be recognized, however, that due to the decreased functional demands in the elderly individuals, that which may be considered to be an unsatisfactory result for articular reduction in a younger active patient, may yield a quite satisfactory functional result for an older patient.
Nonoperative management should also be considered in cases classified as both column fractures with good “secondary congruence.” The both column acetabular fracture pattern as defined by Letournel30 is common in the elderly individuals, due to the poor bone density (Figure 1). This fracture pattern is an intra-articular variant in which there is no continuity between any part of the articular surface and the intact hemipelvis. The columns tend to rotate away from each other, allowing the head to medialize, but they maintain a congruent relationship with the head. This is a distinctly different scenario from transverse fractures or single column fractures in which the femoral head moves with one column of the acetabulum; or when there is an isolated wall fracture that manifests in instability or luxation of the joint. Secondary congruence does not suggest that articular reductions are anatomic. Rather, it indicates that the femoral head would be stable inside a consolidated acetabulum. Indeed, acceptable results can be obtained with nonoperative treatment with this fracture pattern. In a small series, Letournel reported very good or excellent results at an average of 4.3 years of follow-up in 11 (85%) of 13 of the patients treated nonoperatively.34 Ultimately, every attempt should be made to render an anatomic reduction of the articular surface and stability to the joint without compromising patient safety, if an optimal result is to be obtained. The likely good outcomes associated with both column fractures in the elderly individuals treated nonoperatively relate also to the lower functional demands in this group.
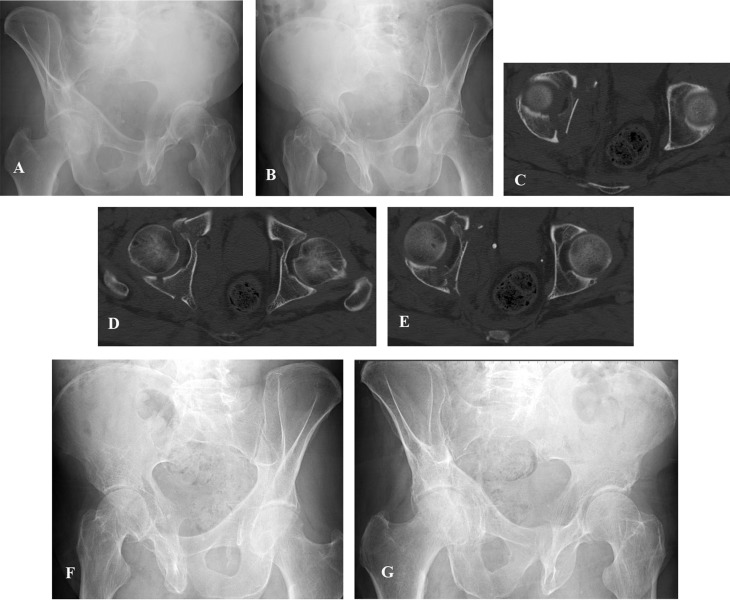
Figure 1.
(A, B) Judet oblique radiographs of a 79-year-old male who fell off a ladder and suffered a both column acetabular fracture with secondary congruence as depicted by the axial computed tomography (CT) scan (C, D, E). Follow-up oblique radiographs (F, G) demonstrated fracture healing and a good overall result after nonoperative management.
Operative Treatment
The surgical indications for acetabular fractures have continued to evolve. Matta et al reported that surgery should be performed in the majority of acetabular fractures and demonstrated congruency of the femoral head to the weight bearing dome within 3 mm of displacement was pivotal to obtaining a good result.4
There are a number of generally well-accepted open approaches to acetabular fractures. The controversy in this population is whether to treat a patient with operative fixation. Once surgery has been determined to be the best treatment option, the question is whether traditional strategies apply in the elderly population, as they do in young patients with the same fracture patterns, or whether a more minimal approach with limited surgical goals but lower immediate risk is chosen. Open reduction and internal fixation, acute or delayed total hip arthroplasty, and percutaneous screw fixation all have their place in the treatment of acetabular fractures.
Open Reduction and Internal Fixation
Comminuted acetabular fractures and poor bone quality affect the ability to achieve and then maintain an anatomic reduction. Matta et al were able to achieve an anatomic reduction in only 44% of patients over 60 years of age, but he had a 74% rate of anatomic reduction in patients under the age of 60.3 Miller et al reported similar difficulties after analyzing 45 acetabular fractures in which they reported an anatomic reduction in 58% of the elderly patients (mean age 67) based on plain radiographs.15 This value diminished to only 11% as seen after CT scan. Other publications have shown that patients over the age of 70 years have poorer reduction with more intra-articular damage.18
Differing opinions exist regarding the correlation of anatomic reduction of the acetabulum with the functional outcome in elderly patients. As previously mentioned, Matta et al retrospectively looked at a cohort of 64 displaced acetabular fractures of all ages and found 24% had excellent or good clinical results in nonoperative treatment and 40% had excellent or good results in operative treatment.3 The results were good or excellent however in 91% of the patients in which the fracture was reduced to within 3 mm. Nousiainen et al reviewed 109 acetabular fractures with posterior hip dislocation and found the quality of reduction was a significant variable associated with the development of arthritis and clinical function, graded by a modified system of Merle d’Aubigne and Postel.35 Even so, other studies have shown no significant correlation between the accuracy of reduction and the functional outcome.15
Letournel cautioned against the abandonment of surgical fixation of acetabular fractures in the older patient after he reported 44 (76%) of 58 surgically treated acetabular fractures in patients over 60 years of age experienced good to excellent clinical results.34 Helfet et al was able to achieve good to excellent results with ORIF, graded by the Harris Hip score, in 15 (88%) out of 17 patients (mean age 67) who were pre-injury ambulators prior to their acetabular fracture.6 This prompted the authors to deduce that elderly patients in good health and capable of independent ambulation should have a favorable prognosis (Figure 2). Other authors have also stressed the importance of attempting primary ORIF in geriatric patients.12,15,36 Carroll et al reported on 93 patients over the age of 55 who underwent ORIF for an acetabular fracture.12 After a follow-up of 5 years, lasting fixation was found in 58 (69%) of the remaining 84 patients, while 26 (30%) required a delayed THA. The authors reported only 3.2% of the patients had serious complications and emphasized that restoring gross alignment and having good bone stock are critical for patients who may be converted to THA in the future. O’Toole et al reviewed 52 patients over the age of 65 who had displaced acetabular fractures treated with ORIF.37 They presented similar outcomes at an average of 4.3 years follow-up that demonstrated conversion to arthroplasty in 28% of the surviving patients but at the expense of a 1 year mortality of 25%.
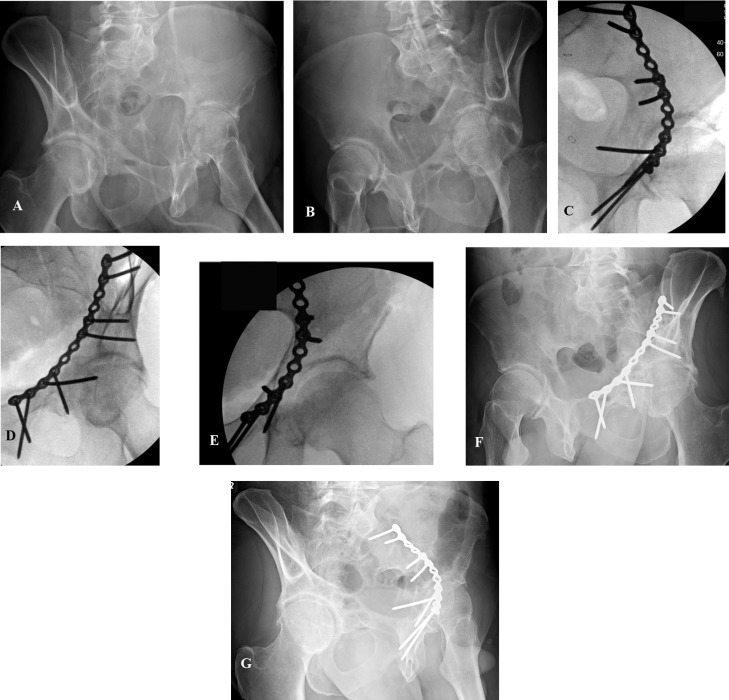
Figure 2.
Preoperative (A, B) Judet oblique injury radiographs of an anterior column fracture of a elderly patient struck by a motor vehicle. Intraoperative (C, D) oblique and hip (E) images after open reduction and internal fixation through an ilioinguinal approach. Postoperative (F, G) oblique radiographs.
Our recommendation is to attempt an anatomic reduction, whenever a patient is deemed safe for surgery and is an independent ambulator, regardless of age. Although it is technically demanding, secondary to impaired bone quality, impaction injury in these variants can possibly be treated effectively (Figure 3). If, due to severe articular injury usually associated with severe central impaction in both column and anterior column variants, posttraumatic arthritis develops, there is always the option to perform delayed THA at some safe interval following the initial ORIF.
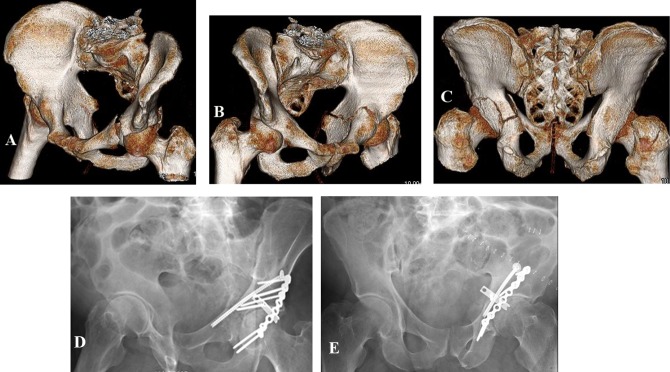
Figure 3.
Preoperative 3-dimensional (3D) computed tomography (CT) reconstruction (A, B) oblique and posterior (C) images of a 67-year-old male that fell >10 feet from a deer stand. 3D reconstruction allowed for clear delineation of the transverse acetabular fracture and massive posterior wall impaction, which was instrumental for preoperative planning. Postoperative (D, E) oblique radiographs after open reduction and internal fixation (ORIF).
Minimally Invasive Techniques
For older patients presenting with displaced acetabular fractures and multiple comorbid conditions or who may have sustained other injuries as a result of high-energy mechanisms, ORIF or THA involving lengthy surgery and major blood loss may be poor treatment options. Minimally invasive osteosynthesis may be a safer option for these fragile patients (Figure 4).
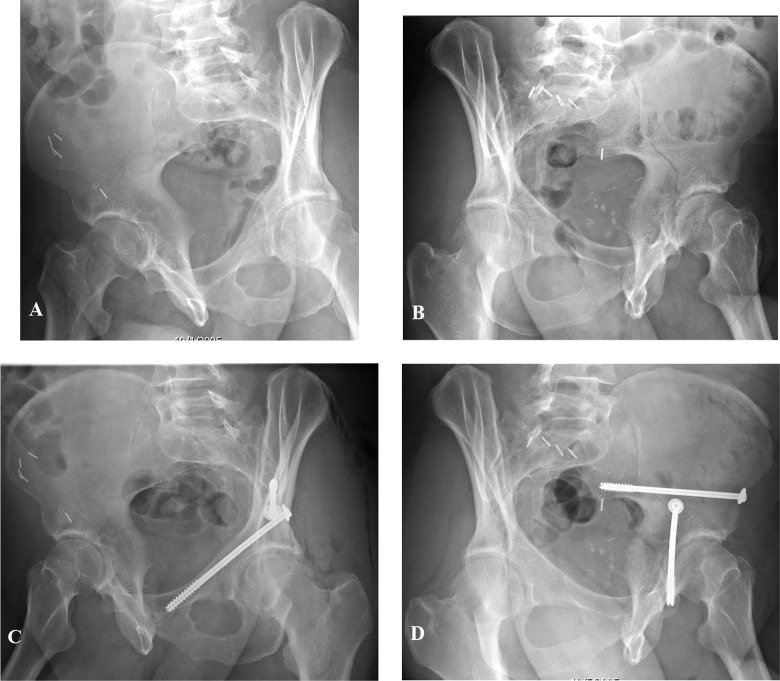
Figure 4.
(A, B) Judet oblique radiographs depicting a minimally displaced acetabular fracture. Postoperative judet oblique radiographs (C, D) after treatment with percutaneous screws allowing for immediate touchdown weight bearing.
Gary et al reported on 75 patients with a mean age of 73 years treated with percutaneous screw fixation for acetabular fractures, who were followed for an average of 46.8 months (range 6-142.8).38 The study population consisted of patients with displaced, unstable acetabular fractures that did not allow early mobilization. Four patients were lost to follow-up, however, only 19 (25%) of the remaining 75 patients treated with percutaneous fixation of their acetabular fractures underwent delayed THA. In spite of the potential promise, the postoperative complication rate was 41% (32 of 79); yet, most of these complications were medical and attributed to the patients’ fragility. The authors concluded percutaneous methods may be used in an attempt to limit soft tissue complications and to lessen the impact of surgery in this frail patient population. More recently, the authors of the previous study reported functional outcomes on 35 of the original 79 patients after an average of 6.8 years post surgery.39 Results from the follow-up study showed the functional outcome scores and rates of conversion to THA were not significantly different when compared with previously published series of elderly patients with acetabular fractures treated by formal ORIF.
Proponents of percutaneous methods to treat acetabular fractures highlight both the minimal blood loss and similar rates of conversion to THA when compared with ORIF.39 Additionally, Schwan et al offered supportive data following an analysis of the revision rates after conversion to THA treated primarily with percutaneous methods versus ORIF after an acetabular fracture.40 In their study of 79 consecutive acetabular fractures requiring subsequent arthroplasty, 20% (14 of 67) treated primarily with ORIF required revision arthroplasty and no revisions (0 of 12) were performed in the patients treated initially by a percutaneous technique.
Total Hip Arthroplasty
Delayed
While older patients seem to tolerate flawed reductions better than their younger counterparts,6 these outcomes are often related to the functional demands unique to the patient. Even when accurate reduction of acetabular fractures is achieved, posttraumatic arthritis occurs in up to 26.6% of the patients.41 When posttraumatic osteoarthritis develops, options for salvage are often limited to THA or resection arthroplasty of the proximal femur (Figure 5). Unfortunately, outcomes of delayed THA after acetabular fractures have been inferior to those of THA performed for nontraumatic arthritis.42,43 Even so, THA can be performed following ORIF or minimally invasive fixation of acetabular fractures, if severe posttraumatic arthritis develops. Conversion to delayed THA may be more common and more difficult following an acetabular fracture initially fixed by ORIF or percutaneous methods, although, with expertise, it can be performed in either circumstance.
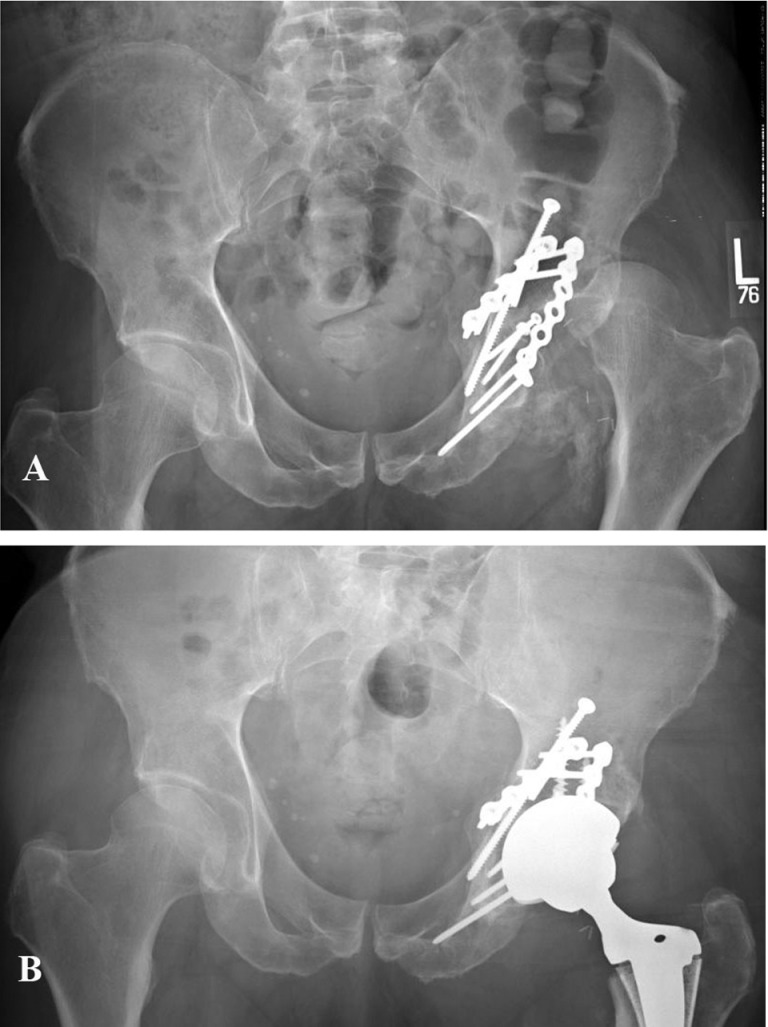
Figure 5.
Anteroposterior (AP) preoperative (A) and postoperative (B) radiographs of a patient who underwent primary open reduction and internal fixation (ORIF) for an acetabular fracture and subsequently had a left total hip arthroplasty after subcapital femoral neck fracture and posterior hip dislocation.
Due to a lack of literature focusing on elderly patients (>60 years) with delayed THA following an acetabular fracture, current opinions are derived from studies in a slightly younger population. In 1998, Weber et al reported on 60 hips (mean age 52) that had been treated with THA following acetabular fractures.44 The complications associated with delayed THA after an attempt at ORIF for acetabular fractures showed higher rates of failure, more heterotopic ossification, greater amounts of scaring and retained hardware causing a more technically demanding operation. In fact, 17 (28%) of the 60 patients required revision THA. The authors still concluded that restoration of the acetabular osseous anatomy at the time of ORIF can be beneficial. Interestingly, none of the 22 cementless acetabular components in this study were revised or had signs ofloosening. Romness and Lewallen analyzed 55 patients (mean age 56) treated with delayed THA after an acetabular fracture and described symptomatic loosening or acetabular failure in 27.5% of their patients.45 When patients over the age of 60 were stratified and analyzed separately, acetabular component loosening was 38.5% compared with 4.8% following THA without acetabular fracture (P < .0001).
Bellabarba et al established superior results, good to excellent Harris Hip Scores in 90% of their patients (mean age 51), in patients who underwent THA after conservative and surgical management of an acetabular fracture using cementless acetabular components.46 The authors noted technically more challenging surgery when THA was done following open reduction internal fixation versus nonoperative treatment. They reported twice as much intraoperative blood loss and increased operating room (OR) time; however, significantly fewer patients in the open reduction group required bone grafting (P = .04) and the clinical results were not compromised.
Immediate Arthroplasty
Although immediate arthroplasty may play a role in treatment of elderly patients who have sustained low-energy acetabular fractures,18,47 the data in high-energy fracture patients are lacking, despite being advocated by some experts for certain well-chosen patients. Proponents indicate that acute total hip replacement provides for immediate mobilization and avoids the risks of multiple surgical procedures.47 Additionally, patients with some fracture patterns have a tendency to do poorly after ORIF.
Mears et al followed 57 patients (mean age 69) for an average of 8.1 years who underwent acute THA for displaced acetabular fractures.18 Seventy-nine percent of the patients had good to excellent Harris hip scores. The authors indicated that patients with displaced acetabular fractures associated with intra-articular comminution, signs of arthritis, and impaction of the femoral head benefitted from acute THA. Mears et al explain that their success with this technique is due to achievement of a stable construct of the acetabular fracture but not necessarily anatomical.18 Another study evaluated the outcomes of 22 elderly patients (>60 years) who sustained acetabular fractures and were treated with acute ORIF and THA during the same anesthesia.48 The indications for the combined procedure included those patients who presented with significant osteoarthritis, poor bone stock, or patients with associated femoral neck fractures. After an average follow-up of 29.4 months, the patients achieved average Harris Hip scores of 74. The surgical times and hospitalizations were consistent with open reductions or delayed THA. However, because of the challenges associated with acute THA and the paucity of data following high-energy injuries, a surgical team with members experienced in acetabular fracture surgery as well as THA is mandatory.
Rehabilitive Care
Multidisciplinary postoperative care of the elderly patient with an acetabular fracture should be undertaken with a focus on several issues vital to the outcome. Early mobilization to avoid the complications associated with recumbency should be encouraged.49 Patients in our institution are prescribed physical therapy instructions toe touch weight bearing initially with aggressive therapy focusing on the ability to be upright and ambulate if safely possible.50 In cases in which fracture instability limits weight bearing status, patients are urged to transfer from chair to bed immediately in the postoperative period.
Pain management can be difficult in the older patients. The challenge is made even greater in multiple injured patients such as those who have sustained their acetabular fracture as a result of high-energy mechanisms. Numerical scales are preferred over visual analog scales in the cognitively intact individuals. Even so, visually limited patients or patients with poor cognition should have a pain scale tailored to their needs. Because postoperative pain may be a risk factor for development of delirium,51 a multimodal approach, that includes the judicial use of opiods, can help prevent complications as well as reduce the side effects associated with stronger drugs.52
The need for thromboprophylaxis prevention in the elderly individuals following lower extremity trauma is well recognized. Early surgery and early mobilization have shown their value in the prevention of thrombotic events.53 Other measures (ie, pharmacological and/or mechanical) are needed but neither evidence-based guidelines nor a consensus has been reached. We recommend early mobilization, sequential compression boots or arteriovenous foot pumps, and at least one form of antithromboembolic pharmacologic prophylaxis.
The nutritional status of elderly trauma patients should be a primary concern of care providers. Several studies have demonstrated that poor nutrition is associated with worse outcomes after hip fractures, such as increased mortality rates, poor wound healing, and ulcer formation.54,55 In a study of predictors of mortality in elderly patients following hip fractures, Pioli et al found an association between albumin levels less than 3 with poorer outcomes.55
Summary
There is a lack of consensus with respect to treatment methods for common acetabular fracture patterns, but general consensus exists on the need for early mobilization aimed at restoring preinjury function. Acetabular fractures in the elderly population, especially those that have occurred as the result of high-energy trauma, can be complex, challenging injuries that demand a multidisciplinary approach for management. The importance of appropriate acknowledgment of the severity of the injury and the correction of hemodynamic instability patients in the elderly population is well documented. Due to the difficult nature in diagnosing these fractures, besides the standardized anteroposterior and oblique radiographs, CT may aid in diagnosis.
Once the patient is stabilized and the diagnosis has been made, a decision, based on the surgical risk and functional baseline of the patients, must be made regarding which treatment options are optimal. Evidence is based on many retrospective cohorts, most often targeting the treatment of fragility fractures (Table 2). Even though clearly defined surgical indications are lacking, special attention should be directed to early mobilization to avoid the complications of recumbency. In minimally displaced fractures, nonoperative management may be adequate but with moderate displacement, conservative methods yield generally unsatisfactory results. More contemporary minimally invasive methods have been shown to avoid lengthy procedures and show promise under certain conditions, but experience and proper technique is vital to avoid complications. Whether ORIF or minimally invasive reduction and fixation is the preferred, the treatment modality largely depends on the presence of osteoporotic bone, fracture pattern, articular damage including impaction to the acetabulum or femoral head, or severe degenerative arthritis (Figure 6).
Table 2.
Published Acetabular Fracture Studies Focusing on Elderly Patients.
| Tx Methods | Year | Author | Study Type | # Patients | Pts Followed | FU % | FU Range (months) | FU mean (months) | Age Range (Yrs) | Mean Age (Yrs) | Findings |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Nonoperative | |||||||||||
| 2001 | Leung et al | Retrospective | 60 | 53 | 88% | 12-65 | 29 | 60-101 | 78 | Patients with pelvic fractures involving the acetabulum have poorer ambulatory status | |
| 1989 | Spencer | Retrospective | 25 | 23 | 92% | 9-52 | NR | 65-95 | 74 | Internal fixation should be considered in elderly patients where there is little possibility a satisfactory results can be obtained by other means; 7 conservatively managed patients (30%) had unacceptable functional result | |
| Percutaneous | |||||||||||
| 2010 | Gary et al | Retrospective | 79 | 75 | 95% | 6-142.8 | 46.8 | nr | 73 | Most acetabular fractures are amenable to percutaneous fixation; although use of technique is limited. Overall, 25% went on to total hip replacements, 41% complication rate. | |
| 2002 | Moushine et al | Retrospective | 21 | 18 | 86% | 24-60 | 42 | 67-90 | 81 | For minimally displaced acetabular fractures, clinical results are satisfactory after percutaneous fixation | |
| Delayed THA | |||||||||||
| 2001 | Bellabarba et al | Prospective | 30 | 30 | 100% | 24-140 | 63 | 26-86 | 51 | Cementless acetabular reconstruction after acetabular fracture good/excellent results in 90% of patients despite longer OR time, greater blood loss, and more complications 17% compared with nontraumatic arthritis THA | |
| 1998 | Weber et al | Retrospective | 66 | 60 | 91% | 28.8-217.2 | 123.6 | 19-80 | 52 | Retained hardware and excessive scar tissue make delayed THA difficult; 17/60 had mechanical failure | |
| 1990 | Romness & Lewallen | Retrospective | 53 | 49 | 93% | 0.2-199 | 87.6 | 19-91 | 56.2 | Presented high rates of acetabular loosening: 4-5× that of previous studies with THA for nontraumatic arthritis | |
| Acute THA | |||||||||||
| 2010 | Herscovici et al | Retrospective | 24 | 22 | 92% | 13-67 | 29.4 | 60-95 | 75.3 | Complications, surgical times, and LOS of the combined hip procedure are similar to ORIF but avoid a second procedure | |
| 2002 | Mears et al | Retrospective | 63 | 57 | 90% | 24-144 | 97.2 | 26-89 | 69 | 78% achieved good to excellent outcomes. Acute THA may be beneficial to selected patients who have fracture patterns with a low likelihood of a favorable outcome after ORIF. | |
| ORIF | |||||||||||
| 2011 | Jeffcoat et al | Retrospective | 143 | 41 | 29% | 24-188 | 63 | 56-85 | 67 | Operative treatment through a limited illioinguinal approach offers less blood loss and a shorter operative time when compared with a traditional illioinguinal approach. The functional outcomes and quality of reduction were not sacrificed by this more minimal method | |
| 2010 | Carrol et al | Registry | 149 | 93 | 62% | 24-188 | 63 | 56-89 | 67 | Surgical intervention was safe and effective with an acceptably low rate of complication | |
| 2010 | Laflame et al | Retrospective | 21 | 19 | 91% | 50.4 | 55-82 | 64.3 | Good functional outcome and results possible with new technique | ||
| 2009 | O’Toole et al | Retrospective | 147 | 61 | 42% | 13.2-94.8 | 51.6 | Nr | 65< | 18% THA after ORIF at 2.5 yrs avg—1yearr mortality at 25% | |
| 2003 | Anglen et al | Retrospective | 48 | 27 | 56% | 1-114 | 37 | 61-88 | 71.6 | Described the gull sign (superomedial dome impaction) as an indicator for poor results with ORIF. | |
| 1992 | Helfet et al | Retrospective | 18 | 17 | 94% | >24 | 31 | 60-81 | 67 | In patients who are pre-injury ambulators, ORIF provided good/excellent results in 15/17 patients (88%) |
Abbreviations: THA, total hip arthroplasty; ORIF, open reduction and internal fixation; LOS, length of hospital stay, TX, treatment; FU, follow up; OR, operating room.
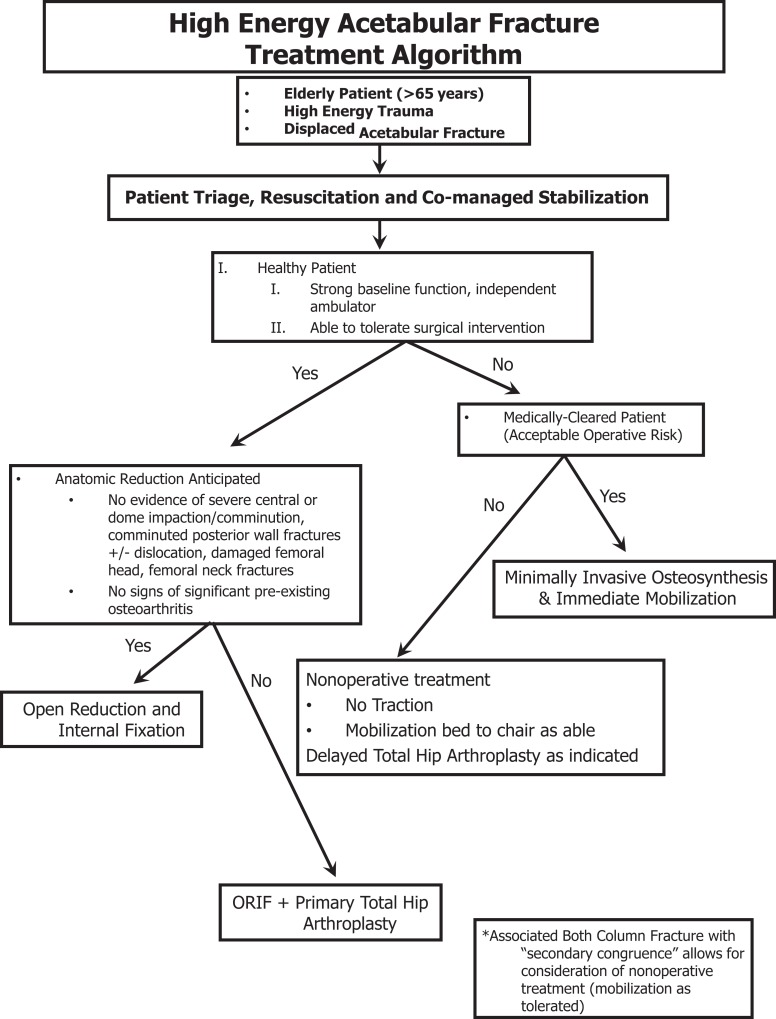
Figure 6.
The regions hospital treatment algorithm for high-energy acetabular fractures in an older population.
Further research needs must focus on this growing patient population that presents with increasing needs from an orthopedic standpoint. As the population ages, and people continue to live longer more active lives, acetabular fractures will continue to increase in prevalence. Our duty as orthopedic surgeons is to critically investigate this population and to seek to scientifically supportable optimal management.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The institution of one or more of the authors (BWH, JAS, PAC) has received, in any 1 year, funding for unrelated research from Synthes USA (Paoli, PA, USA) and Zimmer Inc (Warsaw, IN, USA). Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article:
References
- 1. Liu S, Siegel PZ, Brewer RD, Mokdad AH, Sleet DA, Serdula M. Prevalence of alcohol-impaired driving. Results from a national self-reported survey of health behaviors. JAMA. 1997;277(2):122–125 [DOI] [PubMed] [Google Scholar]
- 2. Tornetta P., 3rd Displaced acetabular fractures: indications for operative and nonoperative management. J Am Acad Orthop Surg. 2001;9(1):18–28 [DOI] [PubMed] [Google Scholar]
- 3. Matta JM, Mehne DK, Roffi R. Fractures of the acetabulum. Early results of a prospective study. Clin Orthop Relat Res. 1986;(205):241–250 [PubMed] [Google Scholar]
- 4. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645 [PubMed] [Google Scholar]
- 5. Spencer RF. Acetabular fractures in older patients. J Bone Joint Surg Br. 1989;71(5):774–776 [DOI] [PubMed] [Google Scholar]
- 6. Helfet DL, Borrelli J, Jr, DiPasquale T, Sanders R. Stabilization of acetabular fractures in elderly patients. J Bone Joint Surg Am. 1992;74(5):753–765 [PubMed] [Google Scholar]
- 7. Moed BR, McMichael JC. Outcomes of posterior wall fractures of the acetabulum. J Bone Joint Surg Am. 2007;89(6):1170–1176 [DOI] [PubMed] [Google Scholar]
- 8. Pagenkopf E, Grose A, Partal G, Helfet DL. Acetabular fractures in the elderly: treatment recommendations. HSS J. 2006;2(2):161–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970-1997 and alarming projections for the new millennium. Osteoporos Int. 2000;11(5):443–448 [DOI] [PubMed] [Google Scholar]
- 10. Ragnarsson B, Jacobsson B. Epidemiology of pelvic fractures in a Swedish county. Acta Orthop Scand. 1992;63(3):297–300 [DOI] [PubMed] [Google Scholar]
- 11. Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53(3):407–414 [DOI] [PubMed] [Google Scholar]
- 12. Carroll EA, Huber FG, Goldman AT, et al. Treatment of acetabular fractures in an older population. J Orthop Trauma. 2010;24(10):637–644 [DOI] [PubMed] [Google Scholar]
- 13. Hesp WL, Goris RJ. Conservative treatment of fractures of the acetabulum. Results after longtime follow-up. Acta Chir Belg. 1988;88(1):27–32 [PubMed] [Google Scholar]
- 14. Tornkvist H, Schatzker J. Acetabular fractures in the elderly: an easily missed diagnosis. J Orthop Trauma. 1993;7(3):233–235 [DOI] [PubMed] [Google Scholar]
- 15. Miller AN, Prasarn ML, Lorich DG, Helfet DL. The radiological evaluation of acetabular fractures in the elderly. J Bone Joint Surg Br. 2010;92(4):560–564 [DOI] [PubMed] [Google Scholar]
- 16. Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92(2):250–257 [DOI] [PubMed] [Google Scholar]
- 17. Sen RK, Veerappa LA. Long-term outcome of conservatively managed displaced acetabular fractures. J Trauma. 2009;67(1):155–159 [DOI] [PubMed] [Google Scholar]
- 18. Mears DC, Velyvis JH. Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve-year results. J Bone Joint Surg Am. 2002;84-A(1):1–9 [DOI] [PubMed] [Google Scholar]
- 19. Anglen JO, Burd TA, Hendricks KJ, Harrison P. The “gull sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma. 2003;17(9):625–634 [DOI] [PubMed] [Google Scholar]
- 20. Bhandari M, Matta J, Ferguson T, Matthys G. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br. 2006;88(12):1618–1624 [DOI] [PubMed] [Google Scholar]
- 21. Grossman MD, Miller D, Scaff DW, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J Trauma. 2002;52(2):242–246 [DOI] [PubMed] [Google Scholar]
- 22. Magnussen RA, Tressler MA, Obremskey WT, Kregor PJ. Predicting blood loss in isolated pelvic and acetabular high-energy trauma. J Orthop Trauma. 2007;21(9):603–607 [DOI] [PubMed] [Google Scholar]
- 23. Scalea TM, Simon HM, Duncan AO, et al. Geriatric blunt multiple trauma: Improved survival with early invasive monitoring. J Trauma. 1990;30(2):129–134; discussion 134-136 [PubMed] [Google Scholar]
- 24. Heffernan DS, Thakkar RK, Monaghan SF, et al. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;69(4):813–820 [DOI] [PubMed] [Google Scholar]
- 25. Ceder L, Thorngren KG, Wallden B. Prognostic indicators and early home rehabilitation in elderly patients with hip fractures. Clin Orthop Relat Res. 1980;(152):173–184 [PubMed] [Google Scholar]
- 26. Zuckerman JD, Sakales SR, Fabian DR, Frankel VH. Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program. Clin Orthop Relat Res. 1992;(274):213–225 [PubMed] [Google Scholar]
- 27. Kates SL, Mendelson DA, Friedman SM. The value of an organized fracture program for the elderly: early results. J Orthop Trauma. 2011;25(4):233–237 [DOI] [PubMed] [Google Scholar]
- 28. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77(10):1551–1556 [DOI] [PubMed] [Google Scholar]
- 29. Sexson SB, Lehner JT. Factors affecting hip fracture mortality. J Orthop Trauma. 1987;1(4):298–305 [DOI] [PubMed] [Google Scholar]
- 30. Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed Berlin, Germany: Springer-Vertag; 1993 [Google Scholar]
- 31. Tile M. Fractures of the acetabulum. Orthop Clin North Am. 1980;11(3):481–506 [PubMed] [Google Scholar]
- 32. Vanderschot P. Treatment options of pelvic and acetabular fractures in patients with osteoporotic bone. Injury. 2007;38(4):497–508 [DOI] [PubMed] [Google Scholar]
- 33. Jain R, Basinski A, Kreder HJ. Nonoperative treatment of hip fractures. Int Orthop. 2003;27(1):11–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993;(292):62–76 [PubMed] [Google Scholar]
- 35. Nousiainen MT, McConnell AJ, Zdero R, McKee MD, Bhandari M, Schemitsch EH. The influence of the number of cortices of screw purchase and ankle position in weber C ankle fracture fixation. J Orthop Trauma. 2008;22(7):473–478 [DOI] [PubMed] [Google Scholar]
- 36. Zelle BA CP. Open reduction and internal fixation of complex geriatric acetabular fracture. Oper Tech Orthop. 2011;21:286–292 [Google Scholar]
- 37. O’Toole RV, Cox G, Shanmuganathan K, et al. Evaluation of computed tomography for determining the diagnosis of acetabular fractures. J Orthop Trauma. 2010;24(5):284–290 [DOI] [PubMed] [Google Scholar]
- 38. Gary JL, Lefaivre KA, Gerold F, Hay MT, Reinert CM, Starr AJ. Survivorship of the native hip joint after percutaneous repair of acetabular fractures in the elderly. Injury. 2011;42(10):1144–1151 [DOI] [PubMed] [Google Scholar]
- 39. Gary JL, Vanhal M, Gibbons SD, Reinert CM, Starr AJ. Functional outcomes in elderly patients with acetabular fractures treated with minimally invasive reduction and percutaneous fixation. J Orthop Trauma. 2012;26(5):278–283 [DOI] [PubMed] [Google Scholar]
- 40. Schwan C, Swanson M, Huo M, et al. Total hip arthroplasty following previous acetabular fracture. Paper Presented at: the 2009 Hip Society Summer Meeting; 2009 [Google Scholar]
- 41. Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87(1):2–9 [PubMed] [Google Scholar]
- 42. Van Flandern GJ, Bierbaum BE, Newberg AH, Gomes SL, Mattingly DA, Karpos PA. Intermediate clinical follow-up of a dual-radius acetabular component. J Arthroplasty. 1998;13(7):804–811 [DOI] [PubMed] [Google Scholar]
- 43. Kavanagh BF, Dewitz MA, Ilstrup DM, Stauffer RN, Coventry MB. Charnley total hip arthroplasty with cement. Fifteen-year results. J Bone Joint Surg Am. 1989;71(10):1496–1503 [PubMed] [Google Scholar]
- 44. Weber M, Berry DJ, Harmsen WS. Total hip arthroplasty after operative treatment of an acetabular fracture. J Bone Joint Surg Am. 1998;80(9):1295–1305 [DOI] [PubMed] [Google Scholar]
- 45. Romness DW, Lewallen DG. Total hip arthroplasty after fracture of the acetabulum. Long-term results. J Bone Joint Surg Br. 1990;72(5):761–764 [DOI] [PubMed] [Google Scholar]
- 46. Bellabarba C, Berger RA, Bentley CD, et al. Cementless acetabular reconstruction after acetabular fracture. J Bone Joint Surg Am. 2001;83-A(6):868–876 [DOI] [PubMed] [Google Scholar]
- 47. Tidermark J, Blomfeldt R, Ponzer S, Soderqvist A, Tornkvist H. Primary total hip arthroplasty with a burch-schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma. 2003;17(3):193–197 [DOI] [PubMed] [Google Scholar]
- 48. Herscovici D, Jr, Lindvall E, Bolhofner B, Scaduto JM. The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma. 2010;24(5):291–296 [DOI] [PubMed] [Google Scholar]
- 49. Harper CM, Lyles YM. Physiology and complications of bed rest. J Am Geriatr Soc. 1988;36(11):1047–1054 [DOI] [PubMed] [Google Scholar]
- 50. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995;(310):150–159 [PubMed] [Google Scholar]
- 51. Juliebo V, Bjoro K, Krogseth M, Skovlund E, Ranhoff AH, Wyller TB. Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture. J Am Geriatr Soc. 2009;57(8):1354–1361 [DOI] [PubMed] [Google Scholar]
- 52. Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E. Equianalgesic dose ratios for opioids. A critical review and proposals for long-term dosing. J Pain Symptom Manage. 2001;22(2):672–687 [DOI] [PubMed] [Google Scholar]
- 53. Marsland D, Mears SC, Kates SL. Venous thromboembolic prophylaxis for hip fractures. Osteoporos Int. 2010;21(suppl 4):S593–S604 [DOI] [PubMed] [Google Scholar]
- 54. Patterson BM, Cornell CN, Carbone B, Levine B, Chapman D. Protein depletion and metabolic stress in elderly patients who have a fracture of the hip. J Bone Joint Surg Am. 1992;74(2):251–260 [PubMed] [Google Scholar]
- 55. Pioli G, Barone A, Giusti A, et al. Predictors of mortality after hip fracture: Results from 1-year follow-up. Aging Clin Exp Res. 2006;18(5):381–387 [DOI] [PubMed] [Google Scholar]