Introduction
The United States has the highest incarceration rate in the industrialized world,1,2 resulting in the imprisonment of 1 in every 100 citizens.3 Approximately ten million people are jailed annually in the U.S., half of whom are released within two days.4 The incarcerated population is comprised of medically and socially vulnerable individuals, many of who have undiagnosed and untreated mental illnesses, substance use disorders (SUDs) and HIV/AIDS.5,6 Released jailed detainees also have difficulty in transitioning to the community, obtaining housing, finding work, and accessing vital healthcare.7,8
For people living with HIV/AIDS (PLWHA), access to antiretroviral therapy (ART) is critical in order to maintain viral suppression; however, incarceration and re-entry into the community post-release have a disruptive effect on their medical treatment.9 It has been shown that the period immediately after release is a highly vulnerable time for HIV-infected individuals; they experience decreased access to ART,10 poor virological and immunological treatment outcomes11,12 and high rates of HIV risk behaviors.13,14 In fact, HIV-infected prisoners who are released to the community, lose the benefits achieved through access to ART provided within a correctional setting.11 For PLWHA with SUDs - a chronic and relapsing disease - medical and psychiatric co-morbidities further complicate HIV treatment and adherence.15-17 Left undiagnosed or untreated, relapse to drug or alcohol use post-release exceeds 85%, which further contributes to the poor health outcomes of these released jail detainees.18 This vicious cycle remains uninterrupted unless evidence-based substance abuse treatments (SATs) are introduced at the time of incarceration or immediately upon release.19
Linking HIV-infected inmates to HIV primary care services upon release from correctional settings, including jails, is essential to improving health outcomes among the recently incarcerated.9 This is especially important for PLWHA, since one sixth of all PLWHA in the U.S. transition through correctional facilities annually.4,20 Apart from potential medical problems and SUDs, released PLWHA detainees also encounter complications arising from social instability, lack of insurance coverage and homelessness.7,8,21 Jails may serve as effective venues for disease screening and initiation of community-based interventions for HIV therapy and SUDs.22 Yet, relatively little evidence exists to support this claim,23 especially due to the short-term periods detainees remain in these settings.24 A deeper understanding of the complex contribution of multiple co-factors, including individual and social factors, environmental determinants, and treatment for SUDs - on post-release outcomes is needed. We therefore sought to examine substance abuse outcomes among a large cohort of HIV-infected jail detainees post-release to better inform researchers, healthcare providers and policy makers.
Methods
Sample and Study Design
This HRSA-funded Special Projects of National Significance (SPNS) initiative was funded to design, implement, and evaluate innovative methods for transitioning PLWHA from the jail setting to post-release services, such as healthcare, HIV medical care, substance abuse treatment and other supplementary services.25 The initiative followed a cohort of detained HIV-infected individuals from incarceration, release, and through the provision of various individual site interventions. HIV-infected inmates were identified either as previously diagnosed or through routine HIV testing 23 through referral to HIV services at ten sites in nine different states (CT, GA, IL, MA, NY, OH, PA, SC, RI).25 A more detailed description of the methods of the initiative is included as an appendix to this supplement.
After referral by the clinical staff, participants were offered transitional services by EnhanceLink staff. Individuals opting to participate in the initiative’s evaluation underwent informed consent procedures and were interviewed during incarceration (baseline) and after release at the six-month time period. In addition to the two interviews, a post-release review was completed by case managers for each inmate one month after release from jail. The multisite study was approved by both central and site-specific Institutional Review Boards; a Certificate of Confidentiality provided additional protections to subjects. Eligibility requirements included being 18 years or older, HIV-infected, and currently incarcerated within a designated jail. Duration of detention was not an eligibility criterion for participation and participants could be approached at any time after referral. All sites provided at a minimum, some element of case management services.25
Figure 1 depicts the disposition of study participants. After providing informed consent, 1270 eligible participants were enrolled between January 2008 and March 2011. Of the enrolled subjects, 1255 completed the baseline interview during which they provided information about their criminal justice history, living conditions, family and social relationships, HIV and health status, medical status, health information and relevant demographic information. In addition, they were asked about drug/alcohol use, psychiatric status, HIV medication utilization, and housing status 30 days prior to incarceration. Among the 1255 with complete baseline data, 222 individuals were excluded from further analysis because they were ineligible to provide follow-up data; reasons for ineligibility included being sentenced to long jail terms, early re-incarceration, death, or deportation.26 The final analytic sample consisted of 1032 subjects who had a completed post-release assessment at the one-month period after release. By the six month post-release assessment, 449 of the 1032 eligible participants had moved or were lost to follow-up, leaving 583 subjects with complete data, including baseline and observable data at the six-month post-release period. The post-release interviews documented participants’ release information, receipt of case management services, utilization of psychiatric and SAT, medical health status, drug and alcohol use, psychiatric status, and living conditions.
Figure 1.
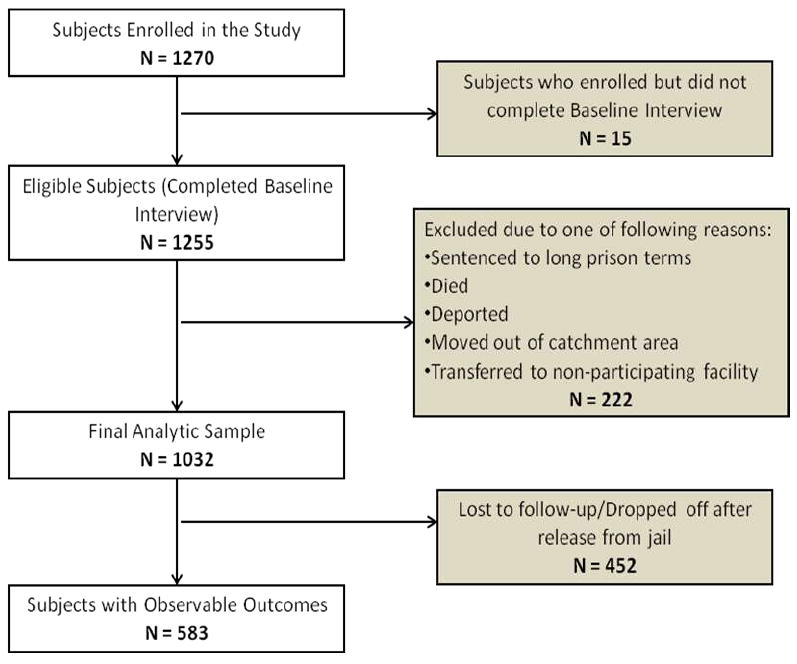
Participant Disposition
Study Instruments
Dependent Variable of Interest
Due to research suggesting that drug and alcohol relapse occurs soon after release,18,19 and that cocaine and heroin are among the most widely abused drugs,27 the two dependent variables of interest employed in this study were: (1) any cocaine use at the end of the six-month post-release assessment, and (2) any opioid (heroin, opiates/analgesics/painkillers) use at the end of the six-month post-release assessment.
Independent Variables of Interest
The analytical approach in this study was guided by the Behavioral Model for Healthcare Utilization in Vulnerable Populations.28,29 At its fundamental basis, this conceptual model asserts that predisposing factors, enabling resources, and need factors collectively influence utilization of healthcare services and subsequent healthcare outcomes, such as substance abuse outcomes. Predisposing factors are demographic and social characteristics (i.e., age, gender, employment status etc.) that have a critical impact on healthcare utilization. Enabling resources are personal and community resources that positively influence linkage to care; e.g., having access to health insurance and substance abuse treatment or evidence-based treatment. Need factors are determined by an individual’s perceived health needs or priorities, current health status, severity of illness, and medical co-morbidities. The Healthcare Behavioral model was adapted for the current study (see Figure 2) by incorporating factors that are salient for HIV-infected jail detainees; these served as independent variables in our analysis.
Figure 2.
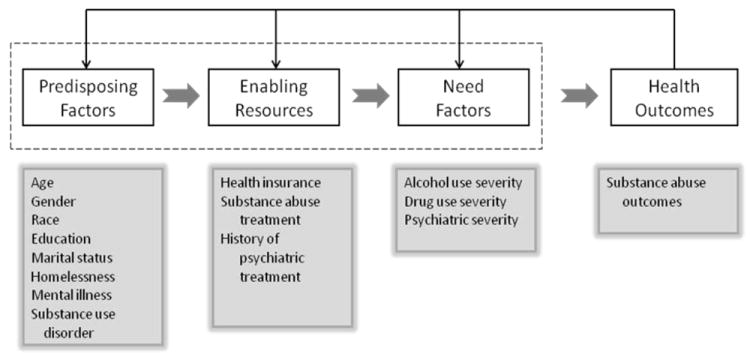
Conceptual model for post-release substance abuse outcomes among HIV-infected jail detainees
All the independent variables in this study except for addiction severity were measured by study-specific instruments. Demographic variables included self-reported measures of age, gender, relationship status, race, education and employment status. Housing status was defined previously as being homeless or not in the 30 days prior to incarceration;21 baseline recent drug use was defined as any cocaine and opioid use 30 days prior to incarceration and pre-incarceration mental illness was operationalized as having had experienced one of the following in the 30 days before incarceration – serious depression, serious anxiety, hallucinations, trouble understanding, concentrating or remembering; trouble controlling violent behavior, serious thoughts of suicide, attempted suicide, having had prescribed medication for psychological problems.
Psychiatric treatment was assessed using two variables: (1) inpatient treatment, operationalized as number of times having been treated in a hospital for psychological or emotional problems during lifetime and (2) outpatient treatment, operationalized as having been treated as a private patient for psychological or emotional problems during lifetime. Substance abuse treatment was assessed using two variables which were both dichotomously defined: (1) the case manager having made contact with a community service provider to obtain substance abuse services for the client and (2) the client attending at least one session of the SAT program after release. Data on whether medication-assisted therapy (MAT) was used to treat alcohol or drug dependence was not collected.
Substance use addiction severity was measured by the Addiction Severity Index (ASI) fifth edition.30 The ASI drug and alcohol composite scores (CS) were reported as both continuous variables ranging from zero to one (with one indicating more severe addiction), and as dichotomous variables by implementing previously validated cut-off points: > 0.17 defined severe alcohol problems and > 0.16 defined severe drug problems. An ASI drug CS cut-off of 0.16 has been shown to have 84% sensitivity (84% of patients meeting DSM-IV criteria were identified) and 81% specificity (81% of patients not meeting diagnostic criteria were accurately identified). Similarly, an ASI alcohol CS cut-off of 0.17 has been shown to have 85% sensitivity and 80% specificity.31 Severity of mental illness was evaluated with the ASI psychiatric CS and was measured as both a continuous (zero to one) and dichotomous variable with a cut-off at 0.22. Similar thresholds have been used in studies looking to identify severe psychiatric illness.32,33
Statistical Analyses
Data was analyzed using SPSS 19 (IBM, New York). Prior to analysis, all the independent variables except demographics were binary-coded. In order to examine the impact of predictor variables (predisposing factors, enabling resources, need factors) on the two dependent variables (cocaine use and opioid use at the end of the 6-month post-release assessment), logistic regression was used. Univariate analysis was first conducted for each independent variable with the two distinct outcomes using the Wald test. Factors with probability value less than 0.10 were then included in the final multivariate model. This approach to the final regression model had the best goodness of fit using the Aikake Information Criterion (AIC).
Results
Table 1 provides the baseline characteristics of the study sample. In general, the subjects were predominantly single, African-American, heterosexual men in their mid-forties. Almost half of the sample reported not having finished high school and three-fifths reported being unemployed in the period before incarceration. Although a majority had stable housing and medical insurance prior to incarceration, correlation analysis revealed that baseline homelessness was negatively correlated with having insurance at baseline (r = -0.16, p < .001), suggesting that individuals without stable housing were more likely to lack insurance. Since subject attrition in this study was high, it is likely that subjects with unstable housing and medical insurance were the ones who were lost to follow-up. There is some evidence of this, as the percentage of people surveyed at the six-month post-release interview had lower rates of homelessness and higher rates of insurance. This strongly suggests that those without stable housing or insurance were more likely to be missing from the sample at six months.
Table 1.
Baseline characteristics of study participants (N=1032)
| N (%) | ||
|---|---|---|
| Age in years (Mean, SD) | (44.3, 8.87) | |
| Sex | ||
| Male | 704(68.2%) | |
| Female | 306 (29.7%) | |
| Transgender | 17 (1.7%) | |
| Race | ||
| White | 205 (19.9%) | |
| Black | 627 (60.8%) | |
| Marital Status | ||
| Single | 571 (55.3%) | |
| Separated/Divorced/Widowed | 1315 (12.6%) | |
| Married/Committed | 329 (31.8%) | |
| Sexual Orientation | ||
| Heterosexual | 802 (77.7%) | |
| Homosexual | 96 (9.3%) | |
| Bisexual | 100 (9.7) | |
| Education | ||
| Some high school | 511 (49.5%) | |
| High school diploma/GED | 344 (33.3%) | |
| College | 159 (15.4%) | |
| Employment | ||
| Full-time work | 93 (9.0%) | |
| Part-time work | 117 (11.4%) | |
| Unemployed | 646 (62.6%) | |
| Homelessness prior to incarceration | ||
| Yes | 372 (36.0%) | |
| No | 657 (63.7%) | |
| Insurance prior to incarceration | ||
| Yes | 774 (75.0%) | |
| No | 255 (24.7%) | |
| Homelessness at six months post-release (N = 583) | ||
| Yes | 111 (19.0%) | |
| No | 468 (80.3%) | |
| Insurance at six months post-release (N = 583) | ||
| Yes | 505 (86.6%) | |
| No | 74 (12.7%) | |
In order to understand the factors that may have lead to large-scale subject attrition, a comparison of retained and lost participants was performed using baseline social characteristics such as homeless and insurance coverage, substance use, mental illness and previous psychiatric care. Table 2 shows that significantly larger percentages (p < 0.01) of subjects who dropped out or were lost to follow-up by the six-month post-release assessment were homeless (41.1% vs. 32.4%) before incarceration. Participants with observations at six months post-release were significantly more likely to have medical insurance (80.2% vs. 68.7%) prior to incarceration. Additionally, participants lost to follow-up were significantly more like to have pre-incarceration mental illness (72.4% vs. 62.4%) compared to those who were retained. The individuals without follow-up data, however, were no more likely to have: (1) used cocaine in the 30 days before incarceration; (2) had higher severity of drug and alcohol use; (3) had severe psychiatric illness; and (4) had higher mean ASI alcohol, drug and psychiatric composite scores compared to those who had complete follow-up data. Thus, for the dependent variables of interest - heroin and cocaine use at six months post-release - these characteristics did not differ, allowing important comparisons for substance use to be assessed.
Table 2.
Comparison of baseline social characteristics, substance use disorders and psychiatric co-morbidities of jail detainees who completed study and who were lost to follow-up
| Completed follow-up (N = 583) N (%) | Lost to follow-up (N = 449) N (%) | p value | ||||
|---|---|---|---|---|---|---|
| Social Characteristics | ||||||
|
| ||||||
| Homelessness | 188 (32.4%) | 184 (41.1%) | < 0.01 | |||
| Has insurance | 467 (80.2%) | 307 (68.7%) | < 0.001 | |||
|
| ||||||
|
Substance Use
|
||||||
| Cocaine use in the 30 days prior to incarceration | 279 (47.9%) | 226 (50.3%) | ns | |||
| Opioid use in the 30 days prior to incarceration | 150 (25.7%) | 109 (24.3%) | ns | |||
| Mean ASI Score - Drugs (SD) | 0.22 (0.28) | 0.22 (0.18) | ns | |||
| Mean ASI Score - Alcohol (SD) | 0.23 (0.63) | 0.25 (0.63) | ns | |||
| High drug use severity (ASI > 0.16) | 291 (53.0%) | 240 (57.3%) | ns | |||
| High alcohol use severity (ASI > 0.17) | 190 (33.3%) | 154 (35.6%) | ns | |||
|
| ||||||
|
Psychiatric Co-morbidities
|
||||||
| Experienced mental illness (30 days pre-incarceration) | 364 (62.4%) | 325 (72.4%) | < 0.001 | |||
| Inpatient treatment for psychiatric illness | 186 (31.9%) | 155 (34.5%) | ns | |||
| Outpatient treatment for psychiatric illness | 153 (26.2%) | 128 (28.5%) | ns | |||
|
| ||||||
|
Psychiatric Co-morbidities
|
||||||
| Mean ASI Score - Psychiatric (SD) | 0.28 (0.31) | 0.32 (0.30) | ns | |||
| High severity of psychiatric illness (ASI > 0.22) | 289 (50.2%) | 242 (55.5%) | ns | |||
Opioid use is defined as having either used heroin or other opiates/analgesics/painkillers.
Abbreviations: ASI = Addiction Severity Index; SD = Standard Deviation; ns = Not Significant
The univariate and multivariate analyses for factors associated with active use of cocaine at the end of the six month post-release assessment are presented in Table 3. Although a number of factors were significantly associated with persistent cocaine use in the univariate analysis, the multivariate analysis showed that post-release homelessness (AOR=1.88, 95% CI 0.90, 3.94), both high alcohol use (AOR=2.03, 95% CI 0.95, 4.34) and high drug use (AOR=11.79, 95% CI 5.70, 24.36) severity, and pre-incarceration cocaine use (AOR=1.97, 95% CI 0.99, 3.90) were significantly associated with increased cocaine use at the six-month post-release period. Receiving health insurance after release, however, significantly decreased the likelihood of post-release cocaine use (AOR=0.42, 95% CI 0.17, 1.03).
Table 3.
Factors associated with cocaine use at the end of the six month post-release assessment
| Factors | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
|
| ||||
| p | OR (95% CI) | p | AOR (95% CI) | |
| Gender | ||||
| Male | Referent | Referent | ||
| Female | < 0.01 | 1.91 (1.20, 3.05) | ns | -- |
| Employment Status | ||||
| Full time | Referent | Referent | ||
| Unemployed | < 0.10 | 3.27 (0.86, 12.41) | ns | -- |
| Mental illness (six-months post-release) | < 0.01 | 2.03 (1.28, 3.24) | ns | -- |
| Insurance (six-months post-release) | < 0.01 | 0.42 (0.24, 0.74) | < 0.10 | 0.42 (0.17, 1.03) |
| Homelessness (pre-incarceration) | < 0.05 | 1.59 (1.01, 2.51) | ns | |
| Homelessness (six-months post-release) | < 0.001 | 4.24 (2.62, 6.88) | < 0.10 | 1.88 (0.90, 3.94) |
| Inpatient treatment for psychiatric illness | < 0.05 | 1.60 (1.01, 2.52) | ns | -- |
| High alcohol use severity (pre-incarceration) | < 0.10 | 1.55 (0.98, 2.45) | ns | -- |
| High alcohol use severity (six-months post-release) | < 0.001 | 5.02 (3.03, 8.31) | < 0.10 | 2.03 (0.95, 4.34) |
| High drug use severity (six-months post-release) | < 0.001 | 20.61 (11.47, 37.05) | < 0.001 | 11.79 (5.70, 24.36) |
| High severity of psychiatric illness (six-months post-release) | < 0.001 | 2.39 (1.52, 3.77) | ns | -- |
| Cocaine use (30 days pre-incarceration) | < 0.001 | 2.38 (1.50, 3.78) | < 0.10 | 1.97 (0.99, 3.90) |
Univariate analyses were performed for age, race, relationship status, sexual orientation, education, outpatient treatment for mental illness, utilization of substance abuse treatments, severity of drug use and psychiatric illness at baseline; however, none of these were significant.
Abbreviations: CI = Confidence Interval; OR = Odds Ratio; AOR = Adjusted Odds Ratio, ns = not significant
Table 4 illustrates the univariate and multivariate analyses for factors associated with opioid use at the end of the six-month post-release assessment. Similar to the findings for cocaine use at the end of the six-month post-release observation period, several factors were significant in the univariate analysis. In the multivariate analysis, however, pre-incarceration opioid use and high drug use severity at the six-month post-release observation portended a 32- and 25-fold increased risk respectively, for ongoing opioid use six months after release. Being in a committed relationship (AOR=4.14, 95% CI 1.21, 14.22) was also associated with increased association with the dependent variable.
Table 4.
Factors associated with opioid use at the end of the six-month post-release assessment
| Factors | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
|
| ||||
| p | OR (95% CI) | p | AOR (95% CI) | |
| Gender | ||||
| Male | Referent | |||
| Female | < 0.05 | 2.18 (1.19, 3.98) | ns | -- |
| Marital status | ||||
| Single | Referent | |||
| Separated | < 0.10 | 2.77 (0.87, 8.86) | ns | -- |
| Married | < 0.01 | 3.29 (1.34, 8.11) | ns | -- |
| Committed (living together) | < 0.05 | 2.63 (1.21, 5.73) | < 0.05 | 4.14 (1.21, 14.22) |
| Homelessness (six-months) | < 0.001 | 3.81 (2.06, 7.04) | ns | -- |
| High alcohol use severity (six-months) | < 0.001 | 3.81 (2.06, 7.04) | ns | -- |
| High drug use severity (pre-incarceration) | < 0.05 | 2.23 (1.14, 4.36) | ns | -- |
| High drug use severity (six-months) | < 0.001 | 19.80 (9.80, 40.01) | < 0.001 | 25.06 (8.02, 78.34) |
| High severity of psychiatric illness (six-months) | < 0.01 | 2.29 (1.25, 4.17) | ns | -- |
| Cocaine use (30 days pre-incarceration) | < 0.001 | 3.61 (1.84, 7.08) | ns | -- |
| Opioid use (30 days pre-incarceration) | < 0.001 | 12.56 (6.21, 25.41) | < 0.001 | 31.86 (9.08, 111.84) |
Univariate analyses were performed for age, race, sexual orientation, education, employment status, insurance, mental illness, utilization of substance abuse treatments, and severity of alcohol use and psychiatric illness at baseline; however, none of these were significant.
Opioid use is defined as having either used heroin or other opiates/analgesics/painkillers.
Abbreviations: CI = Confidence Interval; OR = Odds Ratio; AOR = Adjusted Odds Ratio, ns = not significant
Discussion
The results from this study show that SUDs and rates of mental and psychiatric illness are highly prevalent among PLWHA entering jails. Compared to the general U.S. population,34 this sample had a higher rate of drug use, with nearly half suffering from high drug use severity. Co-morbid mental illness was also high, with three-fifths of this sample reporting having experienced some form of mental illness or psychiatric distress in the 30 days prior to incarceration. Cocaine was the most prevalent illicit drug used, reported by nearly half of the sample. Similarly, one quarter of the sample reported active opioid use at the time of incarceration. The disturbingly high use of heroin and cocaine among this population of HIV-infected jail detainees highlights the importance of screening and initiating treatment for these conditions upon entry into jail. This is particularly salient because active drug use has been associated with a number of negative adverse consequences related to HIV treatment outcomes, including access to HIV care, retention in HIV care, access to and adherence with ART.15,18 One of the most significant findings in our study is that pre-incarceration heroin and cocaine use are associated with relapse after release. This supports the notion that SUDs are chronic and relapsing conditions and that in absence of treatment during incarceration, patients are highly vulnerable to relapse post-release. Left untreated, HIV-infected patients in jail settings with SUDs are vulnerable to relapse, re-incarceration, and the same negative HIV treatment outcomes experienced at the time of imprisonment.15,18
The finding that initial receipt of substance abuse treatment itself did not decrease the likelihood of opioid or cocaine use six months post-release is of concern. Although other studies have shown that evidence-based interventions such as MAT provided after release is effective, 35,36 it is unclear whether evidence-based interventions were deployed in EnhanceLink, nor is it known if study participants remained engaged in treatment. Hence, it is likely that our measurement was insufficient to explain the quality or the retention in the intervention, which has been demonstrated in other post-release studies.35 Unfortunately, evidence-based SAT provided in criminal justice settings is limited, and when provided in jail settings, typically is comprised of supervised withdrawal (“detox”) and without provision of aftercare services.37 Similarly, medication-assisted therapies such as methadone or buprenorphine used for treating opioid dependence37,38 or extended released naltrexone used for alocohol or opioid dependence39 is rarely provided in either jail or prison settings in the U.S. or available upon release unless the patient relapses. Thus, even though our conceptual model suggests that SAT would be an enabling resource, it is unlikely to serve in this capacity due to quality or duration of the post-release intervention. Recent data suggest that even in the presence of an evidence-based treatment like buprenorphine for the treatment of opioid dependence, it is retention in treatment that has the highest correlation with HIV treatment outcomes.35,40
With respect to the application of Vulnerable Populations Behavioral Model for Healthcare Utilization (Figure 2) in explaining substance abuse outcomes, a key predisposing factor was homelessness. According to Maslow’s Hierarchy of Needs, basic needs such as food and housing far outweigh secondary needs such as healthcare management.41 Thus, an individual’s ability to access medical care to manage their HIV status or SUDs is contingent on being able to first address food and housing issues.42,43 In a previous study of released PLWHA detainees, homelessness and food insecurity were shown to decrease the likelihood of managing access to HIV care and antiretroviral treatment outcomes.21 It may be that in the larger scheme of things, PLWHA suffering from SUDs do not prioritize SATs in view of their unstable social and environmental conditions. Using a “Housing First” approach or even initiating evidence-based substance abuse treatment and continuing it upon release to the community, is an appropriate way to deal with individuals grappling with a host of co-morbid conditions in addition to their HIV status.
The only factor associated with a decrease in post-release cocaine use was having health insurance. Since insurance has been shown to have a positive influence in ART adherence and better healthcare management,21 it may also be that it provides PLWHA with a sense of security, thereby allowing them to effectively manage their health, including seeking substance abuse treatments. Moreover, having health insurance is often a pre-requisite to entering or even continuing substance abuse treatment. Despite the obvious importance of this enabling resource especially for a population with a high prevalence of substance abuse and mental disorders, federal and state medical entitlements are actually discontinued upon incarceration and it is often a challenge to reinstate these benefits before a person relapses to drug use.10 Correcting such deficiencies in healthcare coverage along with providing housing stability may be the first concrete step in conquering substance abuse and achieving positive HIV health outcomes. The extent to which the Affordable Care Act will address this limitation in the current healthcare environment is not yet known. In fact, this study has demonstrated that those experiencing homelessness and lack of insurance coverage are significantly more likely to drop out of treatment programs and thereby are unable to benefit from post-release SATs, mental health counseling and other supplementary services.
Central to this study is the finding that both pre-incarceration cocaine and opioid use, in addition to the severity of SUDs, was significantly associated with post-release drug relapse. Specifically, those who had used cocaine and opioids before incarceration and had severe drug and alcohol addictions were most likely to continue abusing these substances six months after release. Although this finding is in consensus with other studies in the literature that support the chronic disease model with high rates of relapse among PLWHA, especially those with co-morbidities such as mental illness and SUDs; 16,17 the sheer magnitude of the effect in this study − 32-fold in the case of opioid use – strongly supports identification and treatment at the point of entry to jail. Recent data from a quality improvement program at Rikers Island’s Project KEEP supports the use of higher levels of methadone in order to improve linkage to care upon release from jail.44 Despite the value of evidence-based SATs, it seems that the most vulnerable subset of our sample – those suffering from chronic SUDs, mental illness, and homelessness – either dropped out or were unable to reap the benefits of post-release substance abuse therapies. This suggests that resources may be best used to target those who are most susceptible to relapse, especially in resource-constrained settings such as jails.
This study has addressed a unique space in the re-entry literature – PLWHA transitioning through jail settings. Jails offer an opportune setting for implementing transitional healthcare programs since most inmates eventually re-enter communities rather than transition to prisons.4,5,9 Utilizing jails as a setting to identify, diagnose and treat infectious diseases22 has potential health benefits for incarcerated individuals as well as the community.45 Very few re-entry studies have been examined in jail settings.23,46 This study extends important findings about prison-based community re-entry programs to the context of jails, and is thus well-poised to make a significant contribution by demonstrating the importance of health intervention and adherence programs for PLWHA transitioning from jail to the community. Such programs that target PLWHA in jails could ultimately have a profound impact on HIV treatment and curtail transmission in the community.
This study is the first comprehensive analysis of substance abuse outcomes following the receipt of SAT, HIV medical care and other ancillary services, as part of the EnhanceLink program to transition PLWHA from the jail setting into the community. In order to maximize the positive impact of post-release interventions for incarcerated PLWHA with varied co-morbid condiitons, it is essential to develop and implement programs that can integrate substance abuse and mental health treatments. For the most vulnerable individuals – those facing multiple social, medical and environmental barriers, the answer to achieving positive health outcomes could lie in a multi-pronged or integrated high-impact intervention47 utilizing substance abuse treatment, mental health counseling, housing assistance and social service programs.
Limitations
Despite the important findings obtained from this study, there are a few limitations. Although the study was longitudinal in nature, measurements of substance use and mental illness were measured only periodically and specifically after six months post-release. The reliance on self-reports for a majority of behavioral and healthcare utilization measures may have limited the scope of findings. As such, we can only make correlations and not determine causality. Self-reports have been shown to be a useful method of data collection; however, in the context of this study, the time delay between actual behavior and interview may have introduced potential recall bias.
The most pressing limitation in the analysis was subject attrition. By the six-month post-release interview, there were no data for more than 40% of the sample. Some of the reasons for losses to follow-up across the sites are described in the Appendix. After comparing the retained and non-retained study participants, not surprisingly those not retained were significantly more likely to be socially vulnerable, with increased likelihood of being homeless and uninsured. Fortunately, however, the substance use characteristics, including the two dependent variables were no different at baseline, thereby minimizing the influence of not including them in the analysis. Given that those for whom we did not have data were more likely to be homeless and uninsured, both of which are associated with worse substance use outcomes, our findings likely “underestimate” the true influence of pre-incarceration drug use and drug use severity on the outcomes here. For that reason, the independent variables used are likely to remain the same, yet the magnitude is likely to be greater. Despite these limitations, this study provides important insights into addressing substance use disorders among PLWHA entering jail and emphasizes the importance of incorporating evidence-based interventions that are both appropriate and feasible in jail populations.
Conclusion
PLWHA who enter jails have an extraordinary burden of SUDs, not only in terms of magnitude, but also in severity. Effective substance abuse treatments can have a positive impact on adherence to ART for incarcerated HIV patients; hence it is crucial that future healthcare initiatives take this need into consideration before adopting new treatment strategies. Despite the urgent need for active substance abuse treatment as a supplement to ART for HIV-infected incarcerated drug users, jails often do not adopt this strategy.36,38 It is time to address the culture that ignores the chronic and relapsing nature of drug dependence and focuses on a continuous model of care that comprehensively addresses the multiple co-morbidities of PLWHA who transition through the criminal justice system. An integrated mixed approach to HIV care needs to be implemented, one that potentially includes federal housing and insurance programs, evidence-based substance abuse treatments and continued community supported adherence programs.
Acknowledgments
Funding for this study was possible through the Enhancing Linkages to HIV Primary Care Services Initiative – an HRSA-funded Special Project of National Significance, and through career development awards from the National Institute on Drug Abuse for Drs. Altice (K24 DA017072) and Springer (K02 DA032322, SAS). The authors would like to acknowledge the data management support provided by Maua Herme and administrative support provided by Paula Dellamura. The authors would especially like to thank the study participants for their time and involvement in this project, and the countless research assistants for their hard work and dedication in collecting, collating, entering and cleaning the data.
References
- 1.Sabol WJ, Minton TD. Jail inmates at midyear 2007. Washington, DC: 2008. [Google Scholar]
- 2.West H, Sabol W. Prisoners in 2007. 2008 [Google Scholar]
- 3.Warren J, Gelb A, Horowitz J, Riordan J. One in 100: Behind Bars in America 2008. Washington, D.C.: The Pew Charitable Trusts, Public Safety Performance Project; 2008. [Google Scholar]
- 4.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: Declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92(11):1789–1794. doi: 10.2105/ajph.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fazel S, Baillargeon J. The health of prisoners. Lancet. 2011;377:956–965. doi: 10.1016/S0140-6736(10)61053-7. [DOI] [PubMed] [Google Scholar]
- 7.Schwarcz SK, Hsu LC, Vittinghoff E, Vu A, Bamberger JD, Katz MH. Impact of housing on the survival of persons with AIDS. BMC Public Health. 2009;9:220. doi: 10.1186/1471-2458-9-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams BA, McGuire J, Lindsay RG, et al. Coming home: Health status and homelessness risk of older pre-release prisoners. J Gen Intern Med. 2010;25(10):1038–1044. doi: 10.1007/s11606-010-1416-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications of adequate transitional care for HIV-infected Prisoners: Five essential components. Clin Infect Dis. 2011;53(5):469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baillargeon J, Giordano TP, Rich JD, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–857. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38(12):1754–1760. doi: 10.1086/421392. [DOI] [PubMed] [Google Scholar]
- 12.Stephenson BL, Wohl DA, Golin CE, Tien HC, Stewart P, Kaplan AH. Effect of release from prison and re-incarceration on the viral loads of HIV-infected individuals. Public Health Rep. 2005;120(1):84–88. doi: 10.1177/003335490512000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stephenson BL, Wohl DA, McKaig R, et al. Sexual behaviours of HIV-seropositive men and women following release from prison. Int J STD AIDS. 2006;17(2):103–108. doi: 10.1258/095646206775455775. [DOI] [PubMed] [Google Scholar]
- 14.MacGowan RJ, Margolis A, Gaiter J, et al. Predictors of risky sex of young men after release from prison. Int J STD AIDS. 2003;14(8):519–523. doi: 10.1258/095646203767869110. [DOI] [PubMed] [Google Scholar]
- 15.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–387. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucas GM, Cheever LW, Chaisson RE, Moore RD. Detrimental effects of continued illicit drug use on the treatment of HIV-1 infection. J Acquir Immune Defic Syndr. 2001;27(3):251–259. doi: 10.1097/00126334-200107010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Arnsten JH, Demas PA, Grant RW, et al. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. J Gen Intern Med. 2002;17(5):377–381. doi: 10.1046/j.1525-1497.2002.10644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gonzalez A, Barinas J, O’Cleirigh C. Substance use: Impact on adherence and HIV medical treatment. Curr HIV/AIDS Rep. 2011;8(4):223–234. doi: 10.1007/s11904-011-0093-5. [DOI] [PubMed] [Google Scholar]
- 19.Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: Results at 12 months postrelease. J Subst Abuse Treat. 2009;37(3):277–285. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Braithwaite RL, Arriola KR. Male prisoners and HIV prevention: A call for action ignored. Am J Public Health. 2003;93(5):759–763. doi: 10.2105/ajph.93.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen NE, Meyer JP, Avery AK, et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2011 doi: 10.1007/s10461-011-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flanigan TP, Zaller N, Beckwith CG, et al. Testing for HIV, sexually transmitted infections, and viral hepatitis in jails: Still a missed opportunity for public health and HIV prevention. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S78–83. doi: 10.1097/QAI.0b013e3181fbc94f. [DOI] [PubMed] [Google Scholar]
- 23.de Voux A, Spaulding AC, Beckwith C, et al. Early identification of HIV: Empirical support for jail-based screening. PLos ONE. 2012;7(5) doi: 10.1371/journal.pone.0037603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White MC, Tulsky JP, Estes M, Jamison R, Long HL. Health and health behaviors in HIV-infected jail inmates, 1999 and 2005. AIDS Patient Care STDS. 2008;22(3):221–231. doi: 10.1089/apc.2007.0043. [DOI] [PubMed] [Google Scholar]
- 25.Draine J, Ahuja D, Altice FL, et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. AIDS Care. 2011;23(3):366–377. doi: 10.1080/09540121.2010.507738. [DOI] [PubMed] [Google Scholar]
- 26.Althoff A, Zelenev A, Meyer JP, et al. Correlates of retention in HIV care after release from jail: Results from a multi-site study. AIDS Behav. 2012 doi: 10.1007/s10461-012-0372-1. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.ADAM II: Arrestee Drug Abuse Monitoring Program II 2010 Annual Report. Washington, D.C.: Office of National Drug Control Policy, Executive Office of the President; May, 2010. [Google Scholar]
- 28.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 29.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: Application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 30.McLellan AT, Kushner H, Metzger D, et al. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):14. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 31.Rikoon SH, Cacciola JS, Carise D, Alterman AI, McLellan AT. Predicting DSM-IV dependence diagnoses from Addiction Severity Index composite scores. J Subst Abuse Treat. 2006;31(1):17–24. doi: 10.1016/j.jsat.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Calsyn DA, Saxon AJ, Bush KR, et al. The Addiction Severity Index medical and psychiatric composite scores measure similar domains as the SF-36 in substance-dependent veterans: Concurrent and discriminant validity. Drug Alcohol Depend. 2004;76(2):165–171. doi: 10.1016/j.drugalcdep.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 33.McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The Addiction Severity Index at 25: Origins, contributions and transitions. American Journal of Addiction. 2006;15(2):11. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- 34.James JD. Profile of jail inmates, 2002. U S Department of Justice; Washington, DC: 2004. [Google Scholar]
- 35.Springer SA, Qiu J, Saber-Tehrani AS, Altice FL. Retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS One. 2012;7(5) doi: 10.1371/journal.pone.0038335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Springer SA, Chen S, Altice FL. Improved HIV and substance abuse treatment outcomes for released HIV-infected prisoners: The impact of buprenorphine treatment. J Urban Health. 2010;87(4):592–602. doi: 10.1007/s11524-010-9438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Friedmann PD, Hoskinson R, Gordon M, et al. Medication-assisted treatment in criminal justice agencies affiliated with the criminal justice-drug abuse treatment studies (CJ-DATS): availability, barriers, and intentions. Subst Abus. 2012;33(1):9–18. doi: 10.1080/08897077.2011.611460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in US prison systems: Results from a nationwide survey. Drug Alcohol Depend. 2009;105(1-2):83–88. doi: 10.1016/j.drugalcdep.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2011;112(3):15. doi: 10.1016/j.drugalcdep.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Altice FL, Bruce RD, Lucas GM, et al. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: Results from a multisite study. J Acquir Immune Defic Syndr. 2011;56(Suppl 1):S22–32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maslow AH. Toward a Pschology of Being. Third Edition. New York, NY: John Wiley and Sons, Inc.; 1998. [Google Scholar]
- 42.Wolitski RJ, Kidder DP, Pals SL, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503. doi: 10.1007/s10461-009-9643-x. [DOI] [PubMed] [Google Scholar]
- 43.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harris A, Selling D, Luther C, et al. Rate of community methadone treatment reporting at jail reentry following a methadone increased dose quality improvement effort. Subst Abus. 2012;33(1):70–75. doi: 10.1080/08897077.2011.620479. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control. HIV Testing Implementation Guidance: Correctional Settings. 2009 [Google Scholar]
- 46.Spaulding AC, Thomas DL. Screening for HCV infection in jails. JAMA. 2012;307(12):1259–1260. doi: 10.1001/jama.2012.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mermin J, Fenton KA. The future of HIV prevention in the United States. JAMA. 2012;308(4):347–348. doi: 10.1001/jama.2012.8693. [DOI] [PubMed] [Google Scholar]


