Abstract
Background/aims
This paper will compare the visual outcomes of two different penetrating keratoplasty (PKP) techniques in patients with keratoconus. It is a retrospective comparative surgical case series of 116 keratoconus patients (137 eyes) who had PKP at the Cornea Eye Institute, Beverly Hills, California, USA.
Methods
56 keratoconus patients (66 eyes) underwent femtosecond laser-enabled keratoplasty (FLEK) with a zig-zag incision configuration. Their visual parameters were compared with those of 60 patients (71 eyes) who had traditional blade mechanical trephination PKP. The range of follow-up was between 3 and 6 months. The main outcome measures included uncorrected visual acuity and best spectacle-corrected visual acuity (BSCVA), manifest refractive spherical equivalent and topographically determined astigmatism.
Results
BSCVA was significantly better as early as 3 months postoperatively (p=0.001) in the FLEK group. Visual recovery to 20/40 after 3 months was significantly better in the FLEK group (p<0.001). Topographic astigmatism was lower in the FLEK group, but the difference between the two groups reached significance only at 3 months of follow-up (p=0.001). Postoperative complications noted were not different between the two groups.
Conclusions
Faster visual recovery and better long-term outcomes were observed in keratoconus patients who had FLEK compared with those who had the mechanical PKP procedure with 6 months of postoperative follow-up.
INTRODUCTION
The femtosecond laser is gaining rapid and widespread acceptance for use in corneal surgery. In penetrating keratoplasty (PKP), initial laboratory models demonstrated superior mechanical stability after laser keratoplasty compared with manual keratoplasty,1 and the first human full-thickness corneal transplant using femtosecond laser was performed in 2005.2 Preliminary results on the applicability of laser-enabled keratoplasty in different corneal disorders have been reported on a relatively small number of patients and with-limited follow-up. These reports demonstrate a biomechanically stable wound, excellent wound apposition, faster suture removal and faster recovery of best spectacle-corrected visual acuity (BSCVA), accompanied by moderate astigmatism.2–5
In 2007, 50 122 PubMed corneal transplants were performed in the USA (statistics provided by Eye Bank of America). PKP is the standard treatment in advanced keratoconus wlth 12–20% of patients eventually requiring PKP at a relatively young age.6 As femtosecond laser-enabled keratoplasty (FLEK) has been reported as a safe and stable procedure,4 specifically in this group of young patients, earlier visual rehabilitation and decreased short and long-term complication rates would greatly benefit them.
This study presents visual outcomes with up to 6 months of follow-up after femtosecond laser-enabled zig-zag-shaped keratoplasty in keratoconus patients and compares the outcomes with the mechanical trephine keratoplasty (PKP) technique in a similar cohort.
METHODS
Patient selection
This is a retrospective chart review study. The ethics committee of the Eye Surgery Center of Beverly Hills approved this research. Our research adheres to the tenets of the Declaration of Helsinki.
We analysed visual outcomes at 3 and 6 months of 116 keratoconus patients (137 eyes) who had corneal transplants at the Cornea Eye Institute, Beverly Hills, California, USA. All procedures were performed by the same surgeon (YSR) using the same surgical technique.
Fifty-six keratoconus patients (66 eyes) had FLEK, while 60 keratoconus patients (71 eyes) had traditional PKP. All conventional PKP surgeries were performed consecutively before acquiring the femtosecond laser. All FLEK surgeries were performed consecutively after the femtosecond laser was obtained. There were no selection criteria other than the need for corneal transplant surgery.
All patients received a complete ophthalmological examination preoperatively and postoperatively at 1 month, 3 months and 6 months. All patients were diagnosed with advanced keratoconus preoperatively and were either contact lens intolerant or had a central corneal scar, with PKP as the only therapeutic option for adequate visual rehabilitation. Deep anterior lamellar keratoplasty patients were not included in this study. Suture removal was started at 3 months in both groups and was complete by 6 months in the FLEK group and later in the PKP group. The parameters collected for comparative analysis were: uncorrected visual acuity, BSCVA, manifest refractive spherical equivalent and topographically determined astigmatism. Videokeratography was performed on all patients with the topographic modelling system (TMS 4; Tomey, Japan) using a saggital algorithm and the absolute scale.
Surgical techniques
All patients reviewed and signed the informed consent for PKP.
FLEK technique
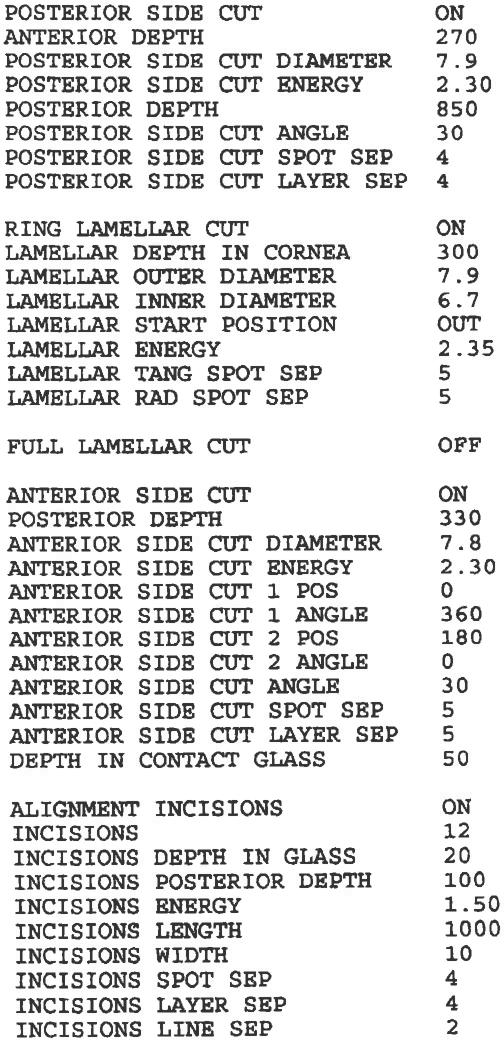
Patients received 10 cc of marcaine and lidocaine as a combination of retrobulbar and peribulbar anaesthesia. The centre of the cornea was marked with a marking pen before the procedure. The zig-zag FLEK pattern was designed on the IntraLase laser (Abbott Medical Optics, Irvine, California, USA) with a 7.9 mm outer diameter and 6.7 mm inner diameter. It was set at a depth of 800 μm to ensure that there was complete perforation of the incision. This is safe in our setting because we have an operating room with a door leading directly to the IntraLase, decreasing the time from laser trephination to removal of the host button to less than 10 min. The rest of the parameters are outlined in figure 1. A same-size donor with the same zig-zag parameters was pre-ordered from the eye bank before the surgery. This allowed for the best postoperative fit donor into recipient. After completion of the host cut, the patient was wheeled through the door from the femtosecond laser to the operating room and the eye was prepped and draped in the usual sterile fashion for intraocular surgery. After a speculum was put in the eye, the wound was opened with a Sinskey hook superiorly and the button was removed entirely with a 0.12 forceps. The pupil was constricted with miochol, and healon was put into the anterior chamber to protect the lens. The donor cornea was then sutured onto the host with 12 interrupted 10-0 nylon sutures on the radial marks made by the IntraLase. This was followed by a running suture in between the interrupted sutures at approximately 50% corneal depth. The running suture was buried within the wound and the knot cut and trimmed. The viscoelastic was irrigated out of the anterior chamber. The patient was given subconjunctival decadron and vancomycin. Erythromycin ointment was put in the eye and a patch and shield were placed on the eye.
Figure 1.
Femtosecond laser parameters used for corneal transplant.
Traditional mechanical (PKP) technique
The PKP technique was identical to the FLEK technique except that a Barron Hessburg 7.5 mm trephine was used to remove the diseased button and a 7.5 mm Katena manual trephine was used to fashion the donor cornea.
Suture removal and measurement of topographic astigmatism
In both groups suture removal was started at 3 months. All sutures were out by 6 months in the FLEK group and later in the PKP group. Sutures were removed when they became loose or when the corneal wound appeared well healed.
Statistical analyses
This was performed with SAS V.9.0. For quantitative traits, comparisons between two groups were tested by the Student's t test when variables had a normal distribution or by the nonparametric Wilcoxon rank test when traits deviated from normal distribution. The χ2 test was used to compare proportions of qualitative traits between groups. As baseline measures were highly correlated with outcome measures during each technique, we also conducted a linear regression model to compare two groups by incorporated baseline values of each trait, as well as age and gender, as covariates.
p Values less than 0.05 were considered statistically significant.
RESULTS
We included 56 keratoconus patients (66 eyes) who underwent FLEK surgery and 60 patients (71 eyes) with PKP surgery in the analysis. All eyes in the two groups were followed at 3 months and most of them were followed at 6 months (54 vs 71).
There were more men in the FLEK group than in the PKP group (74.2% vs 56.3%, p=0.03). No statistically significant difference of age was identified between the two groups (FLEK group: 38.7 years (range 17–75); PKP group: 44.5 years (range 13–80); p=0.07).
There were no significant differences for most ocular parameters, except for BSCVA at baseline between the two groups (table 1).
Table 1.
Baseline characteristics of the two groups of patients
| Variable | FLEK (n=66) | PKP (n=71) | p Value |
|---|---|---|---|
| Logmar UCVA (SD) | 1.44 (0.57) | 1.51 (0.66) | 0.76 |
| Logmar BSCVA (SD) | 0.77 (0.52) | 1.11 (0.69) | 0.002 |
| MRSE (SD) | –7.67 (3.84) | –6.70 (4.47) | 0.38 |
| TA (SD) | 5.94 (3.77) | 6.39 (3.59) | 0.43 |
BSCVA, best spectacle-corrected visual acuity; FLEK, femtosecond laser-enabled keratoplasty; PKP, penetrating keratoplasty; TA, topographically determined astigmatism; UCVA, uncorrected visual acuity.
Three months after corneal transplantation was performed, BSCVA and topographic astigmatism were significantly better in the FLEK group compared with the PKP group of patients (table 2). BSCVA of 20/40 or greater at 3 months was obtained in 28 cases (42.42%) in the FLEK group compared with 9.7% of cases in the PKP group (p<0.001).
Table 2.
Visual outcomes at 3 and 6-month time intervals after treatment
| FLEK (n=66) | PKP (n=71) | p Value | |
|---|---|---|---|
| 3 Months | |||
| Logmar UCVA (SD) | 0.91 (0.55) | 0.94 (0.37) | 0.42 |
| Logmar BSCVA (SD) | 0.46 (0.40) | 0.69 (0.38) | 0.001 |
| MRSE (SD) | –2.79 (5.66) | –0.64 (5.66) | 0.05 |
| TA (SD) | 5.09 (3.55) | 7.33 (4.61) | 0.001 |
| FLEK (n = 54) | PKP (n=71) | p Value | |
|---|---|---|---|
| 6 Months | |||
| LogMar UCVA (SD) | 0.91 (0.69) | 1.00 (0.70) | 0.35 |
| LogMar BSCVA (SD) | 0.44 (0.49) | 0.57 (0.58) | 0.12 |
| MRSE (SD) | –3.76 (4.63) | –3.31 (5.51) | 0.52 |
| TA (SD) | 4.76 (3.41) | 5.91 (4.53) | 0.15 |
BSCVA, best spectacle-corrected visual acuity; FLEK, femtosecond laser-enabled keratoplasty; PKP, penetrating keratoplasty; TA, topographically determined astigmatism; UCVA, uncorrected visual acuity.
At the 6-month follow-up time point, the FLEK group showed better values for all the parameters studied, but the difference between the groups did not reach statistical significance (table 2).
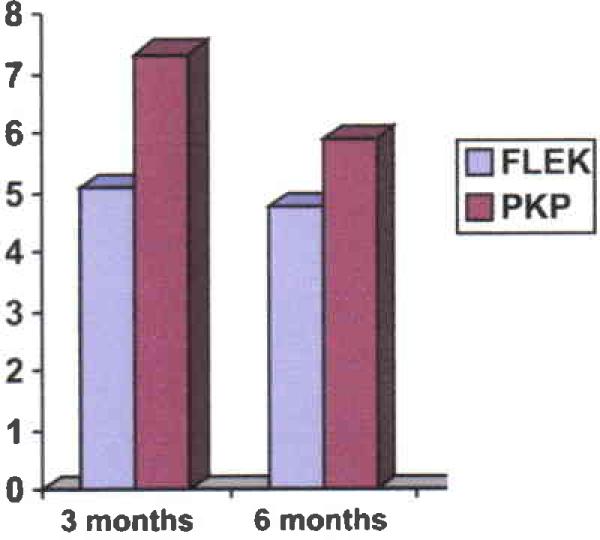
Topographic astigmatism values improved in a time-dependent fashion; although they were lower in the FLEK group at each follow-up time point, they were statistically lower only at 3 months of follow-up (figure 2).
Figure 2.
Time dynamic of topographically determined astigmatism (dioptres) (p=0.001). FLEK, femtosecond laser-enabled keratoplasty; PKP, penetrating kemtoplasty.
Although there were continuous improvements of the manifest refractive spherical equivalent during the follow-up in the FLEK group (table 2), no statistically significant differences were identified between the two groups after adiusting for baseline values (all p>0.05).
All procedures were performed without intraoperative complications. Postoperative complications noted were not different between the two groups. We had one case (1.51%) of graft failure after FLEK and two cases (2.81%) after PKP. Intraocular hypertension or glaucoma was observed in 6.04% of cases after FLEK vercus 4.22% after PKP (p=0.7). No cases of wound dehiscence were seen after suture removal and no cases of postoperative graft rejection.
DISCUSSION
Different laser types and different procedure shapes are available for keratoplasty incisions. Three lasers are approved by the US Food and Drug Administration for corneal cuts: IntraLase (IntraLase Corp., division of Abbott Medical Optics); Femtec (20/10 Perfect Vision; GmbH, Heidelberg, Germany) and FemtoLDV (Ziemer Ophthalmic Systems AG, Port, Switzerland).7,8 Different shapes with different indications have been proposed, some of which include: top hat, mushroom, zig-zag, Christmas tree, zig-squared, tongue and groove.3,9
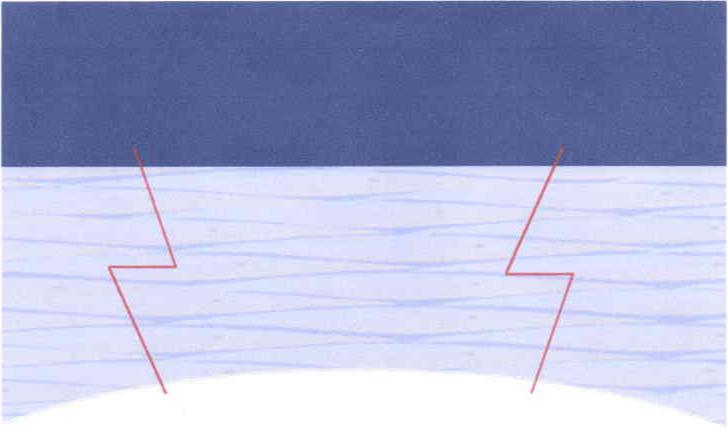
We chose the zig-zag technique (figure 3) for keratoconus patients because the angled incisions from zig-zag-shaped keratoplasty had been described as being more biomechanically favourable, optical coherence tomography images showing excellent alignment of the anterior and posterior layers of the transplant, smooth transition along the anterior surface and excellent host–graft alignment.3
Figure 3.
Diagram of femtosecond laser-enabled keratoplasty zig-zag incision.
In a previously reported study with other corneal disorders, the femtosecond laser-generated zig-zag-shaped incisions resulted in a more rapid recovery of BSCVA and induced less astigmatism compared with conventional blade trephination PKP.10 These data together with the reduced procedure time1 influenced us to make this our procedure of choice. Similar studies have reported results on a small number of keratoconus patients2,10,11 and demonstrated faster recovery of BSCVA and less induced astigmatism at 3 months, but they did not report on visual outcomes at a later time point or make comparison with the mechanical techniques.
Farid et al10 reported on 49 eyes of 43 patients who underwent zig-zag FLEK versus 17 eyes of 14 patients who underwent conventional PKP. All PKP were closed with an identical 24-bite running nylon suture technique. The postoperative follow-up ranged from 1 to 12 months. There was a significant difference in average astigmatism between the groups at postoperative months 1 (p=0.013) and 3 (p=0.018). By month 3, the average astigmatism was 3 dioptres (D) in the FLEK zig-zag group and 4.46 D in the conventional group. Of the patients with normal macular and optic nerve function, a significant difference in BSCVA was seen at month 1 (p=0.0003) and month 3 (p=0.006), with 81% of the FLEK zig-zag group versus 45% of the conventional group achieving BSCVA of 20/40 or greater by month 3 (p=0.03). They concluded that the FLEK zig-zag-shaped incision results in a more rapid recovery of BSCVA and induces less astigmatism compared with conventional PKP.
Bahar et al4 compared 23 eyes that had top-hat FLEK with 35 eyes that had conventional PKP At 12 months postoperatively, the mean cylinder was similar between the two groups: 3.6 D (SD 1.9) in the FLEK group and 4.1 D (SD 1.8) in the PKP group. The mean endothelial cell loss was significantly lower at 12 months in the FLEK group compared with the PKP group (32.4% vs 40.8%). The mean time to suture removal was 4.1 months (SD 1.2) in the FLEK group versus 9.7 months (SD 1.1) in the traditional PKP group.
Huer et al12 analysed eight eyes that underwent FLEK and concluded that long-term control of postoperative astigmatism remains an issue after FLEK, and that suture technique still plays an important role in postoperative astigmatism magnitude. Chamberlain et al13 compared postoperative outcomes in zig-zag FLEK with conventional PKP with 2years of postoperative follow-up. The authors found a significant improvement in astigmatism before but not after the 6-month postoperative follow-up period. However, they did not find significant visual improvement of BSCVA in the FLEK group compared with the conventional PKP group.
Our results on a larger number of keratoconus patients showed a significant improvement of BSCVA and astigmatism early on. Faster visual recovery to the level of being able to obtain a driver's licence and allowing patients to return to functional work earlier represents a great benefit, especially in this young group of patients who are in the most productive period of their lives.
Despite the fact that there was no statistically significant difference between the FLEK and the PKP groups in terms of topographically induced astigmatism at 6 months, the FLEK procedure has become our procedure of choice. There are several reasons for this: (1) visual acuity is better at both postoperative time intervals (3 and 6 months) in our study, which is critical in a young group of patients who are in their actively productive phase of life; (2) the procedure produces a stronger and more stable wound because of its larger surface area, making the eye less prone to corneal rupture; (3) the procedure is much faster with the eye being open for a very short period of time, when the laser is in or very near the operating room, making this a much safer procedure and significantly reducing the chance of intra-operative complications. An added benefit, as suggested by the study by Bahar et al,4 is that there is less endothelial cell loss in the FLEK group versus the PKP group, suggesting that the grafts may survive longer in this group of patients.
Even though PKP has been the standard treatment for advanced keratoconus, the incidence of cases with keratoconus that need a PKP has reduced in recent years due to alternative treatments, such as corneal cross-linking, and a major trend to deep anterior lamellar keratoplasty, in order to preserve the patient's own endothelium.
Future research with different pattern types geared to improving donor–host alignment might also ultimately allow us to achieve our goal of an astigmatism-free or at least significantly reduced astigmatic result in the FLEK procedure.
CONCLUSION
Faster visual rehabilitation and better long-term visual acuity, earlier suture removal, a biomechanically stronger corneal wound, safety, rapidity of the procedure and less endothelial cell loss, make FLEK our procedure of choice in patients with advanced keratoconus whose only option is a corneal transplant. One of the limits of this paper is the retrospective nature of the study. A future randomised, prospective clinical trial will be able to clarify further the true benefits of the FLEK procedure over conventional PKP.
Acknowledgments
Funding This work was supported by Eye Defects Research Foundation grant 005.
Footnotes
Contributors All authors contributed to the writing, editing and data collection for this paper.
Competing interests None.
Ethics approval Ethics approval was provided by the ethics committee of the Eye Surgery Center of Beverly Hills.
Patient consent Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
REFEBENCES
- 1.Steinert RF, Ignacio TS, Sarayba MA. “Top hat”-shaped penetrating keratoplasty using the femtosecond laser. Am J 0phthalmol. 2007;143:689–91. doi: 10.1016/j.ajo.2006.11.043. [DOI] [PubMed] [Google Scholar]
- 2.Slade SG. Applications for the femtosecond laser ln corneal surgery. Curr 0pin Ophthalmol. 2007;18:338–41. doi: 10.1097/ICU.0b013e3281bd88b2. [DOI] [PubMed] [Google Scholar]
- 3.Steinert RF. Femtosecond laser enabled keratoplasty (FLEK). Ann 0phthalmol (Skokie) 2009;41:6–9. [PubMed] [Google Scholar]
- 4.Bahar I, Kaiserman I, Lange A, et al. Femtosecond laser versus manual dissection for top hat penetrating keratoplasty. Br J 0phthalmol. 2009;93:73–8. doi: 10.1136/bjo.2008.148346. [DOI] [PubMed] [Google Scholar]
- 5.Farid M, Kim M, Steinert RF. Results of penetrating keratoplasty performed with a femtosecond laser zigzag incision: initial report. Ophthalmology. 2007;114:2208–12. doi: 10.1016/j.ophtha.2007.08.048. [DOI] [PubMed] [Google Scholar]
- 6.Pramanik S, Musch DC, Sutphin JE, et al. Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology. 2006;113:1633–8. doi: 10.1016/j.ophtha.2006.02.058. [DOI] [PubMed] [Google Scholar]
- 7.Holzer MP, Rabsilber TM, Auffarth GU. Penetrating kentoplasty using femtosecond laser. Am J Ophthalmol. 2007;143:524–6. doi: 10.1016/j.ajo.2006.08.029. [DOI] [PubMed] [Google Scholar]
- 8.Por YM, Cheng JY, Parthasarathy A, et al. Outcomes of femtosecond laser-assisted penetrating keratoplasty. Am J Ophthalmol. 2008;145:772–4. doi: 10.1016/j.ajo.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Price FW, Jr, Price MO. Femtosecond laser shaped penetrating keratoplasty: One-year results utilizing a top-hat configuration. Am J 0phthalmol. 2008;145:210–14. doi: 10.1016/j.ajo.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 10.Farid M, Steinert RF, Gaster RN, et al. Comparison of penetrating keratoplasty performed with a femtosecond laser zig-zag incision versus conventional blade trephination. Ophthalmology. 2009;116:1638–43. doi: 10.1016/j.ophtha.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Burrato L, Böhm E. The use of the femtosecond laser in penetrating keratoplasty. Am J 0phthalmol. 2007;143:137–42. doi: 10.1016/j.ajo.2007.01.056. [DOI] [PubMed] [Google Scholar]
- 12.Heur M, Tang M, Yiu S, et al. Investigation of femtosecond laser-enabled keratoplasty wound geometry using optical coherence tomography. Cornea. 2011;30:889–94. doi: 10.1097/ICO.0b013e3182041fd3. [DOI] [PubMed] [Google Scholar]
- 13.Chamberlain WD, Rush SW, Mathers WD, et al. Comparison of femtosecond laser-assisted keratoplasty versus conventional penetrating keratoplasty. Ophthalmology. 2011;118:486–91. doi: 10.1016/j.ophtha.2010.08.002. [DOI] [PubMed] [Google Scholar]