Introduction
Republication of one of John Lea’s 1849–51 cholera studies1 forces us to admit that our interest in it stems mainly from its influence on John Snow’s ‘Broad Street pump’ and South London studies 5 years later.2 That Snow’s work ultimately survived to become a part of the epidemiological canon,3,4 whereas Lea’s sank quickly into 150 years of obscurity (arguably until 20005), is worth examination. But examination is complicated by a century of Snow-hagiography that may mislead us. The comments below consider men like Lea and Snow in the larger context of their mid-19th century times, in which trying to elucidate the obscure causes of epidemic diseases was among the most important challenges of the day, but an undertaking almost inevitably doomed to failure. To take such a look back in time, we must forget most of what we know about infectious diseases like cholera, and try to accept the mysteries of such diseases as inexplicable in their entirety by any single theory.
To fairly review what Lea, Snow and their contemporaries thought about cholera, when they set out to theorize about its occurrence and spread, would take hundreds of pages, and the results would still be incomplete, contradictory, confusing and paradoxical. In Lea’s/Snow’s time there was not a single major epidemic, let alone communicable, disease for which substantial evidence existed for the theoretical concept of infection, as we use the term today: denoting a microbial cause. Whereas communicability of many diseases had long been accepted, infection was merely one of several theories to explain it, and each theory had multiple perplexing variations. Though widely discussed, the idea of infection as an explanation for communicability was crowded out by competing theories; cholera could not even be shown to be communicable, let alone infectious. Theories of cholera communicability were considered to be particularly weak in their failures to explain such clearly observed phenomena as the repeated appearances of new cholera case patients who had never been exposed to ill persons. To posit microbial disease causation of cholera was to go even further out on a limb.
Nevertheless, by 1849 suspicions about infectious aetiologies of a number of diseases were slowly growing. (Infection would eventually be established by Koch’s 1876 characterization of the full infectious cycle of Bacillus anthracis). Since the 1820s, greatly improved microscope lenses had led to the association of several skin/mucous membrane diseases with various fungi or protozoans, e.g. candidiasis and trichomoniasis. But aetiological proof of microbe/disease associations was frustratingly elusive: microorganisms were everywhere, in almost every sample from every ill or well patient, and from the environment—water, air, soil etc., and there was (yet) no standardized means of cultivating them to speciate them to identify which were harmless and which pathogenic, or to link specific microorganisms to specific diseases. The pitfalls of over-interpreting microbial associations were many, as Snow’s colleague William Budd (1811–80) learned in 1849 when he unwisely joined colleagues in announcing a fungal cause of cholera. Embarrassingly, it turned out to be a microscopic artefact.6
To complicate matters, the relationship between contagion and infection seemed not to be the same for all diseases, and the few stable clues available were misleading and irreconcilable between those diseases. Indeed, cholera was probably the worst possible potentially infectious disease any theorist could choose to study in the mid-19th century, because evidence about its mode of spread was so maddeningly contradictory.7–12 For example, cholera was seemingly contagious at the population level—it infected only humans and strictly followed the movement of humans over thousands of miles via multiple means of conveyance and, despite wind and weather, never travelled faster than humans travelled. Yet at the individual and local levels, common experiences argued against cholera contagion from person to person or via fomites. As physicians and laymen all knew, intense contact with cholera victims did not normally result in either nosocomial cases or even substantial numbers of secondary cases; yet at the same time, well people at intermediate distances, often lacking any contact with index cases whatsoever, were among cholera’s frequent secondary victims. Quarantine had no evident effect; already-affected troops marching into new locales did not transmit cholera to newly-exposed troops; chains of person-to-person spread could not be found; time intervals between successive cases were seemingly random; sudden outbreaks associated with low attack rates often featured widely dispersed cases with almost simultaneous disease onsets; outbreaks appeared in strictly circumscribed urban, but less commonly in rural locales, and prevailed for only very brief periods of time; cholera tended to recur decades later in the very same locales it had struck earlier (e.g. in 1832 and 1849); and human inoculation with cholera material did not produce disease.
Theorists were perplexed. Depending on one’s point of view, cholera appeared simultaneously to be a contagious and a miasmatic disease, or neither contagious nor miasmatic; the American Medical Association hedged that ‘cholera is portable but not contagious’. [The term ‘miasmatic’ refers to hypothesized disease-causing elements in the ambient air, e.g. gases. Many diseases believed to be miasmatic are now known to be infectious by non-miasmatic means, prominently including those with indirect mechanisms of transmission such as waterborne (e.g., cholera, typhoid), insect borne (e.g. yellow fever, malaria) and by other intermediate and environmental means of disease spread (e.g. human gastrointestinal or inhalation anthrax)]. Other missing pieces of the puzzle whose absences confounded disease theorists in the mid-19th century included infectivity before disease onset and after disease resolution, infectivity without recognizable clinical illness, carrier states, environmental persistence of infectious agents, and other epidemiological features that, if known, might have helped make sense of things. But they were not known, and could not be learned without the ability to reliably identify specific aetiological agents or to prove disease associations using standardized reproducible methods and agreed-upon criteria. The brightest minds of science, medicine and public health in the mid-19th century kept going over the facts about cholera occurrence again and again, in thousands of published arguments spanning more than five decades, always to find them irreconcilable. It was into this confusing mix that Lea, Snow and men of their day ventured, certain that any theory could be refuted by any number of observations.
Even so, in retrospect we can see that prescient theories and critical observations about the cause of cholera were becoming plentiful when Snow was still a youth. Cholera’s first major appearance in Europe and the western hemisphere, in 1831–32, led to hundreds of studies and multiple/variable/evolving theories about disease occurrence that foreshadowed and greatly influenced thinking about infectious diseases two decades later. Cholera theorists of the 1840s all knew the cholera literature of the 1830s, and in many ways carried on that earlier work where it had left off, as if there had not been a two-decade hiatus. In this writer’s view, it was during the 1831–32 cholera pandemic (Snow was then 18 years old) that recognizably ‘modern’ epidemiology was born, when Parisian physicians and health workers ably characterized cholera occurrence in person, place and time in large open populations, publishing in ‘real time’ line lists of cases (typically, columns of sequentially-appearing cases with associated demographic data such as age, sex and date/place of onset), and calculated morbidity and mortality rates, case-fatality rates and attributable risks, and statistically examined such suspected risk factors as age, sex, socio-economic status, occupation and crowding.13–19
Studying Cholera
In 1832 America, the ravages of pandemic cholera were as fatal as almost anywhere else. John Lea’s home town of Cincinnati—then the sixth largest US city—was struck particularly hard, experiencing the explosive deaths of about 4% of its population. At the epidemic’s peak, in October 1832, Lea’s brother-in-law William Latta (1798–1832) died, presumably of cholera. It was around this time that Lea apparently developed and began arguing for the prevention of cholera by the use of safe drinking water, and promulgating his ‘geological theory’ of cholera aetiology.
The voluminous pre-1849 cholera literature available to Lea and Snow documents that waterborne transmission—or at least association with impure water and/or sewage exposure—had long been in the minds of medical/scientific and lay observers, as the two men would both later summarize.1,2 As early as the late 1820s, for example, Searle had reported abandonment of a contaminated water tank to control cholera in India.20 Observers of 1831–32 had immediately proposed that cholera was waterborne and caused by a communicable agent,20,21 and began controlling presumably contaminated water to prevent it. In Cincinnati, cabinetmaker Henry Boyd (1802–86), who had bought his way out of slavery, proposed in 1832 that the agent of cholera was waterborne and preventable by boiling all drinking water.22 At the same time Cincinnati’s leading physician, indeed one of the country’s most prominent physicians, Daniel Drake (1785–1852), theorized that cholera was caused by ‘a small microscopic agent—an animalcule [i.e. a microorganism]’,23 although at the time neither Drake nor anyone else was able to distinguish specific aetiological agents among the many microbes seen in cholera dejecta.
Snow eventually learned that Lea’s work implicating impure water in the aetiology of cholera had led the St Louis, Missouri, Board of Health to remove pump handles in 1849, and that some American cities had been so convinced of a possible association that during cholera epidemics they had prohibited well-water use entirely.24 And, of course, Snow knew that the cesspool under the Broad Street pump had been dug up 17 years earlier, in 1838, because it had been, even back then, contaminating the pump water.25 Newspaper articles and letters to the editor about sewage and impure water as suspected determinants of cholera were ubiquitous during and after the 1830s, and remained so in Europe and America during the cholera pandemic beginning in 1848 [e.g. see the numerous letters in The Times (London) during the early days of the Broad Street pump outbreak in September 1854, or a Scientific American editorial on the work of Lea, which also cited Snow’s South London incidence study26].
By 1848 John Lea had apparently collected so much observational and recorded evidence about the association of cholera with drinking water from wells and springs, and its prevention by the use of rainwater or boiled water,1,5,24,27,28 and in some cases its prevention or cessation by pump handle removal,1,5,24,29 that in July of that year—before cholera had fully struck England, but in anticipation of its devastations—he wrote with supporting evidence to urge the British government and other European governments to provide safer water for their subjects.24,30 According to an American newspaper, the French were more receptive to Lea’s suggestions than the British,31 but it does not appear that any European government acted strongly on Lea’s recommendations.
Among Lea’s lines of reasoning were not only his own studies, but his documentation of the rarity of cholera on both the Caribbean Islands and southern US locales that used only cistern water, and his recording of experiences on southern US plantations. On many such plantations, slave owners and other White families using rainwater cisterns escaped cholera while, at the same time, slave families using well or river water were severely attacked; furthermore, when pure rainwater was subsequently provided to slaves they too escaped cholera. Lea also pre-dated Snow in arguing evidence of a similar association between exposure to impure water and endemic non-cholera diarrhoeal complaints; observations of lower cholera incidences in brewery workers in the US, England and France; and other investigations in which drinking water source was directly associated with cholera occurrence. Lea speculated that it was limestone in water that caused cholera, perhaps in part because ‘hard water’ had traditionally been associated with gastrointestinal complaints in newcomers to the Ohio River Valley.
Who was John Lea?
A challenge in evaluating John Lea’s ideas and efforts is that very little is known about Lea other than his four 1850/1851 scientific papers on cholera,1,24,27,28 and several of the apparently numerous letters on cholera prevention he wrote to newspapers and magazines over a period of at least three decades (1832–56; see, for example, references 32 and 33). A successful Cincinnati merchant in the wholesale import business, Lea has been referred to as a geologist and a meteorologist, but there is no evidence he had scientific training in either of these fields. His younger brothers Thomas Gibson Lea (1785–1844) and Isaac Lea (1792–1886), however, became a prominent botanist and a prominent geologist, respectively. After marrying the daughter of patriot/publisher Matthew Carey (1760–1839), Isaac Lea went on to found the famed publishing house of Lea and Febiger, and then became one of America’s most prominent scientists and eventually President of the American Association for the Advancement of Science (AAAS). But John Lea seems never to have received a scientific degree or held a scientific position, other than contributing weather data to the city and the newspapers, and being a member of a horticultural society.
John Lea (Figure 1) was born to a prominent Irish Quaker family in the area of Wilmington, Delaware, during the last year of the Revolutionary War, and grew up among the battlefields on which George Washington had once fought. Lea’s grandfather, James Lea senior (1723–98), a friend of Washington, owned a fleet of ships that traded with Ireland and the West Indies; the Lea brothers knew from childhood the very tree under which the wounded Lafayette had lain. After the 1807 trade wars, Lea’s parents and some of his 10 siblings moved to Pittsburg, while John Lea established himself in business in Philadelphia. In 1822 John Lea joined the bulk of the Lea family in moving from Pennsylvania to Cincinnati, a boom town exploding in growth with the coming of steamboat trade and travel on the Mississippi and Ohio Rivers. Lea spent the rest of his life there in a prosperous family business.
Figure 1.

(A) An undated photograph of John Lea (1782–1862), a prominent Cincinnati merchant who lived through the city’s two major cholera epidemics of 1832 and 1849. Lea spoke privately and publicly about his ‘geologic’ theory of cholera etiology, that cholera could be entirely prevented by drinking only boiled or rain-derived water or, when available, safe city water. He wrote letters to newspapers, magazines and foreign governments, activities he apparently kept up over three decades. None of those communications written in or around 1832 have yet been identified. When cholera returned in 1849 Lea, then 67 years old, once again began an energetic campaign. (B) John Lea’s grave site, Spring Grove Cemetery, Cincinnati. (C) The trademark engraving of Cincinnati cabinetmaker and cholera theorist Henry Boyd on one of his four-poster beds. It is conceivable that Boyd influenced Lea, or vice versa
Though not a scientific investigation with statistical proofs, Lea’s 1849 Sycamore Street, Cincinnati study is nonetheless persuasive in arguing for the role of unsafe water in cholera occurrence.1,24,27,28 The cholera epidemic had begun in the lower parts of the city, smouldered for months, then exploded during the summer and eventually spread upward along Sycamore Street, several blocks above Lea’s business, and moved simultaneously up Vine Street, parallel to Sycamore and six blocks to the west. This was an area of predominantly German immigrant workers, containing a crowded residential area west of Sycamore/east of Vine Street. Although we do not know the denominator of residents in most of the Sycamore households, we do know that all but one residence was a single family unit, and most presumably housed one or more adults and one or more children (the other house contained ‘several families’; a ‘grocery and drinking house’ is not considered in the calculations below). Being a residential neighbourhood of working-class families living in houses of similar size, there is no reason to suspect greatly different denominators of persons per household (Lea estimated a mean of six persons), or differential case-fatality rates in those households for which attack rates were not reported.
In evaluating Lea’s Cincinnati study, it is helpful to know that in 1849 Cincinnati had a new safe water system fed mostly through iron pipes from a holding reservoir filled by intake from an upstream Ohio River source. (Curiously, the reservoir was lined with limestone rock, a fact that Lea omits in discussing his ‘geological theory’.) The cholera outbreak Lea studied, however, took place in the upper hilltop reaches of Sycamore Street (Figure 234), from two to six blocks above the old county line at Liberty Street. Presumably the city water system did not reach that high up, since all of the dwellings in his study were supplied by either rainwater cisterns, springs or wells. Lea records that in 12 households using unsafe spring or well water there were 42 deaths from cholera (3.5 deaths per household), whereas in five residences using only rainwater there was only one cholera death (0.2 deaths per household), and that death was of a previously ill child believed to have drunk from a nearby spring-fed fountain. Lea cites another 1849 observation prefiguring Snow’s studies. On a particular square off Washington Avenue, St Louis, Missouri, 25 households used water from a single pump, whereas the remaining two households took water from a hydrant supplied by (presumably safe) piped-in city water. More than 90 cholera deaths occurred in the households using the pump water, whereas no one even became ill in the homes using safe city water.
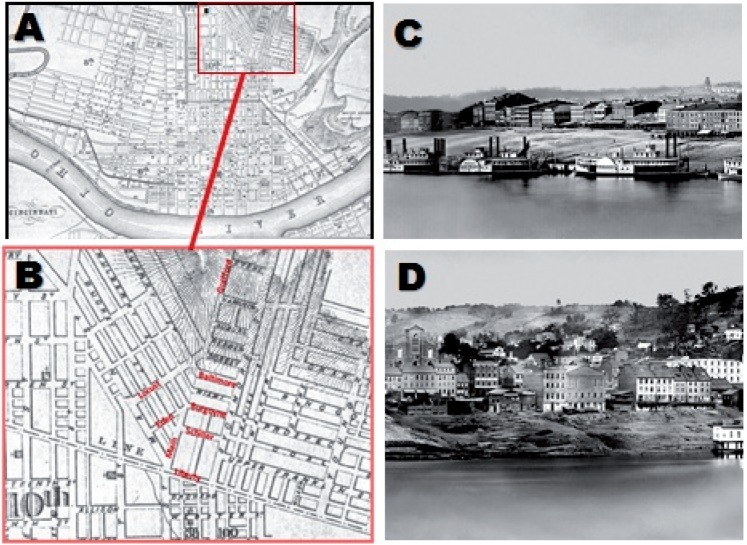
Figure 2.
(A) Map of Cincinnati in 1850;34 the inset is an enlargement of the Sycamore Street epidemic area. (B) Inset of map (A) showing upper Sycamore Street, where the outbreak Lea studied took place; missing street names were added (in red) in 2013. Lea’s hand-drawn map1 clearly differs from this official city map, most notably by Lea’s omission of Sycamore’s cross streets. (C) An 1848 daguerreotype showing Cincinnati several months before the 1849 cholera epidemic. In the 1849 epidemic, Ohio and Mississippi River steamboats like those moored along the waterfront spread cholera throughout the central United States. (D) The Sycamore Street neighbourhood Lea studied cannot be clearly delineated but is in the distance, high up in the central hills above the Jenks & Cline sawmill in the lower centre of the image
Proving Cholera's Cause
Lea’s findings would not have been surprising to anyone following cholera closely, as studies and observations from around the world linking cholera to impure water had become so numerous by that time that no one even bothered to collect them. Among other such observations, Sutherland’s 1849 report of pump water and cholera in Salford made it statistically clear that impure pump water was highly associated with cholera occurrence.35,36 Higher cholera mortality rates in London associated with the Southwark and Vauxhall compared with the Lambeth water supply had even been statistically documented and published37 at least a year before Snow’s famous study.2 Possible links between cholera and sewage were just as plentiful,38 and had been so for decades. Since the earliest well-documented epidemic, in India in 1817, cholera had been associated with low-lying areas, poor drainage of water and filthy conditions. Well before 1850, ideas about a relationship between cholera, water and sewage were ‘in the air’ and widely discussed by physicians and the public alike.
With so much overwhelming—if scientifically imperfect—evidence, and with so many lives at stake, it might be assumed that obsessively focused and perseverant men like Lea and Snow would have found ready audiences for their aetiological associations and proposed preventive measures. But Lea, an amateur self-styled geologist with shaky views about biology—who suspected cholera was being caused by minerals in the water, not by microorganisms—received a mixed and occasionally hostile reception from the medical/scientific community. Nevertheless, Lea’s major scientific publication on cholera prevention was favourably reviewed in at least some quarters, and was supposedly ‘copied by the medical journals of all schools’.39 In early June 1849, apparently in response to Lea's campaign, a Cincinnati newspaper urged citizens to start boiling all drinking water, but no study was done to find out whether this had a beneficial effect. On 3 January 1854, Ohio Senator (later Treasury Secretary and Supreme Court Chief Justice) Salmon P. Chase (1808–73) even introduced a motion on the US Senate floor that John Lea’s works be submitted for unspecified action to a special committee chaired by Senator (later Secretary of State) Hamilton Fish (1808–93). Seven months later, Fish’s committee ‘discharged … [Lea’s work] … from further consideration’,40,41 and aside from Snow’s citation of it, the scientific life work of John Lea virtually disappeared for over a century and a half.
Even Snow, a highly regarded physician, was initially ignored by all but a handful. How could this be so? The answer may lie in a constellation of confusing factors: (1) the overall epidemiological confusion surrounding cholera and indeed all infectious/miasmatic diseases; (2) the plethora of competing explanations for the cause of cholera—each of which seemed to explain some but not all of the agreed-upon observations about cholera’s behaviour; (3) a general inability to appreciate that infection might operate not only directly via contagious person-to-person transmission but also, at the same time, indirectly via ‘miasmatic’ environmental sources such as water, food or (of no relevance to cholera, but important for other important diseases being theorized about) insect vector and animal reservoirs; (4) the lack of a working model for the yet-to-be-established ‘germ theory’; (5) the fact that neither Lea’s nor Snow’s theories tried to, or were capable of, explaining all salient observations about cholera; and (6) in Snow’s case, the relative newness of statistics in characterizing population risk factors. With no biological or other scientific basis to understand confusing and contradictory epidemiological observations, there were seemingly enough well known ‘facts’ around to falsify almost any theory.
Because of its direct bearing on thinking about the mode of transmission of cholera and other infectious diseases, it is here worth noting that well before the cholera epidemics Lea and Snow investigated, spot maps such as the ones they constructed had become common means of envisioning disease clustering and inferring mode of communication.12 They had been repeatedly used since at least the 1790s, when American public health physician Valentine Seaman’s (1770–1817) spot map showed that yellow fever was apparently not being spread by contagion.42 Many other spot maps had also been used to describe the epidemiology of the two major (apparently) miasmatic diseases of the day, yellow fever and cholera (Figure 310,11,34,42–54), as well as other diseases.
Figure 3.
Details from some early (before Snow) cholera and yellow fever spot maps. (A) In 1830, Russian entomologist Vasily Zubkov [B. Zoubkoff (1799–1862)], a close friend of the poet Alexander Pushkin (1799–1837), used a spot map43 to show that cholera was being spread neither by contagious nor miasmatic means, but that cases clustered in low-elevation residences near a river/canal in a flood plain area, associated with apparent waterborne hospital transmission and with consumption of contaminated vegetables. (B) In 1837, working with colleague George Busk (1807–66), William Budd’s older brother George Budd (1808–82), who 21 years later would care for John Snow as he lay dying of a stroke, studied a hospital ship outbreak of cholera using spot maps of cases on three deck levels44 to detail cholera’s epidemiological characteristics. (C) In 1853 Wilson Jewell (1800–67) investigated yellow fever by constructing line lists, calculating time intervals between cases and drawing lines between each successive case on a map to demonstrate that typical person-to-person spread was not easily detectable.45 D. Henry W. Acland (1815–1900) compared locations of cholera cases in Oxford in 1832, 1849 and 1854, providing evidence46 about a tendency of cholera to recur in the same locales that had been struck in earlier epidemics
By 1850 the causes of epidemic disease spread had long been a subject of vital interest to physicians and health personnel, and spot maps/similar maps—often with associated line lists—had become familiar ways of visualizing epidemiologicl events with a bearing upon proposed or doubted theories of disease spread. Indeed, epidemic maps seem to have been assembled in the early weeks of the Broad Street outbreak, before Snow’s investigations and before his own spot map of 4 December 1854; in any case, a Broad Street outbreak map without ‘spots’ of cases was used and published with textual information about case location during the autumn of 1854,55 a common representation of the time that historian Lloyd Stevenson12 has referred to as a ‘verbal map’.
The Legacies of Lea and Snow
With these considerations in mind, we must ask how Lea relates to Snow in the evolution of epidemiological understanding. Lea was among the first to correctly establish an unambiguous association between water source and cholera occurrence by organized observational study, and among the first to propose a valid means of preventing it. That Lea had at least a sense of the scientific approach is suggested by an article he wrote before cholera had even appeared in 1848, in which he previewed the investigative approach he would take later that year: ‘We must be guided in our conclusions by facts only, and not attempt to build up theories on any other foundation … [we must] trace the source of the destroyer [cholera], examine the peculiarities of the regions he has shunned, scrutinize those he has attacked …’ 56. But despite considering suggestive evidence, there is no strong evidence that Lea suspected the involvement of either sewage contamination or a microbial aetiology (in fact, he believed the association indicated a limestone-associated mineral risk), and he did not conduct systematic scientific studies using statistical reasoning. To modern readers, Lea’s ‘geological theory’, which implicated ‘hard water’ from limestone formations, seems at best unscientific. The term ‘geological theory’ was not Lea’s but that of his Cincinnati contemporary Daniel Drake, who had used the term to evoke earlier theories of Robert Boyle (1627–91). Boyle had posited that epidemics arose from release of underground mineral gases [While discussing geological theories of cholera in 1832, Drake nevertheless made it clear that he believed cholera was caused not by geological risk factors but by ‘animalcules’ (microorganisms)].23 And despite the name of his theory, Lea’s main emphasis for almost 30 years was not on the cause of cholera—geological or otherwise—but on an absolute means of preventing it, by drinking only rain/cistern water or boiled water.
Both Lea and Snow were tenacious and thorough in assembling diverse practical and historical evidence, and in inducing what the cumulative data might mean. Neither tried to explain all of the disparate observations by a single theory; rather, both men seem to have instinctively appreciated the value of forming a theory that, although not necessarily capable of explaining every stray ‘fact’, did at least explain most of the important ones using evidence that could not easily be falsified by other ‘facts’. Snow was undoubtedly influenced by Lea’s investigations, but went much further to posit microbial contamination of water, and to develop a more complete, and ultimately correct, picture of the entire cycle of cholera communication, from human transmission to environmental persistence to human acquisition, and did so with statistical support. In Snow’s writings about cholera his use of the term ‘communication’ is noteworthy because it envisions and encompasses a complex cycle of human/environmental relationship that subsumes aspects of both contagious transmission and (seemingly) miasmatic acquisition. Its main points could satisfy even those who doubted infectivity. Examination of Snow’s 1855 argument is a marvel of reasoning and epidemiological puzzle-fitting. Lea provided important pieces of that puzzle.
Accepting that, however insightful or comprehensive, little about Snow’s cholera communication theories was completely original, and indeed that he had been familiar with related/pre-existing theories and observations advanced by men such as Lea, Sutherland and others, should we therefore dismiss Snow as an unoriginal thinker? Some scholars have done so, including those whose well deserved praise of Snow’s colleagues William Budd and Henry Whitehead have seemed at times to implicitly dismiss Snow.57–59 I would argue, however, that Snow remains important in the history of science, although perhaps for different reasons than those offered in hagiographic accounts. Snow may not have invented epidemiology or solved the puzzle of cholera on his own, but he did go well beyond what others had achieved. As Lea had tried to do a few years earlier, Snow first reduced the puzzle of cholera, unsolvable in its totality, to a manageable size. He then focused on a limited theory that would cover both transmission from an affected person to acquisition by an unaffected person, as well as any steps between them—without depending too heavily on the then vague concepts of infection or miasmata—going on to collect and analyze information about cholera occurrences, reducing all of those data to a potential mechanism that could not be easily falsified by other data. That very few things Snow is known to have written or said about cholera turned out to be wrong is perhaps less a testimonial to his (undoubted) genius than an indication of his ability to focus on the critical elements of unsolved problems, and to understand them without being swayed by a need to address less robust ‘facts’.
Snow died before his theories were fully accepted. It is not clear whether the slow approval of his views had by that time (1858) reached a point where he could be confident they would eventually prevail. Having left no protégé, and few friends other than the quirky Benjamin Ward Richardson (1828–96), it is perhaps not coincidental that several of the men who had worked with him on the Broad Street outbreak, at least two of whom had initially been sceptical of his theories, would keep Snow’s work alive. John George French (1804–87), Edwin Lankester (1814–74) and Henry Whitehead (1825–96) all became Snow’s witnesses, whether out of respect for his work, affection for him or because of the shared experience in what was surely the most shocking and unforgettable event of their lifetimes: the Broad Street outbreak. These men kept Snow’s name and his work alive into the microbial era and into the time of identification of the cause of cholera (1884), allowing him to be rediscovered by a new generation of microbiologists, epidemiologists and sanitarians fully capable of appreciating his work and his genius, among them William Henry Welch (1850–1934), William Thompson Sedgwick (1855–1921), Milton Rosenau (1869–1946) and Henry Harold Scott (1874–1956). These observers of later generations, like those of the current era, came to marvel that with so few tools and such imperfect data, John Snow was able to figure out so much, so well, and to prove it to the satisfaction of observers a century and a half after his time.
Had Snow lived until 1880, he would surely have read the words of British biologist Thomas Huxley (1825–95), who wrote about science in general what might have been more cogently said about epidemiology, that it ‘is nothing more than trained and organized common sense’.60 One can easily imagine that Snow saw his theory of cholera communication as just common sense—indeed, the evidence suggests that he never quite understood why others failed to come to the same conclusions he did—and he was tenacious in trying again and again to persuade with evidence from multiple ‘angles’. Even his quixotic, unsuccessful self-nomination for a cholera discovery cash prize seems less like a moment of hubris than evidence of unshakable optimism and a willingness to persevere in the lonely pursuit of an important cause.
Among his distinguishing attributes, ably discussed by Paneth and Colleagues,61 Snow was a consummate, obsessive puzzle-fitter who emerged from cholera’s confusing conundrums to choose the right puzzle, of the right size and no bigger, and to fit its pieces perfectly together, with no pieces left over. Men who came before Snow, like Lea, had identified and sorted out some of those puzzle pieces, but none were able to complete a puzzle of any size. Lea too deserves credit for making and tirelessly promoting, until the end of his life, an observation of and a preventive mechanism against cholera that, if paid attention to or subjected to epidemiological study, could have led to the prevention of almost all epidemic cholera cases, saving countless lives. As a newspaper of the era enthused: ‘Let Mr. Lea and his theory be fairly put on trial, and if pure water proves to be a prophylactic equal to vaccination, he may claim a niche by the side of Jenner, in the pantheon of human benefactors’.62 Unfortunately, no such study was conducted.
Although it is not clear whether Lea’s conviction that drinking pure water completely prevented cholera was his alone, or whether the original observation should be credited to Henry Boyd or unknown others, it was clearly Lea who tirelessly promoted the implications for public health. Boyd, the former slave, went on to become a prominent and prosperous cabinetmaker whose furniture pieces are today highly prized antiques (Figure 1C). It is not known whether Boyd ever advanced his cholera theory after 1832, or whether he and Lea ever discussed it or even knew each other. In 2012, a distant echo of Lea’s theory resounded when prominent US scientists reportedly explained the ongoing Haitian cholera epidemic not by post-earthquake importation of cholera, but by activation of existing cholera strains as a result of, among other factors, earthquake-induced disruption of the limestone bedrock, resulting in increased riverine alkalinity that supported Vibrio cholerae growth.63
In reflecting on Lea and Snow and others of their era, it is worth remembering that for them the quest to solve the puzzle of cholera, the most important fatal epidemic disease of its time, was of commanding moral importance, and that all other considerations such as their methods, beliefs, reputations, personal goals and personal achievements were subordinate. The legacy of John Snow is not that he removed the handle from the Broad Street pump—he did not, and it was soon put back on, and the Broad Street cholera epidemic had already been waning in any case—but that he taught us the value of applying ‘common sense’, so much less common than we would like to think, to piece together population/environmental data about the occurrence of a deadly disease of great human significance. In essence, John Snow taught us above all else how to be good, effective and consequential epidemiologists.
Acknowledgements
I acknowledge Alexander Klosovsky for research about Vasily Zubkov, Nigel Paneth for discussions over the years about John Snow and his work, Eva Åhrén for translation of and discussions about Panum’s cholera studies, Betty Murgolo and the document retrieval staff of the NIH Library, and the staffs of the Library of Congress, the History of Medicine Division, National Library of Medicine, and the Cincinnati Historical Society.
Conflict of interest: None declared.
References
- 1.Lea J. Cholera, With Reference to the Geological Theory: A Proximate Cause – A Law By Which It Is Governed – A Prophylactic. Cincinnati, OH: Wright, Ferris & Co.; 1850. Reprinted in Int J Epidemiol 2013;42:30–42. [DOI] [PubMed] [Google Scholar]
- 2.Snow J. On the Mode of Communication of Cholera. 2nd edn. London: J. Churchill; 1855. [Google Scholar]
- 3.Vinten-Johansen P, Brody H, Paneth N, Rachman S, Rip M. Cholera, Chloroform, and the Science of Medicine: A Life of John Snow. Oxford: Oxford University Press; 2003. [Google Scholar]
- 4.Davey Smith G. Commentary: Behind the Broad Street pump: aetiology, epidemiology and prevention of cholera in mid-19th century Britain. Int J Epidemiol. 2002;31:920–32. doi: 10.1093/ije/31.5.920. [DOI] [PubMed] [Google Scholar]
- 5.Morens DM. Snow and the Broad Street pump: a rediscovery [Letter] Lancet. 2000;356:1688–89. doi: 10.1016/S0140-6736(05)70399-8. [DOI] [PubMed] [Google Scholar]
- 6.Brown PE. John Snow – the autumn loiterer. Bull Hist Med. 1961;35:519–28. [PubMed] [Google Scholar]
- 7.Anonymous. History of the rise, progress, ravages, &c. of the blue cholera of India. Lancet. 1831;2:241–84. [Google Scholar]
- 8.Literary Gazette Editor. Cholera morbus. The Literary Gazette, and Journal of the Belles Lettres, Arts, Sciences. 1831;773:731–33. [Google Scholar]
- 9.Budd G. Cholera. In: Tweedie A, Gerhard WW, editors. A System of Practical Medicine Comprised in a Series of Original Dissertations. Vol. 4. Philadelphia: Lea & Blanchard; 1841. pp. 158–86. [Google Scholar]
- 10.Dickson SH. On the progress of the Asiatic cholera during the years 1844-45-46-47-48. With remarks. The New-York Journal of Medicine. 1849;2:2–20. map. [Google Scholar]
- 11.Gaulter H. The Origin and Progress of the Malignant Cholera in Manchester, Considered Chiefly in their Bearing on the Contagiousness and the Secondary Causes of the Disease. To which are Added some Remarks on the Treatment. London: Longman, Rees, Orme, Brown, Green, and Longman; 1833. [Google Scholar]
- 12.Stevenson LG. Putting disease on the map. The early use of spot maps in the study of yellow fever. J Hist Med. 1965;20:226–61. doi: 10.1093/jhmas/xx.3.226. [DOI] [PubMed] [Google Scholar]
- 13.Benoiston de Châteauneuf L-F, Chevallier J-B, Devaux L, et al. Rapport sur la marche et les effets du choléra-morbus dans Paris et les communes rurales du département de la Seine, par la commission nommée, anec l'approbation de M. le Ministre du commerce et des travacx publics, par MM. les Préfets de la Seine et de police. Paris: Imprimerie royale; 1834. [Google Scholar]
- 14.Caffe P-L-B. Notice statistique pour servir à l'histoire du choléra-morbus de Paris. Journal universel et hebdomadaire de médecine et de chirurgie pratiques et des institutions médicales. 1832;7:157–64. 205–17, 317–34. [Google Scholar]
- 15.Paillard H. Histoire statistique du choléra-morbus qui a régné en France en 1832; suivie de réflexions sur les causes et la propagation de cette épidémie, de 40 tableaux contenant des résultats obtenus par chacun des médecins de l'Hôtel-Dieu, et le chiffre des malades et des morts en France, classés par jour et par arrondissement. Paris: J.-B. Baillière; 1832. [Google Scholar]
- 16.Tacheron C-F. Statistique médicale de la mortalité du choléra-morbus dans le XIe arrondissement de Paris, pendant les mois d'avril, mai, juin, juillet et août 1832; ou documens et observations hygiéniques devant servir à l'étude de cette épidémie. Paris: Béchet jeune; 1832. [Google Scholar]
- 17.Moreau F-M. Histoire statistique du choléra-morbus dans le quartier du faubourg Saint-Denis (5me arrondissement) pendant les mois d'avril, mai, juin, juillet, août et septembre. Paris, Mairie du cinquième arrondissement: 1833. [Google Scholar]
- 18.Villermé L-R. Note sur les ravages du choléra-morbus dans les maisons garnies de Paris, (I) depuis le 29 mars jusqu'au 1er août 1832, et sur les causes qui paraissent avoir favorisé le développement de la maladie dans un grand nombre de maisons. Annales d'hygiène publique et de médecine légale. 1834;11:385–409. two appended tables. [Google Scholar]
- 19.Morens DM. ‘Epidemiology is born:’ cholera in Paris, 1832. In: Bernier RH, St. Pierre JL, editors. Epidemiology Wit & Wisdom. Roswell, GA: Epidemiology Monitor Press; 2000. pp. 98–101. [Google Scholar]
- 20.Searle C. In Searle C. Cholera, Its Nature, Cause, and Treatment; With Original Views Physiological, Pathological, and Therapeutical, In Relation to Fever; the Action of Poisons on the System; &c. Section II. London: John Wilson; 1830. Extracts from various sources adduced in proof of malaria being the cause of cholera in India: and direct evidence of its having been so, in a recent instance in this country, etc. pp. 51–61. [Google Scholar]
- 21.Limousin-Lamothe J-M. Lettre sur les animalcules considéres comme cause du choléra. Gaz méd. 1832;3:232–33. [Google Scholar]
- 22.Hammond C. Liberty Hall and Cincinnati Gazette. Cholera. Thursday, 18 October 1832, p. 3. [Google Scholar]
- 23.Drake D. A Practical Treatise on the History, Prevention and Treatment of Epidemic Cholera. Cincinnati: Corey and Fairbank; 1832. [Google Scholar]
- 24.Lea J. Cholera - the geological theory. Western Lancet. 1851 February:89–97. [Google Scholar]
- 25.The Cholera Inquiry Committee. Report on the Cholera Outbreak in the Parish of St. James, Westminster, During the Autumn of 1854. London: J. Churchill; 1855. [Google Scholar]
- 26.Anonymous. Opinions regarding the cause of cholera. Scientific American. 1856;11:336. [Google Scholar]
- 27.Lea J. Cholera – mistakes corrected – geological theory. Western Lancet. 1851 February:217–21. [Google Scholar]
- 28.Lea J. Geological theory of cholera. The Eclectic Medical Journal. 1850;2 366–73, 401–12. [Google Scholar]
- 29.Anonymous. Reports and evidence on water-supply, 1821, 1828, 1834, 1840. The Quarterly Review. 1850;174:468–502. [Google Scholar]
- 30.Anonymous. Rain water in Asiatic cholera. New Jersey Medical Reporter and Transactions of the New Jersey Medical Society. 1853;6:131. [Google Scholar]
- 31.Anonymous. A prophet is without honor in his own country. South-Western American. 1852;4 Edition 1, 3 November. [Google Scholar]
- 32.Lea J. Blue limestone. Saturday Evening Post. 1849 Vol. 11. [Google Scholar]
- 33.Lea J. Milwaukee Daily Sentinel. A preventive for cholera. Tuesday, 13 December 1853, p. 1, column C. [Google Scholar]
- 34.Mendenhall G. An account of cholera as it appeared in Cincinnati during the year 1850. Trans Amer Med Assoc. 1851;14:181–200. [Google Scholar]
- 35.Sutherland J. EXTRACTS from Appendix (A) [of] the Report of the General Board of Health on the Epidemic Cholera of 1848 & 1849. Int J Epidemiol. 2002;31:900–07. doi: 10.1093/ije/31.5.900. [DOI] [PubMed] [Google Scholar]
- 36.Sutherland J. Appendix (A) to the Report of the General Board of Health on the Epidemic Cholera of 1848 & 1849. London: W. Clowes & Sons; 1850. [DOI] [PubMed] [Google Scholar]
- 37.Anonymous. The London water supply and the cholera. Med Times Gaz. 1854;8:88–89. [Google Scholar]
- 38.Smee A. On the production of cholera by insufficient drainage, with remarks on the hypothesis of an altered electrical state of the atmosphere. Lancet. 1849;2:232–33. [Google Scholar]
- 39.Juettner O. 1785–1909 Daniel Drake and His Followers: Historical and Biographical Sketches. Cincinnati: Harvey Publishing Company; 1909. [Google Scholar]
- 40.Thirty-Third Congress. Perfected Proceedings. First session. In Senate, Tuesday, January 3, 1854. The Daily Globe [Boston] 1854;6:26. [Google Scholar]
- 41.Thirty-Third Congress. First session. In Senate, Wednesday, August 2, 1854. The Daily Globe [Boston] 1854;6:212. [Google Scholar]
- 42.Seaman V. An inquiry into the cause of the prevalence of the yellow fever in New-York. Med Repos. 1798;1:315–32. [Google Scholar]
- 43.Zoubkoff B, [Zubkov VP] Observations faites sur le choléra morbus dans le quartier de la Yakimanka, à Moscou, en 1830. Moscow: Auguste Semen; 1831. [Google Scholar]
- 44.Budd G, Busk G. Report of twenty cases of malignant Cholera, that occurred in the seaman’s hospital-ship, Dreadnought, between the 9th and 28th of October, 1837. Med-Chir Trans. 1838;21:152–86. doi: 10.1177/095952873802100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jewell W. Yellow or Malignant Bilious Fever in the Vicinity of South Street Wharf, Philadelphia, 1853. Philadelphia: T. K. and P. G. Collins; 1853. [Google Scholar]
- 46.Acland HW. Memoir on the Cholera at Oxford, in the Year 1854, With Considerations Suggested by the Epidemic. London: J. Churchill; 1856. [Google Scholar]
- 47.Pascalis-Ouviere F. A Statement of the Occurrences During A Malignant Yellow Fever, in the City of New-York, in the Summer and Autumnal Months of 1819; and of the Check Given to Its Progress by the Board of Health: with a List of Cases and Names of Sick Persons, and a Map of Their Places of Residence within the Infected and Prescribed Limits: with a View of Ascertaining By Comparative Arguments, whether the Distemper was Engendered by Domestic Causes, or Communicated By Human Contagion from Foreign Ports. New-York: William A. Mercein; 1819. [Google Scholar]
- 48.Cobb F. Report to the Chairman of the House Committee, and Medical Officers, of the London Hospital, On the Subject of the Epidemic Now Prevailing at Newcastle and Its Neighborhood. London: School Press; 1833. [Google Scholar]
- 49.Reese DM. A Plain and Practical Treatise on the Epidemic Cholera; As It Prevailed in the City of New York, in the Summer of 1832, Including Its Nature, Causes, Treatment and Prevention. Designed for Popular Instruction. To Which Is Added, by Way of Appendix, A Brief Essay on the Medical Use of Ardent Spirits, Being an Attempt to Show that Alcohol is as Unnecessary and Mischievous in Sickness as in Health. New York: Conner & Cooke; 1833. [Google Scholar]
- 50.Shapter T. The History of the Cholera in Exeter in 1832. London: John Churchill; 1849. [Google Scholar]
- 51.Leigh J, Gardiner N. History of the Cholera in Manchester, in 1849; As Reported to the Registrar General of Births, Deaths, &c. London: Simpkin, marshall, and Co.; 1850. [Google Scholar]
- 52.Panum P. Om cholera-epidemien i Bandholm 1850. Hospitaals-Meddelser. 1850;3:548–630. [Google Scholar]
- 53.Cooper H. On the cholera mortality in Hull during the epidemic of 1849. J Statist Soc London. 1853;16:347–51. [Google Scholar]
- 54.Hatton J. A Lecture of the Sanitary Condition of Chorlton-Upon-Medlock, Delivered at the Request of the Manchester and Salford Sanitary Association, in the Town Hall, Chorlton-Upon-Medlock, on Thursday Evening, January 12th, 1854. Manchester: Beresford & Galt; 1854. [Google Scholar]
- 55.The Senior Curate of St. The Cholera in Berwick Street. London: Hope & Co.; 1854. Luke’s, Berwick Street [Whitehead H] [Google Scholar]
- 56.‘J.L.’ The cholera – local influences. Cincinnati Daily Gazette. 1848 27 December, p. 2. [Google Scholar]
- 57.Clarke WM. William Budd, MD, FRS. “In memoriam” Brit Med J. 1880;1:163–66. [Google Scholar]
- 58.Brown PE. Another look at John Snow. Anesth Analg. 1964;43:646–54. [PubMed] [Google Scholar]
- 59.Koch T. Cartographies of Disease: Maps, Mapping, and Medicine. Redlands, CA: ESRI Press; 2005. The cholera debate. In: Koch T; pp. 105–27. [Google Scholar]
- 60.Huxley TH. On the Method of Zadig. The Nineteenth Century. 1880;7:929–40. [Google Scholar]
- 61.Paneth N, Vinten-Johansen P, Brody H, Rip M. A rivalry of foulness: official and unofficial investigations of the London cholera epidemic of 1854. Am J Public Health. 1998;88:1545–53. doi: 10.2105/ajph.88.10.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sims F. The Asiatic cholera. The Galveston News. 1866 13 May. [Google Scholar]
- 63.Knudsen GR. A questionable ‘new wrinkle’ in Haiti’s Cholera epidemic. 2012; www.gknudsenlaw.com/?page_id=168 (31 January 2013, date last accessed) [Google Scholar]