Introduction
In 2009, when it appeared likely that binge eating disorder (BED) would be recommended for inclusion as an official diagnosis in the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a number of researchers believed that it was important to initiate planning for the next generation of research. At the time, it had been established that BED is associated with significant impairment. The robust relationship between BED and obesity prompted researchers in many fields such as eating disorders, addictions, pediatrics, cardiology, and health disparities, to investigate disinhibited eating. Although a large body of research was generated, the researchers in these varied fields were working largely independently.
To enhance communication and collaboration across fields, we received a grant from the National Institute of Mental Health to conduct a workshop in April, 2012 entitled, “Binge Eating Disorder: The Next Generation of Research”. Investigators, representatives from the National Institutes of Health (NIH), clinicians, and lay advocates in the fields of eating disorders, obesity, and addictions were in attendance. Participants are listed in Table 1 and presentation slides are in Appendix 1. The goal of the workshop was to promote lively and forward-thinking discussions to outline future steps for BED research. This document represents a summary of the proceedings from the workshop.
Table 1.
Workshop Agenda and Participants
| Session | Role | Participant | Title/Affiliation |
|---|---|---|---|
| Why BED will be in DSM 5 | Speaker | Ruth H. Striegel, PhD, FAED* | Professor of Psychology Walter A. Crowell University Professor of the Social Sciences Wesleyan University |
| Lifespan: Risk Factors | Speaker | Marian Tanofsky-Kraff, PhD, FAED* | Associate Professor, Department of Medical & Clinical Psychology Uniformed Services University of the Health Sciences Researcher, Section on Growth & Obesity, Eunice Kennedy Shriver National Institute of Child Health & Human Development NIH |
| Speaker | Cynthia M. Bulik, PhD* | Distinguished Professor of Eating Disorders Department of Psychiatry, School of Medicine Professor of Nutrition, Gillings School of Global Public Health Director, University of North Carolina Eating Disorders Program |
|
| Moderator | Marsha D. Marcus, PhD* | Professor of Psychiatry & Psychology University of Pittsburgh School of Medicine Chief, Behavioral Medicine Program Western Psychiatric Institute & Clinic |
|
| Discussant | Lynne Haverkos, MD, MPH | Director, Pediatric Clinical Obesity Program National Institute of Diabetes & Digestive & Kidney Diseases, NIH, DHHS |
|
| Discussant | Julia L. Zehr, PhD | Program Officer, Developmental Trajectories of Mental Disorders Branch Division of Developmental Translational Research National Institute of Mental Health, NIH, DHHS |
|
| Phenotype | |||
| Assessment | Speaker | B. Timothy Walsh, MD | Ruane Professor of Pediatric Psychopharmacology College of Physicians & Surgeons, Columbia University Director, Division of Clinical Therapeutics New York State Psychiatric Institute |
| Comorbidity & Consequences | Speaker | Stephen A. Wonderlich, PhD* | Chester Fritz Distinguished Professor Associate Chairman, Department of Clinical Neuroscience University of North Dakota School of Medicine & Health Sciences Director of Clinical Research, Neuropsychiatric Research Institute |
| Research Domain Criteria (RDoC) | Speaker | Marsha D. Marcus, PhD* | Professor of Psychiatry & Psychology University of Pittsburgh School of Medicine Chief, Behavioral Medicine Program Western Psychiatric Institute & Clinic |
| Moderator | Cynthia M. Bulik, PhD* | Distinguished Professor of Eating Disorders Department of Psychiatry, School of Medicine Professor of Nutrition, Gillings School of Global Public Health Director, University of North Carolina Eating Disorders Program |
|
| Discussant | Bruce Cuthbert, PhD | Director, Division of Adult Translational Research National Institute of Mental Health, NIH, DHHS |
|
| Addictive Processes & Pathophysiology | |||
| Relationship of Addictions to Obesity | Speaker | Nora D. Volkow, MD | Director, National Institute on Drug Abuse Chief, Laboratory of Neuroimaging National Institute on Alcohol Abuse & Alcoholism |
| Addictive Processes | Speaker | Warren K. Bickel, PhD | Director, Addiction Recovery Research Center Virginia Tech Carilion Research Institute Professor of Psychology, Virginia Tech |
| Moderator | James I. Hudson, MD, ScD* | Professor of Psychiatry, Harvard Medical School Director, Psychiatric Epidemiology Research Program Director, Biological Psychiatry Laboratory, McLean Hospital |
|
| Discussant | James M. Bjork, PhD | Program Official, Clinical Neuroscience Branch Division of Clinical Neuroscience & Behavioral Research National Institute on Drug Abuse, NIH, DHHS |
|
| Discussant | Steven Grant, PhD | Chief, Clinical Neuroscience Branch Division of Clinical Neuroscience & Behavioral Research National Institute on Drug Abuse, NIH, DHHS |
|
| Obesity & Broader Medical Relevance | |||
| Obesity | Speaker | David S. Ludwig, MD, PhD | The John F. Crigler, Jr. & Mary A.S. Crigler Chair in Pediatric Endocrinology Director, New Balance Foundation Obesity Prevention Center Director, Optimal Weight for Life (OWL) Clinic Children’s Hospital Boston Professor of Pediatrics, Harvard Medical School Professor of Nutrition, Harvard School of Public Health |
| Consequences | Speaker | Alison E. Field, ScD | Associate Professor of Pediatrics, Harvard Medical School Associate Professor in the Department of Epidemiology Harvard School of Public Health Associate in Medicine, Children’s Hospital Boston |
| Basic/Animal | Speaker | Mary M. Boggiano, PhD | Associate Professor, Department of Psychology Behavioral Neuroscience Division, University of Alabama at Birmingham |
| Moderator | Stephen A. Wonderlich, PhD* | Chester Fritz Distinguished Professor Associate Chairman, Department of Clinical Neuroscience University of North Dakota School of Medicine & Health Sciences Director of Clinical Research, Neuropsychiatric Research Institute |
|
| Discussant | Mary E. Evans, PhD | Program Director Special Projects in Nutrition, Obesity, & Digestive Diseases Division of Digestive Diseases & Nutrition National Institute of Diabetes & Digestive & Kidney Diseases NIH, DHHS |
|
| Discussant | Marjorie A. Garvey MB, BCh | Program Officer Neurobehavioral Mechanisms of Mental Disorders Branch, Division of Developmental & Translational Research National Institutes of Mental Health, NIH, DHHS |
|
| Interventions | |||
| Psychological | Speaker | Denise E. Wilfley, PhD* | Professor of Psychiatry, Pediatrics, Medicine & Psychology Washington University in St. Louis |
| Pharmacological | Speaker | James I. Hudson, MD, ScD* | Professor of Psychiatry, Harvard Medical School Director, Psychiatric Epidemiology Research Program Director, Biological Psychiatry Laboratory, McLean Hospital |
| Surgical | Speaker | James E. Mitchell, MD | Christoferson Professor & Chair, Department of Clinical Neuroscience Chester Fritz Distinguished University Professor University of North Dakota School of Medicine & Health Sciences President & Scientific Director, Neuropsychiatric Research Institute Vice President for Research, Sanford Health System, Fargo |
| Moderator | Ruth H. Striegel, PhD, FAED* | Professor of Psychology Walter A. Crowell University Professor of the Social Sciences Wesleyan University |
|
| Discussant | Mark Chavez, PhD | Program Chief, Eating Disorders Program Program Chief, Side Effects of Experimental Therapeutics Program Associate Director, Research Training & Career Development Program Division of Adult Translational Research & Treatment Development National Institute of Mental Health, NIH, DHHS |
|
| Discussant | Mary Horlick, MD | Director, Pediatric Clinical Obesity Program National Institute of Diabetes & Digestive & Kidney Diseases NIH, DHHS |
|
| Special Topics | |||
| Relevance to Military Health & Readiness | Speaker | Anne C. Dobmeyer, Ph.D., ABPP | Department of Defense Program Manager Internal Behavioral Health Consultation President-Elect, American Board of Clinical Health Psychology |
| Personal & Societal Cost | Speaker | Chevese Turner | Founder & Chief Executive Officer, Binge Eating Disorder Association |
| Moderator | Marian Tanofsky-Kraff, PhD, FAED* | Associate Professor, Department of Medical & Clinical Psychology Uniformed Services University of the Health Sciences Researcher Section on Growth & Obesity, Eunice Kennedy Shriver National Institute of Child Health & Human Development, NIH |
|
| Discussant | Christine M. Hunter, PhD, ABPP | Commander, United States Public Health Service Director of Behavioral Research Division of Diabetes, Endocrinology, & Metabolic Diseases National Institute of Diabetes & Digestive & Kidney Diseases NIH, DHHS |
Note. Served on Workshop Planning Committee
Why BED will be in DSM-5
State of Current Knowledge
In 1994, BED was introduced into the DSM-IV as a provisional set of criteria describing a syndrome characterized by recurrent episodes of binge eating in the absence of the inappropriate compensatory behaviors that define bulimia nervosa. Its inclusion paved the way for a plethora of studies exploring the epidemiology, etiology, clinical presentation, course and treatment of BED. One of the goals of the DSM-5 Eating Disorders Task Force was to determine, based on these data, whether BED should remain in the DSM and, if so, whether the criteria should be preserved or modified. In doing so, the Task Force considered three guiding principles. First, the DSM should be of maximum clinical utility. Therefore, changes should improve clinicians’ ability to help clients encountered in their daily practice. Second, changes should be based on scientific evidence. Third, care should be taken to preserve continuity from DSM-IV to DSM-5 without conflicting with the former two principles.
Presently, the largest obstacle to optimal clinical utility of the DSM-IV is that a majority of individuals who seek treatment for an eating disorder do not meet diagnostic criteria for anorexia nervosa or bulimia nervosa. Rather, their clinical symptoms best fit a diagnosis of eating disorder not otherwise specified (EDNOS). As a result, EDNOS includes a heterogeneous group of symptom constellations and represents the largest eating disorder category. This limits the clinical utility of the diagnosis of EDNOS in that the prognosis implied by, or the treatments effective for, one form of EDNOS (e.g., subthreshold anorexia nervosa) may differ quite markedly from another (e.g., BED). Moreover, although EDNOS is supposed to represent a full-syndrome psychiatric disorder, some presentations included under EDNOS are subthreshold variants of anorexia nervosa or bulimia nervosa and thus may contribute to the sense that EDNOS conditions are “lesser” problems. Indeed, some insurance companies will not pay for services associated with treating EDNOS.
Several factors led to BED being separated out from EDNOS and becoming a candidate for an independent diagnosis. First, individuals with a diagnosis of BED comprise a large percentage of those receiving an EDNOS diagnosis in clinical settings. Second, BED criteria can be reliably applied to clinical cases. Third, individuals with BED differ on meaningful clinical indicators from individuals without BED and from individuals with conditions that share some clinical features such as bulimia nervosa or obesity. Fourth, effective treatments are available for BED. On the basis of these four observations, including BED as an official diagnosis in DSM-5 is in concert with the first two guiding principles for DSM-5. Its inclusion in DSM-5 as a distinct diagnostic entity would reduce the large EDNOS category without creating a substantial number of new psychiatric cases. With regard to the third principle (i.e., continuity between DSM-IV and 5), the Task Force suggested that only the frequency criterion (D) be modified such that binge eating occurs, on average, at least once a week for 3 months. This minor modification represents a change from BED in DSM-IV, but makes the binge eating frequency criterion BED consistent with the binge eating frequency criterion of bulimia nervosa.
Future Directions of the Task Force
Along with the recommendation to “upgrade” BED to an official diagnosis in the DSM-5, the Eating Disorders Task Force suggested areas for future research. Because the following sections will describe future directions in more detail, only three are briefly mentioned herewith. The next generation of research should consider developmental aspects of BED. For example, defining and measuring binge eating poses a challenge in children since the overeating criterion of a binge episode may be limited by parental restrictions and evaluating a large amount of food may be beyond children’s cognitive capacities. In line with this example, another proposed area for research involves elucidating whether loss of control is a more critical component than overeating in adult binge eating episodes and whether both elements are necessary. Lastly, further exploration is required to determine whether the BED duration criterion of 3 months is unduly restrictive.
Key References
- 1.Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40:337–348. doi: 10.1002/eat.20370. [DOI] [PubMed] [Google Scholar]
- 2.Marcus MD, Wildes JE. Obesity: is it a mental disorder? Int J Eat Disord. 2009;42:739–753. doi: 10.1002/eat.20725. [DOI] [PubMed] [Google Scholar]
- 3.Russell G. Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med. 1979;9:429–448. doi: 10.1017/s0033291700031974. [DOI] [PubMed] [Google Scholar]
- 4.Striegel-Moore RH, Franko DL. Should binge eating disorder be included in the DSM-V? A critical review of the state of evidence. Annual Rev Clin Psychol. 2008;4:305–324. doi: 10.1146/annurev.clinpsy.4.022007.141149. [DOI] [PubMed] [Google Scholar]
- 5.Striegel RH, Bedrosian R, Wang C, Schwartz S. Why men should be included in research on binge eating: Results from a comparison of psychosocial impairment in men and women. Int J Eat Disord. 2012;45:233–240. doi: 10.1002/eat.20962. [DOI] [PubMed] [Google Scholar]
- 6.Stunkard AJ, Grace WJ, Wolff HG. The night-eating syndrome; a pattern of food intake among certain obese patients. Am J Med. 1955;19:78–86. doi: 10.1016/0002-9343(55)90276-x. [DOI] [PubMed] [Google Scholar]
- 7.Walsh BT, Sysko R. Broad categories for the diagnosis of eating disorders (BCD-ED): An alternative system for classification. Int J Eat Disord. 2009;42:754–764. doi: 10.1002/eat.20722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engel SG. The validity and clinical utility of binge eating disorder. Int J Eat Disord. 2009;42:687–705. doi: 10.1002/eat.20719. [DOI] [PubMed] [Google Scholar]
Lifespan: Risk Factors
State of Current Knowledge
BED typically manifests in adolescence or adulthood. However, retrospective data from adult samples and prospective studies in young children suggest that risk for BED may be present well before the manifestation of the disorder or even symptoms of the disorder. For example adult studies show that the heritability of BED is approximately 50%. Moreover, retrospective studies of adults have found self-reported childhood risk factors for BED. Specifically, child obesity, maltreatment including teasing and bullying, as well as perceived stress are risk factors for the disorder.
Although development of the full syndrome of BED is uncommon in childhood, episodes of loss of control eating (an inability to stop eating or control the amount or type of food consumed) are not infrequently reported by pre-adolescent youth. Paralleling adult BED, children who report loss of control eating have excess adiposity and endorse greater eating disordered attitudes and depressive symptoms than children without such episodes. Loss of control eating prior to adolescence appears to confer risk for development of excess weight and fat gain, metabolic syndrome components and most notably, partial or full-syndrome BED. Risk factors for loss of control eating in childhood may include genetic factors (for example, pediatric loss of control eating is associated with at least one candidate gene, FTO rs9939609 obesity risk alleles, after accounting for the contribution of body weight), and psychosocial factors (such as parental under-involvement and critical comments).
Future Directions
An important area for investigation should be identifying early risk factors for BED and loss of control eating in animal and human models. Proposed prospective designs should involve elucidating the biological, psychological, and social factors influencing the entire family, including examining relevant variables related to mothers and fathers prior to conception and during pregnancy (e.g., parental weight history, paternal age, maternal nutrition during pregnancy). Importantly, the interaction among and between physical and environment variables should be considered. Research focused on developing early interventions is an important next step for BED. Once risk profiles for BED are identified, potential areas for early intervention can be pursued such as perinatal identification; training programs for parents of young children; and family-based interventions during middle childhood and early adolescence.
Key References
- 1.Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: A systematic review of the literature. Int J Eat Disord. 2007;40:293–309. doi: 10.1002/eat.20369. [DOI] [PubMed] [Google Scholar]
- 2.Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: A systematic review of randomized controlled trials. Int J Eat Disord. 2007;40:337–348. doi: 10.1002/eat.20370. [DOI] [PubMed] [Google Scholar]
- 3.Fairburn CG, Doll HA, Welch SL, Hay PJ, Davies BA, O’Connor ME. Risk factors for binge eating disorder: a community-based, case-control study. Arch Gen Psychiatry. 1998;55:425–432. doi: 10.1001/archpsyc.55.5.425. [DOI] [PubMed] [Google Scholar]
- 4.Manwaring JL, Hilbert A, Wilfley DE, et al. Risk factors and patterns of onset in binge eating disorder. Int J Eat Disord. 2006;39:101–107. doi: 10.1002/eat.20208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathes WF, Brownley KA, Mo X, Bulik CM. The biology of binge eating. Appetite. 2009;52:545–553. doi: 10.1016/j.appet.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pike KM, Wilfley D, Hilbert A, Fairburn CG, Dohm FA, Striegel-Moore RH. Antecedent life events of binge-eating disorder. Psychiatry Res. 2006;142:19–29. doi: 10.1016/j.psychres.2005.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Striegel-Moore RH, Dohm FA, Pike KM, Wilfley DE, Fairburn CG. Abuse, bullying, and discrimination as risk factors for binge eating disorder. Am J Psychiatry. 2002;159:1902–1907. doi: 10.1176/appi.ajp.159.11.1902. [DOI] [PubMed] [Google Scholar]
- 8.Striegel-Moore RH, Fairburn CG, Wilfley DE, Pike KM, Dohm FA, Kraemer HC. Toward an understanding of risk factors for binge-eating disorder in black and white women: A community-based case-control study. Psychol Med. 2005;35:907–917. doi: 10.1017/s0033291704003435. [DOI] [PubMed] [Google Scholar]
- 9.Tanofsky-Kraff M, Han JC, Anandalingam K, Shomaker LB, Columbo KM, Wolkoff LE, Kozlosky MS, Elliott C, Ranzenhofer LM, Roza CA, Yanovski SZ, Yanovski JA. The FTO gene rs9939609 obesity risk allele and loss of control over eating. Am J Clin Nutr. 2009;90:1483–8. doi: 10.3945/ajcn.2009.28439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zocca JM, Shomaker LB, Tanofsky-Kraff M, Columbo KM, Raciti GR, Brady SM, Crocker MK, Ali AH, Matheson BE, Yanovski SZ, Yanovski JA. Links between Mothers’ and Children’s Disinhibited Eating and Children’s Adiposity. Appetite. 2011;56:324–31. doi: 10.1016/j.appet.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tanofsky-Kraff M, Yanovski SZ, Yanovski JA. Loss of control over eating in children and adolescents. In: Striegel-Moore R, Wonderlich SA, Walsh BT, Mitchell JE, editors. Developing an Evidence-Based Classification of Eating Disorders: Scientific Findings for DSM-5. American Psychiatric Association Press; 2011. pp. 221–236. [Google Scholar]
- 12.Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high-risk for adult obesity. Int J Eat Disord. 2009;42:26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanofsky-Kraff M, Shomaker LB, Roza CA, Wolkoff LE, Columbo KM, Racite G, Zocca JM, Wilfley DE, Yanovski SZ, Yanovski JA. A Prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol 2011, Int J Eat Disord. 2012;45:751–758. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Assessment
State of Current Knowledge
There are two main levels of assessment that should be considered. The first is at the level of the syndrome and involves, for example, diagnostic criteria in the DSM. The second is at the level of the components of the syndrome, and involves assessment of features such as consumption of a large amount of food, sense of loss of control over eating, behavioral indicators of loss of control, and distress about the eating behavior.
Current methods of assessment can be divided into those using self-report (which includes interviews, diaries, and ecological momentary assessment), and direct observation, such as laboratory meals. The reliability of assessments has been examined at the syndromal level for diagnosis, and also at the component level for amount of food consumed and loss of control. Generally, there is acceptable reliability within a method, but the cross-method reliability (e.g., diary vs. laboratory meals for food consumption during binges) is less clear.
Each method of assessment has advantages and disadvantages. Interviews allow structured questions and the ability to probe, but are time consuming and rely on skill of the interviewer and the reporting ability of the interviewee. Self-report is time efficient, but relies on the interviewee’s understanding of questions and accuracy. Ecological momentary assessment obtains data in real time, but relies on the participant’s cooperation and ability to report accurately. Laboratory meals obtain objective data regarding eating, but the non-naturalistic setting influences behavior and psychological state.
In summary, the diagnosis of BED can be reliably established by interview and self-report, with interview being the consensus method of choice. Different methods of assessment have different advantages and disadvantages, and agreement across methods is variable.
Future Directions
A priority for future research is cross-method validation; for example, comparing the results of different methods used to assess the same construct. Also, there should be more study of the relationship between components; for example, the relationship of loss of control to amount consumed. Furthermore, the contributions of the various components of the syndrome to the overall validity of the syndrome should be investigated; for example, examining the relative contribution to diagnostic validity of loss of control over eating vs. amount of food consumed. Finally, objective measures should be developed to help assess components of the syndrome; for example, using biomarkers of stress in the assessment of distress.
Key References
- 1.Engel SG, Kahler KA, Lystad CM, Crosby RD, Simonich HK, Wonderlich SA, Peterson CB, Mitchell JE. Eating behavior in obese BED, obese non-BED, and non-obese control participants: a naturalistic study. Behav Res Ther. 2009;47:897–900. doi: 10.1016/j.brat.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 2.Grilo CM, Masheb RM, Wilson GT. Different methods for assessing the features of eating disorders in patients with binge eating disorder: A replication. Obes Res. 2001;9:418–22. doi: 10.1038/oby.2001.55. [DOI] [PubMed] [Google Scholar]
- 3.Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. J Consult Clin Psychol. 2001;69:317–22. doi: 10.1037//0022-006x.69.2.317. [DOI] [PubMed] [Google Scholar]
- 4.Walsh BT, Boudreau G. Laboratory studies of binge eating disorder. Int J Eat Disord. 2003;34:S30–8. doi: 10.1002/eat.10203. [DOI] [PubMed] [Google Scholar]
Comorbidity and Consequences
State of Current Knowledge
Individuals with BED experience significant impairment in psychosocial functioning. Compared with obese adults without BED, obese adults with the disorder report lower quality of life in the domains of physical health conditions and mobility, emotional well-being, work, sexual life, public distress, and self-esteem. Individuals with BED also experience impaired functioning in both their social life and at home. Moreover, BED is associated with higher levels of disability and health problems. With regard to comorbid diagnoses, similar percentages of adults with BED experience Axis I psychiatric disorders, such as major depressive disorder, anxiety disorders, and substance use disorders as individuals with anorexia nervosa and bulimia nervosa. BED is also commonly comorbid with impulse control disorders such as ADHD. The most common comorbid Axis II (personality) disorders in individuals with BED are avoidant, borderline, and obsessive-compulsive personality disorders. Despite consistent findings from cross-sectional studies that BED is associated with the co-occurrence of a wide range of disorders, the potential impact of the presence of any of these comorbid disorders on the course or outcome of BED is unclear.
Future Directions
Given the dearth of naturalistic prospective studies on the outcome of BED, an essential next research step involves examining the psychiatric consequences, quality of life, and psychosocial functioning of the individuals with the disorder. Furthermore, since BED often presents with various comorbid disorders, the etiologic, pathophysiologic, and treatment implications of psychopathology-related heterogeneity in BED should be investigated.
Key References
- 1.Rieger E, Wilfley DE, Stein RI, Marino V, Crow SJ. A comparison of quality of life in obese individuals with and without binge eating disorder. Int J Eat Disord. 2005;37:234–40. doi: 10.1002/eat.20101. [DOI] [PubMed] [Google Scholar]
- 2.Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engel SG. The validity and clinical utility of binge eating disorder. Int J Eat Disord. 2009;42:687–705. doi: 10.1002/eat.20719. [DOI] [PubMed] [Google Scholar]
- 3.Striegel-Moore RH, Franko DL. Should binge eating disorder be included in the DSM-V? A critical review of the state of the evidence. Annu Rev Clin Psychol. 2008;4:305–324. doi: 10.1146/annurev.clinpsy.4.022007.141149. [DOI] [PubMed] [Google Scholar]
- 4.Kolotkin RL, Westman EC, Østbye T, Crosby RD, Eisenson HJ, Binks M. Does binge eating disorder impact weight-related quality of life? Obes Res. 2004;12:999–1005. doi: 10.1038/oby.2004.122. [DOI] [PubMed] [Google Scholar]
- 5.Stice R, Agras WS, Telch CF, Halmi KA, Mitchell JE, Wilson T. Subtyping binge eating-disordered women along dieting and negative affect dimensions. Int J Eat Disord. 2001;30:11–27. doi: 10.1002/eat.1050. [DOI] [PubMed] [Google Scholar]
- 6.Grilo CM, Crosby RD, Masheb RM, White MA, Peterson CB, Wonderlich SA, Engel SG, Crow SJ, Mitchell JE. Overvaluation of shape and weight in binge eating disorder, bulimia nervosa, and sub-threshold bulimia nervosa. Behav Res Ther. 2009;47:692–696. doi: 10.1016/j.brat.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yanovski SA, Nelson JE, Dubbert BK, Spitzer EIj. Association of binge eating disorder and psychiatric comorbidity in obese subjects. Am J Psychiatry. 1993;150:1472–1479. doi: 10.1176/ajp.150.10.1472. [DOI] [PubMed] [Google Scholar]
- 8.Wilfley DE, Zolar Dounchis J, Stein RI, Robinson Welch R, Friedman MA, Ball SA. Comorbid psychopathology in binge eating disorder: Relation to eating disorder severity at baseline and following treatment. J Consult Clin Psychol. 2000;68:641–649. [PubMed] [Google Scholar]
- 9.Telch CF, Stice E. Psychiatric comorbidity in women with binge eating disorder: Prevalence rates from a non-treatment-seeking sample. J Consult Clin Psychol. 1998;66:768–776. doi: 10.1037//0022-006x.66.5.768. [DOI] [PubMed] [Google Scholar]
- 10.Grilo CM, White MA, Masheb RM. DSM-IV psychiatric disorder comorbidity and its correlates in binge eating disorder. Int J Eat Disord. 2009;42:228–234. doi: 10.1002/eat.20599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
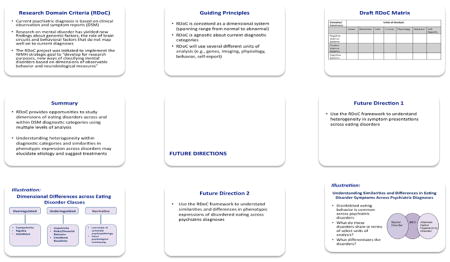
Research Domain Criteria (RDoC)
State of Current Knowledge
At present, psychiatric nosology is based on clinical observation and symptom reports, as exemplified by the Diagnostic and Statistical Manual of the American Psychiatric Association and the International Classification of Diseases. However, new data from neuroscience research on genetic factors, brain circuit abnormalities, and behavioral factors do not map well onto current diagnoses. Thus, the Research Domain Criteria (RDoC) project was initiated to implement the NIMH strategic goal to “develop for research purposes, new ways of classifying mental disorders based on dimensions of observable behavior and neurobiological measures.” There are a number of guiding principles of RDoC. First, RDoC is conceived as a dimensional system, spanning from normal to abnormal. RDoC is agnostic with regard to current diagnostic categories. Thus, the approach involves identifying relevant neurobiological dimensions and linking them to salient clinical phenomena rather than starting with current DSM diagnostic categories. In addition, RDoC proposes the use of multiple units of analysis to assess the validity of the dimensional constructs. Specifically, genes, molecules, cells, circuits, physiology, behavior, and self-reports may be utilized to elucidate the psychopathological phenomena. Thus, RDoC provides a novel heuristic to guide the examination of salient domains and constructs that underlie different eating disorder diagnoses as well as other forms of psychopathology. This approach has promise to promote understanding of the heterogeneity within diagnostic categories (e.g., BED) and similarities in phenotypic expression across disorders.
Future Directions
Although RDoC is a work in progress, this framework may prove useful in elucidating the heterogeneity in symptom presentations within BED and the other eating disorders. RDoC also may hold promise for understanding phenotypic similarities and distinctions among eating disorders and other diagnoses in which binge eating is common (e.g., bipolar disorder and attention deficit hyperactivity disorder).
Key References
- 1.http://www.nimh.nih.gov/research-funding/rdoc/nimh-research-domain-criteria-rdoc.shtml
- 2.Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, Wang PS, Cuthbert BN. Developing constructs for psychopathology research: Research domain criteria. J Abnorm Psychol. 2010;119:631–9. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- 3.Wildes JE, Marcus MD, Crosby RD, Ringham RM, Marin Dapelo M, Gaskill JA, Forbush KT. The clinical utility of personality subtypes in patients with anorexia nervosa. J Consult Clin Psychol. 2011;79:665–674. doi: 10.1037/a0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wonderlich SA, Crosby RD, Joiner T, Peterson CB, Bardone-Cone A, Klein M, Crow S, Mitchell JE, le Grange D, Steiger H, Kolden G, Johnson F, Vrshek S. Personality subtyping and bulimia nervosa: Psychopathological and genetic correlates. Psychol Med. 2005;305:649–657. doi: 10.1017/s0033291704004234. [DOI] [PubMed] [Google Scholar]
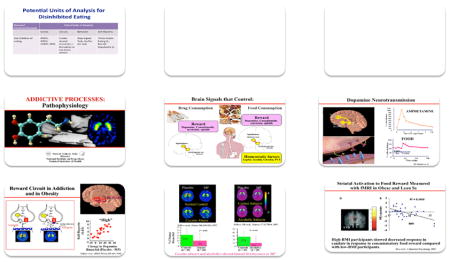
Relationship of Addictions to Obesity
State of Current Knowledge
Similar brain mechanisms may underlie drug addiction and obesity. Brain signals that control drug consumption via the reward circuit and dopaminergic neurotransmission also control food consumption. Individuals with cocaine and alcohol abuse show blunted dopamine increase to stimulants, and individuals with high BMI also show decreased response to food reward compared with individuals with low BMI. Dopamine D2 receptors are decreased in addiction and also in obese individuals. These results and similar studies, including pre-clinical studies, suggest common processes in drug addiction and obesity.
A systems model of addiction and of obesity has been proposed. In the healthy individual, the salience of the rewarding substance (drug or food) is normal, and there is normal self-regulation, which leads to appropriate inhibitory control over the drive to consume. In contrast, in an individual whose system is dysregulated, the salience is enhanced (augmented by amplified memory or conditioning) and the self-regulation is weaker, leading to less control over the drive to consume.
Future Directions
The main potential implication of this body of work for BED is that individuals with BED display not only appetite and weight dysregulation but also other forms of dysregulated behavior, including addictions. Therefore, BED, especially when coupled with overweight or obesity, may represent a form of disordered eating and weight dysregulation driven and maintained by similar pathophysiological abnormalities associated with addictions. Further studies should examine the extent to which BED shares neurobiological abnormalities with addictions and whether these abnormalities are more likely to be present in individuals who are obese and have BED than in obese individuals who do not binge eat (see also future directions for addictive processes below).
Key References
- 1.Volkow ND, Wang GJ, Baler RD. Reward, dopamine and the control of food intake: Omplications for obesity. Trends Cognitive Sci. 2011;15:37–46. doi: 10.1016/j.tics.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Volkow ND, Wang GJ, Fowler JS, Tomasi D, Baler R. Food and Drug Reward: Overlapping Circuits in Human Obesity and Addiction. Curr Topics Behav Neurosciences. 2011 doi: 10.1007/7854_2011_169. [DOI] [PubMed] [Google Scholar]
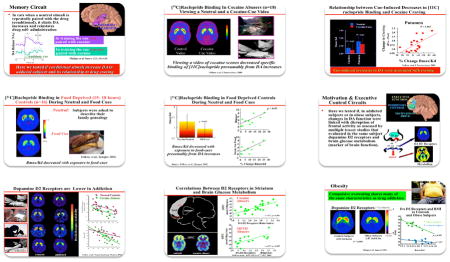
Addictive Processes
State of Current Knowledge
Neuropsychological systems associated with addictions-related processes include the impulsive system and the executive system. The impulsive system is embodied in the limbic and para-limbic brain regions, functions in biological reinforcement, and is most often hyperactive in disease states. The executive system is embodied in the prefrontal cortex, functions in valuation of the future, planning, and remembering of events, and is most often hypoactive in disease states.
Addiction-related processes are relevant to BED in that they may be involved in food reinforcement and loss of control of eating. In terms of food reinforcement, imaging studies have shown that dopamine release is associated with BED (using positron emission tomography), and enhanced reward sensitivity associated with greater activation of the orbitofrontal cortex in BED. Turning to loss of control, studies of executive function, decision-making, or related measures in BED have found impairment in BED compared with non-obese individuals without BED (in all studies), and also compared with individuals with obesity who do not have BED (in most studies).
Future Directions
Future directions for research include examination of the full range of impulsive and executive function categories in BED; comparison of BED with addictive disorders, other eating disorders, and obesity; and investigation of the extent to which BED relates to an underlying addictive process based on neural circuit abnormalities or other endophenotypic abnormalities.
Key References
- 1.Boeka AG, Lokken KL. Prefrontal systems involvement in binge eating. Eat Weight Disord. 2011;16:e121–6. doi: 10.1007/BF03325317. [DOI] [PubMed] [Google Scholar]
- 2.Danner UN, Ouwehand C, van Haastert NL, Hornsveld H, de Ridder DT. Decision-making impairments in women with binge eating disorder in comparison with obese and normal weight women. Eur Eat Disord Rev. 2012;20:e56–62. doi: 10.1002/erv.1098. [DOI] [PubMed] [Google Scholar]
- 3.Davis C, Patte K, Curtis C, Reid C. Immediate pleasures and future consequences. A neuropsychological study of binge eating and obesity. Appetite. 2010;54:208–213. doi: 10.1016/j.appet.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Galioto R, Spitznagel MB, Strain G, Devlin M, Cohen R, Paul R, Crosby RD, Mitchell JE, Gunstad J. Cognitive function in morbidly obese individuals with and without binge eating disorder. Compr Psychiatry. 2011 doi: 10.1016/j.comppsych.2011.09.002. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldfield GS, Adamo KB, Rutherford J, Legg C. Stress and the relative reinforcing value of food in female binge eaters. Physiol Behav. 2008;93:579–87. doi: 10.1016/j.physbeh.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Manwaring JL, Green L, Myerson J, Strube MJ, Wilfley DE. Discounting of various types of rewards by women with and without binge eating disorder: Evidence for general rather than specific differences. Psychol Record. 2011;61:561–582. doi: 10.1007/bf03395777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nasser JA, Evans SM, Geliebter A, Pi-Sunyer FX, Foltin RW. Use of an operant task to estimate food reinforcement in adult humans with and without BED. Obes. 2008;16:1816–20. doi: 10.1038/oby.2008.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raymond NC, Neumeyer B, Warren CS, Lee SS, Peterson CB. Energy intake patterns in obese women with binge eating disorder. Obes Res. 2003;11:869–79. doi: 10.1038/oby.2003.120. [DOI] [PubMed] [Google Scholar]
- 9.Raymond NC, Peterson RE, Bartholome LT, Raatz SK, Jensen MD, Levine JA. Comparisons of Energy Intake and Energy Expenditure in Overweight and Obese Women With and Without Binge Eating Disorder. Obes. 2011 doi: 10.1038/oby.2011.312. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schienle A, Schafer A, Hermann A, Vaitl D. Binge-eating disorder: reward sensitivity and brain activation to images of food. Biol Psychiatry. 2009;65:654–61. doi: 10.1016/j.biopsych.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 11.Svaldi J, Brand M, Tuschen-Caffier B. Decision-making impairments in women with binge eating disorder. Appetite. 2010;54:84–92. doi: 10.1016/j.appet.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Van den Eynde F, Guillaume S, Broadbent H, Stahl D, Campbell IC, Schmidt U, Tchanturia K. Neurocognition in bulimic eating disorders: a systematic review. Acta Psychiatr Scand. 2011;124:120–40. doi: 10.1111/j.1600-0447.2011.01701.x. [DOI] [PubMed] [Google Scholar]
- 13.Wang GJ, Geliebter A, Volkow ND, Telang FW, Logan J, Jayne MC, Galanti K, Selig PA, Han H, Zhu W, Wong CT, Fowler JS. Enhanced striatal dopamine release during food stimulation in binge eating disorder. Obes. 2011;19:1601–8. doi: 10.1038/oby.2011.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Obesity: The relationship of Obesity to Ultra-Processed Energy-Dense Foods
State of Current Knowledge
The current food environment is replete with highly energy-dense, ultra-processed foods served in enormous portion sizes. These food types may promote obesity and associated health comorbidities. Since humans acutely regulate food intake by volume, more so than by calorie content, chronic consumption of highly energy dense foods may increase risk for excess body weight by overeating.
Ultra-processed foods are also low in nutrient and fiber content. Animal data suggest that low intake of micronutrient and phytochemicals may increase energy intake and are associated with increased adiposity. Fiber has been shown to have a modest positive impact on body weight and a major beneficial effect for reducing cardiovascular disease and diabetes. Moreover, a high fiber diet may potentially protect against cancer and reduce mortality.
In addition, ultra-processed foods are often comprised of solid fats, including saturated and trans-fats. Unlike liquid fats that protect against cardiovascular disease, solid fats promote these diseases. Solid fats may also have an impact on body weight. Indeed, trans-fats increase abdominal obesity and insulin resistance in monkeys, while humans fed polyunsaturated experience improved adiposity and adiponectin levels.
Furthermore, the high-intensity flavoring of ultra-processed foods may promote obesity. Sweet, salty and fatty flavors of these foods are enhanced through chemical manipulation. High-intensity flavoring may override endogenous satiety mechanisms and cause naturally sweet foods, such as fruit, to taste bland and unsweet foods, such as vegetables, to taste unpalatable.
Also, ultra-processed foods impact the rate of nutrient digestion and absorption. In contrast to unprocessed foods that are digested slowly and elicit high levels of satiety, highly processed foods are typically digested quickly, likely causing overconsumption. This phenomenon can be described by the glycemic index, a measure of how blood glucose level changes in the postprandial after consumption of carbohydrate-containing foods. A high glycemic index diet is predictive of increased body weight in adults and children.
Taken together, numerous aspects of ultra-processed products may override the biological and behavioral regulators of food intake, causing food consumption to become dysregulated from biological requirements. In susceptible individuals, these stimuli may lead to obesity or disordered eating.
Future Directions
Given data showing that binge and loss of control eating episodes are often comprised of highly palatable, energy-dense foods, an important next research step involves studying the effects of ultra-processed food on BED or loss of control eating. Furthermore, more generally, investigations are needed to elucidate the causal links between BED and obesity.
Key Reference
- 1.Ludwig DS. Technology, diet, and the burden of chronic disease. JAMA. 2011;305:1352–1353. doi: 10.1001/jama.2011.380. [DOI] [PubMed] [Google Scholar]
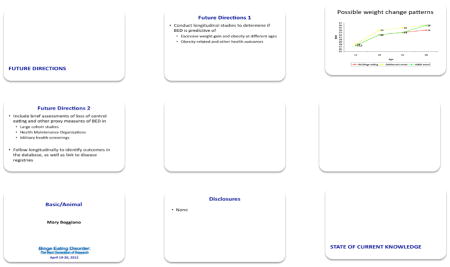
Obesity-Related Consequences
State of Current Knowledge
There is a strong association of BED with obesity in cross-sectional studies. However, there are few longitudinal studies, so that the nature of the causal relationships between BED and obesity is uncertain. Specifically, it is unclear whether BED causes excessive weight gain and obesity. However, among children and adolescents, loss of control of eating predicts subsequent excessive weight gain. In addition, there is some evidence that childhood loss of control eating and adult BED are associated with subsequent development of components of the metabolic syndrome independent of potential mediating effects of obesity.
Future Directions
A major priority for future research is to conduct longitudinal studies to determine if the development of BED or loss of control eating at different ages is predictive of subsequent excessive weight gain and obesity, as well as obesity-related and other health outcomes. To facilitate this goal and to link data on BED and loss of control eating to disease registries, it will be useful to include brief assessments of loss of control eating and other proxy measures of BED in large cohort studies, assessments used by health maintenance organizations, and surveys used in military screening.
Key References
- 1.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117:1203–9. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–58. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skinner HH, Haines J, Austin SB, Field AE. A prospective study of overeating, binge eating, and depressive symptoms among adolescent and young-adult women. J Adolesc Health. 2012;50(5):478–83. doi: 10.1016/j.jadohealth.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Field AE, Corliss HL, Skinner HH, Horton NJ. Loss of control eating as a predictor of weight gain and the development of overweight, depressive symptoms, binge drinking, and substance use. In: Striegel-Moore R, Wonderlich SA, Walsh BT, Mitchell JE, editors. Toward an Evidence-Based Classification of Eating Disorders. Arlington, VA: American Psychiatric Association; 2011. pp. 77–88. [Google Scholar]
- 5.Hudson JI, Lalonde JK, Coit CE, Tsuang MT, McElroy SL, Crow SJ, Bulik CM, Hudson MS, Yanovski JA, Rosenthal NR, Pope HG., Jr Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. Am J Clin Nutr. 2010;91:1568–1573. doi: 10.3945/ajcn.2010.29203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Presnell K, Stice E, Seidel A, Madeley MC. Depression and eating pathology: prospective reciprocal relations in adolescents. Clin Psychol Psychother. 2009;16:357–65. doi: 10.1002/cpp.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tanofsky-Kraff M, Shomaker LB, Stern EA, Miller R, Sebring N, Dellavalle D, Yanovski SZ, Hubbard VS, Yanovski JA. Children’s binge eating and development of metabolic syndrome. Int J Obes. 2012;36:956–62. doi: 10.1038/ijo.2011.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, Treasure J, Solmi F, Horton NJ. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012;130:e289–e295. doi: 10.1542/peds.2011-3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
Animal/Basic
State of Current Knowledge
Animal models of binge eating have been developed in rodents. In these models, rodents are exposed to cyclic caloric restriction and re-feeding to simulate dieting, and are exposed to stress (e.g., foot shock or letting rat see and smell, but not taste, food). The binge eating that appears in animal models has clinical human parallels in that large food intakes are greater than those produced by hunger; persist despite punishment; can be triggered by stress or a single “morsel” of palatable food; and are associated with biomarkers of stress, depression, and anxiety.
The primary physiologic targets investigated in animal models have included stress mechanisms (e.g., corticosterone, brain stress-hormone receptors); reward and craving mechanisms (e.g., dopamine, opioids, glutamate, gamma amino butyric acid); and hunger and satiety mechanisms (serotonin and the melanocortin system).
Different drug types work best on different animal models of BED, depending on the factors used to develop these models. These results suggest that different etiologic factors may affect the brain differently to express binge eating.
Future Directions
A priority for future research is to refine drug testing to develop more targeted and efficacious treatments. Animal models should be used to help identify genetic markers, the biology of BED-relevant gene-environment interactions, and the biology discriminating risk for BED associated with obesity versus BED not associated with obesity.
Key References
- 1.Boggiano MM, Chandler PC, Viana JB, Oswald KD, Maldonado CR, Wauford PK. Combined dieting and stress evoke exaggerated responses to opioids in binge-eating rats. Behav Neurosci. 2005;119:1207–1214. doi: 10.1037/0735-7044.119.5.1207. [DOI] [PubMed] [Google Scholar]
- 2.Boggiano MM, Artiga AI, Pritchett CE, Chandler PC, Smith ML, Eldridge AJ. High intake of palatable food predicts binge-eating characteristics independent of susceptibility to obesity: An animal model of lean vs. obese binge eating and obesity with and without binge-eating. Int J Obes. 2007;31:1357–1367. doi: 10.1038/sj.ijo.0803614. [DOI] [PubMed] [Google Scholar]
- 3.Corwin RL, Avena NM, Boggiano MM. Feeding and reward: Perspectives from three rat models of binge eating. Physiol Behav. 2011;104 doi: 10.1016/j.physbeh.2011.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campbell IC, Mill J, Uher R, Schmidt U. Eating disorders, gene-environment interactions and epigenetics. Neurosci Biobehav Rev. 2011;35:784–793. doi: 10.1016/j.neubiorev.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Cifani C, Polidori C, Melotto S, Ciccocioppo R, Massi MA. Preclinical model of binge eating elicited by yo-yo dieting and stressful exposure to food: Effect of sibutramine, fluoxetine, topiramate, and midazolam. Psychopharmacol. 2009;204:1113–1115. doi: 10.1007/s00213-008-1442-y. [DOI] [PubMed] [Google Scholar]
- 6.Klump KL, Suisman JL, Culbert KM, Kashy DA, Sisk CL. Binge eating proneness emerges during puberty in female rats: A longitudinal study. J Abnorm Psychol. 2011;120:948–55. doi: 10.1037/a0023600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Psychological Treatment
State of Current Knowledge
Psychological treatment for BED targets reducing binge eating, weight, and shape concerns, and preventing excess weight gain and/or inducing modest weight loss. The psychotherapies most evaluated in clinical trials include cognitive-behavioral therapy (CBT), interpersonal psychotherapy (IPT), behavioral weight loss (BWL) and CBT self-help approaches (CBTgsh). CBT is based on the restraint model, which proposes that decreasing dietary restraint will improve attitudes toward eating, weight, and shape, which in turn, will decrease binge eating. IPT proposes that by improving interpersonal functioning and self-esteem, negative affect is decreased and, in turn, binge eating is reduced. CBT and IPT produce marked and long-lasting impact on binge eating and associated psychopathology and lead to modest, long-term weight loss in those who cease binge eating. CBT demonstrates significant specificity of treatment effects compared to medication, supportive psychotherapy, and BWL. As compared to medication, CBT may be especially relevant for those BED patients with overvaluation of shape and weight on the outcomes of depression and associated eating disorder psychopathology. IPT evidences high retention and treatment acceptability, and is superior to CBTgsh for more severely ill patients; for example, those presenting with high frequency of binge eating and compensatory behavior, high weight/shape concern, negative affect, and distress and in patients with low self-esteem. BWL does not specifically target binge eating, but may be more easily disseminated than CBT and IPT, and increases restraint and induces modest weight loss in the short term. However, it is not as effective as CBT or IPT with respect to remission of binge eating in the long term. Given its cost-effectiveness, CBTgsh may be an optimal first-line treatment option, especially when specialist care (e.g., CBT or IPT) is not available.
Future Directions
Given that effective treatments exist for most individuals with BED, future research is needed to bolster public health impact by improving access to empirically supported treatments, by investigating how best to disseminate such treatments into the community. Specifically, future research should examine best implementation methods for training therapists and best methods for increasing scalability of these interventions. Another area requiring study involves addressing the diverse needs of patients, particularly those who do not respond to established treatments. Research is also needed that focuses on early intervention. Finally, data on the cost effectiveness of early intervention and treatment are needed.
Key References
- 1.Devlin MJ, Goldfein JA, Petkova E, Liu L, Walsh BT. Cognitive behavioral therapy and fluoxetine for binge eating disorder: Two-year follow-up. Obes. 2007;15:1702–9. doi: 10.1038/oby.2007.203. [DOI] [PubMed] [Google Scholar]
- 2.Grilo CM, Masheb RM, Wilson G, Gueorguieva R, White MA. Cognitive–behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: A randomized controlled trial. J Consult Clin Psychol. 2011;79:675–685. doi: 10.1037/a0025049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grilo CM, Masheb RM, Crosby RD. Predictors and moderators of response to cognitive behavioral therapy and medication for the treatment of binge eating disorder. J Consult Clin Psychol. 2012 doi: 10.1037/a002700. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hilbert A, Bishop M, Stein R, Tanofsky-Kraff M, Swenson A, Welch R, Wilfley D. Long-term Efficacy of Psychological Treatments for Binge Eating Disorder. Brit J Psychiatry. 2012;200:232–237. doi: 10.1192/bjp.bp.110.089664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lynch FL, Dickerson J, Perrin N, DeBar L, Wilson GT, Kraemer H, Striegel-Moore R. Cost-effectiveness of treatment for recurrent binge eating. J Consult Clin Psychol. 2010;78:322–333. doi: 10.1037/a0018982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peterson CB, Mitchell JE, Crow SJ, Crosby RD, Wonderlich SA. The efficacy of self-help group treatment and therapist-led group treatment for binge eating disorder. Am J Psychiatry. 2009;166:1347–1354. doi: 10.1176/appi.ajp.2009.09030345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley DE. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): Causal pathways and treatment implications. Clin Psychol Rev. 2010;30:400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Safer DL, Robinson AH, Jo B. Outcome from a randomized controlled trial of group therapy for binge eating disorder: Comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behav Ther. 2010;41:106–20. doi: 10.1016/j.beth.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Striegel-Moore RH, Wilson GT, DeBar L, Perrin N, Lynch F, Rosselli F, Kraemer H. Cognitive behavioral guided self-help for the treatment of recurrent binge eating. J Consult Clin Psychol. 2010;78:312–321. doi: 10.1037/a0018915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, Dounchis JZ, Frank MA, Wiseman CV, Matt GE. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of binge eating disorder. Arch Gen Psychiatry. 2002;59:713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]
- 11.Wilson GT, Grilo C, Vitousek K. Psychological treatment of eating disorders. Am Psychologist. 2007;62:199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- 12.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Allegiance bias and therapist effects: results of a randomized controlled trial of binge eating disorder. Clin Psychol: Sci Pract. 2011;18:119–125. doi: 10.1111/j.1468-2850.2011.01243.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
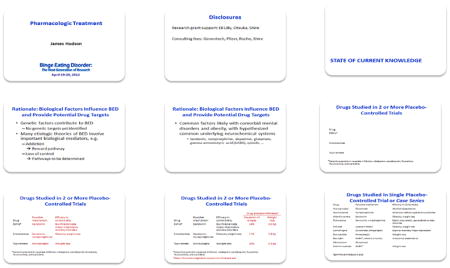
Pharmacologic Treatment
State of Current Knowledge
The underlying rationale for pharmacologic treatment is that biological factors influence BED, and medications have been useful in the treatment in the treatment of conditions commonly comorbid with BED, such as mood disorders, anxiety disorders, and substance use disorders. Although as yet no specific targets identified for BED (or for its comorbid conditions), potential targets include neurotransmitters (such as monoamines) and medications targeting certain brain pathways, such as the reward circuit via dopamine modulation.
Examining the results of clinical trials of pharmacologic treatment in BED, three medications or classes of medications have been studied in two or more placebo-controlled trials and therefore provide some basis for preliminary conclusions about efficacy. There have been six studies of selective serotonin reuptake inhibitors (SSRIs), two studies of sibutramine, and two studies of topiramate. All three of these groups produce clinically meaningful reductions in frequency of binge eating relative to placebo in short-term trials, and sibutramine and topiramate (but not SSRIs) also produce clinically meaningful reductions in body weight. However, sibutramine has been withdrawn from the market and topiramate is frequently associated with problematic cognitive effects, thus limiting its clinical utility.
A number of medications have been studied in either a single-placebo controlled trial or in an open-label case series. It is difficult to assess efficacy from these reports. However, none of these medications has thus far shown extraordinary promise in terms of its combination of efficacy and safety so that future development will likely seek to find other medications for BED, rather than develop further these particular agents.
The medications used thus far in clinical studies have a large variety of potential mechanisms of action in BED, including effects on neurotransmitters (serotonin, norepinephrine, dopamine, glutamate, gamma-aminobutyric acid), effects that are antiepileptic (e.g., topiramate, zonisamide and lamotrigine), and effects related potentially to the reward pathway (e.g., dopamine).
Future Directions
Larger, more definitive trials command a high research priority to determine the efficacy and safety of drug treatment for BED. Another priority for future research is to identify better targets for drug intervention, including genetic factors, neural circuit abnormalities, and mechanisms controlling food intake. Also, since no drug for treatment of BED is approved for marketing in the US or other countries, a pathway for approval should be developed that includes consensus about what constitute adequate demonstration of efficacy and how to integrate the effects of treatment not only on binge eating, but also on body weight, into the overall assessment of efficacy.
Key References
- 1.Appolinario JC, Bacaltchuk J, Sichieri R, et al. A randomized, double-blind, placebo-controlled study of sibutramine in the treatment of binge-eating disorder. Arch Gen Psychiatry. 2003;60:1109–1116. doi: 10.1001/archpsyc.60.11.1109. [DOI] [PubMed] [Google Scholar]
- 2.Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: A systematic review of randomized controlled trials. Int J Eat Disord. 2007;40:337–348. doi: 10.1002/eat.20370. [DOI] [PubMed] [Google Scholar]
- 3.Carter WP, Hudson JI, Lalonde JK, Pindyck L, McElroy SL, Pope HG., Jr Pharmacologic treatment of binge eating disorder. Int J Eat Disord. 2003;34 (Suppl):S74–88. doi: 10.1002/eat.10207. [DOI] [PubMed] [Google Scholar]
- 4.McElroy SL, Arnold LM, Shapira NA, et al. Topiramate in the treatment of binge eating disorder associated with obesity: A randomized, placebo-controlled trial. Am J Psychiatry. 2003;160:255–261. doi: 10.1176/appi.ajp.160.2.255. [DOI] [PubMed] [Google Scholar]
- 5.McElroy SL, Hudson JI, Capece JA, Beyers K, Fisher AC, Rosenthal NR. Topiramate for the treatment of binge eating disorder associated with obesity: a placebo-controlled study. Biol Psychiatry. 2007;61:1039–1048. doi: 10.1016/j.biopsych.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Wilfley DE, Crow SJ, Hudson JI, et al. Efficacy of sibutramine for the treatment of binge eating disorder: A randomized multicenter placebo-controlled double-blind study. Am J Psychiatry. 2008;165:51–58. doi: 10.1176/appi.ajp.2007.06121970. [DOI] [PubMed] [Google Scholar]
Surgical Treatment
State of Current Knowledge
Currently, the three main procedures used for bariatric surgery are Roux-en-Y gastric bypass, gastric banding, and sleeve gastrectomy. All induce loss of body weight, but the gastric band is less effective than the other two procedures. The mechanisms involved include restriction (all three), malabsorption (gastric bypass), and hormonal changes such as effects on glucagon-like peptide 1 (GLP-1) and peptide YY3-36 (gastric bypass and sleeve gastrectomy). In terms of the relationship of bariatric surgery to BED, the presence of BED predicts less weight loss or more weight regain in some studies, but this is not a consistent finding. However, the presence of loss of control eating post-surgery consistently predicts less loss or greater weight regain.
Future Directions
A priority for future research is to develop pre- and post-surgical interventions to prevent the emergence or reemergence of loss of control eating. Also of importance is elucidating the mechanism whereby bariatric surgery suppresses binge eating and by which loss of control eating emerges post-surgery. In particular, it is likely that these mechanisms involve hormonal changes (in addition to other effects), and understanding these hormonal changes, in turn, could help shed light on mechanisms related to loss of control eating. In this regard, studies using the gastric sleeve may be useful, in that this procedure has no pouch, but does induce hormonal changes.
Key Reference
- 1.Engel SG, Mitchell JE, de Zwaan M, Steffen K. Eating disorders and eating problems pre-and post-bariatric surgery, in Psychosocial Assessment and Treatment of Baritaric Surgery Patients. In: Mitchell JE, de Zwaan M, editors. Routledge; New York, NY: 2011. [Google Scholar]
Relevance to Military Health and Readiness
State of Current Knowledge
Members of the military are likely at high-risk for BED. Although this hypothesis has not been tested, the strict requirements for weight and fitness to which military personnel must adhere result in a heightened external pressure for weight loss. It is proposed that this pressure often leads to excessive dietary restraint and, in response individuals are led to engage in binge eating. In addition, deployments as well as frequent relocations may contribute to binge eating in response to stress. To date, only five studies of binge eating have been conducted in military populations and most used of self-report questionnaires. Notably, none specifically captured DSM-IV criteria for BED; rather research assessed for EDNOS. Across studies, the prevalence estimates for binge eating have ranged from 10% – 35%, with higher estimates (upwards of 60%) for those not meeting their service weight standards. However, there are no data on whether BED is accurately identified and diagnosed in military settings, and there is no research on treatment efficacy in military populations. There are also no studies on the numbers of military members not deployable due to BED, and no information on the frequency of fitness and weight “failures” among individuals with the disorder. Although military members who receive effective treatment for BED may be able to remain in service, personnel failing weight standards may be separated from (no longer allowed to serve in) the military. Given the strong association between BED and excess body weight, members who suffer from the disorder likely struggle to meet the required weight and fitness regulations mandated by their service. Therefore, members may be separated from the military due to their weight, rather than receiving appropriate treatment for BED and remaining in service.
Future Directions
Given the dearth of data on BED and the military, the future research directions proposed were relatively straightforward. Less straightforward, and beyond the scope of the workshop, was a discussion of the barriers and challenges to conduct research in military populations. Nevertheless, there was unanimous agreement that the primary next research step includes determining the prevalence of BED in military populations and subpopulations to elucidate not only the scope of the problem, but to understand if military members are at greater risk for the disorder than civilian populations. Part of this effort should involve examining whether one branch or service of the military is at greater risk for BED than another. In addition, it should be determined how many of those individuals not meeting weight or fitness standards are struggling with BED. Another important research direction should involve determining whether treatment response to BED is similar to that observed in civilian studies. Lastly, studies should be conducted to assess the impact of BED on both military readiness and the financial burden on the Department of Defense.
Key References
- 1.Antczak AJ, Brininger TL. Diagnosed eating disorders in the U.S. Military: A nine year review. Eat Disord. 2008;16:363–377. doi: 10.1080/10640260802370523. [DOI] [PubMed] [Google Scholar]
- 2.Beekley MD, Byrne R, Yavorek T, Kidd K, Wolff J, Johnson M. Incidence, prevalence, and risk of eating disorder behaviors in military academy cadets. Military Med. 2009;174:637–641. doi: 10.7205/milmed-d-02-1008. [DOI] [PubMed] [Google Scholar]
- 3.Carlton JR, Manos GH, Van Slyke JA. Anxiety and abnormal eating behaviors associated with cyclical readiness testing in a Naval hospital active duty population. Military Med. 2005;170:663–667. doi: 10.7205/milmed.170.8.663. [DOI] [PubMed] [Google Scholar]
- 4.Garber AK, Boyer CB, Pollack LM, Chang YJ, Shafer M. Body mass index and disordered eating behaviors are associated with weight dissatisfaction in adolescent and young adult female military recruits. Military Med. 2008;173:138–145. doi: 10.7205/milmed.173.2.138. [DOI] [PubMed] [Google Scholar]
- 5.Lauder TD, Campbell CS. Abnormal eating behaviors in female reserve officer training corps cadets. Military Med. 2001;166:264–268. [PubMed] [Google Scholar]
- 6.McNulty PA. Prevalence and contributing factors of eating disorder behaviors in a population of female Navy nurses. Military Med. 1997;162:703–706. [PubMed] [Google Scholar]
- 7.McNulty PA. Prevalence and contributing factors of eating disorder behaviors in active duty Navy men. Military Med. 1997;162:753–758. [PubMed] [Google Scholar]
- 8.Peterson AL, Talcott GW, Kelleher WJ, Smith SD. Bulimic weight-loss behaviors in military versus civilian weight-management programs. Military Med. 1995;160:616–620. [PubMed] [Google Scholar]
- 9.Warner C, Warner C, Matuszak T, Rachal J, Flynn J, Greiger TA. Disordered eating in entry-level military personnel. Military Med. 2007;172:147–151. doi: 10.7205/milmed.172.2.147. [DOI] [PubMed] [Google Scholar]
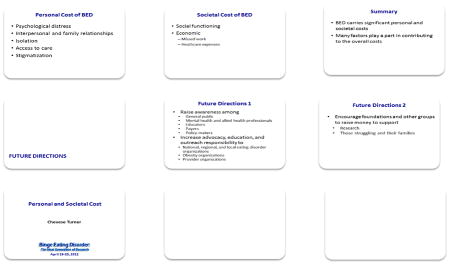
Personal and Societal Cost
State of Current Knowledge
There is clear personal cost to BED. Individuals with the disorder suffer from psychological distress including isolation, stigmatization, and difficulties with interpersonal and family relationships. Despite some effective treatments for BED, it is often difficult for individuals with the disorder to access care. Lack of knowledge, limited numbers of trained professionals, and insufficient insurance coverage are among the reasons that individuals with BED do not receive appropriate intervention. BED also incurs a cost to society. In addition to poor social functioning with friends, family and co-workers, those with BED have a higher prevalence of multiple health problems that often result in missed work, which in turn impacts on individual businesses and the broader economy. Furthermore, healthcare expenses incurred due to the associated physical problems also result in societal costs.
Future Directions
Raising awareness of BED and its associated costs is required. Individuals and organizations need to be informed about how BED impacts society. This effort involves educating the general public, mental health and allied health professionals, educators, payers, and policy-makers. Another important next step includes increasing advocacy, education, fund-raising, and outreach responsibility to national, regional, and local eating disorder, obesity and provider organizations.
Key References
- 1.Crow SJ, Peterson CB. In: The Economic and Social Burden of Eating Disorders, in Eating Disorders. Maj M, Halmi K, López-Ibor JJ, Sartorius N, editors. Vol. 6. John Wiley & Sons, Ltd; Chichester, UK: 2003. [Google Scholar]
- 2.Lynch FL, Striegel-Moore RH, Dickerson JF, Perrin N, DeBar L, Wilson GT, Kraemer HC. Cost-effectiveness of guided self-help treatment for recurrent binge eating. J Consult Clin Psychol. 2010;78:322–333. doi: 10.1037/a0018982. [DOI] [PMC free article] [PubMed] [Google Scholar]
Conclusion
With the inclusion of BED in the DSM-5, we face a new frontier of exciting and important research opportunities. To date, investigators in the fields of eating disorders, obesity and addictions have worked primarily independently. In a workshop including representatives from many fields and from the NIH, overviews of the state of the field and future directions for research were discussed. While the current report represents the proceedings from the meeting, it is not comprehensive in terms of all potential directions for study, but rather provides a foundation for the next generation of BED research.
Acknowledgments
Research support: National Institute of Mental Health R13 MH094127-01 to Marian Tanofsky-Kraff and James I. Hudson.
Appendix 1. Binge Eating Disorder: The Next Generation of Research Slide Presentations


Footnotes
Conflict of Interests
Drs. Tanofsky-Kraff and Bulik report no conflicts of interest. Dr. Marcus served on the DSM-5 Eating Disorders Work Group and is on the Scientific Advisory Board of United Health Care. Dr. Striegel has received consultant fees from Wellness and Prevention, Inc. (a Johnson & Johnson company) and served on the DSM-5 Eating Disorders Work Group. Dr. Wilfley has received research support from Shire Development and consulting fees from GlaxoSmithKline Consumer Healthcare; Minnesota Obesity Center; United Health Group, Childhood Obesity Initiative; and Wellspring Healthy Living Academy. Dr. Wonderlich served on the DSM-5 Eating Disorders Work Group. Dr. Hudson has received research support from Eli Lilly, Otsuka, and Shire, and consulting fees from Genentech, HealthCore, Pfizer, Roche, and Shire.


