Abstract
Situs inversus totalis (SIT) is a rare anomaly in which the abdominal and thoracic cavity structures are opposite their usual positions. Occasionally, a few patients with a combination of this condition and malignant tumors have been encountered. Recently, several laparoscopic operations have been reported in patients with SIT. We report a case of an 83-year-old man with situs inversus totalis who developed colon cancer after open distal gastrectomy. Laparoscopic hemicolectomy with radical lymphadenectomy in such a patient was successfully performed by careful consideration of the mirror-image anatomy. Techniques themselves was not different from those in ordinary cases. Thus, curative laparoscopic surgery for colon cancer in the presence of situs inversus totalis is feasible and safe.
Keywords: Situs inversus totalis, Laparoscopic surgery, Hemicolectomy, Colon cancer, Radical lymphadenectomy
INTRODUCTION
Situs inversus totalis (SIT) is a rare congenital anomaly and denotes complete right-left inversion of thoracic and abdominal viscera. Although laparoscopic experience in such patients often has been reported, the majority of reported cases are of laparoscopic cholecystectomy[1]. Reports of advanced laparoscopic surgeries are increasing in accordance with the progression of laparoscopic procedures. However, reports of laparoscopic surgery for colorectal malignancy are very few, and only 2 laparoscopic colorectal surgeries with lymphadenectomy have been reported[2,3]. Here we present a third case and a review of the literature.
CASE REPORT
In a follow-up after open distal gastrectomy performed for gastric cancer at the age of 77 years, an 83-year-old man with a history of SIT visited our department, reporting bloody stool. After colonoscopy yielded a diagnosis of transverse (splenic flexure) colon cancer, the patient was admitted to our hospital for further evaluation and surgical treatment. Abdominal examination revealed an upper midline scar. Laboratory examination confirmed anemia (red blood cell count, 396 × 104/mm2; hemoglobin, 11.1 g/dL; hematocrit, 34.6%). Serum carcinoembryonic antigen was not elevated (2.8 ng/mL; reference range, 0-5 ng/mL). Chest radiography showed dextrocardia and a right subphrenic gastric bubble (Figure 1A). Abdominal computed tomography revealed complete transposition of abdominal viscera, confirming SIT (Figure 1B). Barium enema and colonoscopy showed an ulcerated lesion in the splenic flexure of the transverse colon and polyps in the descending and transverse colon (Figure 2). Histologic examination of specimens from colonoscopic biopsy indicated adenocarcinoma. According to the findings described above, laparoscopic hemicolectomy with radical lymphadenectomy was performed.
Figure 1.
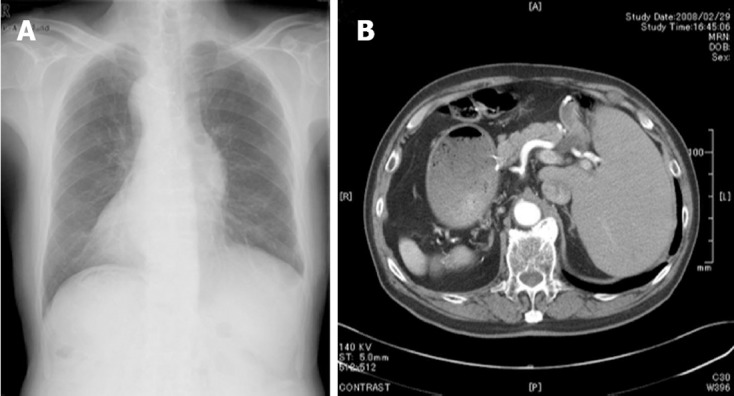
Chest radiography (A) and abdominal computer tomography (B) of the patient. A: Dextrocardia and a right subphrenic gastric bubble are evident; B: Complete transposition of abdominal viscera is shown, confirming situs inversus totalis.
Figure 2.
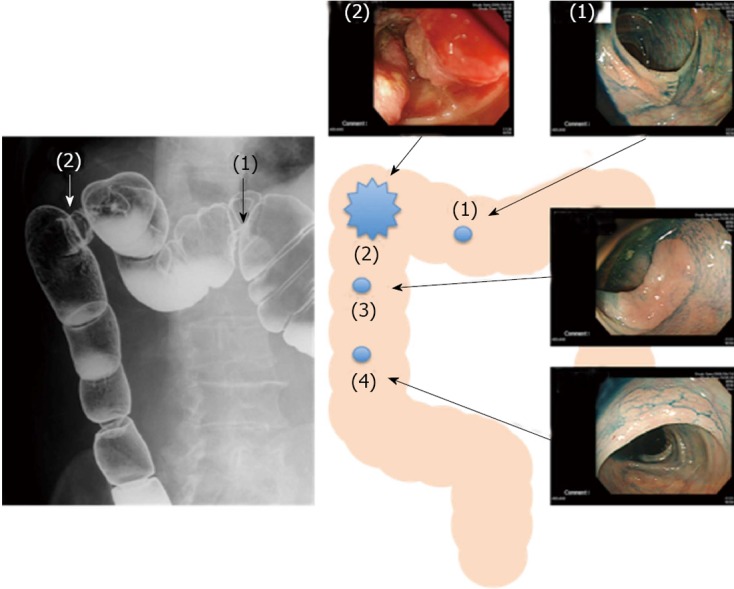
Barium enema and colonoscopy. Barium enema and colonoscopy showed an ulcerated lesion (2) in the splenic flexure of the transverse colon and a polyp (1) in the transverse colon. Polyps (3, 4) in the descending colon were not detected by barium enema, but were detected by colonoscopy.
After general anesthesia was induced, the patient was placed in a modified lithotomy position. The operator was situated on the right because of the need to dissect the adhesion between the liver and the transverse colon, the endoscopist was between the legs, and the first assistant was on the left side. A 12-mm infraumbilical port was placed using the Hasson technique and a 30° telescope was introduced into the peritoneal cavity. In the peritoneal cavity, we recognized the adhesion between the liver and the transverse colon. Additional ports were placed, including a 12-mm trocar in the right lower quadrant and two 5-mm trocars in the right upper quadrant for the operator, and a 12-mm trocar in the left upper quadrant and 5-mm trocar in the left quadrant for the assistant (Figure 3A). After the adhesion between the jejunum and the mesocolon was dissected carefully because the reconstruction in the last distal gastrectomy was a Billroth II via retrocolic root (Figure 3B), the transverse colon was dissected from the liver. The mesentery was incised from the area dissected between the jejunum and mesocolon to the origin of the middle colic artery. Radical lymphadenectomy was continued up to the root of the middle colic artery and the branch of the splenic flexure was divided (Figure 3C). The incision of the mesentery was extended up to the origin of the right colic artery (the left in an orthotopic patient) and the branch of the right colic artery was divided (Figure 3D). After mobilization up to the descending colon, dissection and reconstruction of the colon were performed extracorporeally through a 5-cm skin incision continued to the right port using a functional end-to-end stapling method. Operating time was 402 min and blood loss was 230 mL. Compared to orthotopic patients, the operating time was longer and the blood loss greater because of the intraabdominal adhesions after open distal gastrectomy. According to the Japanese classification of colorectal carcinoma[4], macroscopically, the tumors were a 51 mm × 41 mm type 3 lesion in the transverse colon, a 38 mm × 17 mm IIc lesion in the transverse colon, and 17 mm × 13 mm and 10 mm × 10 mm IIa lesions in the descending colon. Histological examination of the resected specimens disclosed a moderately-differentiated adenocarcinoma (type 3, pSS, pN0, sH0, sP0, cM0, ly1, v0, Stage II) and well-differentiated adenocarcinomas (IIa and IIc lesions, pM, pN0, sH0, sP0, cM0, ly0, v0, stage 0) (Figure 4). After an uneventful postoperative course, the patient was started on a clear liquid diet on the 4th postoperative day and was discharged on the 16th postoperative day according to the clinical pathway at our hospital.
Figure 3.
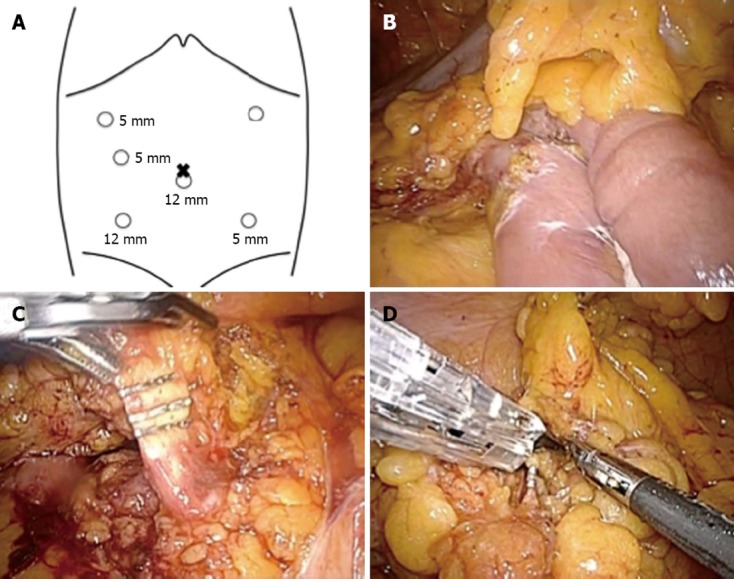
Sites of trocar placement and intraoperative finding. A: A camera was inserted into the subumbilical area through a 12-mm trocar; B: The reconstruction in the last distal gastrectomy was Billroth II via retrocolic root; C: Radical lymphadenectomy was continued up to the root of the middle colic artery and the branch of the splenic flexure was divided; D: The branch of the right colic artery (the left in an orthotopic patient) was divided.
Figure 4.
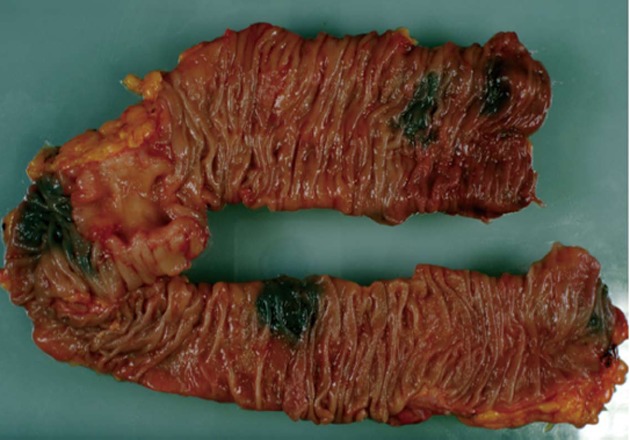
Macroscopic findings. The main tumor was a 51 mm × 41 mm type 3 lesion in the transverse colon. A 38 mm × 17 mm IIc lesion was in the transverse colon and 17 mm × 13 mm and 10 mm × 10 mm IIa lesions were in the descending colon.
DISCUSSION
Situs inversus (SI) is a rare congenital anomaly in which the organs are transposed from their normal site to the opposite side of the body. SI may involve transposition of thoracic or abdominal organs, or both. SIT denotes complete inversion of thoracic and abdominal viscera[5-7]. The incidence is 1 in 5000-20 000[1]. Apart from a genetic predisposition, no etiologies have been established, and SI itself has no pathophysiologic significance[6,7]. Cardiovascular malformations (8%) and bronchiectasis (10%) are often present[8]. With SIT, abnormal vascularization of the arteries and veins is common; therefore, the preoperative confirmation of any abnormal vascularization is very important. Particularly with laparoscopic surgery, it is important to determine the presence of vascular anomalies on preoperative CT or angiography. In the report of Iwamura et al[6], several cases having a combination of SIT and malignant tumors, such as cancer of the lung, stomach, liver, colon, and rectum, were described. Including our case, only 7 cases with SIT complicated by colorectal malignancy have been reported in the English literature[2,3,6,7,9,10].
Surgical procedures, especially laparoscopic procedures, are considered more difficult in patients with SIT than in other patients because of the mirror-image anatomy. Thus, because laparoscopic surgery in patients with SIT is a technical challenge for the surgeon, it remains relatively rare. However, it has been performed more often in recent years in such patients, but most of these procedures have been laparoscopic cholecystectomies[1], and only 10 advanced laparoscopic procedures have been described (Table 1)[2,3,5,11-17]. Furthermore, for malignancy, only 4 laparoscopic procedures have been reported[2,3,13,14]. While laparoscopic colorectal surgery has recently become a standard procedure, only 5 (only 2 for colorectal cancer) reports of laparoscopic surgery for colorectal disease with SI have been published[2,3,5,11,12]. The reason is considered to be that the number of SI patients is so small, and the anatomic abnormality has made surgeons reluctant to attempt laparoscopic surgery.
Table 1.
Reports of advanced laparoscopic surgery for situs inversus totalis
| Operation | Author | Year | Disease | Operation time (min) | Blood loss (mL) |
| Laparoscope-assisted distal gastrectomy | Futawatari et al[14] | 2010 | Gastric cancer | 300 | 350 |
| Yamaguchi et al[13] | 2003 | Gastric cancer | 280 | 240 | |
| Laparoscopic gastro bypass | Ahmed et al[16] | 2006 | Obesity | 160 | ND |
| Wittgrove et al[15] | 1998 | Obesity | ND | ND | |
| Laparoscopic sleeve gastrectomy | Cateline et al[17] | 2006 | Obesity | ND | ND |
| Laparoscopic hemicolectomy | Fujiwara et al[2] | 2007 | Colon cancer | 191 | 60 |
| Laparoscopic sigmoidectomy | Jobanputra et al[12] | 2007 | Diverticulitis | ND | ND |
| Kobus et al[5] | 2004 | Diverticulitis | 180 | ND | |
| Davies et al[11] | 2002 | Diverticulitis | ND | ND | |
| Laparoscopic total mesorectal excision | Huh et al[3] | 2010 | Rectal cancer | 250 | 120 |
Only 10 advanced laparoscopic procedures have been reported, 4 of which were for malignancies. ND: Not determined.
The positions of the operator, assistant, and trocar did not differ from those in orthotopic patients. We found no technical difficulties using the laparoscopic procedure because we had acquired images of the anatomy. Attention to the fundamentals of laparoscopic procedures, such as the careful handling of devices and keeping the operating field dry, is very important. Of course, accurate preoperative anatomic assessment and careful preoperative planning of laparoscopic procedures (positions of operator, assistants, and trocar sites as well as instrumentation) are needed to ensure a safe and smooth procedure, as mentioned in previous reports of laparoscopic surgery in patients with SI[5,11]. Although advanced surgical skill is required for radical lymphadenectomy in a patient with SIT, careful recognition of the mirror image anatomy is more important. In the present patient, we had obtained information on vascularization of the arteries and veins from operative records of the previous open distal gastrectomy. Although this operation was after open surgery, we could safely perform the laparoscopic procedure by adhering to the fundamentals of laparoscopic procedures.
In summary, laparoscopic colectomy for colon cancer in a patient with SIT can be performed safely by a skilled surgeon and surgical team after thorough preoperative planning including assessment of the anomaly. This procedure is a feasible option to enable such patients to benefit from minimally invasive surgery.
Footnotes
P- Reviewers Plummer JM, MD, Hotta T, Tiberio GA S- Editor Wen LL L- Editor A E- Editor Xiong L
References
- 1.Nursal TZ, Baykal A, Iret D, Aran O. Laparoscopic cholecystectomy in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech A. 2001;11:239–241. doi: 10.1089/109264201750539772. [DOI] [PubMed] [Google Scholar]
- 2.Fujiwara Y, Fukunaga Y, Higashino M, Tanimura S, Takemura M, Tanaka Y, Osugi H. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol. 2007;13:5035–5037. doi: 10.3748/wjg.v13.i37.5035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huh JW, Kim HR, Cho SH, Kim CY, Kim HJ, Joo JK, Kim YJ. Laparoscopic total mesorectal excision in a rectal cancer patient with situs inversus totalis. J Korean Med Sci. 2010;25:790–793. doi: 10.3346/jkms.2010.25.5.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Japanese Society for Cancer of the Colon and Rectum. Japanese classification of colorectal carcinoma. 2nd ed. Tokyo: Kanehara and Co. Ltd; 2009. [Google Scholar]
- 5.Kobus C, Targarona EM, Bendahan GE, Alonso V, Balagué C, Vela S, Garriga J, Trias M. Laparoscopic surgery in situs inversus: a literature review and a report of laparoscopic sigmoidectomy for diverticulitis in situs inversus. Langenbecks Arch Surg. 2004;389:396–399. doi: 10.1007/s00423-004-0500-0. [DOI] [PubMed] [Google Scholar]
- 6.Iwamura T, Shibata N, Haraguchi Y, Hisashi Y, Nishikawa T, Yamada H, Hayashi T, Toyoda K. Synchronous double cancer of the stomach and rectum with situs inversus totalis and polysplenia syndrome. J Clin Gastroenterol. 2001;33:148–153. doi: 10.1097/00004836-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Goi T, Kawasaki M, Yamazaki T, Koneri K, Katayama K, Hirose K, Yamaguchi A. Ascending colon cancer with hepatic metastasis and cholecystolithiasis in a patient with situs inversus totalis without any expression of UVRAG mRNA: report of a case. Surg Today. 2003;33:702–706. doi: 10.1007/s00595-002-2567-y. [DOI] [PubMed] [Google Scholar]
- 8.Fonkalsrud EW, Tompkins R, Clatworthy HW. Abdominal manifestations of situs inversus in infants and children. Arch Surg. 1966;92:791–795. doi: 10.1001/archsurg.1966.01320230139025. [DOI] [PubMed] [Google Scholar]
- 9.Brillantino A, Marano L, Schettino M, Torelli F, Izzo G, Cosenza A, Monaco L, Porfidia R, Reda G, Foresta F, et al. Report of a rare case of colon cancer complicated by anomalies of intestinal rotation and fixation: a case report. Cases J. 2009;2:6555. doi: 10.4076/1757-1626-2-6555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uchida H, Kawamura YJ, Takegami K, Matsuda K, Watanabe T, Masaki T, Minami M, Muto T. Colon cancer complicated by vascular and intestinal anomaly. Hepatogastroenterology. 2004;51:156–158. [PubMed] [Google Scholar]
- 11.Davies H, Slater GH, Bailey M. Laparascopic sigmoid colectomy for diverticular disease in a patient with situs inversus. Surg Endosc. 2003;17:160–161. doi: 10.1007/s00464-002-4231-4. [DOI] [PubMed] [Google Scholar]
- 12.Jobanputra S, Safar B, Wexner SD. Laparoscopic diverticular resection with situs inversus totalis (SIT): report of a case. Surg Innov. 2007;14:284–286. doi: 10.1177/1553350607311089. [DOI] [PubMed] [Google Scholar]
- 13.Yamaguchi S, Orita H, Yamaoka T, Mii S, Sakata H, Hashizume M. Laparoscope-assisted distal gastrectomy for early gastric cancer in a 76-year-old man with situs inversus totalis. Surg Endosc. 2003;17:352–353. doi: 10.1007/s00464-002-4504-y. [DOI] [PubMed] [Google Scholar]
- 14.Futawatari N, Kikuchi S, Moriya H, Katada N, Sakuramoto S, Watanabe M. Laparoscopy-assisted distal gastrectomy for early gastric cancer with complete situs inversus: report of a case. Surg Today. 2010;40:64–67. doi: 10.1007/s00595-009-4007-8. [DOI] [PubMed] [Google Scholar]
- 15.Wittgrove AC, Clark GW. Laparoscopic gastric bypass for morbid obesity in a patient with situs inversus. J Laparoendosc Adv Surg Tech A. 1998;8:53–55. doi: 10.1089/lap.1998.8.53. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed AR, O’malley W. Laparoscopic Roux-en-Y gastric bypass in a patient with situs inversus. Obes Surg. 2006;16:1392–1394. doi: 10.1381/096089206778663670. [DOI] [PubMed] [Google Scholar]
- 17.Catheline JM, Rosales C, Cohen R, Bihan H, Fournier JL, Roussel J, Bénichou J. Laparoscopic sleeve gastrectomy for a super-super-obese patient with situs inversus totalis. Obes Surg. 2006;16:1092–1095. doi: 10.1381/096089206778026352. [DOI] [PubMed] [Google Scholar]


