Abstract
Background
Few emergency department (ED) evaluations on acute lung injury (ALI) have been carried out; hence, we sought to describe a cohort of hospitalized ED patients at risk for ALI development.
Methods
Patients presenting to the ED with at least one predisposing condition to ALI were included in this study, a subgroup analysis of a multicenter observational cohort study (USCIITG-LIPS 1). Patients who met ALI criteria within 6 h of initial ED assessment, received end-of-life care, or were readmitted during the study period were excluded. Primary outcome was frequency of ALI development; secondary outcomes were ICU and hospital mortality.
Results
Twenty-two hospitals enrolled 4,361 patients who were followed from the ED to hospital discharge. ALI developed in 303 (7.0 %) patients at a median onset of 2 days (IQR 2–5). Of the predisposing conditions, frequency of ALI development was highest in patients who had aortic surgery (43 %) and lowest in patients with pancreatitis (2.8 %). Compared to patients who did not develop ALI, those who did had higher ICU (24 % vs. 3.0 %, p < 0.001) and hospital (28 % vs. 4.6 %, p < 0.001) mortality, and longer hospital length of stay (16 vs. 5 days, p < 0.001). Among the 22 study sites, frequency of ALI development varied from less than 1 % to more than 12 % after adjustment for APACHE II.
Conclusions
Seven percent of hospitalized ED patients with at least one predisposing condition developed ALI. The frequency of ALI development varied significantly according to predisposing conditions and across institutions. Further research is warranted to determine the factors contributing to ALI development.
Background
Adult respiratory distress syndrome (ARDS) was first described by Ashbaugh [1] in 1967. Since then, the definition and criteria for this syndrome have evolved. At the 1994 American–European Consensus Conference (AECC), experts agreed to the following terminology: Acute lung injury (ALI) was defined as the acute onset of hypoxemia [PaO2/FiO2 (partial pressure of arterial oxygen/fractional concentration of inspired oxygen) ≤ 300 mmHg] and bilateral infiltrates on frontal chest x-ray (Figure 1), in the clinical absence of left atrial hypertension (or when measured, pulmonary-artery wedge pressure < 18 mm Hg) [2]. ARDS is the more severe form of ALI with hypoxemia at 200 mmHg or less [2-4]. In the US, approximately 150,000 to 190,600 cases of ALI occur annually, with an associated mortality rate of 38 to 44 %, 3.6 million hospital days, and long-term functional disabilities and cost after intensive care unit (ICU) discharge [5-8]. Pathophysiologically, ALI is classically characterized by an increased permeability of the alveolar-capillary membrane resulting in the influx of protein-rich edema fluid into the air spaces, and etiologies of ALI are myriad, including direct (pulmonary) and indirect (extrapulmonary) causes [3,4,9].
Figure 1.
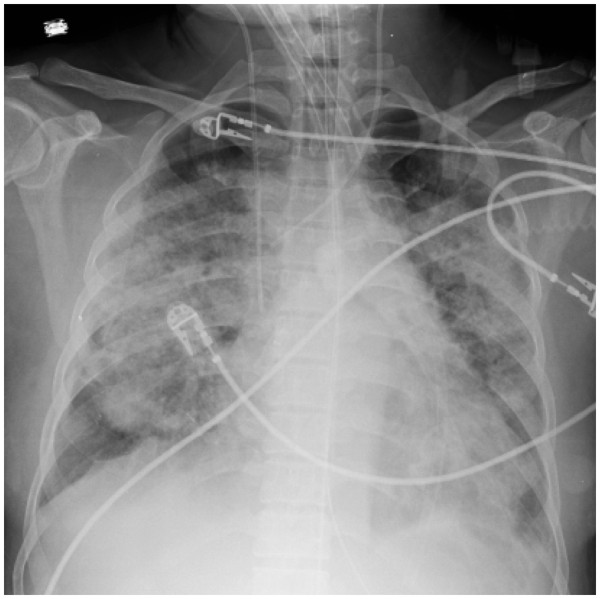
Chest x-ray representing acute lung injury.
Importance
Despite numerous randomized controlled trials, a lung protective strategy during mechanical ventilation remains the only therapy shown to improve survival in patients with established ALI [3,4,10-12]. According to the “two-hit” model of ALI development before ALI becomes clinically apparent, a pre-ALI state exists following the first injury to the lungs. The United States Critical Illness and Injury Trials Group-Lung Injury Prevention Study (USCIITG-LIPS 1) investigators focused on defining patient characteristics that would allow us to identify these patients before overt ALI develops. Interventions delivered in this early phase of care can offer potential prevention of ALI. As most clinical studies in ALI have primarily focused on mechanically ventilated patients, insight into a potentially preventable phase of ALI prior to its development is currently lacking [13,14]. Data suggest that ALI is rarely present at the time of initial Emergency Department (ED) evaluation; however, a search in top emergency medicine journals yielded many case reports of patients presenting with ALI [15-18]. In reality, many ED patients may have unrecognized ALI and possess many predisposing conditions for ALI development. Recently, a National Heart Lung Blood Institute Workshop Report on future clinical research in ALI recommended to continue the development of strategies to perform ALI prevention trials and observational studies of patients without ALI undergoing prolonged mechanical ventilation [19]. Following the paradigm of trauma team care for major trauma, activation of the cardiac catheterization laboratory team for ST-elevation myocardial infarction and acute stroke teams for ischemic stroke, and early goal-directed therapy for severe sepsis, clinical benefit may be derived from early identification of and preventative interventions for patients at risk of developing ALI.
Goal of this investigation
We evaluated the frequency of ALI development in at-risk hospitalized ED patients among the study sites, described the predisposing conditions and risk modifiers of ALI development, and determined the attribution of ALI to hospital mortality.
Methods
Study design
This is a subgroup analysis of data from a multicenter, observational cohort study, the United States Critical Injury and Illness Trials Group-Lung Injury Prevention Study 1 (USCIITG-LIPS 1) [20,21]. All participating study sites received approval from their respective local institutional review board. The study flow diagram is illustrated in Additional file 1: Appendix 1.
Study setting
From March through August 2009, 22 centers (20 American and 2 Turkish hospitals) enrolled patients with at least one ALI predisposition admitted from the ED. Patients were enrolled prospectively at 19 study sites and retrospectively at 3 sites.
Selection of participants
Consecutive adult ED patients admitted to academic and community acute care hospitals were eligible for the study if they presented with one or more a priori defined conditions predisposing to ALI (shock, aspiration, sepsis, pancreatitis, pneumonia, high-risk trauma: traumatic brain injury, smoke inhalation, near drowning, lung contusion, multiple fractures; high-risk surgery: thoracic, spine, acute abdomen, cardiac, aortic vascular; and emergency surgery). Patients were excluded when ALI was present at initial assessment, if they were transferred from an in-patient setting, died in the ED, admitted for comfort or hospice care, or re-admitted during the study period. Hospital admission logs were reviewed to minimize the possibility that patients with predisposing conditions were missed. After identification of at-risk ED patients, they were followed through their hospitalization prospectively in 19 hospitals. In the three hospitals that enrolled retrospectively, investigators followed the same protocol and definitions, but data were collected after patient discharge.
Data collection and processing
Baseline characteristics, including demographics, comorbidities, and clinical variables, were collected during the first 6 h of initial ED evaluation. Predisposing conditions and ALI risk modifiers were identified and collected. Predisposing conditions were pre-defined, and ALI risk modifiers included: alcohol abuse, obesity chemotherapy, diabetes mellitus, smoking, tachypnea, hypoxemia, oxygen supplementation, hypoalbuminemia, and acidosis.
De-identified subject information was entered at each center into the secure, password-protected NIH-supported web form (REDCap http://www.project-redcap.org). Electronic range checks and validation rules were utilized to eliminate erroneous data entry and artifacts in numeric values. Prior to study initiation at each site, investigators and study coordinators reviewed the definitions of each risk factor (see Additional file 1: Appendix 2) and received mandatory structured online training for ALI assessment. Briefly, in determining if a chest radiograph is consistent with ALI, assessment begins with interpretability of the x-ray followed by evaluation for bilateral opacities generally described as infiltrates consistent with pulmonary edema. Only when the bilateral opacities are not fully explained by non-qualifying opacities (i.e., pulmonary fibrosis) and not limited to the lower lung zones with normal parenchyma above is the chest radiograph consistent with ALI. In addition, a formal training session was provided during the 2009 USCIITG meeting in Nashville, TN. The principal investigators from each site were responsible for data collection and entry, as well as quality control.
Outcome measures
The primary outcome was the development of AECC-defined ALI during the hospital admission of at-risk ED patients. Secondary outcomes included time to ALI development; proportion and duration of invasive and non-invasive mechanical ventilation; vasopressor requirement; acute renal failure requiring hemodialysis; and ICU and hospital length of stay and mortality.
Primary data analysis
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were followed in the design and reporting of this observational study [22]. PCH and AM analyzed the data, which were summarized as number (in percentage) and median (with inter-quartile range). Missing data were coded explicitly as described and handled by using logic expression. Continuous variables were dichotomized at the median. The odds ratios and 95 % confidence intervals were computed from performing logistic regression. Statistical significance was set at 0.05 for regression analysis. Frequency of ALI was calculated per number of ED patients presenting with predisposing condition at the time of hospital admission.
In order to evaluate our secondary outcome measures, we compared hospital and ICU mortality and length of stay between ED patients at risk who developed ALI and those who did not. To determine the mortality burden attributed to the development of ALI, we performed a logistic regression analysis adjusted for the baseline Acute Physiology and Chronic Health Evaluation (APACHE II) score [23]. In addition, we described the utilization and duration of invasive and non-invasive mechanical ventilation, and performed an exploratory analysis comparing patients who did and did not develop ALI with respect to their initial vent settings, specifically tidal volume per predicted body weight, plateau pressure, and positive end expiratory pressure (PEEP). Lastly, we illustrated the frequency of ALI development for each predisposing condition, at hospital day onset, and at each hospital setting. All statistical analysis was performed in SAS 9.2 (SAS Institute, Cary, NC).
Sensitivity analysis
Sites with retrospective data and extreme frequencies of ALI development were excluded, and a sensitivity analysis of the prospective cohort from the entire ED cohort was performed.
Results and discussion
Results
Characteristic of study subjects
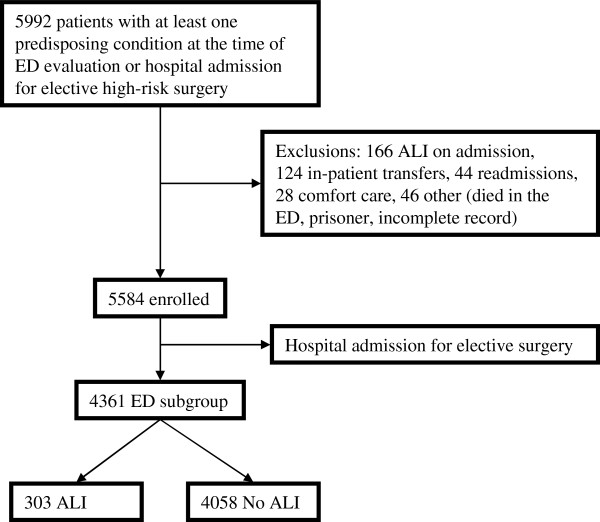
Twenty-two centers screened 5,992, excluded 166 patients with ALI at admission and other criteria, and enrolled 5,584 patients with at least one ALI predisposition, of which 4,361 patients were admitted from the ED (Figure 2).
Figure 2.
Patient enrollment flow diagram.
ALI Developed within 48 H of Admission in At-Risk Patients and Markedly Increased Mortality
ALI developed in 303 (7.0 %) admitted ED patients with a median of 2 days, inter-quartile range (IQR) 2–5 days. Among patients who developed ALI, a subset of 198 (65.3 %) met the ARDS criteria. The follow-up to hospital discharge was complete in all patients. Baseline characteristics, severity of illness, and predisposing conditions and ALI risk modifiers differed between patients who did and those who did not develop ALI (Table 1). Patients who developed ALI were more likely male and heavier, and had a higher APACHE II score. The majority of patients had all measurements available at the time of hospital admission except for serum albumin (n = 2,423) and arterial pH (n = 1,499). As these tests are usually ordered based on clinical suspicion, missing data were considered normal (i.e., if serum albumin or arterial pH was not measured, hypoalbuminemia and acidosis were coded as absent), similarly to APACHE score calculation. The odds ratios for ALI development were highest in risk modifiers of tachypnea and a fraction of inspired oxygen 35 % or greater; and in predisposing conditions of aortic vascular, cardiac, and spinal surgeries, near-drowning, and smoke inhalation. However, the numbers of subjects in some of these categories were small compared to others. The frequency of ALI varied according to predisposing condition with the highest rate occurring after emergent aortic surgery (42.9 %) and the lowest rate occurring in pancreatitis (2.8 %) (Figure 3).
Table 1.
Demographics, predisposing conditions, and risk modifiers in total, no ALI, ALI
| Variable | Total (n = 4361) | No ALI (n = 4058) | ALI (n = 303) | OR (95 % CI) | P-value |
|---|---|---|---|---|---|
|
Demographics |
|
|
|
|
|
| Median age (Q1, Q3) |
56.0 (41.0, 71.0) |
56.0 (41.0, 71.0) |
54.0 (41.0, 67.0) |
0.99 (0.99, 1.00) |
0.050 |
| Male, no. (%) |
2,422 (55.5 %) |
2222 (54.8 %) |
200 (66.0 %) |
1.60 (1.26, 2.05) |
< 0.001 |
| Caucasian (n = 4220), no. (%), |
2608 (61.8 %) |
2424 (61.8 %) |
184 (62.0 %) |
1.01 (0.79, 1.28) |
0.956 |
| Weight (n = 3905), median (Q1, Q3) |
76.5 (63.5, 91.0) |
76.0 (63.5, 91.0) |
83.2 (69.2, 96.0) |
1.84 (1.43, 2.37) |
< 0.001 |
| PBW(n = 3551), median (Q1, Q3) |
63.8 (64.7, 73.0) |
63.8 (54.6, 73.0) |
66.1 (56.4, 75.0) |
1.42 (1.10, 1.84) |
0.007 |
| Admission source (n = 4311), no. (%) |
|
|
|
|
|
| Home |
3,331 (77.3 %) |
3,125 (78.0 %) |
206 (68.2 %) |
1.00 |
|
| Nursing facility |
338 (7.8 %) |
322 (8.0 %) |
16 (5.3 %) |
0.75 (0.45, 1.27) |
0.002 |
| Outside ED |
440 (10.2 %) |
396 (9.9 %) |
44 (14.6 %) |
1.69 (1.20, 2.37) |
0.253 |
| Other |
202 (4.7 %) |
166 (4.1 %) |
36 (11.9 %) |
3.29 (2.23, 4.84) |
< 0.001 |
| APACHE II (Q1, Q3) |
10.0 (6.0, 15.0) |
9.0 (5.0, 14.0) |
15.0 (10.0, 21.0) |
1.11 (1.09, 1.13) |
< 0.001 |
|
Predisposing conditions |
|
|
|
|
|
| Shock |
395 (9.1 %) |
327 (8.1 %) |
68 (22.4 %) |
3.30 (2.46, 4.42) |
< 0.001 |
| Aspiration |
210 (4.8 %) |
176 (4.3 %) |
34 (1.2 %) |
2.79 (1.89, 4.11) |
< 0.001 |
| Sepsis |
1,806 (41.4 %) |
1,684 (41.5 %) |
122 (40.3 %) |
0.95 (0.75, 1.21) |
0.674 |
| Pancreatitis |
323 (7.4 %) |
314 (7.7 %) |
9 (3.0 %) |
0.37 (0.19, 0.72) |
0.003 |
| Pneumonia |
1,227 (28.1 %) |
1,127 (27.8 %) |
100 (33.0 %) |
1.28 (0.99, 1.64) |
0.051 |
| High-risk trauma |
|
|
|
|
|
| Traumatic brain injury |
490 (11.2 %) |
445 (11.0 %) |
45 (14.9 %) |
1.42 (1.02, 1.97) |
0.040 |
| Smoke inhalation |
27 (0.6 %) |
20 (0.5 %) |
7 (2.3 %) |
4.78 (2.00, 11.38) |
< 0.001 |
| Near drowning |
3 (0.1 %) |
2 (0.1 %) |
1 (0.3 %) |
6.72 (0.61, 74.27) |
0.120 |
| Lung contusion |
188 (4.3 %) |
161 (4.0 %) |
27 (8.9 %) |
2.37 (1.55, 3.63) |
< 0.001 |
| Multiple fractures |
330 (7.6 %) |
304 (7.5 %) |
26 (8.6 %) |
1.16 (0.76, 1.76) |
0.489 |
| High-risk surgery |
|
|
|
|
|
| Thoracic (noncardiac) |
5 (0.1 %) |
4 (0.1 %) |
1 (0.3 %) |
3.36 (0.37, 30.12) |
0.280 |
| Orthopedic spine |
17 (0.4 %) |
13 (0.3 %) |
4 (1.3 %) |
4.16 (1.35, 12.85) |
0.013 |
| Acute abdomen |
295 (6.8 %) |
268 (6.6 %) |
27 (8.9 %) |
1.38 (0.91, 2.09) |
0.125 |
| Cardiac surgery |
20 (0.5 %) |
14 (0.3 %) |
6 (2.0 %) |
5.84 (2.23, 15.30) |
< 0.001 |
| Aortic vascular |
14 (0.3 %) |
8 (0.2 %) |
6 (2.0 %) |
10.23 (3.53, 29.68) |
< 0.001 |
| Emergency surgery |
339 (7.7 %) |
282 (7.0 %) |
57 (18.8 %) |
3.10 (2.27, 4.24) |
< 0.001 |
|
Risk modifiers |
|
|
|
|
|
| Alcohol abuse |
421 (9.7 %) |
381 (9.4 %) |
40 (13.2 %) |
1.47 (1.04, 2.08) |
0.031 |
| Obesity (n = 3,508) |
1,020 (29.1 %) |
929 (28.6 %) |
91 (35.0 %) |
1.34 (1.03, 1.75) |
0.029 |
| Chemotherapy |
158 (3.6 %) |
145 (3.6 %) |
13 (4.3 %) |
1.21 (0.68, 2.16) |
0.520 |
| Diabetes mellitus |
1,042 (23.9 %) |
987 (24.3 %) |
55 (18.2 %) |
0.69 (0.51, 0.93) |
0.016 |
| Smoking (n = 4,019) |
|
|
|
|
|
| None |
2,060 (51.3 %) |
1,931 (51.6 %) |
129 (47.1 %) |
1.00 |
-- |
| Former |
888 (22.1 %) |
829 (22.1 %) |
59 (21.5 %) |
1.07 (0.78, 1.47) |
0.644 |
| Active |
1,071 (26.7 %) |
985 (26.3 %) |
86 (31.4 %) |
1.31 (0.98, 1.74) |
0.089 |
| RR (n = 4,137), median (Q1,Q3) |
20.0 (18.0, 24.0) |
20.0 (18.0, 24.0) |
22.0 (18.0, 27.0) |
|
|
| Tachypnea (n = 4,137), no. (%) |
315 (7.6 %) |
269 (6.8 %) |
52 (18.8 %) |
3.18 (2.29, 4.40) |
< 0.001 |
| SpO2 (n = 4,361), median (Q1, Q3) |
97.0 (94.0, 99.0) |
97.0 (94.0, 99.0) |
95.0 (92.0, 98.0) |
|
|
| SpO2 < 95 % (n = 4,361) |
1,203 (27.6 %) |
1,076 (26.5 %) |
127 (41.9 %) |
2.17 (1.56, 3.02) |
< 0.001 |
| FiO2 (n = 4,361), median (Q1, Q3) |
0.2 (0.2, 0.3) |
0.2 (0.2, 0.3) |
0.4 (0.2, 1.0) |
|
|
| FiO2 >0.35 (n = 4,796), no. (%) |
841 (19.3 %) |
688 (17.0 %) |
153 (50.5 %) |
4.92 (3.87, 6.25) |
< 0.001 |
| Albumin (n = 2,423), median (Q1, Q3) |
3.5 (2.9, 4.0) |
3.5 (3.0, 4.0) |
3.2 (2.4, 3.7) |
|
|
| Hypoalbuminemia (n = 2,423), no. (%) |
945 (47.1 %) |
838 (45.6 %) |
107 (64.5 %) |
2.17 (1.56, 3.02) |
< 0.001 |
| pH (n = 1,499), median (Q1, Q3) |
7.4 (7.3, 7.4) |
7.4 (7.3, 7.4) |
7.3 (7.2, 7.4) |
|
|
| Acidosis (pH <7.35), no. (%) | 476 (45.9 %) | 364 (43.3 %) | 112 (56.6 %) | 1.70 (1.25, 2.33) | < 0.001 |
PRW: Predicted body weight; RR: respiratory rate; tachypnea = RR > 30; SpO2: oxygen saturation; FiO2: fraction of inspired oxygen.
Figure 3.
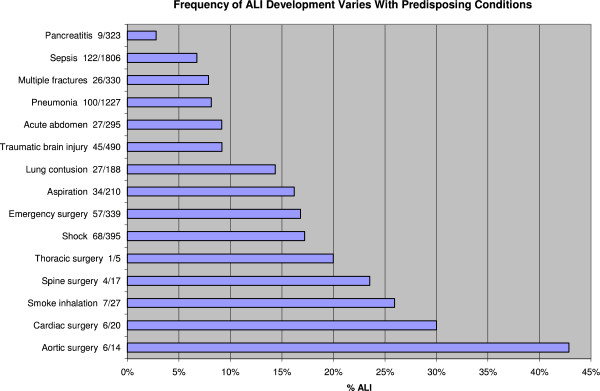
Frequency of ALI Development Varies with Predisposing Condition.
Outcome data for the study cohort are shown in Table 2. More than half of the entire cohort and 91 % of patients who developed ALI were treated in the ICU; and 31 % of the entire cohort and 95 % of patients with ALI were either invasively or non-invasively mechanically ventilated. Compared to at-risk patients who did not develop ALI, those who developed ALI were more likely to be ventilated invasively (88 % vs 19 %) and non-invasively (30 % vs 10 %), respectively. Similarly, comparing to patients who did not develop ALI, those who did had increased resource utilization as reflected in more vasopressor usage (38 % vs 8 %), a higher percentage of acute hemodialysis requirement (11 % vs 3 %), and longer ICU (9 vs 2 days) and hospital (16 vs 5 days) lengths of stays. More importantly, patients who developed ALI had increased ICU (24 % vs 3 %) and hospital (28 % vs 5 %) mortality. When adjusted for severity of illness using the APACHE II score, the development of ALI markedly increased the risk of in-hospital death by more than four-fold [OR 4.45, 95%CI (3.23, 6.14)].
Table 2.
Hospital Course and Outcomes for Total, No ALI, and ALI
| Variable | Total (n = 4,361) | No ALI (n = 4,058) | ALI (n = 303) | OR (95 % CI) | P-value |
|---|---|---|---|---|---|
| ICU admission, no. (%) |
2,320 (53.2 %) |
2,043 (50.3 %) |
277 (91.4 %) |
10.50 (6.99, 15.77) |
< 0.001 |
| ICU LOS (n = 2,320), median (Q1, Q3) |
2.0 (1.0, 5.0) |
2.0 (0.0, 4.0) |
9.0 (5.0, 17.0) |
19.12 (9.79, 37.38) |
< 0.001 |
| Hospital LOS (n = 4361), median (Q1, Q3) |
6.0 (3.0, 10.0) |
5.0 (3.0, 9.0) |
16.0 (9.0, 26.0) |
8.60 (5.94, 12.36) |
< 0.001 |
| Vasopressors use, no. (%) |
448 (10.3 %) |
334 (8.2 %) |
114 (37.6 %) |
6.73 (5.20, 8.71) |
< 0.001 |
| Acute hemodialysis (n = 4,290), no. (%) |
148 (3.5 %) |
115 (2.9 %) |
33 (11.0 %) |
4.15 (2.76, 6.23) |
< 0.001 |
| ICU mortality, no. (%) |
194 (4.5 %) |
120 (3.0 %) |
74 (24.4 %) |
10.61 (7.71, 14.59) |
< 0.001 |
| Hospital mortality, no. (%) |
272 (6.2 %) |
188 (4.6 %) |
84 (27.7 %) |
7.90 (5.90, 10.56) |
< 0.001 |
| Mechanical ventilation (n = 4,223) |
1,299 (30.8 %) |
1,013 (25.8 %) |
286 (94.7 %) |
51.29 (30.85, 85.28) |
< 0.001 |
| Non-invasive (n = 4,146), no. (%) |
470 (11.3 %) |
387 (10.0 %) |
83 (30.1 %) |
3.87 (2.93, 5.11) |
< 0.001 |
| Non-invasive duration (n = 461), median (Q1, Q3) |
2.0 (1.0, 5.0) |
2.0 (1.0, 5.0) |
3.0 (2.0, 5.5) |
1.29 (0.73, 2.25) |
0.379 |
| Invasive (n = 4,228), no. (%) |
997 (23.6 %) |
730 (18.6 %) |
267 (88.4 %) |
33.40 (23.27, 47.94) |
< 0.001 |
| Invasive duration (n = 932), median (Q1, Q3) |
3.0 (1.0, 8.0) |
2.0 (1.0, 5.0) |
8.0 (4.0, 15.0) |
6.53 (4.52, 9.42) |
< 0.001 |
| TV/PBW (n = 768), median (Q1, Q3) |
8.3 (7.4, 9.5) |
8.4 (7.5, 9.7) |
8.1 (7.3, 9.2) |
0.70 (0.51, 0.96) |
0.029 |
| Plateau pressure (n = 435), median (Q1, Q3) |
19.0 (16.0, 24.0) |
19.0 (15.0, 23.0) |
21.0 (17.0, 27.2) |
1.77 (1.17, 2.69) |
0.007 |
| PEEP (n = 916), median (Q1, Q3) |
5.0 (5.0, 5.5) |
5.0 (5.0, 5.0) |
5.0 (5.0, 8.0) |
2.30 (1.32, 4.01) |
0.003 |
| Mode: Volume control |
762 (83.9 %) |
561 (86.4 %) |
201 (77.6 %) |
1.00 |
-- |
| Mode: Pressure control | 111 (12.2 %) | 63 (9.7 %) | 48 (18.5 %) | 2.13 (1.41, 3.20) | 0.010 |
ICU: Intensive care unit; LOS: length of stay; TV: tidal volume; PBW: predicted body weight; PEEP: peak end-expiratory pressure.
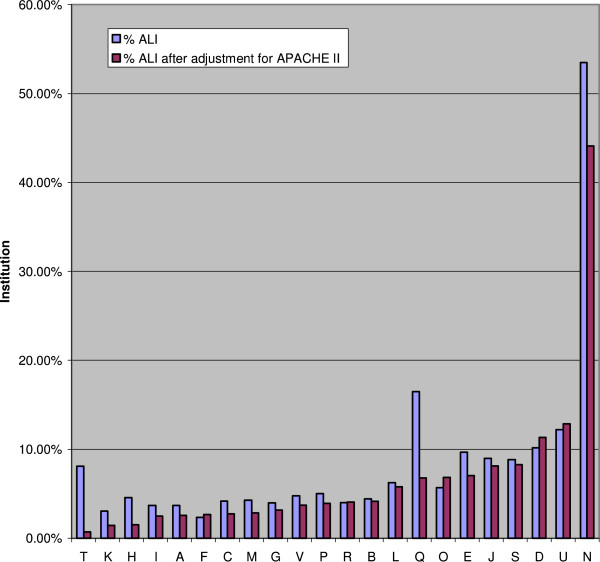
The variation in the frequency of ALI development among the 22 study sites is illustrated in Figure 4. Even after adjustment for each site’s APACHE II score, a significant variation in the frequency of ALI development remained. By excluding the one outlier (44 %), the frequency of ALI development varied from 0.7 to 12.8 %.
Figure 4.
Frequency of ALI Development Varies by Institution.
Since the data set is fairly large, the utilization of invasive mechanical ventilation and onset of ALI development were explored. Figure 5 provides a description of ALI development and initiation of invasive mechanical ventilation by hospital day. The majority of patients who developed ALI and who received invasive mechanical ventilation did so within the first 2 days after hospital admission. As illustrated in Figure 6, the majority of patients who developed ALI had initiation of invasive mechanical ventilation on the day of ALI onset. Unfortunately, no data were recorded regarding the exact timing (in hours and minutes) and the reason for initiation of invasive mechanical ventilation with respect to the onset of ALI development. Although relatively few patients developed ALI prior to initiation of invasive mechanical ventilation, many developed ALI a day or more after initiation of invasive mechanical ventilation.
Figure 5.
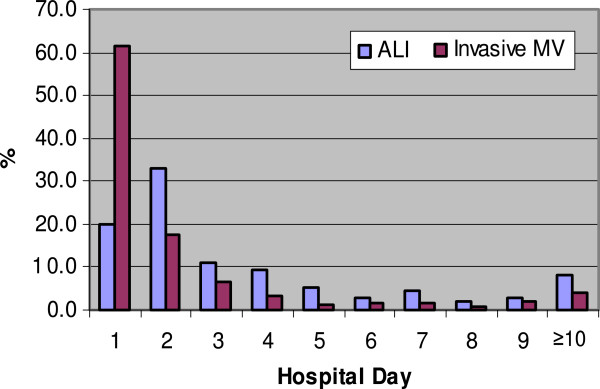
Percentage of ALI Development and Invasive Mechanical Ventilation Onset by Hospital Day.
Figure 6.
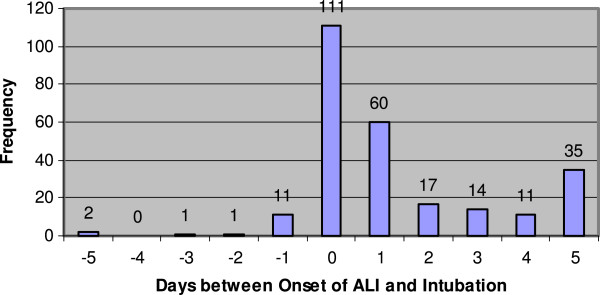
Days between Onset of ALI Development and Invasive Mechanical Ventilation.
Sensitivity analyses
When data from the two non-US study sites were removed (n = 4,233) from the analysis (see Additional file 1: Appendix 3), ALI developed in 266 (6.3 %) patients with a median of 2 days (IQR 2–5 days) after admission to the hospital. The frequency of ALI varied according to predisposing condition with the highest rate of ALI occurring after aortic surgery (36.4 %) and the lowest rate occurring in pancreatitis (2.9 %). Baseline characteristics, severity of illness, predisposing conditions and ALI risk modifiers, and secondary outcomes remained different between patients who did and those who did not develop ALI. However, there were no significant differences in the group characteristics from the US study sites when comparing to the entire cohort.
In addition, when data from the three retrospective US study sites were removed (n = 3,981) from our descriptive analysis (see Additional file 1: Appendix 4), ALI developed in 241 (6.1 %) patients with a median of 2 days (IQR 2–4 days) after admission to the hospital. The frequency of ALI varied according to predisposing condition with the highest rate of ALI occurring after aortic surgery (40 %) and the lowest rate occurring in pancreatitis (2.4 %). Baseline characteristics, severity of illness, predisposing conditions and ALI risk modifiers, and secondary outcomes maintained their differences between patients who did and did not develop ALI. However, there were no significant differences in the group characteristics when comparing the prospective US sites and the entire US cohort.
Effects of initial ventilator settings on the development of ALI
Since there is growing evidence to suggest that a lung protective strategy with low tidal volume ventilation may be protective in at-risk patients, we explored the effect of the initial vent setting on ALI development [24,25]. We evaluated the initial tidal volume divided by predicted body weight (TV/PBW in cc/kg) in 768 patients who underwent invasive mechanical ventilation (Table 2). Comparing those who did not, patients who developed ALI received a significant lower initial TV/PBW [8.1 vs 8.4, OR 0.70 (95 % CI 0.51-0.96), p = 0.029] but had a significantly higher plateau pressure [21 vs 19, OR 1.77 (95 % CI 1.17-2.69), p = 0.007] and peak end-expiratory pressure (PEEP) [OR 2.30 (95 % CI 1.32-4.01), p = 0.003]. Regarding the mode of mechanical ventilation, a significantly higher proportion of patients who developed ALI was initiated on pressure control ventilation [OR 2.13 (95 % CI 1.41-3.2), p = 0.01] and non-invasive ventilation [OR 3.87 (95 % CI 2.93-5.11), p < 0.001] compared to those who did not develop ALI; in contrast, no significant difference was found in those who underwent initial volume control ventilation.
Limitations
Our study carries the limitations of observational cohort studies and those inherent to clinical research with ALI: inter-observer reliability of portable chest X-ray interpretation, ALI imitators, and consistency in determining exclusion of left atrial hypertension as the principal cause of pulmonary edema [26-28]. We instituted a mandatory structured training in ALI assessment and held the site-principal investigators responsible for quality control. These measures were intended to mitigate these limitations.
Regarding the variation in the frequency in ALI development among the study sites, two non-US sites had the highest rate and could be explained by differences in their health-care delivery system, specifically emergency medical care and critical care services, and possibly population and environmental factors. When the data from these two non-US centers were excluded, no significant difference in the frequency of ALI development (p = 0.216) was found between the US sites. In addition, the vast majority of patients were enrolled prospectively ensuring close follow-up and reducing the risk of misclassification from medical record review. When data from those centers enrolling retrospectively were excluded, no significant difference in the frequency of ALI development (p = 0.665) was found comparing the prospective US sites to the entire US cohort. Hence, although a significant variation in the frequency of ALI development across institutions was found, the US sites and the prospectively enrolling US sites were not significantly different when each subgroup was compared to the entire cohort.
Discussion
Even though ALI is classified as a rare disease [29], it is a major public health concern. It is, however, unclear how much if variations in initial management of ALI-prone patients by emergency physicians contribute to its development. To our knowledge, this is the largest detailed study of a cohort of hospitalized adult ED patients at risk for ALI development. The strengths of this study include the large sample size from a geographically diverse population of patients at both academic and community hospitals. Using routinely available clinical data, we identified ED patients at risk for ALI development early in the course of their illness. The early identification of predisposing conditions and risk modifiers as well as subsequent interventions in the ED and ICU may potentially prevent disease development by minimizing or avoiding secondary insults.
Interestingly, in our study we found that ALI developed with lower frequencies than previously reported following conditions recognized to predispose patients at risk for ALI such as: aspiration, pneumonia, sepsis, and trauma [30,31]. This may be explained by the fact that our patients were enrolled early (in the ED) without any signs of ALI (with at least one predisposing factor present) and we excluded those who developed ALI within 6 h of ED presentation, while those other studies enrolled patients upon ICU admission. Consistent with our findings, a recent study by Ferguson et al. showed that 7 % of patients with sepsis, 2 % of patients with pancreatitis, 10 % of patients with pneumonia, and 15 % of patients with witnessed aspiration developed ALI [32]. Similarly, the majority of patients with predisposing conditions never developed ALI, and many were not admitted to the ICU.
Our inclusion criteria required the presence of at least one ALI risk factor at the time of hospital admission, potentially missing the patients who acquire a predisposing condition and received a secondary injury later in the hospital stay. We cannot rule out that a minority of our patients identified as high risk were already progressing to develop full-blown ALI at the time of enrollment, although the exclusion of those who developed ALI within 6 h of ED presentation intended to minimize this possibility. However, we do believe that earlier identification of such patients would also be of benefit, and could help limit the progression of ALI development and improve patient outcomes by alerting providers to make efforts to limit second-hit exposures. To support this notion, a population-based study in Olmsted County, Minnesota, has recently shown a steady decline in ARDS incidence. This was attributable entirely to a reduced incidence of hospital-acquired ARDS and suggests that recent improvements in prevention, early recognition, and critical care delivery may in part be responsible for this [33].
From Olmsted County’s experience, major system changes within the hospital throughout the years were progressively made. These include electronic medical records with computerized order entry to monitor data and institute decision support, restrictive transfusion protocol with leukoreduction and male donor predominant plasma transfusion, respiratory therapy protocol on limiting initial volume according to predicted body weight on all patients, increased staffing of intensivists with 24-h on site, sepsis resuscitation protocols and teams, rapid response teams, standardization of inpatient pneumonia care, and staff education and training. Regarding potential interventions that may affect the development of ALI, a checklist for lung injury prevention (CLIP) has been proposed and developed by experts in the field [34]. The CLIP domains (and elements) consist of routine ICU practices of morbidity prevention and include: respiratory support (lung protective strategies, minimizing oxygen toxicity) [12,24,25]; aspiration precautions (rapid sequence intubation, head-of-bed elevation, oral care with chlorhexidine) [35-37]; infection control (early and appropriate antibiotic therapy, source control, prevention of nosocomial infection transmission) [38]; fluid management (early fluid resuscitation in severe sepsis and septic shock, fluid restriction after shock resolution) [39,40]; transfusion management (restrictive red blood cell transfusion threshold, transfusion guidelines for blood products) [40,41]; and communication (validated structured handoffs such as SBAR: situation, background, assessment, and recommendation) [42]. As a continuum in the care of the critically ill starting in the ED and transitioning to the ICU, all of these domains and many of these proposed elements are being followed to a certain extent, but inconsistently as reflected in our own experiential observations and practice variations. However, such a proposed checklist will require validation for its utility in adherence to best practices and ALI prevention.
Conclusions
Many ED patients who are hospitalized have risk factors for ALI development. In this cohort, we found 7 % of ED patients with at least one predisposing condition developed ALI, and there is variation in the frequency of ALI development across study sites. In addition, more resources are utilized in patients who do develop ALI, and more importantly, ALI significantly increased the patient’s risk of death in the hospital. Hence, is there a role for emergency physicians in the management of patients at risk for ALI development?
Currently, pre-planned ancillary studies are ongoing to explore potential differences in development of ALI at different hospital settings, in different disease-related groups, and their specific treatment modalities. In addition, acute lung injury prevention trials are being proposed. Further research is also warranted to develop a prediction model to identify hospitalized ED patients at risk of ALI development at an early stage in their illness.
Abbreviations
AECC: American-European consensus conference; ALI: acute lung injury; APACHE: acute physiology and chronic health evaluation; ARDS: acute respiratory distress syndrome; CLIP: checklist for lung injury prevention; ED: emergency department; ICU: intensive care units; LIPS: lung injury prediction score; PEEP: positive end expiratory pressure; PBW: predicted body weight; TV: tidal volume; USCIITG-LIPS 1: United States Critical Injury and Illness Trials Group-Lung Injury Prevention Study 1; VALI: ventilator-associated lung injury.
Competing interests
The STAR Center provided internal funding (Dr. Frendl), research staff, and biostatistical support, Brigham and Women’s Hospital, Boston, MA. Dr. Gajic is supported in part by grants from the National Heart, Lung, and Blood Institute HL78743-01A1; National Center for Research Resources 1 KL2 RR024151. Dr. Gentile is supported in part by grants from the National Institute of Neurological Disorders and Stroke 5U10NS059039-04. The rest of the authors have no disclosures or conflict of interest.
Authors' contributions
PCH, MCE, OG, and NTG conceived the study, designed the review, and supervised the conduct of the review and data collection. GF obtained research funding. PCH, AM, and OG extracted and managed the data and performed quality control of the data. AM provided statistical advice on study design, and all authors analyzed the data. PCH drafted the manuscript, and all authors provided significant contributions to its revision. PCH takes responsibility for the paper as whole. All authors read and approved the final manuscript.
Supplementary Material
Contributor Information
Peter C Hou, Email: phou@partners.org.
Marie-Carmelle Elie-Turenne, Email: elie@ufl.edu.
Aya Mitani, Email: aya.a.mitani@gmail.com.
Jonathan M Barry, Email: jon.m.barry@gmail.com.
Erica Y Kao, Email: ericakao@gmail.com.
Jason E Cohen, Email: jcohendo@gmail.com.
Gyorgy Frendl, Email: gfrendl@partners.org.
Ognjen Gajic, Email: gajic.ognjen@mayo.edu.
Nina T Gentile, Email: ngentile@temple.edu.
Acknowledgments
US Critical Illness and Injury Trials Group: Lung Injury Prevention Study Investigators (see Additional file 1: Appendix 5).
References
- Ashbaugh DG Bigelow DB Petty TL Levine BE Acute respiratory distress in adults Lancet 19672319–323.4143721 [Google Scholar]
- Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342:1334–1349. doi: 10.1056/NEJM200005043421806. [DOI] [PubMed] [Google Scholar]
- Wheeler AP, Bernard GR. Acute lung injury and the acute respiratory distress syndrome: a clinical review. Lancet. 2007;369:1553–1564. doi: 10.1016/S0140-6736(07)60604-7. [DOI] [PubMed] [Google Scholar]
- National Heart and Lung Institute. Task force on problems, research approaches, needs: the lung program. Department of Health, Education, and Welfare, Washington, D.C; 1972. pp. 73–432. [Publication no. (NIH) [Google Scholar]
- Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- Phua J, Badia JR, Adhikari NK, Friedrich JO, Fowler RA, Singh JM, Scales DC, Stather DR, Li A, Jones A, Gattas DJ, Hallett D, Tomlinson G, Stewart TE, Ferguson ND. Has mortality from acute respiratory distress syndrome decreased over time?: A systematic review. Am J Respir Crit Care Med. 2009;179:220–227. doi: 10.1164/rccm.200805-722OC. [DOI] [PubMed] [Google Scholar]
- Herridge MS, Tansey CM, Matte A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- Pugin J, Verghese G, Widmer MC, Matthay MA. The alveolar space is the site of intense inflammatory and profibrotic reactions in the early phase of acute respiratory distress syndrome. Crit Care Med. 1999;27:304–312. doi: 10.1097/00003246-199902000-00036. [DOI] [PubMed] [Google Scholar]
- Salzer WL, McCall CE. Primed stimulation of isolated perfused rabbit lung by endotoxin and platelet activating factor induces enhanced production of thromboxane and lung injury. J Clin Invest. 1990;85:1135–1143. doi: 10.1172/JCI114545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silliman CC, Voelkel NF, Allard JD, Elzi DJ, Tuder RM, Johnson JL, Ambruso DR. Plasma and lipids from stored packed red blood cells cause acute lung injury in an animal model. J Clin Invest. 1998;101:1458–1467. doi: 10.1172/JCI1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- Levitt JE, Bedi H, Calfee CS, Gould MK, Matthay MA. Identification of early acute lung injury at initial evaluation in an acute care setting prior to the onset of respiratory failure. Chest. 2009;135:936–943. doi: 10.1378/chest.08-2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur SJ, Trillo-Alvarez CA, Malinchoc MM, Kashyap R, Thakur L, Ahmed A, Reriani MK, Cartin-Ceba R, Sloan JA, Gajic O. Towards the prevention of acute lung injury: a population based cohort study protocol. BMC Emerg Med. 2010;10:8–17. doi: 10.1186/1471-227X-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catchings TT, Beamer WC, Lundy L, Prough DS. Adult respiratory distress syndrome secondary to ethylene glycol ingestion. Ann Emer Med. 1985;14:594–596. doi: 10.1016/S0196-0644(85)80789-7. [DOI] [PubMed] [Google Scholar]
- Van Sickle D, Wenck MA, Belflower A, Drociuk D, Ferdinands J, Holguin F, Svendsen E, Bretous L, Jankelevich S, Gibson JJ, Garbe P, Moolenaar RL. Acute health effects after exposure to chlorine gas released after a train derailment. The Am J Emer Med. 2009;27:1–7. doi: 10.1016/j.ajem.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SQ, Li CS, Song YG. Multiply organ dysfunction syndrome due to tramadol intoxication alone. Am J Emer Med. 2009;27:903. doi: 10.1016/j.ajem.2008.11.013. e5–7. [DOI] [PubMed] [Google Scholar]
- Wu J, Sheng L, Ma Y, Gu J, Zhang M, Gan J, Xu S, Jiang G. The analysis of risk factors of impacting mortality rate in severe multiple trauma patients with posttraumatic acute respiratory distress syndrome. Am J Emer Med. 2008;26:419–424. doi: 10.1016/j.ajem.2007.06.032. [DOI] [PubMed] [Google Scholar]
- Spragg RG, Bernard GR, Checkley W, Curtis JR, Gajic O, Guyatt G, Hall J, Israel E, Jain M, Needham DM, Randolph AG, Rubenfeld GD, Schoenfeld D, Thompson BT, Ware LB, Young D, Harabin AL. Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. pp. 1121–7. [DOI] [PMC free article] [PubMed]
- Cobb JP, Ognibene FP, Ingbar DH, Mann HJ, Hoyt DB, Angus DC, Thomas AV Jr, Danner RL, Suffredini AF. Forging a critical alliance: Addressing the research needs of the United States critical illness and injury community. Crit Care Med. 2009;37:3158–3160. doi: 10.1097/CCM.0b013e3181b03434. [DOI] [PubMed] [Google Scholar]
- Gajic O, Dabbagh O, Park PK, Adesanya A, Chang SY, Hou P, Anderson H 3rd, Hoth JJ, Mikkelsen ME, Gentile NT, Gong MN, Talmor D, Bajwa E, Watkins TR, Festic E, Yilmaz M, Iscimen R, Kaufman DA, Esper AM, Sadikot R, Douglas I, Sevransky J, Malinchoc M. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2010;183:462–470. doi: 10.1164/rccm.201004-0549OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Int Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. doi: 10.1097/00003246-198510000-00009. [DOI] [PubMed] [Google Scholar]
- Determann RM, Royakkers A, Wolthuis EK, Vlaar AP, Choi G, Paulus F, Hofstra JJ, de Graaff MJ, Korevaar JC, Schultz MJ. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care. 2010;14:R1–R31. doi: 10.1186/cc8230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, Rana R, St Sauver JL, Lymp JF, Afessa B, Hubmayr RD. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32:1817–1824. doi: 10.1097/01.CCM.0000133019.52531.30. [DOI] [PubMed] [Google Scholar]
- Aberle DR, Wiener-Kronish JP, Webb WR, Matthay MA. Hydrostatic versus increased permeability pulmonary edema: diagnosis based on radiographic criteria in critically ill patients. Radiology. 1988;168:73–79. doi: 10.1148/radiology.168.1.3380985. [DOI] [PubMed] [Google Scholar]
- Esteban A, Fernandez-Segoviano P, Frutos-Vivar F, Aramburu JA, Najera L, Ferguson ND, Alia I, Gordo F, Rios F. Comparison of clinical criteria for the acute respiratory distress syndrome with autopsy findings. Ann Int Med. 2004;141:440–445. doi: 10.7326/0003-4819-141-6-200409210-00009. [DOI] [PubMed] [Google Scholar]
- Schwarz MI, Albert RK. "Imitators" of the ARDS: implications for diagnosis and treatment. Chest. 2004;125:1530–1535. doi: 10.1378/chest.125.4.1530. [DOI] [PubMed] [Google Scholar]
- National Organization for Rare Disorders. http://www.rarediseases.org/search/rdbdetail_abstract.html?disname=Acute%20Respiratory%20Distress%20Syndrome (Accessed December 20, 2010, at.
- Fowler AA, Hamman RF, Good JT, Benson KN, Baird M, Eberle DJ, Petty TL, Hyers TM. Adult respiratory distress syndrome: risk with common predispositions. Ann Int Med. 1983;98:593–597. doi: 10.7326/0003-4819-98-5-593. [DOI] [PubMed] [Google Scholar]
- Hudson LD, Milberg JA, Anardi D, Maunder RJ. Clinical risks for development of the acute respiratory distress syndrome. Am J Respir Crit Care Med. 1995;151:293–301. doi: 10.1164/ajrccm.151.2.7842182. [DOI] [PubMed] [Google Scholar]
- Ferguson ND, Frutos-Vivar F, Esteban A, Gordo F, Honrubia T, Penuelas O, Algora A, Garcia G, Bustos A, Rodriguez I. Clinical risk conditions for acute lung injury in the intensive care unit and hospital ward: a prospective observational study. Crit Care. 2007;11:R96. doi: 10.1186/cc6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G, Malinchoc M, Cartin-Ceba R, Venkata CV, Kor DJ, Peters SG, Hubmayr RD, Gajic O. Eight-year trend of acute respiratory distress syndrome: a population-based study in Olmsted County, Minnesota. Am J Respir Crit Care Med. 2011;183:59–66. doi: 10.1164/rccm.201003-0436OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Personal communications with Drs. Michelle Gong and Ognjen. Checklist for Lung Injury Prevention – CLIP. https://ephpublic.aecom.yu.edu/clip/default.aspx Accessed May 26, 2011, 2011.
- Li J, Murphy-Lavoie H, Bugas C, Martinez J, Preston C. Complications of emergency intubation with and without paralysis. Am J Emer Med. 1999;17:141–143. doi: 10.1016/S0735-6757(99)90046-3. [DOI] [PubMed] [Google Scholar]
- Drakulovic MB, Torres A, Bauer TT, Nicolas JM, Nogue S, Ferrer M. Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomised trial. Lancet. 1999;354:1851–1858. doi: 10.1016/S0140-6736(98)12251-1. [DOI] [PubMed] [Google Scholar]
- Koeman M, van der Ven AJ, Hak E, Joore HC, Kaasjager K, de Smet AG, Ramsay G, Dormans TP, Aarts LP, de Bel EE, Hustinx WN, van der Tweel I, Hoepelman AM, Bonten MJ. Oral decontamination with chlorhexidine reduces the incidence of ventilator-associated pneumonia. Am J Respir Crit Care Med. 2006;173:1348–1355. doi: 10.1164/rccm.200505-820OC. [DOI] [PubMed] [Google Scholar]
- Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. The New Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, de Boisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- Gong MN, Thompson BT, Williams P, Pothier L, Boyce PD, Christiani DC. Clinical predictors of and mortality in acute respiratory distress syndrome: potential role of red cell transfusion. Crit Care Med. 2005;33:1191–1198. doi: 10.1097/01.CCM.0000165566.82925.14. [DOI] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement. http://www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.html Accessed May 26, 2011.
- Moss M, Bucher B, Moore FA, Moore EE, Parsons PE. The role of chronic alcohol abuse in the development of acute respiratory distress syndrome in adults. Journal of the American Medical Association. 1996;50:54. [PubMed] [Google Scholar]
- Selzer ML. The Michigan alcoholism screening test: the quest for a new diagnostic instrument. Am J Psychiatry. 1971;127(12):1653–8. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR. et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR. et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Hunt SA. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) J Am Coll Cardiol. 2005;46(6):e1–82. doi: 10.1016/j.jacc.2005.08.022. [DOI] [PubMed] [Google Scholar]
- Diagnosis and classification of diabetes mellitus. Diabetes Care. 2007;30(Suppl 1):S42–S47. doi: 10.2337/dc07-S042. [DOI] [PubMed] [Google Scholar]
- Pauwels RA, Buist AS, Ma P, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: National Heart, Lung, and Blood Institute and World Health Organization Global Initiative for Chronic Obstructive Lung Disease (GOLD): executive summary. Respir Care. 2001;46(8):798–825. [PubMed] [Google Scholar]
- Expert Panel Report 3 (EPR-3) Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002;165(2):277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- Sonnenberg A, Everhart JE. Health impact of peptic ulcer in the United States. Am J Gastroenterol. 1997;92(4):614–20. [PubMed] [Google Scholar]
- Anthony PP, Ishak KG, Nayak NC, Poulsen HE, Scheuer PJ, Sobin LH. The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health Organization. J Clin Pathol. 1978;31(5):395–414. doi: 10.1136/jcp.31.5.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- K/DOQI clinical practice guidelines for chronic kidney disease. evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- Levey AS, Eckardt KU, Tsukamoto Y. et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2005;67(6):2089–100. doi: 10.1111/j.1523-1755.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36(3):959–69. doi: 10.1016/S0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50(22):2173–95. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- Hirsch AT, Haskal ZJ, Hertzer NR. et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239–312. doi: 10.1016/j.jacc.2005.10.009. [DOI] [PubMed] [Google Scholar]
- Adams HP Jr, del Zoppo G, Alberts MJ. et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478–534. doi: 10.1161/CIRCULATIONAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- Knopman DS, DeKosky ST, Cummings JL. et al. Practice parameter: diagnosis of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56(9):1143–53. doi: 10.1212/WNL.56.9.1143. [DOI] [PubMed] [Google Scholar]
- Karon JM, Buehler JW, Byers RH. et al. Projections of the number of persons diagnosed with AIDS and the number of immunosuppressed HIV-infected persons--United States, 1992–1994. MMWR Recomm Rep. 1992;41(RR-18):1–29. [PubMed] [Google Scholar]
- Steinman TI, Becker BN, Frost AE. et al. Guidelines for the referral and management of patients eligible for solid organ transplantation. Transplantation. 2001;71(9):1189–204. doi: 10.1097/00007890-200105150-00001. [DOI] [PubMed] [Google Scholar]
- Knaus WA, Wagner DP, Draper EA. et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–36. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- Calandra T, Cohen J. The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med. 2005;33(7):1538–48. doi: 10.1097/01.CCM.0000168253.91200.83. [DOI] [PubMed] [Google Scholar]
- American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20(6):864–74. doi: 10.1097/00003246-199206000-00025. [DOI] [PubMed] [Google Scholar]
- Antonelli M, Levy M, Andrews PJ. et al. Hemodynamic monitoring in shock and implications for management. International Consensus Conference, Paris, France, 27–28 April 2006. Intensive Care Med. 2007;33(4):575–90. doi: 10.1007/s00134-007-0531-4. [DOI] [PubMed] [Google Scholar]
- Rivers E, Nguyen B, Havstad S. et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- Gutierrez G, Reines HD, Wulf-Gutierrez ME. Clinical review: hemorrhagic shock. Crit Care. 2004;8(5):373–81. doi: 10.1186/cc2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollenberg SM, Kavinsky CJ, Parrillo JE. Cardiogenic shock. Ann Intern Med. 1999;131(1):47–59. doi: 10.7326/0003-4819-131-1-199907060-00010. [DOI] [PubMed] [Google Scholar]
- Hochman JS, Boland J, Sleeper LA. et al. Current spectrum of cardiogenic shock and effect of early revascularization on mortality. Results of an International Registry. SHOCK Registry Investigators Circulation. 1995;91(3):873–81. doi: 10.1161/01.cir.91.3.873. [DOI] [PubMed] [Google Scholar]
- Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665–71. doi: 10.1056/NEJM200103013440908. [DOI] [PubMed] [Google Scholar]
- Banks PA. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 1997;92(3):377–86. [PubMed] [Google Scholar]
- Sachdeva RC. Near drowning. Crit Care Clin. 1999;15(2):281–96. doi: 10.1016/S0749-0704(05)70055-5. [DOI] [PubMed] [Google Scholar]
- Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–88. doi: 10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- Voelkel NF. High-altitude pulmonary edema. N Engl J Med. 2002;346(21):1606–7. doi: 10.1056/NEJM200205233462102. [DOI] [PubMed] [Google Scholar]
- Derdak S. Acute respiratory distress syndrome in trauma patients. J Trauma. 2007;62(6 Suppl):S58. doi: 10.1097/TA.0b013e318065ab4e. [DOI] [PubMed] [Google Scholar]
- Arozullah AM, Khuri SF, Henderson WG, Daley J. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med. 2001;135(10):847–57. doi: 10.7326/0003-4819-135-10-200111200-00005. [DOI] [PubMed] [Google Scholar]
- Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg. 2000;232(2):242–53. doi: 10.1097/00000658-200008000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today's critically ill patients. Crit Care Med. 2006;34(5):1297–310. doi: 10.1097/01.CCM.0000215112.84523.F0. [DOI] [PubMed] [Google Scholar]
- Rubenfeld GD, Angus DC, Pinsky MR, Curtis JR, Connors AF Jr, Bernard GR. Outcomes research in critical care: results of the American Thoracic Society Critical Care Assembly Workshop on Outcomes Research. The Members of the Outcomes Research Workshop. Am J Respir Crit Care Med. 1999;160(1):358–67. doi: 10.1164/ajrccm.160.1.9807118. [DOI] [PubMed] [Google Scholar]
- Kleinman S, Caulfield T, Chan P. et al. Toward an understanding of transfusion-related acute lung injury: statement of a consensus panel. Transfusion. 2004;44(12):1774–89. doi: 10.1111/j.0041-1132.2004.04347.x. [DOI] [PubMed] [Google Scholar]
- Toy P, Popovsky MA, Abraham E. et al. Transfusion-related acute lung injury: definition and review. Crit Care Med. 2005;33(4):721–6. doi: 10.1097/01.CCM.0000159849.94750.51. [DOI] [PubMed] [Google Scholar]
- McGregor JC, Rich SE, Harris AD. et al. A systematic review of the methods used to assess the association between appropriate antibiotic therapy and mortality in bacteremic patients. Clin Infect Dis. 2007;45(3):329–37. doi: 10.1086/519283. [DOI] [PubMed] [Google Scholar]
- Kumar A, Roberts D, Wood KE. et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–96. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- Dellinger RP, Carlet JM, Masur H. et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32(3):858–73. doi: 10.1097/01.CCM.0000117317.18092.E4. [DOI] [PubMed] [Google Scholar]
- Jimenez MF, Marshall JC. Source control in the management of sepsis. Intensive Care Med. 2001;27(Suppl 1):S49–62. doi: 10.1007/pl00003797. [DOI] [PubMed] [Google Scholar]
- Esteban A, Anzueto A, Frutos F. et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345–55. doi: 10.1001/jama.287.3.345. [DOI] [PubMed] [Google Scholar]
- Vincent JL, Akca S, De Mendonca A. et al. The epidemiology of acute respiratory failure in critically ill patients(*) Chest. 2002;121(5):1602–9. doi: 10.1378/chest.121.5.1602. [DOI] [PubMed] [Google Scholar]
- Vincent JL, Moreno R, Takala J. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Sessler CN, Gosnell MS, Grap MJ. et al. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. American Journal of Respiratory and Critical Care Medicine. 2002;166(10):1338–44. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- Ely EW, Inouye SK, Bernard GR. et al. Delirium in mechanically ventilated patients: Validity and reliability of the Confusion Assessment Method for the intensive care unit (CAM-ICU) Journal of the American Medical Association. 2001;286(21):2703–10. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware LB. Comparison of the SpO2/FiO2 Ratio and the PaO2/FiO2 Ratio in Patients with Acute Lung Injury or Acute Respiratory Distress Syndrome. Chest. 2007. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.