Abstract
Objectives:
To evaluate disparities in cardiovascular risk factors among Asians and Native Hawaiians and other Pacific Islanders (NHPI) in Hawaii who are hospitalized with ischemic stroke.
Methods:
We performed a retrospective study on consecutive patients hospitalized for ischemic stroke at a single tertiary center in Honolulu between 2004 and 2010. The prevalence of cardiovascular risk factors was compared for NHPI, Asians, and whites who were hospitalized for ischemic stroke.
Results:
A total of 1,921 patients hospitalized for ischemic stroke were studied. NHPI were less likely to be older (odds ratio [OR] 0.95, 95% confidence interval [CI] 0.94–0.96), more likely to be female (OR 1.55, 95% CI 1.07–2.24), and more likely to have diabetes (OR 2.74, 95% CI 1.87–4.00), hypertension (OR 1.98, 95% CI 1.27–3.10), and obesity (OR 1.82, 95% CI 1.25–2.65) than whites. NHPI had higher low-density lipoprotein levels (114 ± 50 mg/dL vs 103 ± 45 mg/dL, p = 0.001) and lower high-density lipoprotein levels (38 ± 11 mg/dL vs 45 ± 15 mg/dL, p < 0.0001) than whites. Compared with Asians, NHPI were less likely to be older (OR 0.95, 95% CI 0.94–0.97) and more likely to have diabetes (OR 1.88, 95% CI 1.35–2.61), previous stroke or TIA (OR 1.57, 95% CI 1.09–2.25), and obesity (OR 6.05, 95% CI 4.31–8.48).
Conclusions:
Asians, NHPI, and whites with ischemic stroke have substantially different cardiovascular risk factors. Targeted secondary prevention will be important in reducing disparities among these racial groups.
Stroke occurs in approximately 800,000 people annually in the United States and is the leading cause of disability among adults.1 Recent evidence suggests that the burden of ischemic stroke is not borne equally by all, with racial minority groups reported to have a higher burden of stroke risk factors2–7 and younger age of stroke onset compared with non-Hispanic whites.4,8 However, these studies mainly focused on blacks and Hispanics, leaving a paucity of data on other racial/ethnic groups with ischemic stroke. Specifically, Asian Americans and Native Hawaiians and other Pacific Islanders (NHPI) are underrepresented in many stroke studies.9 Furthermore, NHPI have been historically aggregated with Asians into a single racial/ethnic category in many clinical studies, which masks differences that may, at times, be substantial.
For example, NHPI in the community have been shown to have higher prevalence of major cardiovascular risk factors10–15 and die at a younger age from various cardiovascular disease–related complications compared with other major racial groups.16,17 However, the specific disease burden related to ischemic stroke in the NHPI and Asian populations has not been studied.18 Therefore, we sought to assess racial disparities in risk factors among an ischemic stroke patient population that predominantly consists of NHPI, Asians, and whites. We hypothesized that NHPI with ischemic stroke are younger and have a higher burden of cardiovascular risk factors compared with whites and have different characteristics compared with Asians.
METHODS
We conducted a single-center, observational study using the Get With the Guidelines–Stroke (GWTG-Stroke) registry, a national quality-improvement initiative and stroke registry used by many participating hospitals nationwide.19 Since its inception in 2004, the GWTG-Stroke registry has been used in our institution to measure and monitor the quality of hospital-based stroke-care delivery.
Patients.
The Queen's Medical Center (QMC) is a 505-bed medical center located on Oahu, the largest hospital in Hawaii and the tertiary referral center for the Pacific Basin (Hawaii, American Samoa, the Commonwealth of the Northern Mariana Islands, Micronesia, and the US territories of Guam). QMC has the only Joint Commission–certified Primary Stroke Center and the only Neuroscience Intensive Care Unit for the state of Hawaii.
All patients hospitalized at QMC with a diagnosis of ischemic stroke between January 1, 2004 and August 31, 2010 were identified using the QMC GWTG-Stroke database. This database includes all patients with ischemic stroke, hemorrhagic stroke, or TIA, identified at the time of hospital admission through imaging results and admission diagnosis, with confirmation of eligibility based on medical record review by a trained nurse reviewer (S.M.A.).
Baseline characteristics.
Patient demographics and whether the patient was transferred from another hospital were obtained through the database. The race and ethnicity information was collected from the hospital's administrative database and obtained during the registration or admission process according to a standard protocol. Race was initially categorized as NHPI, Asian, white, black, American Indian/Alaska native, or “other” race. Because of the low number of black and American Indian/Alaska native patients, these racial groups were combined with the “other” group. Because a mixed racial background is relatively common in Hawaii, race was defined as the racial background that the patient most closely associated with and was based on patient self-identification or family's identification if the patient was incapacitated. Additional data on body mass index (BMI), total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides were also collected if they were available. The patients were considered to be obese if BMI was ≥30 kg/m2.20
Outcome measures.
The prevalence of cardiovascular risk factors including history of diabetes mellitus, hypertension, atrial fibrillation/atrial flutter, congestive heart failure, prior stroke or TIA, coronary artery disease or prior myocardial infarction, peripheral vascular disease, smoking, dyslipidemia, and prosthetic valve replacement were the selected clinical outcomes.
Standard protocol approvals, registrations, and patient consents.
We received approval from the QMC Research and Institutional Review Committee to conduct this retrospective review of the prospectively collected QMC GWTG-Stroke database. Waiver of consent was obtained to conduct this study.
Statistical analysis.
Data were analyzed using commercially available statistical software (SPSS 19.0; SPSS, Inc., Chicago, IL). Patient characteristics were summarized using descriptive statistics appropriate to variable type. The prevalence of each cardiovascular risk factor was estimated for NHPI, Asians, and whites. In the primary analysis, NHPI and Asians were compared with whites (reference group) using χ2 test or Fisher exact test for categorical data and 2-tailed t test for normally distributed, continuous variables. In the multivariable analyses, we developed 2 separate logistic regression models to compare 1) NHPI with whites, and 2) Asians with whites, after incorporating age, sex, and each of the cardiovascular risk factors in the 2 models. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated from the β coefficients and their standard errors. In secondary analyses, NHPI were compared with Asians (reference group) using univariate and multivariable analyses similar to the above approach. Data are presented as means ± SD, and levels of p < 0.05 were considered statistically significant.
RESULTS
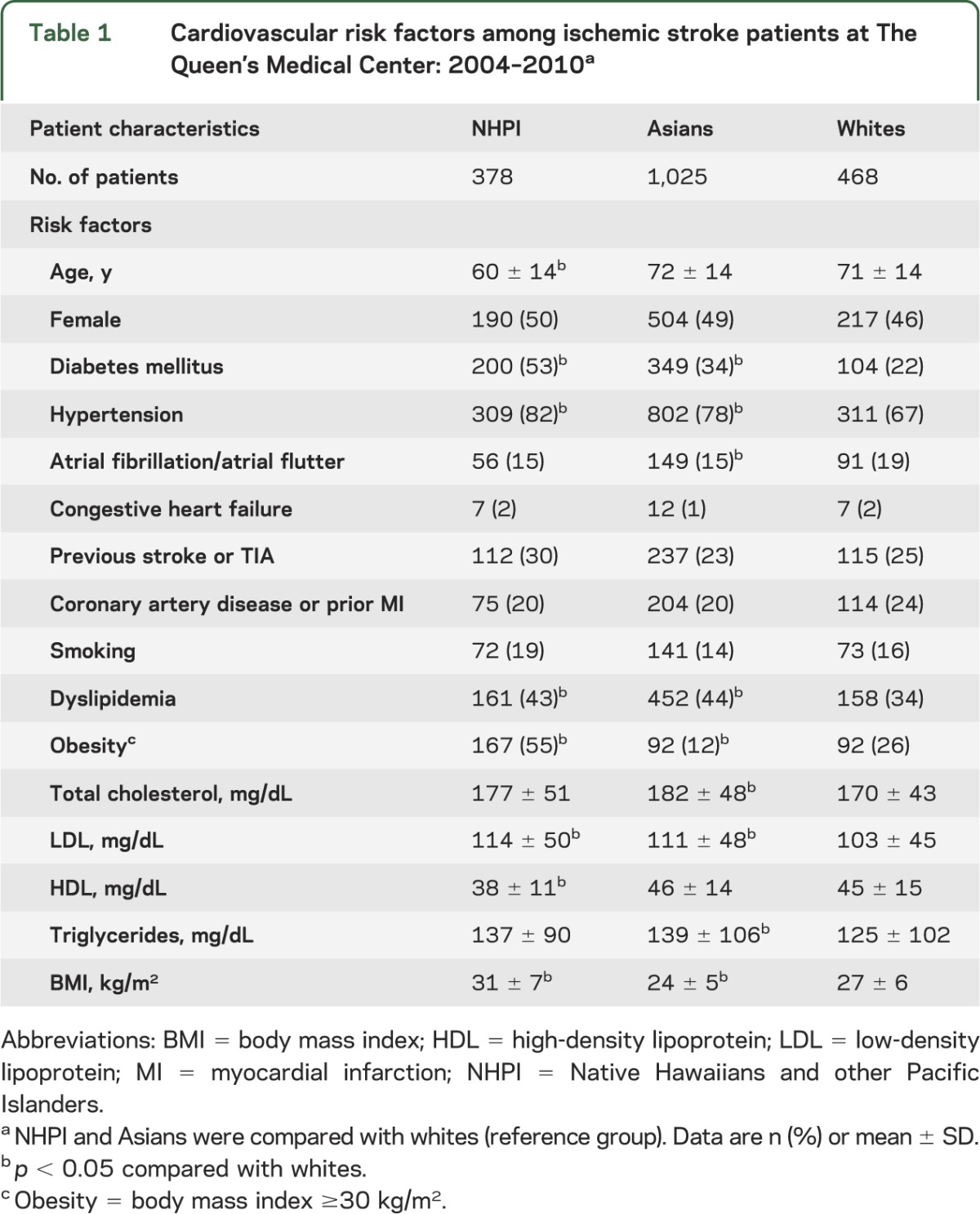
Between January 2004 and August 2010, a total of 1,921 consecutive patients hospitalized for ischemic stroke (NHPI 20%, Asians 53%, whites 24%, and others 3%) were identified. Unadjusted analyses showed that NHPI were younger (60 ± 14 years vs 71 ± 14 years, p < 0.0001) and more likely to have diabetes, hypertension, dyslipidemia, and obesity than whites (table 1). NHPI also had higher LDL, lower HDL, and higher BMI than whites (table 1). Asians were more likely to have diabetes, hypertension, and dyslipidemia than whites, but less likely to have atrial fibrillation/atrial flutter and obesity (table 1). Asians had higher total cholesterol, LDL levels, and triglyceride levels, and lower BMI than whites (table 1).
Table 1.
Cardiovascular risk factors among ischemic stroke patients at The Queen's Medical Center: 2004–2010a
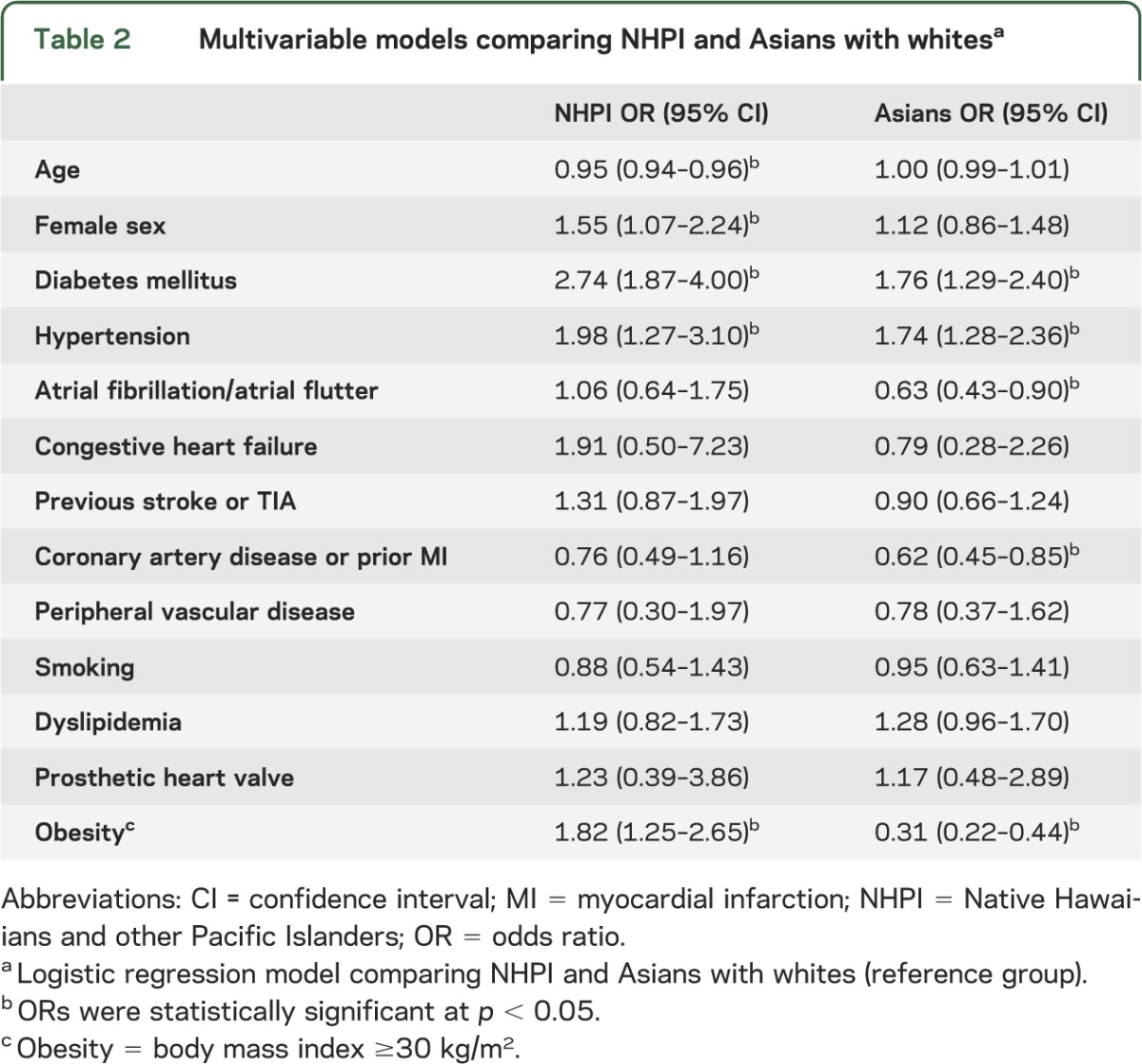
All results from logistic regression models, comparing NHPI with whites and Asians with whites, are shown in table 2. NHPI were less likely to be older (OR 0.95, 95% CI 0.94–0.96), more likely to be female (OR 1.55, 95% CI 1.07–2.24), and more likely to have diabetes (OR 2.74, 95% CI 1.87–4.00), hypertension (OR 1.98, 95% CI 1.27–3.10), and obesity (OR 1.82, 95% CI 1.25–2.65) than whites. Asians were more likely to have diabetes (OR 1.76, 95% CI 1.29–2.40) and hypertension (OR 1.74, 95% CI 1.28–2.36) but less likely to have atrial fibrillation/atrial flutter (OR 0.63, 95% 0.43–0.90), coronary artery disease or prior myocardial infarction (OR 0.62, 95% CI 0.45–0.85), and obesity (0.31, 95% 0.22–0.44) than whites.
Table 2.
Multivariable models comparing NHPI and Asians with whitesa
Secondary analyses, comparing NHPI with Asians, showed that NHPI were younger (p < 0.0001) and had higher prevalence of diabetes (p < 0.0001), prior stroke or TIA (p = 0.01), smoking (p = 0.01), obesity (p < 0.0001), and had lower HDL levels (p < 0.0001) and higher BMI (p < 0.0001) compared with Asians in the univariate analyses. In the logistic regression model, NHPI were less likely to be older (OR 0.95, 95% CI 0.94–0.97) and more likely to have diabetes (OR 1.88, 95% CI 1.35–2.61), previous stroke or TIA (OR 1.57, 95% CI 1.09–2.25), and obesity (OR 6.05, 95% CI 4.31–8.48) than Asians.
DISCUSSION
Our study demonstrates that NHPI and Asians hospitalized for ischemic stroke substantially differ from whites, and from each other, supporting recent recommendations for the need to further study these underrepresented populations.9 We found that NHPI are younger and have a higher burden of cardiovascular risk factors compared with whites. Furthermore, NHPI have a higher prevalence of metabolic syndrome characteristics (diabetes, obesity, and/or lower HDL levels) compared with whites, which is consistent with prior studies.10–15
In our study, NHPI with ischemic stroke were a decade younger than whites, a finding similar to the results of other observational ischemic stroke studies that compared non-Hispanic whites to Maoris from New Zealand,21 Hispanics,4,22 and blacks.4,22 The higher burden of cardiovascular risk factors seen in NHPI is similar to the disparities seen among Hispanics and blacks,5–7,22 and supports the idea that minority racial groups overall have a younger age of stroke onset and higher burden of cardiovascular risk factors compared with whites.18 Importantly, in our study, the clinical characteristics of NHPI substantially differ from those of the Asians.
Asians in our study who experienced ischemic stroke were more likely to have hypertension and diabetes compared with whites, but were less likely to have atrial fibrillation/atrial flutter, coronary artery disease or prior myocardial infarction, and obesity. In contrast with NHPI, there was no difference in the age of presentation between Asians and whites. Although there were prior studies that characterized Asian stroke patients, many focused on Asians living outside of the United States, rather than Asian Americans living in the United States.23–28 Because the incidence of ischemic stroke and the prevalence of cardiovascular risk factors are known to differ between Asians living in Asia and Asian Americans living in the United States,29 possibly through the effect of diet and other environmental factors, it is difficult to generalize the results of these prior studies to the Asian Americans. One study that compared the stroke incidence between first- or second-generation Japanese-American men in the Honolulu Heart Program and white men in the Framingham Study showed that the incidence of thromboembolic stroke was significantly less among Japanese-American men than white men after adjusting for traditional risk factors.30 Another study showed that Asian Americans have more severe stroke complications, such as dysphagia, hemiplegia, and aphasia, compared with whites.31 Nevertheless, the paucity of data on the burden of stroke among a more diverse and acculturated population of Asian Americans emphasizes the need for further studies in this racial group.
Reasons for racial disparities in ischemic stroke are complex, and likely involve both biological and social determinants of the disease. The disparities in cardiovascular risk factors may partially be attributed to the biological differences in genetic polymorphisms among the different racial groups, which may predispose one racial group to be more susceptible to developing a cardiovascular disease compared with another racial group. Furthermore, the response to cardiovascular prevention drugs may be influenced by variability in drug metabolism due to genetic polymorphisms.32 However, more recent studies suggest that many of these differences in cardiovascular disease burden may be attributed to the consequences of gene-environment interactions,9 and emphasize the complex effect of the social environment. Indeed, significant racial disparities in awareness of stroke symptoms and signs, attitude and beliefs toward health care, health literacy, medication adherence, access to care, and primary prevention have been reported in a number of stroke studies.18 Although addressing each of these factors is important in the future endeavor to reduce stroke disparities, little emphasis has been placed on developing a culturally specific secondary stroke prevention program. Because NHPI and Asians with ischemic stroke in our study had a substantially different cardiovascular disease burden compared with whites, a uniform approach to secondary stroke prevention may not adequately address the health care needs in these populations. Therefore, a future, culturally sensitive, and targeted secondary stroke prevention trial may be warranted to effectively reduce the burden of stroke in these unique racial groups that have a different cardiovascular disease burden than whites.
This study has several limitations. First, the data on the pattern of the ischemic strokes and intracranial/extracranial vascular anatomy were not available, and thus it is unclear whether there are racial disparities in stroke etiologies (i.e., lacunar strokes, intracranial/extracranial large-artery diseases, and cardioembolic strokes). Second, Asian ethnicity was not further specified (i.e., Japanese, Filipino, Chinese, Korean, etc.), and thus it is unclear whether there are disparities between each of the specific Asian ethnic groups. Third, we were unable to assess for potential disparities in long-term outcome among the NHPI with ischemic stroke as previously shown in black stroke patients in the United States33,34 and the Pacific people in New Zealand.35 Fourth, our database did not exclude repeat hospitalizations, and it is possible that individual patients were included in the database more than once. Fifth, we did not have sufficient data on insurance status, and thus we were unable to assess its impact on the observed disparities. Sixth, due to the single-center study design, our results may not be generalizable to other populations. Overall, our institution captures approximately 21% of all ischemic stroke hospitalization for the state of Hawaii (data from Hawaii Health Information Corporation). Because our institution is a tertiary referral center, there may have been a referral bias toward patients with more severe stroke and more extensive comorbidities. Also, it is possible that older stroke patients with preexisting do-not-resuscitate orders or those with terminal illness may not have transferred to our facility, creating a possible selection bias toward younger stroke patients. Although we acknowledge the limitation of a single-center study, we believe this is an important first glance at the possible racial disparities in stroke risk factors seen in the state of Hawaii.
Asians, NHPI, and whites with ischemic stroke have substantially different cardiovascular risk factors. Our study highlights the importance of not aggregating NHPI with Asians in future stroke studies given their marked differences in the burden of risk factors. A culturally sensitive and targeted secondary prevention strategy will be important in reducing disparities among these racial groups.
DISCLAIMER
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Hawaii Community Foundation, AHA, NSF, NCRR, NCMHD, AHRQ, or NIH.
GLOSSARY
- BMI
body mass index
- CI
confidence interval
- GWTG-Stroke
Get With the Guidelines–Stroke
- HDL
high-density lipoprotein
- LDL
low-density lipoprotein
- NHPI
Native Hawaiians and other Pacific Islanders
- OR
odds ratio
- QMC
Queen's Medical Center
AUTHOR CONTRIBUTIONS
K.N. participated in the conception and design of the study, the analysis and interpretation of data, and was responsible for drafting and finalizing the manuscript. M.A.K. participated in the analysis and interpretation of data and helped to draft and finalize the manuscript. S.M.A. participated in the acquisition of data, analysis and interpretation of data, and finalization of the manuscript. C.W.C. participated in the analysis and interpretation of the data, and helped to draft and finalize the manuscript. T.B.S. participated in the conception and design of the study, study supervision, analysis and interpretation of data, and helped to draft and finalize the manuscript. All authors read and approved the final manuscript.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
K. Nakagawa has received research support from the American Heart Association (11CRP7160019), Hawaii Community Foundation (10ADVC-47086), and Queen Emma Research Fund. M. Koenig has received research support from the Hawaii Community Foundation (11ADVC-49231) and Queen Emma Research Fund. S. Asai and C. Chang have no disclosures to report. T. Seto has received research support from the NCMHD (5P20MD000173), AHRQ (1R01HS019990-01), NCRR (U54RR026136), NSF (CBET-1160326), and Hawaii Community Foundation (10ADVC-47032). Go to Neurology.org for full disclosures.
REFERENCES
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011;123:e18–e209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke 2005;36:374–386 [DOI] [PubMed] [Google Scholar]
- 3.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:480–486 [DOI] [PubMed] [Google Scholar]
- 4.Sacco RL, Boden-Albala B, Gan R, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol 1998;147:259–268 [DOI] [PubMed] [Google Scholar]
- 5.McGruder HF, Malarcher AM, Antoine TL, Greenlund KJ, Croft JB. Racial and ethnic disparities in cardiovascular risk factors among stroke survivors: United States 1999 to 2001. Stroke 2004;35:1557–1561 [DOI] [PubMed] [Google Scholar]
- 6.Hajat C, Dundas R, Stewart JA, et al. Cerebrovascular risk factors and stroke subtypes: differences between ethnic groups. Stroke 2001;32:37–42 [DOI] [PubMed] [Google Scholar]
- 7.Hassaballa H, Gorelick PB, West CP, Hansen MD, Adams HP., Jr Ischemic stroke outcome: racial differences in the trial of danaparoid in acute stroke (TOAST). Neurology 2001;57:691–697 [DOI] [PubMed] [Google Scholar]
- 8.Schwamm LH, Reeves MJ, Pan W, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation 2010;121:1492–1501 [DOI] [PubMed] [Google Scholar]
- 9.Palaniappan LP, Araneta MR, Assimes TL, et al. Call to action: cardiovascular disease in Asian Americans: a science advisory from the American Heart Association. Circulation 2010;122:1242–1252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erber E, Hopping BN, Grandinetti A, Park SY, Kolonel LN, Maskarinec G. Dietary patterns and risk for diabetes: the multiethnic cohort. Diabetes Care 2010;33:532–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curb JD, Aluli NE, Kautz JA, et al. Cardiovascular risk factor levels in ethnic Hawaiians. Am J Public Health 1991;81:164–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mau MK, Grandinetti A, Arakaki RF, Chang HK, Kinney EK, Curb JD. The insulin resistance syndrome in native Hawaiians: Native Hawaiian Health Research (NHHR) Project. Diabetes Care 1997;20:1376–1380 [DOI] [PubMed] [Google Scholar]
- 13.Henderson SO, Haiman CA, Wilkens LR, Kolonel LN, Wan P, Pike MC. Established risk factors account for most of the racial differences in cardiovascular disease mortality. PLoS One 2007;2:e377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mau MK, Sinclair K, Saito EP, Baumhofer KN, Kaholokula JK. Cardiometabolic health disparities in native Hawaiians and other Pacific Islanders. Epidemiol Rev 2009;31:113–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moy KL, Sallis JF, David KJ. Health indicators of Native Hawaiian and Pacific Islanders in the United States. J Community Health 2010;35:81–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aluli NE, Reyes PW, Tsark J. Cardiovascular disease disparities in native Hawaiians. J Cardiometab Syndr 2007;2:250–253 [DOI] [PubMed] [Google Scholar]
- 17.Balabis J, Pobutsky A, Kromer Baker K, Tottori C, Salvail F. The Burden of Cardiovascular Disease in Hawaii 2007. Honolulu: Hawaii State Department of Health; 2007 [Google Scholar]
- 18.Cruz-Flores S, Rabinstein A, Biller J, et al. Racial-ethnic disparities in stroke care: the American experience—a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:2091–2116 [DOI] [PubMed] [Google Scholar]
- 19.Schwamm LH, Fonarow GC, Reeves MJ, et al. Get With the Guidelines–Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation 2009;119:107–115 [DOI] [PubMed] [Google Scholar]
- 20.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002;288:1723–1727 [DOI] [PubMed] [Google Scholar]
- 21.Feigin V, Carter K, Hackett M, et al. Ethnic disparities in incidence of stroke subtypes: Auckland Regional Community Stroke Study, 2002–2003. Lancet Neurol 2006;5:130–139 [DOI] [PubMed] [Google Scholar]
- 22.Sacco RL, Kargman DE, Zamanillo MC. Race-ethnic differences in stroke risk factors among hospitalized patients with cerebral infarction: the Northern Manhattan Stroke Study. Neurology 1995;45:659–663 [DOI] [PubMed] [Google Scholar]
- 23.Fang XH, Zhang XH, Yang QD, et al. Subtype hypertension and risk of stroke in middle-aged and older Chinese: a 10-year follow-up study. Stroke 2006;37:38–43 [DOI] [PubMed] [Google Scholar]
- 24.Jiang B, Wang WZ, Chen H, et al. Incidence and trends of stroke and its subtypes in China: results from three large cities. Stroke 2006;37:63–68 [DOI] [PubMed] [Google Scholar]
- 25.Hu HH, Chu FL, Chiang BN, et al. Prevalence of stroke in Taiwan. Stroke 1989;20:858–863 [DOI] [PubMed] [Google Scholar]
- 26.Urakami K, Igo M, Takahashi K. An epidemiologic study of cerebrovascular disease in western Japan: with special reference to transient ischemic attacks. Stroke 1987;18:396–401 [DOI] [PubMed] [Google Scholar]
- 27.Banerjee TK, Choudhury D, Das A, Sekhar A, Roy D, Sen S. Analysis of hospital-based stroke registry in a neurological centre in Kolkata. J Indian Med Assoc 2005;103:665–668 [PubMed] [Google Scholar]
- 28.Razdan S, Koul RL, Motta A, Kaul S. Cerebrovascular disease in rural Kashmir, India. Stroke 1989;20:1691–1693 [DOI] [PubMed] [Google Scholar]
- 29.Takeya Y, Popper JS, Shimizu Y, Kato H, Rhoads GG, Kagan A. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: incidence of stroke in Japan and Hawaii. Stroke 1984;15:15–23 [DOI] [PubMed] [Google Scholar]
- 30.Rodriguez BL, D'Agostino R, Abbott RD, et al. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke 2002;33:230–236 [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez-Fernandez M, Kuhlemeier KV, Palmer JB. Racial disparities in the development of dysphagia after stroke: analysis of the California (MIRCal) and New York (SPARCS) inpatient databases. Arch Phys Med Rehabil 2008;89:1358–1365 [DOI] [PubMed] [Google Scholar]
- 32.Takahashi H, Wilkinson GR, Caraco Y, et al. Population differences in S-warfarin metabolism between CYP2C9 genotype-matched Caucasian and Japanese patients. Clin Pharmacol Ther 2003;73:253–263 [DOI] [PubMed] [Google Scholar]
- 33.Horner RD, Matchar DB, Divine GW, Feussner JR. Racial variations in ischemic stroke-related physical and functional impairments. Stroke 1991;22:1497–1501 [DOI] [PubMed] [Google Scholar]
- 34.Horner RD, Swanson JW, Bosworth HB, Matchar DB. Effects of race and poverty on the process and outcome of inpatient rehabilitation services among stroke patients. Stroke 2003;34:1027–1031 [DOI] [PubMed] [Google Scholar]
- 35.McNaughton H, Feigin V, Kerse N, et al. Ethnicity and functional outcome after stroke. Stroke 2011;42:960–964 [DOI] [PubMed] [Google Scholar]


