Craving is what makes addiction to drugs so difficult to overcome. The intense craving that follows a cue that has been previously associated with the drug, combined with a stressful state or a dysphoric state, represents an unstoppable force that leads to drug intake and relapse for most addicted individuals. However, although difficult, some people successfully control this craving, but the brain mechanisms responsible for this self-control are largely unknown. In the paper by Hayashi et al. (1), the authors unveil some of the neuropsychological mechanisms responsible for self-control by demonstrating that inactivation of the dorsolateral prefrontal cortex (dlPFC) decreases the craving that a smoker experiences when told that he will be able to smoke a cigarette a few minutes later, through inhibition of the process of valuation of drug-related stimuli mediated by the medial orbitofrontal cortex (mOFC), anterior cingulate cortex (ACC), and ventral striatum (VS). A two-stage process of cue reactivity is proposed by Hayashi et al., in which the mOFC tracks the subjective value of the drug, indexed by craving self-reports, and the dorsolateral prefrontal cortex (DLPFC) incorporates intertemporal availability and cue information to modulate the presumed mOFC value signal. This is a compelling conceptual advance consistent with existing models of frontal decision-making circuitry.
Drug cues, such as the sight or smell of cigarettes, provoke intense craving in smokers that can be very difficult to control and often lead to drug-seeking and -taking (2). Several brain regions, such as the OFC, ACC, and VS, have been shown to be activated in response to the presentation of drug cues. These structures have been hypothesized to encode not only the subjective value of drug-related cues but also the value and cost of the actions related to procuring the drug (3–5). The DLPFC has been hypothesized to combine these valuations together with other information, such as the drug context, drug availability, affective states, and outcome, to allow efficient decision-making (6). Dissecting the specific roles of these brain regions during craving and how they interact with each other is a challenging task in humans. The elegance of the study by Hayashi et al. (1) lies in its within-subject design that combines functional magnetic resonance imaging (fMRI) and focal inactivation of the DLPFC using transcranial magnetic stimulation (TMS) in smokers to allow them to obtain correlational and causal evidence of the role of the DLPFC in craving.
Hayashi et al. (1) first demonstrate that cue-induced craving for cigarettes is dramatically increased when subjects are instructed that they will be given the possibility to smoke immediately after testing (compared with 4 h later). This increased craving is associated with recruitment of the DLPFC (7). To test the causal role of the increased activity of the DLPFC in craving, Hayashi used TMS to inactivate the DLPFC during exposure to the cues and show that it prevents the increase in craving. This result alone is critical for the field because it demonstrates the causal relationship between activation of the DLPFC and cue-induced craving in a situation that is very similar to what abstinent smokers experience in the real world, in which smoking-related cues are often indicative of the imminent possibility to smoke. What is remarkable in the study by Hayashi et al. is that they did not stop here: they further investigated how inactivation of the DLPFC reduces craving through the modulation of other brain regions. They used fMRI to show that after inactivation of the dlPFC, the sensitivity of the mOFC, ACC, and VS to drug-related cues is dramatically attenuated. Moreover, the intensity of the cue-related signal in the mOFC predicts the individual’s craving intensity, suggesting that interindividual differences in self-control when experiencing craving may arise from interindividual differences in the capacity of the DLPFC to stimulate the mOFC (6).
These results are a critical step forward in our understanding of the brain mechanisms that underlie self-control during craving that may lead to better prevention and treatment of drug addiction in the future by identifying subjects with a specific neurocircuitry-based vulnerability to a lack of self-control.
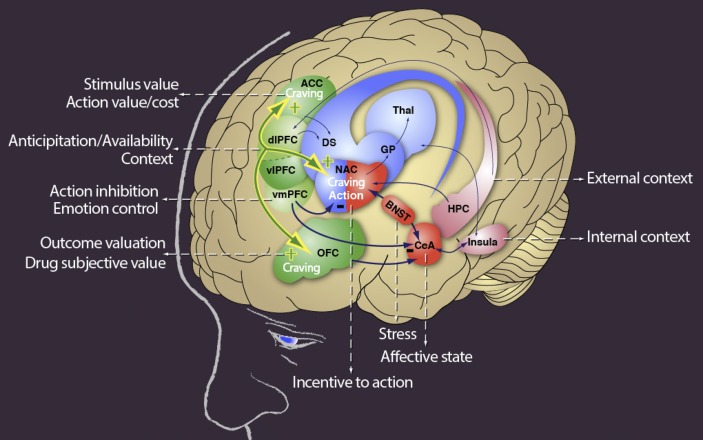
This report clearly demonstrates how hyperactivity of the DLPFC in response to contextual and drug-related cues increases craving in smokers and raises several questions. Drug addiction and pathological gambling have also been associated with general hypofunction of the ventromedial (vm) PFC (8–11). Considering the key role of the vmPFC in processing the consequences of future actions (12), inhibition of actions (13), and control of emotions (14), investigating the interaction between the vmPFC (processing a “STOP” signal) and DLPFC (processing a “GO” signal) would be important. For example, is the cue-induced hyperactivity of the DLPFC related to the decreased activity of the vmPFC? What is the contribution of stress and emotional states in the dysregulation of the proposed dlPFC, OFC, ACC, and VS? Cue-induced craving is often assumed to reflect the subjective value of drugs, but an alternative hypothesis is that cue-induced craving also reflects the emergence of a negative emotional state or, more likely, is augmented by the emergence of a negative emotional state. Research in animal models has demonstrated that cocaine-related cues produce an aversive state that drives subsequent cocaine intake (15), and key brain regions that are involved in processing stress and affective states, such as the amygdala and bed nucleus of the stria terminalis (BNST), are known to also be modulated by the PFC (Fig. 1). Therefore, hyperactivity of the dlPFC, OFC, ACC, and VS may also be associated with a facilitation of cigarette-related cue-induced negative emotions, thereby increasing the motivation to smoke to obtain relief from the negative affective
Fig. 1.
Neuroanatomy of drug craving. Craving-related information is processed by the OFC, ACC, and nucleus accumbens in response to drug-related cues. Craving-related information can be modulated by the external/internal context, stress, and affective states through the hippocampus, insula, central nucleus of the amygdala, and BNST. Activation of the DLPFC produces increased craving by potentiating the response to drug-related cues through its connection with the OFC, ACC, and nucleus accumbens. The vmPFC plays a key role in emotional control and the inhibition of action associated with poor deleterious consequences. CeA, central nucleus of the amygdala; DS, dorsal striatum; GP, globus pallidus; HPC, hippocampus; NAC, nucleus accumbens; Thal, thalamus.
The report by Hayashi et al. represents a major step forward in our understanding of the mechanisms that underlie self-control during craving.
state. Consistent with this hypothesis, deep brain stimulation of the PFC, particularly subregions that are known to modulate the OFC, ACC, and VS, are being investigated for the potential treatment of mood disorders, such as depression (16, 17). Considering the high comorbidity between substance abuse and mood disorders and the key role of the PFC in controlling the reward and stress systems, dysregulation of specific subregions of the PFC may be involved in both disorders.
Activation of the dlPFC, OFC, ACC, and VS during craving may reflect increases in the positive or negative reinforcing effects of drug-related cues. The report by Hayashi et al. represents a major step forward in our understanding of the mechanisms that underlie self-control during craving and leads to a converging hypothesis about how dysregulation of specific subregions of the PFC and striatum produces vulnerability in response to drug-related cues. Their results certainly pave the ground for the future development of novel treatments for drug addiction.
Footnotes
The authors declare no conflict of interest.
See companion article on page 4422.
References
- 1.Hayashi T, Ko JH, Strafella AP, Dagher A. Dorsolateral prefrontal and orbitofrontal cortex interactions during self-control of cigarette craving. Proc Natl Acad Sci USA. 2013;110:4422–4427. doi: 10.1073/pnas.1212185110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drummond DC, Tiffany ST, Glautier S, Remington B. Addictive Behaviour: Cue Exposure Theory and Practice. Chichester, UK: Wiley; 1995. pp. 1–17. [Google Scholar]
- 3.Kable JW, Glimcher PW. The neural correlates of subjective value during intertemporal choice. Nat Neurosci. 2007;10(12):1625–1633. doi: 10.1038/nn2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McBride D, Barrett SP, Kelly JT, Aw A, Dagher A. Effects of expectancy and abstinence on the neural response to smoking cues in cigarette smokers: An fMRI study. Neuropsychopharmacology. 2006;31(12):2728–2738. doi: 10.1038/sj.npp.1301075. [DOI] [PubMed] [Google Scholar]
- 5.Walton ME, Devlin JT, Rushworth MFS. Interactions between decision making and performance monitoring within prefrontal cortex. Nat Neurosci. 2004;7(11):1259–1265. doi: 10.1038/nn1339. [DOI] [PubMed] [Google Scholar]
- 6.George O, Koob GF. Individual differences in prefrontal cortex function and the transition from drug use to drug dependence. Neurosci Biobehav Rev. 2010;35(2):232–247. doi: 10.1016/j.neubiorev.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McBride D, Barrett SP, Kelly JT, Aw A, Dagher A. Effects of expectancy and abstinence on the neural response to smoking cues in cigarette smokers: An fMRI study. Neuropsychopharmacology. 2006;31(12):2728–2738. doi: 10.1038/sj.npp.1301075. [DOI] [PubMed] [Google Scholar]
- 8.Potenza MN, et al. Gambling urges in pathological gambling: A functional magnetic resonance imaging study. Arch Gen Psychiatry. 2003;60(8):828–836. doi: 10.1001/archpsyc.60.8.828. [DOI] [PubMed] [Google Scholar]
- 9.Potenza MN, et al. An FMRI Stroop task study of ventromedial prefrontal cortical function in pathological gamblers. Am J Psychiatry. 2003;160(11):1990–1994. doi: 10.1176/appi.ajp.160.11.1990. [DOI] [PubMed] [Google Scholar]
- 10.Reuter J, et al. Pathological gambling is linked to reduced activation of the mesolimbic reward system. Nat Neurosci. 2005;8(2):147–148. doi: 10.1038/nn1378. [DOI] [PubMed] [Google Scholar]
- 11.London ED, Ernst M, Grant S, Bonson K, Weinstein A. Orbitofrontal cortex and human drug abuse: Functional imaging. Cereb Cortex. 2000;10(3):334–342. doi: 10.1093/cercor/10.3.334. [DOI] [PubMed] [Google Scholar]
- 12.Bechara A. Risky business: Emotion, decision-making, and addiction. J Gambl Stud. 2003;19(1):23–51. doi: 10.1023/a:1021223113233. [DOI] [PubMed] [Google Scholar]
- 13.Ghazizadeh A, Ambroggi F, Odean N, Fields HL. Prefrontal cortex mediates extinction of responding by two distinct neural mechanisms in accumbens shell. J Neurosci. 2012;32(2):726–737. doi: 10.1523/JNEUROSCI.3891-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verdejo-García A, Bechara A. A somatic marker theory of addiction. Neuropharmacology. 2009;56(Suppl 1):48–62. doi: 10.1016/j.neuropharm.2008.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wheeler RA, et al. (2008) Behavioral and electrophysiological indices of negative affect predict cocaine self-administration. Neuron 13;57(5):774-785. [DOI] [PubMed]
- 16.Giacobbe P, Mayberg HS, Lozano AM. Treatment resistant depression as a failure of brain homeostatic mechanisms: Implications for deep brain stimulation. Exp Neurol. 2009;219(1):44–52. doi: 10.1016/j.expneurol.2009.04.028. [DOI] [PubMed] [Google Scholar]
- 17.Mayberg HS. Targeted electrode-based modulation of neural circuits for depression. J Clin Invest. 2009;119(4):717–725. doi: 10.1172/JCI38454. [DOI] [PMC free article] [PubMed] [Google Scholar]