Abstract
Appearance concerns are common among HIV-infected individuals, and previous cross-sectional and longitudinal data indicate that these concerns are associated with antiretroviral therapy (ART) non-adherence. However, to date, no known prospective data have explored the mechanism behind this relationship. Thus, the aim of the current study was to test depression severity as a prospective mediator of the relationship between appearance concerns and ART non-adherence in HIV-infected individuals with a history of injection drug use (IDU). Participants were 89 HIV-infected individuals with a history of IDU who participated in a prospective, randomized controlled trial of cognitive behavioral therapy for depression and medication adherence. Clinician-administered measures of depression severity and appearance concerns, along with electronic monitoring of ART non-adherence were included. Data were analyzed using longitudinal linear mixed-level modeling, and mediation was tested via the Monte Carlo Method of Assessing Mediation. Appearance concerns were predictive of depression severity, γ = .31, SE = .076, 95 % CI [.16, .46], t = 4.1, p = .0001, and depression severity was predictive of ART non-adherence, γ = 3.3, SE = 1.3, 95 % CI [.8, 5.8], t = 2.6, p = .01. The effect of appearance concerns on ART non-adherence, however, was significantly mediated by depression severity, γ = 1.02, 95 % CI [.21, 2.1]. Appearance concerns are associated with depression severity, which in turn is associated with ART non-adherence. Integrative interventions addressing appearance concerns, depression and ART adherence are needed, as this is one potential pathway towards worse health outcomes in HIV-infected individuals.
Keywords: HIV/AIDS, Appearance, Body image, Depression, ART adherence, Lipodystrophy
Introduction
Appearance concerns are common among HIV-infected individuals, with studies indicating that nearly one third of HIV-infected men and one half of HIV-infected women are dissatisfied with their bodies (Sharma et al., 2006, 2007). Appearance-related concerns comprise a significant stressor for HIV-infected individuals (Blashill & Vander Wal, 2010; Huang et al., 2006; Marín et al., 2006; Santos et al., 2005; Tate & George, 2001; Theodore et al., 2011). One factor that can lead to appearance concerns among this population is changes in adipose tissue distribution, known generally as lipodystrophy (Huang et al., 2006; Marín et al., 2006; Sharma et al., 2006, 2007). This condition is associated with both HIV disease progression (Giralt et al., 2006) as well as sustained adherence to ART (Ammassari et al., 2002; Marín et al., 2006). Sixty percent of individuals experience moderate or severe changes in body fat (Guaraldi et al., 2008), including lipoatrophy (e.g., in the face, arms, legs, and/or buttocks) and/or lipohypertrophy (e.g., in the stomach, back of the neck, and/or breasts). Despite the high prevalence of appearance concerns among HIV-infected individuals, few studies have explored this construct among HIV-infected IDU (e.g., Blashill et al., 2012), representing a notable gap in the literature. Perhaps this gap is due to beliefs that self-care behaviors among HIV-infected IDU are overwhelmingly explained by their drug use, and thus, additional explanatory variables, such as psychosocial concerns, may be overlooked (e.g., Spire et al., 2007). Given that the majority of research on appearance concerns in HIV-infected individuals has focused on men who have sex with men (MSM), it is important to determine if this construct is similarly salient among IDU.
Although the advent of modern antiretroviral therapy (ART) in the late 1990s transformed HIV from a life-threatening disease into a chronic, manageable condition, HIV-infected individuals must maintain high levels of adherence in order to reap optimal treatment benefits (e.g., 95 % adherence for traditional antiretroviral medications, Low-Beer et al., 2000; Paterson et al., 2000; and 80 % for newer boosted protease inhibitors, Kobin & Sheth, 2011; Martin et al., 2008). Unfortunately, studies utilizing electronic pill caps have found that the average rates of adherence for HIV-infected individuals on ART regimens seem to be between 56 % and 65 % (Bangsberg et al., 2001, Genberg et al., 2012; Liu et al., 2001). Identifying possible psychosocial variables that impact adherence is crucial for both the treatment and prevention of HIV, as those with suppressed viral loads confer a significantly diminished risk of transmitting the disease to others (for a recent review, see Ambrosioni et al., 2011). This may be particularly salient for depressed IDU who are HIV-infected, as these characteristics predict suboptimal ART adherence that persists even throughout methadone treatment (Carrieri et al., 2003; Avants et al., 2001).
Importantly, appearance-related concerns have been associated with self-reported ART non-adherence, both cross-sectionally (Corless et al., 2005), as well as longitudinally (Ammassari et al., 2002; Duran et al., 2001; Glass et al., 2010; Plankey et al., 2009); however, there is a paucity of research explaining the mechanism behind this relationship. One possible mediator of the link between appearance concerns and ART non-adherence is depression. Appearance related concerns have been associated with depression in HIV-infected individuals (Marín et al. 2006; Sharma et al., 2006, 2007). Moreover, depression has been related to non-adherence, with a recent meta-analysis of 95 studies finding that those with depression were significantly less adherent to ART regimens than those without depression (Gonzalez et al., 2011). Given the bivariate relationships between depression and both appearance-related concerns and ART non-adherence, further examination of the mechanistic effect depression has on non-adherence in the context of appearance concerns is warranted.
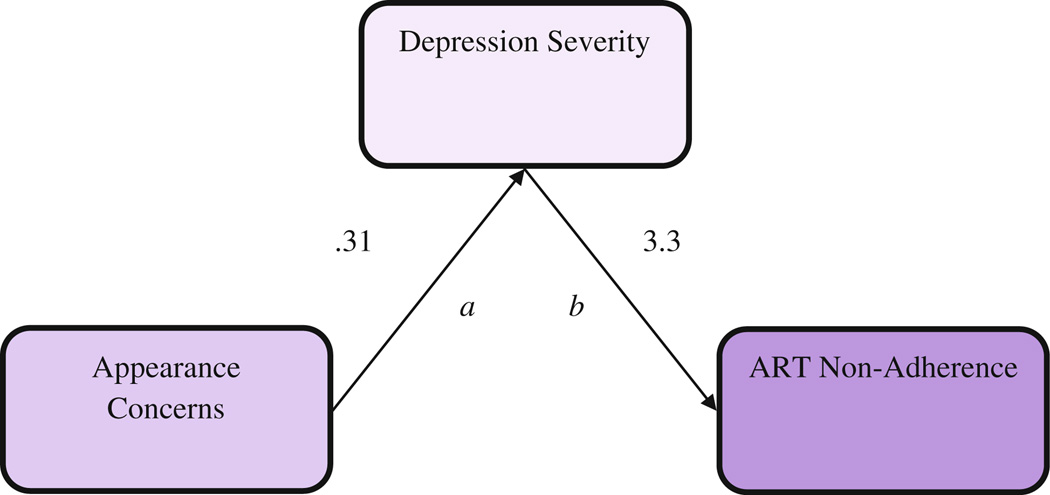
Our prior work is the only study we know of that has tested the relationship between depression, body dissatisfaction, and ART non-adherence (Blashill & Vander Wal, 2010). In this cross-sectional study, self-reported depression mediated the relationship between body dissatisfaction and self-reported non-adherence among HIV-infected MSM with high levels of body dissatisfaction. Nevertheless, the cross-sectional nature of this study precludes temporal inferences inherent to properly assessing mediational models (e.g., Kraemer et al., 2008). The current research builds on the existing literature by assessing, prospectively, over a 1 year period, the relationships between appearance concerns, ART non-adherence, and depression severity. Moreover, rather than rely on participant self-report data, we introduce objectively measured adherence measures through electronic pill cap monitoring, as well as a clinician-administered assessment of depression severity and appearance concerns. Given the literature to date, it was hypothesized that depression severity would significantly mediate the relationship between appearance concerns and ART non-adherence (Fig. 1).
Fig. 1.
Depression severity as a mediator between appearance concerns and ART non-adherence. Note The indirect effect = 1.02, 95 % CI [.21, 2.1]. Units = Unstandardized regression coefficients
Method
Participants
Participants were 89 HIV-infected individuals with comorbid depression, between the ages of 18 and 65, who were receiving treatment for opioid dependence. The current study is a secondary analysis of data from a randomized controlled efficacy trial investigating the use of cognitive behavioral therapy (CBT) for treating depression and enhancing ART adherence in those living with HIV. Enrollment occurred between July 2005 and October 2008. All participants were diagnosed with current or subsyndromal depressive disorder, were prescribed antiretroviral therapy, had a history of injection drug use, and were in opioid treatment during the past month (for more exhaustive study details, please see Safren et al., 2012). Sample characteristics are portrayed in Table 1.
Table 1.
Sociodemographic characteristics of participants
| Variable | N | % |
|---|---|---|
| Gender | ||
| Male | 54 | 61 |
| Female | 35 | 39 |
| Race | ||
| African American/Black | 26 | 33 |
| White | 38 | 48 |
| Native American | 2 | 3 |
| Ethnicity | ||
| Hispanic or Latino | 23 | 30 |
| Sexual orientation | ||
| Exclusively heterosexual | 60 | 79 |
| Bisexual | 5 | 7 |
| Exclusively homosexual | 2 | 3 |
| Employment | ||
| Full-time work or school | 3 | 4 |
| Part-time work or school | 8 | 10 |
| Neither work nor school | 17 | 22 |
| On disability | 53 | 67 |
| Education level | ||
| Eighth grade or lower | 12 | 15 |
| Partial high school | 21 | 26 |
| High school graduate/GED | 23 | 29 |
| College graduate | 6 | 8 |
| Psychiatric comorbity | ||
| At least one additional DSM-IV diagnosis | 55 | 62 |
| Two or more additional DSM-IV diagnoses | 37 | 42 |
| Additional DSM-IV diagnoses | ||
| Panic disorder | 17 | 30 |
| Generalized anxiety disorder | 10 | 18 |
| Social anxiety disorder | 8 | 14 |
| M | SD | |
| Age | 46.85 | 7.15 |
Percentages do not always sum to 100 due to overlap or some participants reporting more than one demographic category
Procedure
Participants were recruited through methadone treatment clinics, community outreach, and HIV clinics in the greater Boston area. All participants received a complete description of the study and provided written informed consent, and all study procedures were approved by the IRBs at Massachusetts General Hospital in Boston and Rhode Island Hospital in Rhode Island. Participants were seen for four major assessment visits over the course of the study, a baseline assessment (TI), 3 months from baseline (T2), 6 months from baseline (T3), and 12 months from baseline (T4). At each of these visits, participants completed clinician-administered measures of depression severity and physical symptoms related to HIV infection, as well as electronic pill cap evaluations for non-adherence (MEMS; Medication Event Monitoring System; AARDEX).
Measures
ART non-adherence
Participants were assigned a MEMS cap to use with the antiretroviral medication they were prescribed to use most frequently or reported having the most difficulty remembering to take. The MEMS cap recorded each time the bottle was opened; however, to account for doses that participants may have taken without using the bottle (e.g., if participants took out afternoon doses for later when they opened the bottle in the morning), doses were also counted as taken if participants could recount specific times in which they took their medications but did not use the pill cap (Liu et al., 2001, 2006; Llabre et al., 2006). This multiple method approach to measuring adherence has been found to increase the validity of adherence assessment (see Llabre et al., 2006). Although MEMS is an objective indicator, adherence may be underestimated if the MEMS cap is not used. Thus, using a corrected adherence score that accounts for doses taken without opening the bottle mitigates this concern. A dose was counted as missed if it was not taken within ±2 hours of a previously designated target time (Applebaum et al., 2009; Safren et al., 2009, 2012). One was subtracted from percent of adherence for purposes of converting the variable from an adherence metric to a non-adherence metric. This approach was taken to enhance the interpretability of the indirect effect (see below). That is, all relevant mediation variables (i.e., appearance concerns, depression severity, and ART non-adherence) were coded in a fashion that allowed higher scores to reflect poorer outcomes.
Depression severity
Clinicians rated the Clinical Global Impression (CGI) of severity, a rating of distress and impairment for depression on a scale from 1 (not ill) to 7 (extremely ill; NIH, 1985). In order to maximize measure validity, CGI scores were reviewed during audiotape supervision meetings with a licensed clinical psychologist. The CGI has been found to have strong convergent validity (r > .85) with other measures of depression, such as the Montgomery-Asberg Depression Rating Scale and Hamilton Depression rating scale (e.g., Leon et al., 1993; Müller et al., 2003).
Appearance-related HIV symptoms
At each visit, a clinician administered the 20-item ACTG Symptoms Distress Module (Justice et al., 2001), which assesses symptoms commonly reported among those on antiretroviral regimens. The measure asks participants to indicate whether they had each symptom during the past 4 weeks and to what extent it bothered them on a five-point scale (i.e., “0—I do not have this symptom”; “4—I have this symptom and it bothers me a lot”). Three of these items were appearance-related and assessed weight gain, weight loss, and hair loss. Specifically, items asked if participants had noticed “changes in the way your body looks such as fat deposits or weight gain,” “problems with weight loss or wasting,” or “hair loss or changes in the way your hair looks.” Responses to these items were extracted and combined to create a total score reflective of distress associated with appearance-related changes. For the current sample, internal consistency was α = .76.
Statistical analyses
The main analyses of the study, longitudinally examining the relationships between appearance concerns, depression severity, and ART non-adherence were conducted via linear mixed-effects modeling in PASW 18 (MIXED Procedure). The level-one variables represent the time variable (i.e., baseline, 3, 6, and 12 months post-baseline), in addition to other time-variant predictor variables: appearance concerns and depression severity, as well as time-variant covariates (CD4 count and viral load). Level-two variables included time-invariant covariates: study condition (CBT vs. TAU), age, and gender (see Table 2 for correlations among study variables). It should be noted that results did not significantly vary between adjusted and unadjusted models. Participants were treated as random effects, with random slopes and intercepts, whilst all remaining variables were fixed effects. In doing so, each participant was allowed to have a unique growth trajectory. Further, the diagonal covariance structure was chosen based on the best goodness-of-fit (as evaluated by the Akaike Information Criterion—AIC), compared to competing covariance structures. The restricted maximum likelihood—REML—estimation method was chosen in lieu of maximum likelihood (ML) estimation, as the former approach tends to result in unbiased estimates of the variances and covariances (West, 2009).
Table 2.
Correlations among study variables at baseline
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. |
|---|---|---|---|---|---|---|---|---|
| 1. ART non-adherence | 1 | .04 | .04 | −.10 | .28** | −.10 | .09 | .14 |
| 2. Appearance concerns | 1 | .41** | −.06 | −.02 | .14 | .01 | .12 | |
| 3. Depression severity | 1 | .06 | −.02 | −.14 | .03 | .22* | ||
| 4. CD4 | 1 | −.26* | .23** | .06 | −.09 | |||
| 5. Viral load | 1 | −.01 | −.22* | .05 | ||||
| 6. Tx condition | 1 | −.02 | .02 | |||||
| 7. Age | 1 | −.05 | ||||||
| 8. Gender | 1 |
p < .05;
p < .01.
Tx Condition 1 = CBT, 2 = TAU. Gender 1 = male, 2 = female
Longitudinal mediation was tested via the Monte Carlo Method of Assessing Mediation (MCMAM; Bauer et al., 2006; MacKinnon et al., 2004), which is a form of bootstrapping. Using the inputted parameter estimates and the associated standard errors, random draws from the a and b distributions are simulated and the product of these values is computed. This procedure is repeated a large number of times (i.e., 2,000) and the resulting distribution of the a * b values is used to estimate a 95 % confidence interval around the observed value of a * b. In doing so, the a * b path, or the indirect effect, allows one simple calculation to determine the presence of a mediated effect. The indirect (i.e., meditational) effect is interpreted as “statistically significant” if 0 is not contained between the lower and upper CIs. Bootstrapping methods are generally preferred over traditional methods of studying mediation (see Hayes, 2009; MacKinnon et al., 2004; Preacher & Hayes, 2008; Shrout & Bolger, 2002). In the current study, the MCMAM method was employed via software created by Selig and Preacher (2008).
Results
Preliminary analyses explored appearance concerns, depression severity, and ART non-adherence independently, as a function of time. Results indicated that depression severity significantly declined over time, γ = −.10, SE = .02, 95 % CI [−.13, −.06], t = −6.3, p = .0001. ART non-adherence worsened over time, γ = .68, SE = .30, 95 % CI [.08, 1.3], t = 2.2, p = .03. Conversely, appearance concerns remained stable over time, γ = −.001, SE = .01, 95 % CI [−.02, .02], t = −.07, p = .94.
The relationship between appearance concerns and depression severity (path a) emerged as significant, γ = .31, SE = .076, 95 % CI [.16, .46], t = 4.1, p = .0001, indicating that a one unit increase in appearance concerns was associated with a .31 increase in depression severity (on a 7-point scale). This finding indicates that reporting the highest level of appearance concerns compared to no appearance concerns corresponded to a 1.5 point increase in depression severity on the CGI (e.g., from a 3-“mildly depressed” to a 5-“markedly depressed”). The path between depression severity and ART non-adherence (path b) was also significant, γ = 3.3, SE = 1.3, 95 % CI [.8, 5.8], t = 2.6, p = .01, indicating that a one unit increase in depression severity was associated with a 3.3 increase in ART non-adherence (on a 100-point scale). Finally, to test the mediational effect of depression severity in the relationship between appearance concerns and ART non-adherence, the indirect effect (a * b) was assessed via the MCMAM, which yielded a significant effect, γ = 1.02, 95 % CI [.21, 2.1].
Discussion
Appearance concerns are prevalent among HIV-infected individuals, and are associated with increased depression (Blashill et al., 2012; Marín et al., 2006; Sharma et al., 2006, 2007) and ART non-adherence (Ammassari et al., 2002, Duran et al., 2001; Glass et al., 2010; Plankey et al., 2009). The findings from the current study revealed that among a depressed, opioid-dependent sample of HIV-infected men and women, the temporal relationship between appearance concerns and ART non-adherence was mediated by depression severity, even in a sample with elevated levels of depression, and hence a potentially restricted range, due to qualifying for a depressive diagnosis. Previous research in this area has largely relied on cross-sectional and/or self-report instruments and scant literature exist examining mechanisms behind the relationship between appearance concerns and ART non-adherence. Thus, the current study adds to the literature by providing a longitudinal mediational model with clinician-rated measures of distress and electronic monitoring of adherence.
Despite the additions to the literature the current study yields, several limitations are noted. Although the model in the current study was parsimonious and accounted for significant variance in ART non-adherence, more nuanced models should be also be explored. For instance, identifying the mechanisms and/or the conditions under which appearance concerns predict depression severity, as well as further exploring the link between depression severity and ART non-adherence would be important steps for future research. Further, while the CGI has been found to have strong convergent validity with other measures of depression, and CGI ratings were reviewed during supervision meetings with an independent rater, data on inter-rater reliability was not available. In addition, the current sample was exclusively comprised of HIV-infected individuals who were depressed, opioid-dependent, and largely heterosexual. Thus, findings may not translate to HIV-infected individuals who do not meet criteria for a depressive or opioid-dependent diagnosis, or men who have sex with men (MSM). However, cross-sectional research with gay and bisexual HIV-infected individuals has revealed similar findings (Blashill & Vander Wal, 2010), although longitudinal research focusing on these associations among MSM is needed, especially considering that MSM are likely to experience elevated levels of appearance concerns (Morrison et al., 2004). Also, the significant results of depression severity to non-adherence, even in a sample of individuals with pre-existing depression, speaks to the magnitude of this effect emerging even in the context of a possibly restricted range. An additional limitation was the assessment of ART adherence. A conservative window was applied in operationally defining non-adherence in the sample, a technique for which there is precedent (Applebaum et al., 2009; Safren et al., 2009, 2012). However, it is important to note that for modern ART regimens, there may be more flexibility with dosing time and a larger window may be used. Another limitation is the measurement of appearance concerns. Despite including three items, it did not assess specific body locations in regard to lipohypertrophy and lipoatrophy. There is preliminary evidence that, among women, abdominal hypertrophy is particularly related to ART non-adherence (Plankey et al., 2009). Given this, future research should explicitly assess lipohypertrophy and lipoatrophy as a function of specific regions of the body in the context of ART non-adherence. Moreover, participants’ perceived etiology of body changes were not assessed, and future research might examine individuals’ attributions of ART to body morphology and the subsequent relationship with adherence. However, the association of appearance concerns to both depression severity and to non-adherence in the current study more generally speaks to the relevance of appearance among HIV-infected individuals as an important part of quality of life and managing a chronic medical illness.
The findings from the current study have the potential to inform clinical practice. Not only do appearance concerns create elevated levels of depression and anxiety (Blashill et al., 2012), but as the results of the current study yield, through increased depression severity, predict ART non-adherence. ART non-adherence leads to disease progression and has increasingly become a concern for secondary prevention, as an individual with suppressed viral load confers significantly lower probability of transmitting HIV compared to those with a detectable viral load (Ambrosioni et al., 2011, Cohen et al., 2011). This is notable given that elevated levels of appearance concerns are associated with increased HIV sexual transmission risk behaviors (e.g., Wilton, 2009; Wingood et al., 2002).
An integrative cognitive behavioral intervention for depression and ART adherence (CBT-AD) has recently been developed and tested among HIV-infected populations (e.g., Safren et al., 2009, 2012). Generally, this intervention showed significant and sustained effects in reducing depressive symptoms, and at least acute effects on increasing ART adherence. Given that appearance concerns are common among HIV-infected individuals, and are prospectively associated with depression and ART non-adherence, researchers and clinicians should consider integrative interventions that not only address depression and ART adherence, but also explicitly address appearance concerns. Such interventions could not only have an impact on quality of life and depression, but also physical health and secondary HIV prevention.
Acknowledgments
Funding from this project came from the National Institutes of Health [R01 DA018603 to S.A.S]. Some investigator time was supported by the National Institutes of Health [K24 MH094214 to S.A.S.] and the Harvard University Center for AIDS Research/National Institutes of Health [5P30 AI060354-08 to A.J.B.].
Contributor Information
Aaron J. Blashill, Email: ablashill@partners.org, Department of Psychiatry, Massachusetts General Hospital, Boston, MA, USA; Harvard Medical School, 1 Bowdoin Square, 7th Floor, Boston, MA 02114, USA.
Janna R. Gordon, Department of Psychiatry, Massachusetts General Hospital, Boston, MA, USA
Steven A. Safren, Department of Psychiatry, Massachusetts General Hospital, Boston, MA, USA Harvard Medical School, 1 Bowdoin Square, 7th Floor, Boston, MA 02114, USA.
References
- Ambrosioni J, Calmy A, Hirschel B. HIV treatment for prevention. Journal of the International AIDS Society. 2011;14:28. doi: 10.1186/1758-2652-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammassari A, Antinori A, Cozzi-Lepri A, Trotta MP, Nasti G, Ridolfo AL. Relationship between HAART adherence and adipose tissue alterations. Journal of Acquired Immune Deficiency Syndromes. 2002;31:S140–S144. doi: 10.1097/00126334-200212153-00011. [DOI] [PubMed] [Google Scholar]
- Applebaum AJ, Reilly LC, Gonzalez JS, Richardson MA, Leveroni CL, Safren SA. The impact of neuropsychological functioning on adherence to HAART in HIV-infected substance abuse patients. AIDS Patient Care and STDs. 2009;23:455–462. doi: 10.1089/apc.2008.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avants SK, Margolin A, Warburton LA, Hawkins KA, Shi J. Predictors of nonadherence to HIV-related medication regimens during methadone stabilization. The American Journal on Addictions. 2001;10:69–78. doi: 10.1080/105504901750160501. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods. 2006;11:142–163. doi: 10.1037/1082-989X.11.2.142. [DOI] [PubMed] [Google Scholar]
- Blashill AJ, Vander Wal JS. The role of body image dissatisfaction and depression on HAART adherence in HIV positive men: Tests of mediation models. AIDS and Behavior. 2010;14:280–288. doi: 10.1007/s10461-009-9630-2. [DOI] [PubMed] [Google Scholar]
- Blashill AJ, Gordon JR, Safren SA. Appearance concerns and psychological distress among HIV-infected individuals with injection drug use histories: Prospective analyses. AIDS Patient Care and STDs. 2012;26:557–561. doi: 10.1089/apc.2012.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrieri M, Chesney M, Spire B, Loundou A, Sobel A, Lepeu G, et al. Failure to maintain adherence to HAART in a cohort of French HIV-positive injecting drug users. International Journal of Behavioral Medicine. 2003;10:1–14. doi: 10.1207/s15327558ijbm1001_01. [DOI] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N. Prevention of HIV-1 infection with early antiretroviral therapy. The New England Journal of Medicine. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corless IB, Kirksey KM, Kemppainen J, Nicholas PK, McGibbon C, Davis SM, et al. Lipodystrophy-associated symptoms and medication adherence in HIV/AIDS. AIDS Patient Care and STDs. 2005;19:577–586. doi: 10.1089/apc.2005.19.577. [DOI] [PubMed] [Google Scholar]
- Duran S, Savès M, Spire B, Cailleton V, Sobel A, Carrieri P. Failure to maintain long-term adherence to highly active antiretroviral therapy: The role of lipodystrophy. AIDS. 2001;15:2441–2444. doi: 10.1097/00002030-200112070-00012. [DOI] [PubMed] [Google Scholar]
- Genberg GL, Wilson IB, Bangsberg DR, Arnsten J, Goggin K, Remien RH. Patterns of antiretroviral therapy adherence and impact on HIV RNA among patients in North America. AIDS. 2012;26:1415–1423. doi: 10.1097/QAD.0b013e328354bed6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giralt M, Domingo P, Guallar JP, Rodriguez de la Concepción ML, Alegre M, Domingo JC, et al. HIV-1 infection alters gene expression in adipose tissue, which contributes to HIV-1/HAART-associated lipodystrophy. Antiviral Therapy. 2006;11:729–740. [PubMed] [Google Scholar]
- Glass TR, Battegay M, Cavassini M, De Geest S, Furrer H, Vernazza PL. Longitudinal analysis of patterns and predictors of changes in self-reported adherence to antiretroviral therapy: Swiss HIV Cohort Study. Journal of Acquired Immune Deficiency Syndromes. 2010;54:197–203. doi: 10.1097/QAI.0b013e3181ca48bf. [DOI] [PubMed] [Google Scholar]
- Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes. 2011;58:181–187. doi: 10.1097/QAI.0b013e31822d490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guaraldi G, Murri R, Orlando G, Giovanardi C, Squillace N, Vandelli M. Severity of lipodystrophy is associated with decreased health-related quality of life. AIDS Patient Care and STDs. 2008;22:577–585. doi: 10.1089/apc.2007.0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. [Google Scholar]
- Huang JS, Lee D, Becerra K, Santos R, Barber E, Mathews WC. Body image in men with HIV. AIDS Patient Care and STDs. 2006;20:668–677. doi: 10.1089/apc.2006.20.668. [DOI] [PubMed] [Google Scholar]
- Justice AC, Holmes W, Gifford AL, Rabeneck L, Zackin R, Sinclair G. Development and validation of a self-completed HIV symptom index. Journal of Clinical Epidemiology. 2001;54:S77–S90. doi: 10.1016/s0895-4356(01)00449-8. [DOI] [PubMed] [Google Scholar]
- Kobin AB, Sheth NU. Levels of adherence required for virologic suppression among newer antiretroviral medications. The Annals of Pharmacotherapy. 2011;45:372–379. doi: 10.1345/aph.1P587. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27:S101–S108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Shear MK, Klerman GL, Portera L, Rosenbaum JF, Goldenberg I. A comparison of symptom determinants of patient and clinician global ratings in patients with panic disorder and depression. Journal of Clinical Psychopharmacology. 1993;13:327–331. [PubMed] [Google Scholar]
- Liu C, Ostrow D, Detels R, Hu Z, Johnson L, Kingsley L, et al. Impacts of HIV infection and HAART use on quality of life. Quality of Life Research. 2006;15:941–949. doi: 10.1007/s11136-005-5913-x. [DOI] [PubMed] [Google Scholar]
- Liu H, Golin CE, Miller LG, Hays RD, Beck CK, Sanandaji S. A comparison study of multiple measures of adherence to HIV protease inhibitors. Annals of Internal Medicine. 2001;134:968–977. doi: 10.7326/0003-4819-134-10-200105150-00011. [DOI] [PubMed] [Google Scholar]
- Llabre MM, Weaver KE, Durán RE, Antoni MH, McPherson-Baker S, Schneiderman N. A measurement model of medication adherence to highly active antiretroviral therapy and its relation to viral load in HIV-positive adults. AIDS Patient Care & STDs. 2006;20:701–711. doi: 10.1089/apc.2006.20.701. [DOI] [PubMed] [Google Scholar]
- Low-Beer S, Yip B, O’Shaughnessy MV, Hogg RS, Montaner JSG. Adherence to triple therapy and viral load response. Journal of Acquired Immune Deficiency Syndromes. 2000;23:360. doi: 10.1097/00126334-200004010-00016. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marín A, Casado JL, Aranzabal L, Moya J, Antela A, Fernando D. Validation of a specific questionnaire on psychological and social repercussions of the lipodystrophy syndrome in HIV-infected patients. Quality of Life Research. 2006;15:767–775. doi: 10.1007/s11136-005-5001-2. [DOI] [PubMed] [Google Scholar]
- Martin M, Del Cacho E, Codina C, Tuset M, De Lazzari E, Mallolas J. Relationship between adherence level, type of the antiretroviral regimen, and plasma HIV Type 1 RNA viral load: A prospective cohort study. AIDS Research and Human Retroviruses. 2008;24:1263–1268. doi: 10.1089/aid.2008.0141. [DOI] [PubMed] [Google Scholar]
- Morrison MA, Morrison TG, Sager C. Does body satisfaction differ between gay men and lesbian women and heterosexual men and women?: A meta-analytic review. Body Image. 2004;1:127–138. doi: 10.1016/j.bodyim.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Müller MJ, Himmerich H, Kienzle B, Szegedi A. Differentiating moderate and severe depression using the Montgomery-Asberg depression rating scale (MADRS) Journal of Affective Disorders. 2003;77:255–260. doi: 10.1016/s0165-0327(02)00120-9. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. CGI (Clinical Global Impression) Scale. Psychopharmacological Bulletin. 1985;21:839–843. [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Plankey M, Bacchetti P, Jin C, Grimes B, Hyman C, Cohen M. Self-perception of body fat changes and HAART adherence in the Women’s Interagency HIV Study. AIDS and Behavior. 2009;13:53–59. doi: 10.1007/s10461-008-9444-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Safren SA, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected drug users: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2012;80:404–415. doi: 10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, O’Cleirigh C, Tan J, Raminani SR, Reilly LC, Otto MW, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychology. 2009;28:1–9. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos CP, Felipe YX, Braga PE, Ramos D, Lima RO, Segurado A. Self-perception of body changes in persons living with HIV/AIDS: Prevalence and associated factors. AIDS. 2005;19:S14–S21. doi: 10.1097/01.aids.0000191485.92285.c7. [DOI] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects [Computer software] 2008 Available from http://quantpsy.org/ [Google Scholar]
- Sharma A, Howard AA, Schoenbaum EE, Buono D, Webber MP. Body image in middle-aged HIV-infected and uninfected women. AIDS Care. 2006;18:998–1003. doi: 10.1080/09540120500521517. [DOI] [PubMed] [Google Scholar]
- Sharma A, Howard A, Klein R, Schoenbaum E, Buono D, Webber M. Body image in older men with or at-risk for HIV infection. AIDS Care. 2007;19:235–241. doi: 10.1080/09540120600774354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Spire B, Lucas GM, Carrieri M. Adherence to HIV treatment among IDUs and the role of opioid substitution treatment (OST) International Journal of Drug Policy. 2007;18:262–270. doi: 10.1016/j.drugpo.2006.12.014. [DOI] [PubMed] [Google Scholar]
- Tate H, George R. The effect of weight loss on body image in HIV-positive gay men. AIDS Care. 2001;13:163–169. doi: 10.1080/09540120020027323. [DOI] [PubMed] [Google Scholar]
- Theodore PS, Achiro RP, Duran REF, Antoni MH. Body dissatisfaction and methamphetamine use among HIV-positive gay and bisexual men: A pilot study. Substance Use and Misuse. 2011;46:1745–1749. doi: 10.3109/10826084.2011.618998. [DOI] [PubMed] [Google Scholar]
- West BT. Analyzing longitudinal data with the linear mixed models procedure in SPSS. Evaluation and the Health Professions. 2009;32:207–228. doi: 10.1177/0163278709338554. [DOI] [PubMed] [Google Scholar]
- Wilton L. A preliminary study of body image and HIV sexual risk behavior in black gay and bisexual men: Implications for HIV prevention. Journal of Gay & Lesbian Social Services. 2009;21:309–325. [Google Scholar]
- Wingood GM, Diclemente RJ, Harrington K, Davies SL. Body image and African American females’ sexual health. Journal of Women’s Health & Gender-Based Medicine. 2002;11:433–439. doi: 10.1089/15246090260137608. [DOI] [PubMed] [Google Scholar]