ABSTRACT
BACKGROUND
An increasing number of patients are visiting retail clinics for simple acute conditions. Physicians worry that visits to retail clinics will interfere with primary care relationships. No prior study has evaluated the impact of retail clinics on receipt of primary care.
OBJECTIVE
To assess the association between retail clinic use and receipt of key primary care functions.
DESIGN
We performed a retrospective cohort analysis using commercial insurance claims from 2007 to 2009.
PATIENTS
We identified patients who had a visit for a simple acute condition in 2008, the “index visit”. We divided these 127,358 patients into two cohorts according to the location of that index visit: primary care provider (PCP) versus retail clinic.
MAIN MEASURES
We evaluated three functions of primary care: (1) where patients first sought care for subsequent simple acute conditions; (2) continuity of care using the Bice–Boxerman index; and (3) preventive care and diabetes management. Using a difference-in-differences approach, we compared care received in the 365 days following the index visit to care received in the 365 days prior, using propensity score weights to account for selection bias.
KEY RESULTS
Visiting a retail clinic instead of a PCP for the index visit was associated with a 27.7 visits per 100 patients differential reduction (p < 0 .001) in subsequent PCP visits for new simple acute conditions. Visiting a retail clinic instead of a PCP was also associated with decreased subsequent continuity of care (10.9 percentage-point differential reduction in Bice–Boxerman index, p < 0 .001). There was no differential change between the cohorts in receipt of preventive care or diabetes management.
CONCLUSIONS
Retail clinics may disrupt two aspects of primary care: whether patients go to a PCP first for new conditions and continuity of care. However, they do not negatively impact preventive care or diabetes management.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-012-2243-x) contains supplementary material, which is available to authorized users.
KEY WORDS: primary health care, continuity of patient care, acute diseases, health services accessibility
INTRODUCTION
Retail clinics are clinics located within retail stores, such as pharmacies or grocery stores, that provide walk-in care for simple acute and preventive concerns. By July 2012, 1,351 retail clinics were operating, a number projected to grow in future years.1,2 Among commercially insured patients, retail clinic visits increased ten-fold between 2007 and 2009.3
Physicians’ organizations are concerned that retail clinics negatively impact relationships between patients and primary care physicians (PCPs); each retail clinic visit could represent one fewer visit to a PCP, one fewer opportunity to build a primary care relationship. Primary care serves four principal functions: (1) first-contact access for new health needs, (2) long-term person-focused care (continuity), (3) comprehensive care for prevention and chronic disease needs, and (4) coordination of care.4 When patients receive these from a usual source of care, they have greater satisfaction, superior outcomes, and lower utilization and costs.5–12
Unlike PCPs, retail clinics provide just one primary care function: first-contact care. Some physicians and policymakers worry that by displacing PCP visits, retail clinics could harm continuity and preventive and chronic care.13,14 However, most retail clinic patients lack a usual source of care, and have no primary care relationship to disrupt.15,16 In one study limited to Minnesota, patients who visited a retail clinic were as likely to receive a limited set of preventive services as those who visited a PCP.17 Despite this controversy, no prior study has assessed the impact of retail clinics on multiple primary care functions. Using a national sample of health plan claims, we evaluated retail clinic visits’ effect on three core primary care functions: (1) first-contact care, (2) continuity of care, and (3) preventive care.
METHODS
Study Design and Population
We obtained 2007–2009 claims data from Aetna, representing care received by 13.3 million enrollees in 20 insurance regions. The sample included all 367,488 patients who visited a retail clinic and a random sample of 1,010,910 patients who did not. Aetna provided claims with primary diagnosis codes corresponding to the following services types: primary care, specialist, ambulatory facility, emergency room, laboratory, radiology, and immunizations.
Inclusion Criteria and Primary Independent Variable
For each patient, our analyses centered on an “index visit”, defined as a patient’s first visit in 2008 to a retail clinic or PCP for one of 11 simple acute conditions treatable at a retail clinic. These conditions accounted for 88 % of acute retail clinic visits in our data, and were identified as an evaluation and management visit [Current Procedural Terminology (CPT) codes 99201–99205 or 99211–99215],18 with an International Classification of Diseases (ICD)-9 primary diagnosis code for one of the 11 conditions: upper respiratory infection (460.xx, 465.xx), sinusitis (461.xx, 473.xx), bronchitis (490.xx, 466.xx), pharyngitis (462.xx, 463.xx, 034.xx), otitis media (381.xx, 382.xx), otitis externa (380.xx), conjunctivitis (372.xx), urinary tract infection (599.xx, 595.xx), allergic rhinitis (477.xx), influenza (487.xx), or unspecified viral infection (079.99).19 We grouped patients by the location of the index visit: retail clinic versus PCP. We identified index visits in 2008, because this allowed us to compare 365 days of claims before and after the index visit. To ensure that the index visit captured a patient’s first-recorded exposure to retail clinics, we excluded patients with any prior retail clinic claims. PCP visits were identified by a provider specialty coded as Family/General Practice, Internal Medicine, Obstetrics/Gynecology, or Pediatrics, and location of service coded as “Outpatient” or “Office.” Lacking data on the clinical focus of Nurse Practitioners and Physician Assistants, we did not identify these as PCPs; we included these in sensitivity analyses (Online Appendix).
We excluded patients who were not continuously enrolled in the health plan for 365 days before and after the index visit, those aged 65 or older during the study period, and those who lived farther than 20 miles (32.2 km) from the nearest retail clinic, to ensure comparability in access to care (Details in Online Appendix). The vast majority of retail clinic patients (97.6 %) lived within this radius.
Outcomes Measures
For all measures, we compared the care received in the 365 days before the index visit to that in the 365 days after.
First-Contact Care for Simple Acute Conditions
First-contact care captures the idea of patients visiting their PCP as their first source of care when they develop a new problem. We evaluated where patients initiated care for the 11 simple acute conditions treatable at retail clinics. For this analysis, we excluded the index visit and focused on other instances of simple acute care. We calculated the number of such visits at retail clinics, PCPs, or Emergency Departments (EDs), defined via ICD-9 codes and CPT codes for evaluation and management (99201–99205, 99211–99215) or ED visits (99281–5). To distinguish visits representing first-contact care from follow-up care for the same condition, we excluded visits with the same 3-digit ICD-9 diagnosis code occurring within 21 days of an initial, first-contact visit. Sensitivity analyses using 14-day and 28-day cut-offs yielded similar results (Online Appendix).
Primary Care Continuity
We assessed continuity in three ways: (1) Bice–Boxerman Continuity of Care (COC) Index; (2) total visits to a retail clinic or a PCP; and (3) the frequency of repeat visits with the same PCP. The COC Index measures the dispersion of care across providers:  , where nj is the number of visits with provider j and N is the total number of visits across all s providers. A score of 1 corresponds to perfect continuity and 0 to no continuity. We calculated the index using all PCP and retail clinic visits for all diagnoses for evaluation and management (CPT Codes 99201–99205 and 99211–99215) and health maintenance (CPT Codes 99381–7 and 99391–7). Because the COC index lacks meaningful interpretation with only one visit, we excluded patients with fewer than two visits in either the 365 days preceding or following the index visit. In sensitivity analyses, we recalculated the index including varying visit types and sites and, because the COC index can be less reliable with fewer visits, including only patients with at least three or four visits before and after the index visit (Appendix). We also measured a patient’s total number of PCP and retail clinic visits for evaluation and management or health maintenance for any diagnosis, and having one, two, or three or more of these visits with the same PCP. We excluded from all continuity measures the index visit and follow-up visits for the problem treated at the index visit (defined as above). We included follow-up visits in sensitivity analyses (Online Appendix).
, where nj is the number of visits with provider j and N is the total number of visits across all s providers. A score of 1 corresponds to perfect continuity and 0 to no continuity. We calculated the index using all PCP and retail clinic visits for all diagnoses for evaluation and management (CPT Codes 99201–99205 and 99211–99215) and health maintenance (CPT Codes 99381–7 and 99391–7). Because the COC index lacks meaningful interpretation with only one visit, we excluded patients with fewer than two visits in either the 365 days preceding or following the index visit. In sensitivity analyses, we recalculated the index including varying visit types and sites and, because the COC index can be less reliable with fewer visits, including only patients with at least three or four visits before and after the index visit (Appendix). We also measured a patient’s total number of PCP and retail clinic visits for evaluation and management or health maintenance for any diagnosis, and having one, two, or three or more of these visits with the same PCP. We excluded from all continuity measures the index visit and follow-up visits for the problem treated at the index visit (defined as above). We included follow-up visits in sensitivity analyses (Online Appendix).
Preventive Care and Diabetes Management
We assessed (1) preventive health examinations; (2) screenings; and (3) diabetes management. Preventive health examinations were defined as PCP visits for evaluation and management or health maintenance services with ICD-9 codes V20.2, V70.0, V70.3, V70.8, V70.9, or V72.3.18,19 We calculated rates of screening for cervical cancer, breast cancer, colon cancer, and Chlamydia, and diabetes management using HEDIS specifications modified to apply to 365 day periods (Definitions in Appendix).20
Covariables
Our analyses account for patient-level (gender, age, chronic diagnoses) and area-level confounders (distance from the nearest retail clinic, Health Professional Shortage Area [HPSA] status, and median household income). We identified chronic diagnoses using ICD-9 criteria described by Charlson and Kuhlthau, using claims in the year preceding the index visit.21,22 Median income and HPSA status for the ZIP Code Tabulation Area (ZCTA) including each patient’s address were drawn from the 2006 Primary Care Service Area Data sets.23 When no ZCTA was available (2.5 % of patients), we imputed a value from the closest neighboring ZIP code.
Statistical Analyses
To account for selection bias due to measurable and unmeasurable differences between patients who visited retail clinics versus PCPs, we used a “doubly robust approach” of difference-in-differences analyses with propensity score weighting.24,25
Propensity Score Weighting
For each patient, we generated a propensity score representing the probability of having an index visit at a retail clinic instead of a PCP, based on patient and area-level predictors, the index visit primary diagnosis, and PCP visit patterns in the 365 days preceding the index visit (Details in Online Appendix). Using these propensity scores, we weighted PCP patients so that they had a similar distribution to retail clinic patients for observed characteristics. Statistical modeling using these weights tested the effect of an index visit to a retail clinic instead of a PCP among patients who were equally as likely to have sought retail clinic care (i.e., average treatment effect on the treated).26
Difference-in-Differences Approach
We compared each outcome in the 365 days before and after the index visit. This difference-in-differences approach allowed each patient to serve as his or her own longitudinal control, further reducing the potential for bias due to selection and unobservable confounders. The interaction between index visit location (retail clinic versus PCP) and time (before index visit versus after) estimated the effect of visiting a retail clinic instead of a PCP.
We fit regression models using functional forms appropriate to each outcome: linear for first-contact visits for simple acute care, total primary care visits, and the COC index, and logistic for the remaining outcomes. We adjusted for patient and area-level confounders and the primary diagnosis of the index visit and applied propensity score weights. We report the marginal effect of a retail clinic index visit, defined as the average difference in the predicted value of each outcome attributable to visiting a retail clinic instead of a PCP (Details in Online Appendix).27
Subgroup Analyses
We repeated these analyses among pediatric and adult patients, and patients with and without chronic diagnoses. Because the effect of retail clinic visits might vary by prior primary care exposure, in sensitivity analyses, we stratified by the number of PCP visits in the year preceding the index visit (Online Appendix).
To address the testing of multiple comparisons, we calculated the critical p-value that limited the false discovery rate to 5 %, and considered p-values below this threshold statistically significant.28 All statistical analyses were performed using SAS (SAS Institute Inc., Cary, NC). The University of Pittsburgh and RAND Institutional Review Boards reviewed and exempted the study.
RESULTS
Study Cohort
The study cohort consisted of 23,023 patients with retail clinic index visits and 104,335 with PCP index visits (Online Appendix). Compared to those visiting PCPs, retail clinic patients were disproportionately female (62.6 % vs. 57.5 %), young adult (50.7 % vs. 34.2 % between ages 18 and 44), higher income (81.4 % vs. 74.8 % in highest three income quartiles), and healthy (90.0 % vs. 85.3 % with no chronic diagnoses). After applying propensity score weights, there were no significant differences in these characteristics (Table 1).
Table 1.
Patient Characteristics
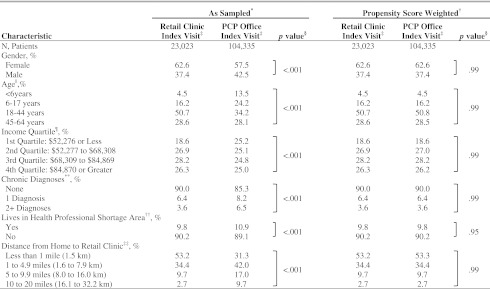
*Weighted only to account for sampling (i.e. by inverse of probability of selection)
†PCP Office Index Visit Patients weighted by “Average Treatment effect on the Treated” (ATT) propensity score weights
‡Some values do not sum to 100 % because of rounding
§Represents p-value from Chi Square test; Critical p-value = 0.031, allowing for a maximum false discovery rate of 5 %
||At time of index visit
¶ZCTA median household income
#Using Charlson et al. and Kuhlthau et al.
**Majority of ZIP code corresponds to ZCTA with HPSA designation
††Measured via straight-line distances from retail clinic and patient address ZIP Code centroids
First-Contact Care for Simple Acute Conditions
We examined where patients initiated care for subsequent instances of simple acute conditions (i.e., first-contact care). In adjusted difference-in-differences analyses, visiting a retail clinic instead of a PCP for the index visit was associated with a 27.7 visits per 100 patients relative reduction in subsequent PCP visits for new simple acute conditions (p < 0.001, retail clinic index visit: 26.6 visits per 100 patients before and 40.0 visits per 100 patients after; PCP index visit: 27.5 visits per 100 patients before and 68.5 visits per 100 patients after) (Table 2). Visiting a retail clinic instead of a PCP for the index visit was associated with a 33.8 visits per 100 patients relative increase in subsequent retail clinics visits for new simple acute conditions (p < 0 .001, retail clinic index visit: 36.6 visits per 100 patients after; PCP index visit: 2.8 visit per 100 patients after). Of note, by definition, neither had any retail clinic visits before the index visit.
Table 2.
Associations Between Retail Clinic Visits and Site of First-Contact Visits for Simple Acute Conditions (Propensity Score Weighted, Adjusted, Differences-in-Differences Analysis)
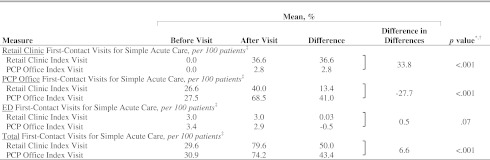
*p-values correspond to significance level of (treatment*time) interaction coefficient via the Partial F-test
†Critical p-value = 0.031, allowing for a maximum false discovery rate of 5 %
‡First-contact visits for simple acute care defined as visits for the 11 simple acute conditions treatable at retail-clinics, excluding follow-up visits with the same 3-digit ICD-9 occurring within 21 days
Primary Care Continuity
Compared to PCP patients, retail clinic patients had relative reductions in all measures of primary care continuity. Subsequent to the index visit, retail clinic patients experienced a 10.9 percentage-point relative reduction in COC index scores, (p < 0 .001; retail clinic: 54.4 % before and 44.7 % after; PCP: 54.7 % before and 55.8 % after) (Table 3). Smaller, but still significant, reductions were seen when the COC index was calculated using PCP visits only (1.5 percentage-points, p = 0 .024) or excluding visits for simple acute conditions treatable at retail clinics (3.3 percentage-points, p < 0 .001) (Online Appendix).
Table 3.
Associations Between Retail Clinic Visits and Continuity of Care (Propensity Score Weighted, Adjusted, Differences-in-Differences Analysis)
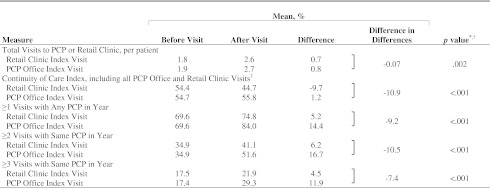
*p-values correspond to significance level of (treatment*time) interaction coefficient via Partial F-test and Wald’s Chi Squared test for linear and logistic regressions, respectively
†Critical p-value = 0.031, allowing for a maximum false discovery rate of 5 %
‡COC Index analyses exclude patients with fewer than two eligible visits in the 365-days before or after the index visit; Analyses include 7,906 patients with Retail Clinic Index Visits, and 59,395 patients with PCP Office Index Visits
Retail clinic patients experienced a 9.2 percentage-point relative reduction in having one or more visits for any reason with a PCP (p < 0 .001; retail clinic: 69.6 % before and 74.8 % after; PCP: 69.6 % before and 84.0 % after) and a 10.5 percentage-point relative reduction in having two or more such visits with the same PCP (p < 0 .001; retail clinic: 34.9 % before and 41.1 % after; PCP: 34.9 % before and 51.6 % after) (Table 3). Similar effects were observed in stratified analyses (Table 5).
Table 5.
Patient Subsets: Associations Between Retail Clinic Visits and Continuity of Care and Preventive Care (Propensity Score Weighted, Adjusted, Differences-in-Differences Analysis)
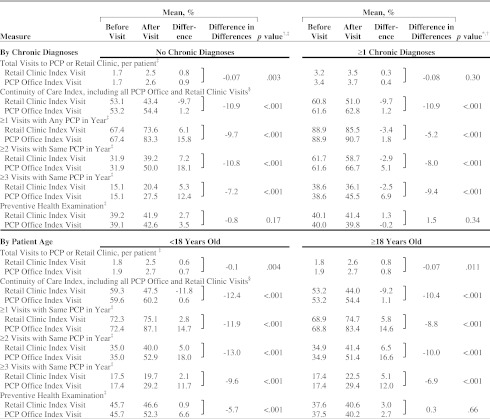
*p-values correspond to significance level of (treatment*time) interaction coefficient via Partial F-test and Wald’s Chi Squared test for linear and logistic regressions, respectively
†Critical p-value = 0.031, allowing for a maximum false discovery rate of 5 %
‡N, patients for visit counts and preventive health examination: no chronic diagnoses 20,717 retail clinic and 88,629 PCP patients; ≥1 chronic diagnoses 2,306 retail clinic patient and 15,706 PCP patients; <18 years 4,751 retail clinic and 42,449 PCP patients; ≥18 years 18,272 retail clinic and 61,886 PCP patients
§N, patients for COC Index: no chronic diagnoses 6,540 retail clinic and 47,322 PCP Patients; ≥1 chronic diagnoses 1,366 retail clinic and 12,073 PCP patients; <18 years 1,571 retail clinic and 24,688 PCP patients; ≥18 years 6,335 retail clinic and 34,707 PCP patients
Preventive Care
There were no differences between PCP and retail clinic patients’ rates of preventive health examinations; screening for breast cancer, cervical cancer, colorectal cancer, or Chlamydia; or diabetes management, including hemoglobin A1c testing, eye examinations, LDL testing, and nephropathy care (Table 4). Among pediatric patients, retail clinic patients experienced a 5.7 percentage-point relative reduction in preventive health examinations (p < 0 .001; retail clinic: 45.7 % before, 46.6 % after; PCP: 45.7 % before, 52.3 % after) (Table 5).
Table 4.
Associations Between Retail Clinic Visits and Preventive Care (Propensity Score Weighted, Adjusted, Differences-in-Differences Analysis)
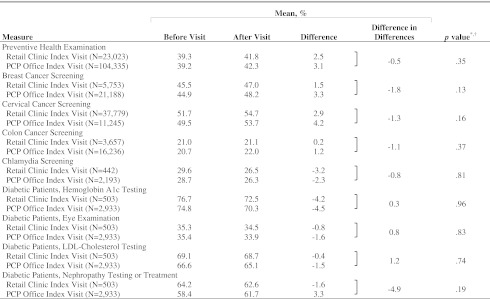
*p-values correspond to significance level of (treatment*time) interaction coefficient via Wald’s Chi Squared test
†Critical p-value = 0.031, allowing for a maximum false discovery rate of 5 %
Sensitivity Analyses
In the Online Appendix we present additional methodological detail; unadjusted analyses; and sensitivity analyses in which we stratified patients by baseline PCP visits, varied definitions of PCPs and follow-up care, and recalculated the COC Index with varying visit types and eligibility criteria.
DISCUSSION
Retail clinics visits are associated with adverse impacts on two aspects of primary care: compared to similar patients who visited PCPs, patients who visited retail clinics subsequently had less first-contact care and less continuity with PCPs. However, there were no associations between retail clinic visits and preventive care or diabetes management.
Given retail clinics’ emphasis on convenience and patient satisfaction,29,30 it may be unsurprising that patients who visited retail clinics were likely to go back to a retail clinic for subsequent acute problems. Retail clinic patients are generally healthy and so these visits represent a sizeable portion of their primary care visits; therefore, the observed modest decreases in continuity may also predictable. However, we also observed decreased continuity when excluding retail clinic visits and simple acute visits from our measures of continuity, suggesting that the negative impact on continuity is not solely due to a shift of simple acute visits from PCP offices to retail clinics.
The lack of association between retail clinic visits and preventive care is consistent with previous studies.17 Retail clinics did not offer these services during the years we observed, so retail clinics could not provide these services in PCPs’ stead. We cannot comment as to the impact of retail clinics’ more recent scope of care expansions to include more preventive and chronic disease management services.31,32
Taken together, the interpretation of our findings depends on one’s view on the relative importance of different aspects of primary care. Some might contend that continuity is the cornerstone of primary care and, therefore, retail clinics’ negative impact on continuity is critical. Others might argue that continuity and first-contact care are less important than preventive care, especially for a healthy patient population. In this light, retail clinics’ impact on primary care may not be as great as feared.
While the patients and concerns that lead them to seek care were similar, the ultimate content of index visits likely differed between the two sites. This was reflected in the evaluation and management billing codes: PCPs coded 92.4 % at the more complex 3–4 range, while retail clinics coded 99.4 % in the less complex 2–3 range. We sought to assess how such differences between retail clinic and PCP visits for similar concerns impacted subsequent primary care.
One concern with our study is how we measure continuity. We focus on visit-continuity, rather than informational-continuity; the latter results when a provider can marshal complete information regarding a patient’s history.33 The relative importance of visit-continuity versus informational-continuity in primary care is unclear, especially as primary care moves towards a team-based model. Information-continuity could be achieved if retail clinic notes were sent and incorporated into PCPs’ records. However, we do not know whether this is common, and strategies to increase informational-continuity, such as regional health information organizations, have proven challenging to implement.2,13,14,34,35 Nonetheless, policies that establish better communication and collaboration between retail clinics and PCPs seem justified if informational-continuity can compensate for reductions in visit-continuity.14,36–38 Further, the practical significance of the 10.9 percentage-point decrease in the COC Index is unclear. Decreases in the COC Index are associated with lower quality and coordination of care, but the Index varies across patient populations and settings.9,10,39–41 Additionally, we could not assess whether a provider was a patient’s perceived usual source of care; our claims-based approach and look-back period precluded reliable definition of such relationships. Lastly, lacking practice-level identifiers, we assess only within-provider continuity and cannot address within-practice continuity, be it among physicians alone or among physicians and mid-level providers.
Our study compared the care received by patients who visited a retail clinic to patients who visited a PCP. Yet, most patients who visit retail clinics lack PCPs and those with a PCP may not be able to obtain a timely appointment. These patients may instead stay home, visit a nurse practitioner in the practice, or visit an ED.29,42 Future work might compare patients who visit a retail clinic to those who do not seek care, who visit a nurse practitioner in a primary care practice, or who go to an ED.
Given the novelty of retail clinics and the data available, we focused on the short-term (12 month) impact of retail clinics. Future studies should assess the impact over the longer term. Over time, a more negative impact of retail clinics on preventive care or continuity may be observed, particularly among younger, healthy patients who infrequently visit PCPs and preferentially visit retail clinics.
Our study has other limitations. While we use propensity score methods and a difference-in-difference design to account for selection bias, concerns about unobservable confounders might remain. Because we only had access to health plan claims, we cannot assess preventive services, counseling, or disease management services only available in the medical chart. We concentrate on commercially insured patients, the majority of retail clinic users;15,16 however, our findings may not be generalizable to publicly-insured or uninsured patients. Our study lacked direct measures of health outcomes and costs of care. Finally, the increase in simple acute visits following the index visit is largely an artifact of how we identified index visits and our focus on patients most likely to visit retail clinics. Defined as the first simple acute visit in 2008, index visits, by default, had some preceding period with no such care, while no such restriction applied to the post-period. In addition, we used propensity score methods to ensure that PCP patients’ demographics and baseline visit patterns were similar to retail clinic patients’: lower baseline-users of primary care services for whom a year-to-year increase was inherently more likely. The definitional restriction was consistently applied to both groups and they were well-matched on baseline simple acute care utilization; consequently, comparisons of subsequent utilization between the two are not undermined.
In conclusion, we find that when substituting for PCP visits, retail clinic visits are associated with negative impacts on first-contact for simple acute care and continuity, but not on preventive and chronic disease care.
Electronic supplementary material
(DOCX 474 KB)
Acknowledgements
We thank Aetna Health Plan for donating the data and answering our technical questions. We also thank Martin Gaynor, Ph.D. at Carnegie Mellon University for his useful input on this work.
Ms. Reid had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This project was funded by the Robert Wood Johnson Foundation’s Changes in Health Care Financing and Organization (HCFO) Initiative. Ms. Reid was supported by a Clinical Research Fellowship from the Doris Duke Charitable Foundation via the University of Pittsburgh School of Medicine, and a Clinical and Translational Science Institute Multidisciplinary Predoctoral Fellowship, awarded through the Clinical and Translational Science Institute and the Institute for Clinical Research Education at the University of Pittsburgh (Grant 5TL1RR024155-05). Dr. Mehrotra was supported by a career development award (KL2 RR024154) from the National Center for Research Resources, a component of the National Institutes of Health.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.U.S. Walk-In Clinic Market Report. Vol 5(7) Shoreview: Merchant Medicine LLC; 2012. pp. 1–7. [Google Scholar]
- 2.Cassel CK. Retail clinics and drugstore medicine. JAMA. 2012;307(20):2151–2152. doi: 10.1001/jama.2012.3966. [DOI] [PubMed] [Google Scholar]
- 3.Ashwood JS, Reid RO, Setodji CM, Weber ED, Gaynor MS, Mehrotra A. Trends in retail clinic use among the commercially insured. Am J Manag Care. 2011;17(11):e443-448. [PMC free article] [PubMed]
- 4.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grumbach K, Selby JV, Damberg C, et al. Resolving the gatekeeper conundrum: what patients value in primary care and referrals to specialists. JAMA. 1999;282(3):261–266. doi: 10.1001/jama.282.3.261. [DOI] [PubMed] [Google Scholar]
- 6.Forrest CB, Starfield B. The effect of first-contact care with primary care clinicians on ambulatory health care expenditures. J Fam Pract. 1996;43(n1):40–49. [PubMed] [Google Scholar]
- 7.Gill JM, Mainous AG., 3rd The role of provider continuity in preventing hospitalizations. Arch Fam Med. 1998;7(4):352–357. doi: 10.1001/archfami.7.4.352. [DOI] [PubMed] [Google Scholar]
- 8.Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974–980. [PubMed] [Google Scholar]
- 9.Christakis DA, Mell L, Wright JA, Davis R, Connell FA. The association between greater continuity of care and timely measles–mumps–rubella vaccination. Am J Public Health. 2000;90(6):962–965. doi: 10.2105/AJPH.90.6.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524–529. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- 11.Saultz JW. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3(2):159–166. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff. 2010;29(5):766–772. doi: 10.1377/hlthaff.2010.0025. [DOI] [PubMed] [Google Scholar]
- 13.Pollack CE, Gidengil C, Mehrotra A. The growth of retail clinics and the medical home: two trends in concert or in conflict? Health Aff. 2010;29(5):998–1003. doi: 10.1377/hlthaff.2010.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinick RM, Pollack CE, Fisher MP, Gillen EM, Mehrotra A. Policy Implications of the Use of Retail Clinics. 2010; http://www.rand.org/pubs/technical_reports/TR810. Accessed September 8, 2012. [PMC free article] [PubMed]
- 15.Mehrotra A, Wang MC, Lave JR, Adams JL, McGlynn EA. Retail clinics, primary care physicians, and emergency departments: a comparison of patients’ visits. Health Aff (Millwood) 2008;27(5):1272–1282. doi: 10.1377/hlthaff.27.5.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tu HT, Cohen GR. Checking up on retail-based health clinics: is the boom ending? Issue Brief (Commonw Fund) 2008;48:1–11. [PubMed] [Google Scholar]
- 17.Mehrotra A, Hangsheng L, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for three common illnesses. Ann Intern Med. 2009;151(5):321–328. doi: 10.7326/0003-4819-151-5-200909010-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CPT Standard Edition: Current Procedural Terminology. Chicago, IL: American Medical Association Press; 2010.
- 19.International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). 5th ed. Geneva, Switzerland: World Health Organization; 1994.
- 20.National Committee on Quality Assurance. HEDIS 2011. 2011;2, Technical Specifications.
- 21.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 22.Kuhlthau K, Ferris TGG, Beal AC, Gortmaker SL, Perrin JM. Who cares for medicaid-enrolled children with chronic conditions? Pediatrics. 2001;108(4):906–912. doi: 10.1542/peds.108.4.906. [DOI] [PubMed] [Google Scholar]
- 23.Health Resources and Services Administration. Primary Care Service Areas—2006 Edition. 2006; http://datawarehouse.hrsa.gov/pcsa2006.aspx. Accessed September 8, 2012.
- 24.Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics. 2005;61(4):962–973. doi: 10.1111/j.1541-0420.2005.00377.x. [DOI] [PubMed] [Google Scholar]
- 25.Kang JDY, Schafer JL. Demystifying double robustness: a comparison of alternative strategies for estimating a population mean from incomplete data. Stat Sci. 2007;22(4):523–539. doi: 10.1214/07-STS227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. doi: 10.1093/biomet/70.1.41. [DOI] [Google Scholar]
- 27.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. doi: 10.1111/j.0006-341X.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 28.Benjamini Y, Hochberg Y. Controlling the false discovery rate—a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57(1):289–300. [Google Scholar]
- 29.Wang MC, Ryan G, McGlynn EA, Mehrotra A. Why do patients seek care at retail clinics, and what alternatives did they consider? Am J Med Qual. 2010;25(2):128–134. doi: 10.1177/1062860609353201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laws M, Scott MK. The emergence of retail-based clinics in the United States: early observations. Health Aff (Millwood) 2008;27(5):1293–1298. doi: 10.1377/hlthaff.27.5.1293. [DOI] [PubMed] [Google Scholar]
- 31.Freiden J. Retail Clinics Branch into Chronic Disease Treatment. 2010; http://www.medpagetoday.com/PracticeManagement/PracticeManagement/19207. Accessed September 8, 2012.
- 32.Porter S. AAFP Board Revises Retail Health Clinic Policy: Academy Opposes Ongoing Expansions in Scope of Service. AAFP News Now 2010; http://www.aafp.org/online/en/home/publications/news/news-now/inside-aafp/20100224retail-policy.html. Accessed September 8, 2012.
- 33.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adler-Milstein J, Bates DW, Jha AK. U.S. Regional Health Information Organizations: progress and challenges. Health Aff. 2009;28(2):483–492. doi: 10.1377/hlthaff.28.2.483. [DOI] [PubMed] [Google Scholar]
- 35.Adler-Milstein J, McAfee AP, Bates DW, Jha AK. The State Of Regional Health Information Organizations: current activities and financing. Health Aff. 2008;27(1):w60–w69. doi: 10.1377/hlthaff.27.1.w60. [DOI] [PubMed] [Google Scholar]
- 36.American Academy of Family Practice. AAFP Policy on Retail Health Clinics. 2010; http://www.aafp.org/online/en/home/policy/policies/r/retailhealth.html. Accessed September 8, 2012.
- 37.Retail-Based Clinic Policy Work Group AAP principles concerning retail-based clinics. Pediatrics. 2006;118(6):2561–2562. doi: 10.1542/peds.2006-2681. [DOI] [PubMed] [Google Scholar]
- 38.American College of Physicians. ACP Principles on Retail Health Clinics. 2007; http://www.acponline.org/advocacy/where_we_stand/other_issues/prhc.htm. Accessed September 8, 2012.
- 39.Liss DT, Chubak J, Anderson ML, Saunders KW, Tuzzio L, Reid RJ. Patient-reported care coordination: associations with primary care continuity and specialty care use. Ann Fam Med. 2011;9(4):323–329. doi: 10.1370/afm.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Christakis DA, Wright JA, Koepsell TD, Emerson S, Connell FA. Is greater continuity of care associated with less emergency department utilization? Pediatrics. 1999;103(4):738–742. doi: 10.1542/peds.103.4.738. [DOI] [PubMed] [Google Scholar]
- 41.Christakis DA, Wright JA, Zimmerman FJ, Bassett AL, Connell FA. Continuity of care is associated with high-quality careby parental report. Pediatrics. 2002;109(4):e54. doi: 10.1542/peds.109.4.e54. [DOI] [PubMed] [Google Scholar]
- 42.Pitts SR, Carrier ER, Rich EC, Kellermann AL. Where Americans get acute care: increasingly, it’s not at their doctor’s office. Health Aff (Millwood) 2010;29(9):1620–1629. doi: 10.1377/hlthaff.2009.1026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 474 KB)


