Abstract
Background:
It is not known whether cardiovascular disease (CVD) risk level is related to knowledge of the leading cause of death of women or heart attack symptoms.
Hypothesis:
Women with higher CVD risk estimated by Framingham Risk Score (FRS) or metabolic syndrome (MS) have lower CVD knowledge.
Methods:
Women visiting primary care clinics completed a standardized behavioral risk questionnaire. Blood pressure, weight, height, waist size, fasting glucose, and lipid profile were assessed. Women were queried regarding CVD knowledge.
Results:
Participants (N = 823) were Hispanic women (46%), non‐Hispanic white (37%), and non‐Hispanic black (8%). FRS was determined in 278: low (63%), moderate (29%), and high (8%); 24% had ≥3 components of MS. The leading cause of death was answered correctly by 54%, heart attack symptoms by 67%. Knowledge was lowest among racial/ethnic minorities and those with less education (both P< 0.001). Increasing FRS was inversely associated with knowing the leading cause of death (low 72%, moderate 68%, high 45%, P = 0.045). After multivariable adjustment, moderate/high FRS was inversely associated with knowing symptoms (moderate odds ratio [OR] 0.52, 95% confidence interval [CI]: 0.28‐0.98; high OR 0.29, 95% CI: 0.11–0.81), but not the leading cause of death. MS was inversely associated with knowing the leading cause of death (P< 0.001) or heart attack symptoms (P = 0.018), but not after multivariable adjustment.
Conclusions:
Women with higher FRS were less likely to know heart attack symptoms. Efforts to target those at higher CVD risk must persist, or the most vulnerable may suffer disproportionately, not only because of risk factors but also inadequate knowledge. Clin. Cardiol. 2011 DOI: 10.1002/clc.22092
This work was supported in part by the US Department of Health and Human Services (1HHCWH05003‐01‐11); Arlene and Joseph Taub Foundation, Paterson, New Jersey; Edwina and Charles Adler Foundation; and by Columbia University's CTSA grant, UL1‐RR024156 from the NCRR/NIH.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Introduction
Knowledge of cardiovascular disease (CVD) among women continues to be suboptimal despite advances made in the last 15 years as a result of educational and public awareness efforts. Although awareness of the leading cause of death increased between 1997 and 2009, there is room for improvement.1, 2 Moreover, CVD knowledge remains lower among Hispanic and African American women.3, 4
Improving CVD knowledge remains an important goal, as it is integral to promoting healthy lifestyles and preventing disease. Barriers to increased awareness include low levels of education, low health literacy, low socioeconomic status, shortcomings in clinician and public health education, and systems‐level barriers.5, 6 Presumably, women at highest risk for CVD receive education about cardiovascular disease, and whereas improving CVD knowledge may improve CVD outcomes,7 there are conflicting data about whether cardiovascular risk level is associated with the level of CVD health knowledge. One study reported that a higher risk for stroke was associated with more knowledge about stroke risk factors,8 whereas others have shown no significant difference9, 10 or an inverse relationship.11, 12 Although one study found that increased cardiovascular risk was associated with less knowledge of heart attack symptoms,13 there are overall little data regarding the relationship between CVD risk level and knowledge about CVD.
Although cardiovascular mortality among young women ages 35 to 54 years decreased from 1989 to 2000, mortality increased between 2000 and 2002,14 signaling a need to emphasize primary prevention. Among patients without known cardiovascular disease, research has helped to identify those at risk for future CVD and mortality by defining Framingham Risk Score (FRS)15, 16 and metabolic syndrome (MS).17 Less is known about whether risk is related to knowledge. It is not known whether cardiovascular risk among women is associated with CVD knowledge.
Accordingly, the goal of this study was to examine the association between cardiovascular risk in women without known CVD, an important target for primary prevention, and their knowledge about CVD. We focused on the leading cause of death of women and symptoms of a heart attack, initiated by the American Heart Association and Healthy People 2010,18 continuing to Healthy People 2020.19 Given that obesity has been identified as a modifiable CVD risk factor,20 and that FRS and MS are used to predict risk for CVD, we sought to characterize participants along these lines to determine if there was an association between these factors and CVD knowledge.
Methods
Participants were a convenience sample of women attending the outpatient clinics of New York Presbyterian Hospital, Columbia University, who took part in a cross‐sectional study to evaluate cardiovascular disease knowledge and cardiovascular risk among urban women. The study was approved by the Columbia University Institutional Review Board, and all participants provided informed consent. Participants were enrolled from April 2007 to June 2011. Exclusion criteria included known history of coronary artery disease, history of cerebrovascular disease, pregnancy, and age younger than 18 years.
All participants completed a standardized face‐to‐face questionnaire in English or Spanish adapted from the Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System.21 Demographic data including age, race/ethnicity, education, health insurance, income, and geographic area of residence were collected. Self‐reported medical history of diagnoses of diabetes, hypertension, and smoking were also collected. Electronic charts were reviewed for fasting glucose and lipid profile within 3 months of study enrollment. Laboratory data were used if they were drawn 3 months prior to enrollment at the earliest or 3 months after enrollment at the latest. Blood pressure and waist circumference were determined in all, as well as height and weight to calculate body mass index (BMI). BMI (weight [kg]/height [m2]) was calculated and classified as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2).
Participants were asked about knowledge of cardiovascular disease, based on American Heart Association and Healthy People 2010 to improve cardiovascular health and quality of life. We asked: (1) What is the leading cause of death of women? (2) What are the early warning symptoms or signs of heart attack? (3) What are the actions to take if experiencing a heart attack? Options for the leading cause of death were (1) breast cancer, (2) lung cancer, (3) HIV/AIDS, (4) heart disease, (5) stroke. The correct answer was heart disease. Options for early warning symptoms or signs of heart attack were (1) shortness of breath, (2) dizziness, (3) chest pain or discomfort, (4) significant fatigue, (5) all of the above. The correct answer was all of the above. Options for what are the actions to take if experiencing a heart attack were (1) call 911, (2) drive yourself to the hospital, (3) ask a friend to drive you to the hospital, (4) make an appointment with your doctor. The correct answer was to call 911.
FRS and MS were used to classify participants' cardiovascular risk, as these risk scores have been shown to be powerful predictors of future CVD and are used commonly in clinical practice.15, 16, 17 FRS was determined using a 10‐year prediction tool, similar to the calculator from the National Cholesterol Education Program Third Report of the Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults.16, 22 The tool estimated 10‐year risk of having a cardiovascular event such as stroke, myocardial infarction, peripheral arterial disease, and heart failure. The calculator for women used includes age, total cholesterol, high‐density lipoprotein (HDL) cholesterol, smoking status, systolic blood pressure, currently on medication to treat blood pressure, and diabetes. Low FRS was defined as <10% risk of cardiovascular event within 10 years, moderate risk was 10% to <20%, and high risk was 20% or more. FRS was determined in all participants who had information on all components needed for calculation (age, blood pressure, documented laboratory data within 3 months of enrollment in the study, and information on smoking status, medication to treat blood pressure, diabetes). MS was determined by the presence of three or more of the following: waist size >35 inches, triglycerides ≥150, HDL <50, blood pressure ≥130/85, fasting glucose ≥100. Participants were characterized as without metabolic syndrome if they had <3 components present. Participants were characterized for MS if all information was available (waist size, blood pressure, laboratory data within 3 months.)
Analyses were completed with SAS 9.2 (SAS Institute, Cary, NC). The significance of differences in knowledge among participants with low, moderate, and high FRS was determined using the Mantel‐Haenszel χ 2 test. Differences in knowledge between women with and without MS were assessed using the 2‐sided Fisher exact test for categorical variables. Multivariable logistic regression analysis was used to test for the effect of cardiovascular risk on knowledge after controlling for race/ethnicity and years of education. Similar analyses were performed for MS and BMI categories. A P value of <0.05 was considered significant for all analyses.
Results
Demographics and Cardiovascular Risk Profile
Of the 823 participants, 382 (46%) were Hispanic (primarily of Caribbean origin), 301 (37%) were non‐Hispanic white, 66 (8%) were non‐Hispanic black, 60 (7%) were Asian, and 14 (2%) were other race/ethnicity. Mean age was 48 ± 15 years, and mean education was 14 ± 4 years. The average body mass index was 27 ± 6 kg/m2, and 447 (55%) of the participants were overweight or obese. FRS was determined in 278 women; 175 (63%) were low risk, 81(29%) were moderate risk, and 22 (8%) were high risk. In addition, 322 were characterized for the components of metabolic syndrome; 76 (24%) had ≥3 components of MS (Table 1). The vast majority of participants who could not have FRS determined or be characterized for the components of MS lacked laboratory data within 3 months of study enrollment. The percentage of participants classified as low, moderate, or high FRS did not differ by race/ethnicity. A greater percentage of Hispanic and non‐Hispanic black participants had ≥3 components of MS, compared to non‐Hispanic white (44% vs 10%, P < 0.0001 and 27% vs 10%, P = 0.013, respectively). In addition, a greater percentage of Hispanic and non‐Hispanic black participants were obese compared to non‐Hispanic white (41% vs 15%, P < 0.0001 and 33% vs 15%, P < 0.0001, respectively). Participants with lower levels of education (≤8 years and 9–12 years) were more likely to have moderate or high FRS, have ≥3 components of MS, and be obese (Table 2).
Table 1.
Characteristics of Participants (N = 823)
| Race/ethnicity | |
|---|---|
| Hispanic | 382 (46%) |
| Non‐Hispanic white | 301 (37%) |
| Non‐Hispanic black | 66 (8%) |
| Asian | 60 (7%) |
| Other | 14 (2%) |
| Age, mean ± SD, y | 48 ± 15 |
| Education, mean ± SD, y | 14 ± 4 |
| BMI (kg/m2), mean ± SD, n = 819 | 27 ± 6 |
| Underweight (BMI <18.5) | 19 (2%) |
| Normal weight (BMI 18.5–24.9) | 353 (43%) |
| Overweight (BMI 25–29.9) | 246 (30%) |
| Obese (BMI ≥ 30) | 201 (25%) |
| Framingham Risk Score, n = 278 | |
| Low | 175 (63%) |
| Moderate | 81 (29%) |
| High | 22 (8%) |
| Metabolic syndrome, n = 322 | |
| ≥3 components of MS | 76 (24%) |
| <3 components of MS | 246 (76%) |
Abbreviations: BMI, body mass index; MS, metabolic syndrome; SD, standard deviation.
Table 2.
Race/Ethnicity, Education, and Framingham Risk Score and Metabolic Syndrome
| Framingham Risk, n = 278 | Metabolic Syndrome, n = 322 | ||||
|---|---|---|---|---|---|
| Low, n (%) | Moderate, n (%) | High, n (%) | <3 Components of Metabolic Syndrome, n (%) | ≥3 Components of Metabolic Syndrome, n (%) | |
| Race/ethnicity | |||||
| Non‐Hispanic white | 102 (68) | 41 (27) | 7 (5) | 141 (90) | 15 (10) |
| Hispanic | 47 (55) | 28 (33) | 10 (12) | 64 (56) | 50 (44) |
| Non‐Hispanic black | 13 (46) | 11 (39) | 4 (14) | 22 (73) | 8 (27) |
| Asian | 9 (82) | 1 (9) | 1 (9) | 15 (83) | 3 (17) |
| Other | 4 (100) | 0 (0) | 0 (0) | 4 (100) | 0 (0) |
| P value | 0.09 | <0.0001 | |||
| Education years | |||||
| ≤8 | 12 (33) | 16 (44) | 8 (22) | 19 (39) | 30 (61) |
| 9–12 | 21 (51) | 15 (37) | 5 (12) | 24 (11) | 22 (45) |
| ≥12 | 139 (70) | 50 (25) | 9 (5) | 195 (89) | 27 (55) |
| P value | <0.0001 | <0.0001 | |||
Knowledge of Leading Cause of Death
The leading cause of death of women was answered correctly by 445 of 819 (54%) participants. Hispanic participants and those who had fewer years of education were less likely to know the leading cause of death of women (Table 3). Those with increasing FRS were less likely to know the leading cause of death (low risk 72%, moderate risk 67.5%, and high risk 45%, P = 0.045) (Figure 1). Participants with ≥3 components of MS were less likely than those with <3 components of MS to know the leading cause of death of women (39% vs 72%, P < 0.001) (Figure 1). Additionally, women who were overweight or obese were less likely to know the leading cause of death compared to normal weight women (normal weight 62%, overweight 50%, obese 45%, P < 0.001).
Table 3.
Knowledge by Race/Ethnicity and Education
| Know Leading Cause of Death, n = 819, n (%) | Know Heart Attack Symptoms, n = 820, n (%) | |
|---|---|---|
| Race/ethnicity | ||
| Non‐Hispanic white | 265 (88) | 244 (81) |
| Hispanic | 100 (26) | 221 (58) |
| Non‐Hispanic black | 37 (56) | 46 (70) |
| Asian | 33 (55) | 29 (48) |
| Other | 33 (55) | 29 (48) |
| P value | <0.001 | <0.001 |
| Education years | ||
| ≤8 | 14 (14) | 41 (42) |
| 9–12 | 43 (23) | 110 (59) |
| >12 | 384 (73) | 393 (75) |
| P value | <0.001 | <0.001 |
Figure 1.
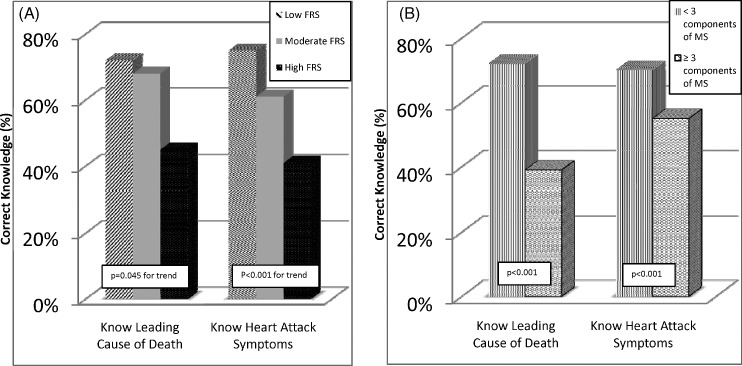
(A) Univariate association between knowledge of the leading cause of death, knowledge of heart attack symptoms, and Framingham Risk Score (low, moderate, high). (B) Univariate association between knowledge of the leading cause of death, knowledge of heart attack symptoms, and Metabolic Syndrome (MS).
However, in multivariable logistic regression analysis that included years of education and race/ethnicity, higher FRS was no longer significantly associated with lower knowledge of the leading cause of death (Table 4). Additionally, the presence of ≥3 components of MS and having a BMI classified as overweight or obese were no longer associated with lower knowledge of leading cause of death.
Table 4.
Multivariable Model: Framingham Risk Score and Knowledge
| Know Leading Cause of Death, OR (95% CI) | Know Heart Attack Symptoms, OR (95% CI) | |
|---|---|---|
| Moderate Framingham risk | 1.34 (0.60–3.02) | 0.52 (0.28–0.98) |
| High Framingham risk | 0.84 (0.23–3.14) | 0.29 (0.11–0.81) |
| Demographic factors | ||
| Education years | 1.29 (1.15–1.45) | 1.06 (0.98–1.15) |
| Hispanic race/ethnicity | 0.14 (0.06–0.33) | 0.33 (0.15–0.73) |
| Non‐Hispanic black | 0.37 (0.13–1.09) | 0.76 (0.29–2.01) |
| Asian | 0.23 (0.05–1.09) | 0.18 (0.05–0.67) |
| Other race/ethnicity | 0.35 (0.03–3.64) | 0.55 (0.05–5.59) |
Abbreviations: CI, confidence interval; OR, odds ratio.
Knowledge of Heart Attack Symptoms
The question evaluating symptoms of a heart attack was answered correctly by 548 of 820 (67%) women. Hispanic participants and those who had fewer years of education were less likely to know the symptoms of a heart attack (Table 3). Those with increasing FRS were less likely to know heart attack symptoms (low risk 75%, moderate risk 61%, high risk 41%, P < 0.001) (Figure 1). Women with ≥3 components of MS were also less likely to know heart attack symptoms (55% vs 70%, P = 0.018) (Figure 1). There was no significant difference in knowledge of heart attack symptoms in participants who were overweight or obese, compared to those of normal weight (normal 68%, overweight 63%, obese 68%).
In multivariable logistic regression analysis that included years of education and race/ethnicity, moderate and high FRS was still associated with less knowledge of heart attack symptoms (Table 4). However, the presence of ≥3 components of MS was not associated with less knowledge of heart attack symptoms.
Knowledge About Calling 911
Knowledge about calling 911 if experiencing heart attack was answered correctly by 725 of 819 (89%) of participants. There was no significant difference in knowledge of the need to call 911 by FRS (low 89%, moderate 90%, high 95%) or by presence of ≥3 components of MS (88% vs 91%).
Discussion
Despite public health efforts, knowledge of the leading cause of death of women and knowledge of heart attack symptoms remains suboptimal. Although most efforts to understand CVD knowledge gaps have focused on demographic factors such as race/ethnicity and education level, we further characterized a primary prevention population of women by including CVD risk classification based on laboratory and clinical data. The addition of CVD risk categories afforded a deeper understanding of the known knowledge disparities, and we found that women at higher risk for cardiovascular disease, assessed by moderate or high FRS, were less likely to know symptoms of a heart attack than their lower risk counterparts. We found no difference in knowledge of the leading cause of death of women by FRS after multivariable adjustment. Although we found that the presence of ≥3 components of MS was associated with lower knowledge of both heart attack symptoms and leading cause of death, after multivariable analysis, the relationship was no longer present. However, it is notable that a large proportion of women with MS were of Hispanic origin and also had low knowledge of leading cause of death and heart attack symptoms, so this may be a particularly low knowledge group.
In this study of an urban primary care population of women, we found results that correspond to previous surveys showing lower knowledge of leading cause of death and heart attack symptoms among racial/ethnic minorities2, 3 and those with fewer years of education.23, 24 The findings are also similar to reports of lower knowledge of stroke symptoms among racial/ethnic minorities.9, 11 In contrast to merely 53% who knew to call 911 if experiencing symptoms of a heart attack in previous work,2 in this study 89% answered correctly, and there was no difference by FRS or MS. This difference may be attributed to increasing efforts to improve action taken for heart attack symptoms given suboptimal awareness of importance of calling 911,25 such as in campaigns from the US Department of Health and Human Services “Make The Call, Don't Miss a Beat.”26 Furthermore, a large percentage of racial/ethnic minority women residing in New York City utilize emergency services for many healthcare needs, which is a well‐recognized target for improvement.27, 28
Patients with the very highest cardiovascular risk, such as those with previous events, might be expected to have higher knowledge of heart attack symptoms because they may have experienced a prior incident. Here, by excluding patients with known CVD, we focused on an important primary prevention population, that is, those with multiple risk factors. FRS is a recognized tool to evaluate risk in a primary care population, traditionally with high risk being delineated as ≥20% risk of CVD event in 10 years,16, 22 and more recently more stringent criteria have been utilized, suggesting that ≥10% risk of CVD event in 10 years should be considered high risk.6 Thus, our moderate risk population is at least moderate risk by traditional FRS but may even be considered as at high risk. The association between lower knowledge of heart attack symptoms and higher FRS in patients without a previous event is troubling. Decreased knowledge of stroke and heart attack symptoms was described among self‐reported high‐risk CVD participants,13 and decreased knowledge of leading cause of death was found among those with MS.25 This is a collective cause for concern because higher‐risk patients are most likely to experience stroke or heart attacks that are potentially preventable with risk factor modification.22, 29, 30, 31
The explanation for the association between higher FRS and lower knowledge of heart attack symptoms is not clear. Action steps to reduce risk including patient engagement, consistent medical care,32 identification of risk factors,33 delivery of patient‐centered educational messages,6, 34 and development of a risk reduction plan22, 29, 30, 31 are critical. Although participants were recruited from primary care clinics, factors such as inconsistent healthcare, lack of sensitive educational messages, and inadequate plans for risk reduction could have contributed to the higher FRS. These deficiencies may also represent a missed opportunity for discussions of heart attack symptoms.
Given that patients with more knowledge of symptoms have a greater likelihood of calling 911,35 inadequate knowledge of heart attack symptoms among higher‐risk participants is troublesome. Delay in symptom recognition is a barrier to prompt therapy,36 and timely action resulting from recognition of symptoms leads to superior outcomes.37 Attempts to improve outcomes by increasing knowledge have been mixed. After CVD media campaigns, a Swedish study reported that acute myocardial infarction therapy was more timely.7 On the other hand, the US Rapid Early Action for Coronary Treatment trial showed more knowledge of heart attack symptoms,1 but no change in delay time.38 Although progress has been made in decreasing cardiovascular mortality by risk factor modification and therapeutic advances,39, 40 health education has been outlined as an important goal for prevention of CVD in women overall in 2011 guidelines,6 and symptom recognition and prompt therapy has been outlined as a goal of Healthy People 202019 and plays an important role in improving outcomes.
Limitations
A self‐report questionnaire was used, which is subject to recall and social desirability bias. The use of multiple‐choice questions may have allowed some to guess the correct answer. Participants were women from the urban Northeast and results may not be comparable among other geographic areas or among men.
Conclusion
Women with higher FRS were less likely to know the symptoms of heart attack than their lower risk counterparts. Educational efforts aimed at racial/ethnic minority women, specifically Hispanic women, individuals with lower education, and women who have moderate or high FRS should target persons with lowest knowledge about symptoms of heart attack. Future research should query participants' knowledge of personal risk factors as an important step in prevention of cardiovascular disease. Efforts to focus on those at high risk for cardiovascular disease must persist lest the vulnerable may suffer disproportionately not only due to risk profile but also because of inadequate knowledge.
References
- 1. Goff DC Jr, Mitchell P, Finnegan J, et al. Knowledge of heart attack symptoms in 20 US communities. Results from the Rapid Early Action for Coronary Treatment Community Trial. Prev Med. 2004;38:85–93. [DOI] [PubMed] [Google Scholar]
- 2. Mosca L, Mochari‐Greenberger H, Dolor RJ, et al. Twelve‐year follow‐up of American women's awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes. 2010;3:120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McGruder HF, Greenlund KJ, Malarcher AM, et al. Recognizing signs of heart attack and taking action. Ethn Dis. 2008;18:236–237. [PubMed] [Google Scholar]
- 4. Christian AH, Rosamond W, White AR, et al. Nine‐year trends and racial and ethnic disparities in women's awareness of heart disease and stroke: an American Heart Association national study. J Womens Health (Larchmt). 2007;16:68–81. [DOI] [PubMed] [Google Scholar]
- 5. Olomu AB, Grzybowski M, Ramanath VS, et al. Evidence of disparity in the application of quality improvement efforts for the treatment of acute myocardial infarction: the American College of Cardiology's Guidelines Applied in Practice Initiative in Michigan. Am Heart J. 2010;159:377–384. [DOI] [PubMed] [Google Scholar]
- 6. Mosca L, Benjamin EJ, Berra K, et al. Effectiveness‐based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Herlitz J, Blohm M, Hartford M, et al. Follow‐up of a 1‐year media campaign on delay times and ambulance use in suspected acute myocardial infarction. Eur Heart J. 1992;13:171–177. [DOI] [PubMed] [Google Scholar]
- 8. Ellis C, Egede LE. Stroke recognition among individuals with stroke risk factors. Am J Med Sci. 2009;337:5–10. [DOI] [PubMed] [Google Scholar]
- 9. Greenlund KJ, Neff LJ, Zheng ZJ, et al. Low public recognition of major stroke symptoms. Am J Prev Med. 2003;25:315–319. [DOI] [PubMed] [Google Scholar]
- 10. Travis LH, Flemming KD, Brown RD Jr, et al. Awareness of stroke risk factors, symptoms, and treatment is poor in people at highest risk. J Stroke Cerebrovasc Dis. 2003;12:221–227. [DOI] [PubMed] [Google Scholar]
- 11. Schneider AT, Pancioli AM, Khoury JC, et al. Trends in community knowledge of the warning signs and risk factors for stroke. JAMA. 2003;289:343–346. [DOI] [PubMed] [Google Scholar]
- 12. Ferris A, Robertson RM, Fabunmi R, et al. American Heart Association and American Stroke Association national survey of stroke risk awareness among women. Circulation. 2005;111:1321–1326. [DOI] [PubMed] [Google Scholar]
- 13. Lambert C, Vinson S, Shofer F, et al. The relationship between knowledge and risk for heart attack and stroke [published online ahead of print March 12, 2012]. J Stroke Cerebrovasc Dis. doi:10.1016/j.jstrokecerebrovasdis.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 14. Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–2132. [DOI] [PubMed] [Google Scholar]
- 15. D'Agostino RB Sr, Grundy S, Sullivan LM, et al. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–187. [DOI] [PubMed] [Google Scholar]
- 16. D'Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. [DOI] [PubMed] [Google Scholar]
- 17. Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta‐analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. [DOI] [PubMed] [Google Scholar]
- 18. Veazie MA, Galloway JM, Matson‐Koffman D, et al. Taking the initiative: implementing the American Heart Association Guide for Improving Cardiovascular Health at the Community Level: Healthy People 2010 Heart Disease and Stroke Partnership Community Guideline Implementation and Best Practices Workgroup. Circulation. 2005;112:2538–2554. [DOI] [PubMed] [Google Scholar]
- 19.Healthy People 2020. http://www.healthypeople.gov/2020. Accessed September 1, 2012.
- 20. Eckel RH, Krauss RM. American Heart Association call to action: obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation. 1998;97:2099–2100. [DOI] [PubMed] [Google Scholar]
- 21. US Department of Health and Human Services. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. 2004..
- 22. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 23. O'Brien F, O'Donnell S, McKee G, et al. Knowledge, attitudes, and beliefs about acute coronary syndrome in patients diagnosed with ACS: an Irish cross‐sectional study [published online ahead of print May 30, 2012]. Eur J Cardiovasc Nurs. doi: 10.1177/1474515112446544. [DOI] [PubMed] [Google Scholar]
- 24. Swanoski MT, Lutfiyya MN, Amaro ML, et al. Knowledge of heart attack and stroke symptomology: a cross‐sectional comparison of rural and non‐rural US adults. BMC Public Health. 2012;12:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Giardina EG, Sciacca RR, Foody JM, et al. The DHHS Office on Women's Health Initiative to Improve Women's Heart Health: focus on knowledge and awareness among women with cardiometabolic risk factors. J Womens Health (Larchmt). 2011;20:893–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Make the call, don't miss a beat. http://www.womenshealth.gov/heartattack. Accessed November 1, 2012.
- 27. Billings J, Parikh N, Mijanovich T. Emergency department use in New York City: a substitute for primary care? Issue Brief (Commonw Fund). 2000;(433):1–5. [PubMed] [Google Scholar]
- 28. Carrillo JE, Shekhani NS, Deland EL, et al. A regional health collaborative formed by New York‐Presbyterian aims to improve the health of a largely Hispanic community. Health Aff (Millwood). 2011;30:1955–1964. [DOI] [PubMed] [Google Scholar]
- 29. Selvin E, Marinopoulos S, Berkenblit G, et al. Meta‐analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141:421–431. [DOI] [PubMed] [Google Scholar]
- 30. Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2004;110:2952–2967. [DOI] [PubMed] [Google Scholar]
- 31. Hebert PR, Moser M, Mayer J, et al. Recent evidence on drug therapy of mild to moderate hypertension and decreased risk of coronary heart disease. Arch Intern Med. 1993;153:578–581. [PubMed] [Google Scholar]
- 32. Boulware LE, Marinopoulos S, Phillips KA, et al. Systematic review: the value of the periodic health evaluation. Ann Intern Med. 2007;146:289–300. [DOI] [PubMed] [Google Scholar]
- 33. From the Centers for Disease Control and Prevention. Decline in deaths from heart disease and stroke—United States, 1900–1999. JAMA. 1999;282:724–726. [PubMed] [Google Scholar]
- 34. Teutsch C. Patient‐doctor communication. Med Clin North Am. 2003;87:1115–1145. [DOI] [PubMed] [Google Scholar]
- 35. Meischke H, Yasui Y, Kuniyuki A, et al. How women label and respond to symptoms of acute myocardial infarction: responses to hypothetical symptom scenarios. Heart Lung. 1999;28:261–269. [DOI] [PubMed] [Google Scholar]
- 36. Goff DC Jr, Nichaman MZ, Ramsey DJ, et al. A population‐based assessment of the use and effectiveness of thrombolytic therapy. The Corpus Christi Heart Project. Ann Epidemiol. 1995;5: 171–178. [DOI] [PubMed] [Google Scholar]
- 37. Newby LK, Rutsch WR, Califf RM, et al. Time from symptom onset to treatment and outcomes after thrombolytic therapy. GUSTO‐1 Investigators. J Am Coll Cardiol. 1996;27:1646–1655. [DOI] [PubMed] [Google Scholar]
- 38. Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284:60–67. [DOI] [PubMed] [Google Scholar]
- 39. Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. [DOI] [PubMed] [Google Scholar]
- 40. Vaccarino V, Parsons L, Peterson ED, et al. Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med. 2009;169:1767–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]


