Abstract
The field of heart failure has seen striking advances during the past 50 years, yet the overall economic and social burden imposed by heart failure continues to rise. While neurohormonal models provide many insights in terms of explaining disease progression and informing drug development, mounting clinical evidence suggests that this model provides only a partial explanation of the disease. This paper evaluates the emerging models of heart failure and their potential to reverse the disturbing trends in heart failure morbidity and mortality.
Keywords: heart failure, acute decompensated HF, Winters Center for Heart Failure Research


Introduction
The last 50 years has seen a veritable renaissance regarding the level of interest and innovation in the field of heart failure (HF). Whereas clinicians initially viewed HF as a problem of excessive salt and water retention caused by abnormalities of renal blood flow (the “cardiorenal model”1), it soon became apparent that HF also was associated with reduced cardiac output and excessive peripheral vasoconstriction. This led to the development of the “cardiocirculatory” or “hemodynamic” model, in which heart failure was thought to develop secondary to abnormalities of the pumping capacity of the heart and excessive peripheral vasoconstriction.1 Although the cardiorenal models provided the rational basis for using diuretics to control the volume status of HF patients, and the cardiocirculatory model provided the rational basis for using inotropes and intravenous vasodilators to augment cardiac output, these therapeutic strategies did not prevent HF from progressing, nor did they lead to prolonged life or reduced hospitalizations for patients with moderate to severe HF.2, 3 Recent basic and clinical insights have suggested that HF progression results from the overexpression of biologically active molecules that are capable of exerting toxic effects on the heart and circulation (the “neurohormonal model”).2 Thus far, a variety of proteins including norepinephrine, angiotensin II, and aldosterone have been implicated as some of the potentially biologically active molecules whose biochemical properties are sufficient to contribute to disease progression in the failing heart. Indeed, in the latter part of the 1980s and early 1990s, clinical trials with angiotensin converting enzyme inhibitors and β-adrenergic blocking agents demonstrated favorable impacts on patient outcomes as well as cardiac remodeling.
Despite the many strengths of neurohormonal models in terms of explaining disease progression, and the many insights that neurohormonal models have provided regarding drug development for HF, there is increasing clinical evidence to suggest that our current neurohormonal models fail to completely explain disease progression in HF. More recently, it has been suggested that HF progression stems from deleterious changes in cardiac function and cardiac remodeling that result from sustained neurohormonal activation, prompting the view of HF as a “biomechanical model.”4 This model extends the insights provided by the neurohormonal paradigm by focusing the treatment of HF on the downstream biological consequences of neurohormonal activation rather than on neurohormonal activation itself. The biomechanical model predicts that therapeutic strategies that are designed to interrupt the vicious cycle of myocardial dysfunction and/or cardiac remodeling will favorably impact the HF phenotype and the natural history of HF progression. From the clinician’s point of view, the biomechanical model explains the salutary effects of cardiac resynchronization therapy and circulatory assist devices. The exciting developments in the field of myocardial regeneration are also predicted to have favorable impact in HF, if they can be shown to disrupt the deleterious cycle of myocardial dysfunction and/or cardiac remodeling. Moreover, there is enormous promise in personalized approaches to caring for patients with HF. Viewed together, one would be tempted to speculate that with all of this activity and innovation, the glass should be more than half full.
Just How Full is the Glass?
Despite the striking advances in HF over the past 50 years, the overall economic and social burden imposed by HF continues to rise. The most recent epidemiological data suggest that 6.6 million Americans have HF. By 2030, it is estimated that an additional 3 million people will have HF, which will represent a 25% increase in prevalence since 2010. Thirty-day readmission rates for HF hospitalization approach 25% among Medicare beneficiaries, and the rates of admission have essentially remained unchanged despite multiple strategies to prevent rehospitalizations.5 Although overall crude mortality rates for HF are improving, the risk-adjusted mortality within the first year following an HF hospitalization is approximately 30%, and the overall 3-year mortality for HF remains at a sobering 50%.6 Even more concerning is that the number of new therapeutic agents for treating the growing epidemic of HF is astonishingly low. Indeed, with the exception of the bradycardic agent ivabradine,7 which is not currently available in the United States, there have been no new agents approved for HF since 2003. Moreover, there are no effective therapies for acute decompensated HF, nor therapies for HF patients with preserved ejection fraction, despite extensive efforts to develop new therapies in these areas. When these sobering statistics are viewed together, the glass certainly appears less than half full.
Meeting the Clinical Need
Multidisciplinary HF programs have been developed specifically to deliver specialized care to patients with high morbidity and mortality and have been reported to reduce adverse outcomes such as rehospitalizations and all-cause mortality.8 The current staffing profile of HF programs9 reported by the ACCF/AHA Heart Failure and Transplant Committees and Heart Failure Society of America show that current HF centers employ approximately 2.65 physician full-time equivalents (FTEs), 2.21 nonphysician practitioner FTEs (nurse practitioner or physician assistant), and 2.61 nurse coordinator FTEs annually, all of whom provide care to approximately 1,641 outpatients annually. These centers also require patient care coordination with specialists other than cardiologists, including financial consultants, social workers, exercise physiologists, nutritionists, psychologists, pharmacologists, home health care specialists, endocrinologists, primary care physicians, and others.9
Meeting the Quality Need
There has been an increasing awareness that the quality of U.S. medical care — which should be effective, timely, safe, equitable, efficient, and patient-centered — has room for improvement, especially in highly prevalent and complex chronic medical conditions such as heart failure.10 With this recognition, and in the interest of promoting high-quality, patient-centered care and accountability, third-party payers and government agencies are increasingly monitoring the quality and outcomes of care, the number of hospital readmissions for HF, and the process of care in HF.10, 11 These mandates have spurred the development of standards outlining the necessary components to achieve training and clinical competence in the care of these patients.12, 13 Heart failure specialists are expected to play a key role in delivering the highest quality of complex care in the most cost-effective manner. In the years to come, the specialty of HF must adapt to the rapid expansion of evidence-based knowledge in this field to continue to provide the highest level of care and the best outcomes to patients.13
Unmet Need: Academic HF Centers with an Expanding Research Portfolio
There is an increasing demand for trained specialists who can provide quality care in HF and perform innovative research to define effective new treatment strategies, thus underscoring the need to develop academic centers with a training and research portfolio in the area of HF. To date, there are only a few centers with expanding research portfolios to develop effective new drugs and treatment strategies; clinical trials to demonstrate efficacy and safety; and outcomes studies to determine comparative effectiveness, affordability, and generalizability in real-world patients. With this recognition, the National Institutes of Health developed the “Roadmap for Medical Research” to address roadblocks to research and transform the way biomedical research is conducted by overcoming specific hurdles or filling defined knowledge gaps.14 The program is implementing interventions to foster high-risk/high-reward research, enable the development of transformative tools and methodologies, fill fundamental knowledge gaps, and change academic culture to foster collaboration. One of these interventions is the Heart Failure Clinical Research Network, which aims to improve the treatment of HF through rigorous testing; randomized clinical trials; interventions that aid in diagnosis, therapy, and heart failure management; and prevention. Specifically, the Heart Failure Clinical Research Network is charged with 1) establishing a knowledge base that will improve therapeutic decision making by testing approaches to manage acute and chronic HF; 2) developing methods to predict individual responses to interventions; 3) evaluating quality of life and cost effectiveness of HF interventions; 4) establishing collaborations between the practice community and regional clinical centers; 5) disseminating findings to the medical community; and 6) training physicians in HF clinical investigations.15 Up to eight regional clinical centers and a single data coordinating center were awarded in the first phase, and the Winters Center for Heart Failure Research at Baylor College of Medicine was one of them. Interestingly, the Winters Center for Heart Failure Research was established in 1998, before the NIH roadmap, with a vision very similar to the Heart Failure Clinical Research Network.
Winters Center for Heart Failure Research
The Winters Center for Heart Failure Research (www.bcm.edu/medicine/winterscenter) functions as a fully integrated heart failure research program that translates new technologies from bench to bedside and translates findings from relevant health outcomes research into meaningful clinical results for patients. Its emphasis is early phase clinical investigations that help identify optimal diagnosis, evaluation, and therapy to improve ventricular function and structure. The center was named in honor of the editor of this journal, Dr. William L. Winters Jr., for his enduring contributions to cardiology. One of the legendary pioneers at the Texas Medical Center, Dr. Winters was the first to bring echocardiography to Houston as a diagnostic test in the late 1960s and the angioplasty technique in conjunction with others in the late 1970s; he also was the driving force and endorser behind such a center. Since its inception, the Winters Center has been providing comprehensive research programs for treating patients with heart failure; training clinician scientists in clinical trial design and grantsmanship; and providing regulatory infrastructure for protocol approval, core laboratory functions for biomarker analyses, biostatistical support, and a coordinator pool for clinical studies.
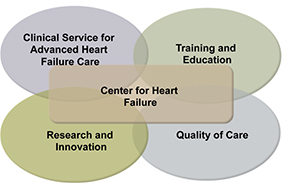
There are more than 14,000 research centers in the United States.16 A center might be assessed on its ability to attain short- and long-range goals, time spent on preparing proposals, award ratios, its ability to adapt to changes in science, its contributions to regional and national needs, and its efficiency in achieving multidisciplinary outcomes.16 Based on these criteria, the Winters Center for Heart Failure Research has had a transformative impact on its members, most of whom have been successful in obtaining federal grants, conducting clinical trials, and pursuing thriving academic careers. Since its inception in 1998, the center has provided the infrastructure and intellectual home for health care workers and investigators from Baylor College of Medicine, Weill Cornell Medical College, The University of Texas, Michael E. DeBakey VA Medical Center, Ben Taub General Hospital, The Methodist Hospital, and Texas Heart Institute. Moreover, the Winters Center has allowed these investigators to collaborate effectively across disciplines and institutions. Indeed, center investigators have published nearly 90 basic, translational, and clinical research articles in the field of heart failure and have trained numerous students and M.D./Ph.D. investigators who are now engaged in heart failure research at other institutions in the United States, Europe, and Japan. The center has participated in more 60 clinical trials since its inception, has had steady funding from the NIH and other federal agencies, and has successfully developed a biorepository and a database. Clinical studies with the Winters Center straddle the spectrum of heart failure research, ranging from prevention to advanced heart failure and cardiac transplantation. Some of the critical ingredients of its success lie in the fact that it not only facilitates research and innovation, but it also provides training and education for the next generation of heart failure specialists and the clinical experience in patient care and quality metrics (Figure 1). Thus, the Winters Center for Heart Failure Research has been successful in training clinicians and researchers to develop new treatment strategies and deliver quality care for heart failure patients.
Figure 1.
The profile of a successful heart failure center
The Way Forward
The moral imperative of reversing the disturbing trends in heart failure morbidity and mortality has never been more obvious nor more urgent. It is our belief that future advances in heart failure will require collaborative interdisciplinary teams of health care workers and researchers working together across different institutions to address the complex problem of heart failure. As long as health care professionals and investigators continue to collaborate, educate each other, and perform innovative research to improve outcomes in heart failure patients, the glass will remain half full, now and for the foreseeable future.
Funding Statement
Funding/Support: Dr. Bozkurt receives research funding from the National Institutes of Health and Forest Pharmaceutical. Dr. Mann receives research funding from the National Institutes of Health.
Footnotes
Conflict of Interest Disclosure: All authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
References
- 1.Packer M. How should physicians view heart failure? The philosophical and physiological evolution of three conceptual models of the disease. Am J Cardiol. 1993 Mar 25;71(9):3C–11C. doi: 10.1016/0002-9149(93)90081-m. [DOI] [PubMed] [Google Scholar]
- 2.Packer M. The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol. 1992 Jul;20(1):248–54. doi: 10.1016/0735-1097(92)90167-l. [DOI] [PubMed] [Google Scholar]
- 3.Massie BM. 15 years of heart-failure trials: what have we learned? Lancet. 1998 Aug;352 (Suppl 1):SI29–SI33. doi: 10.1016/s0140-6736(98)90016-2. [DOI] [PubMed] [Google Scholar]
- 4.Mann DL, Bristow MR. Mechanisms and models in heart failure: the biomechanical model and beyond. Circulation. 2005 May 31;111(21):2837–49. doi: 10.1161/CIRCULATIONAHA.104.500546. [DOI] [PubMed] [Google Scholar]
- 5.Ross JS, Chen J, Lin Z, Bueno H, Curtis JP, Keenan PS, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010 Jan;3(1):97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012 Jan 3;125(1):188–97. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 7.Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, et al. SHIFT Investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010 Sep 11;376(9744):875–85. doi: 10.1016/S0140-6736(10)61259-7. [DOI] [PubMed] [Google Scholar]
- 8.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004 Aug 18;44(4):810–9. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 9.Jessup M, Albert NM, Lanfear DE, Lindenfeld J, Massie BM, Walsh MN, et al. ACCF/AHA/HFSA 2011 survey results: current staffing profile of heart failure programs, including programs that perform heart transplant and mechanical circulatory support device implantation: a report of the ACCF Heart Failure and Transplant Committee, AHA Heart Failure and Transplantation Committee, and Heart Failure Society of America. J Am Coll Cardiol. 2011 May 17;57(20):2115–24. doi: 10.1016/j.jacc.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Bonow RO, Ganiats TG, Beam CT, Blake K, Casey DE, Jr, Goodlin SJ, et al. ACCF/AHA/AMA-PCPI 2011 Performance Measures for Adults With Heart Failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. Circulation. 2012 May 15;125(19):2382–2401. doi: 10.1161/CIR.0b013e3182507bec. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services [Internet]. Baltimore MD: Centers for Medicare & Medicaid Services; c2012. Outcome Measures; 2012 Oct 23 [cited 2012 Dec 12]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html. [Google Scholar]
- 12.Francis GS, Greenberg BH, Hsu DT, Jaski BE, Jessup M, LeWinter MM, et al. ACCF/AHA/ACP/HFSA/ISHLT 2010 clinical competence statement on management of patients with advanced heart failure and cardiac transplant: a report of the ACCF/AHA/ACP Task Force on Clinical Competence and Training. J Am Coll Cardiol. 2010 Jul 27;56(5):424–53. doi: 10.1016/j.jacc.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Konstam MA, Jessup M, Francis GS, Mann DL, Greenberg B. Advanced heart failure and transplant cardiology: a subspecialty is born. J Am Coll Cardiol. 2009 Mar 10;53(10):834–6. doi: 10.1016/j.jacc.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 14.The NIH Common Fund: Office of Strategic Coordination [Internet]. Bethesda MD: National Institutes of Health; c2012. About the NIH Roadmap; 2011 Dec 28 [cited 2012 Dec 12]. Available from: http://commonfund.nih.gov/aboutroadmap.aspx. [Google Scholar]
- 15.National Institutes of Health Grants & Funding [Internet]. Bethesda MD: National Institutes of Health; c2012. Overview Information--Department of Health and Human Services: Heart Failure Clinical Research Network Regional Clinical Centers; 2010 Jun 4 [cited 2012 Dec 12]. Available from: http://grants.nih.gov/grants/guide/rfa-files/RFA-HL-12-001.html. [Google Scholar]
- 16.Tash WR. Evaluating research centers and institutes for success: a manual and guide with case studies. 2nd ed. Fredericksburg VA: WT & Associates; c2006. [Google Scholar]


