Abstract
Background
For patients with ST-segment–elevation myocardial infarction transferred for primary percutaneous coronary intervention, guidelines have called for device activation within 90 minutes of initial presentation. Fewer than 20% of transferred patients are treated in such a timely fashion. We examine the association between transfer drive times and first door-to-device (D2D) times in a network of North Carolina hospitals. We compare the feasibility of timely percutaneous coronary intervention using ground versus air transfer.
Methods and Results
We perform a retrospective analysis of the relationship between transfer drive times and D2D times in a 119-hospital ST-segment–elevation myocardial infarction statewide network. Between July 2008 and December 2009, 1537 ST-segment–elevation myocardial infarction patients underwent interhospital transfer for reperfusion via primary percutaneous coronary intervention. For ground transfers, median D2D time was 93 minutes for drive times ≤30 minutes, 117 minutes for drive times of 31 to 45 minutes, and 121 minutes for drive times >45 minutes. For air transfers, median D2D time was 125 minutes for drive times of 31 to 45 minutes and 138 minutes for drive times >45 minutes. Helicopter transport was associated with longer door-in door-out times and, ultimately, was associated with median D2D times that exceeded guideline recommendations, no matter the transfer drive time category.
Conclusions
In a well-developed ST-segment–elevation myocardial infarction system, D2D times within 90 to 120 minutes appear most feasible for hospitals within 30-minute transfer drive time. Helicopter transport did not offer D2D time advantages for transferred STEMI patients. This finding appears to be attributable to comparably longer door-in door-out times for air transfers.
Keywords: acute myocardial infarction, primary coronary intervention, fibrinolysis, door to device time, transfer
In the treatment of ST-segment–elevation myocardial infarction (STEMI), it is well established that faster times to reperfusion result in less myocardial damage and better outcomes.1,2 Numerous studies demonstrate that prompt reestablishment of coronary flow via emergent, timely percutaneous coronary intervention (PCI) is associated with lower mortality.3,4 For emergent reperfusion via primary PCI for STEMI patients, American College of Cardiology/American Heart Association guidelines had, until recently, called for the achievement of PCI within 90 minutes of initial presentation.5,6 The latest guideline update extends the acceptable window to 120 minutes from first medical contact to device for STEMI patients requiring interhospital transfer.7 As first medical contact for transferred patients is not reliably measured by existing national databases including that used by our system, we focus our analysis on the earliest reliable measure, first hospital door-in time.
It is additionally important to note that the new guidelines explicitly emphasize the continued relevance of the 90-minute mark as a systems goal, despite the new adoption of 120 minutes as acceptable: “[T]he PCI and STEMI guideline writing committees have modified the first medical contact-to-device time goal from 90 minutes to 120 minutes for interhospital transfer patients, while emphasizing that systems should continue to strive for times <90 minutes.”7
When coronary reperfusion via PCI cannot be feasibly accomplished within a reasonable time period after initial patient presentation, fibrinolytic therapy offers an effective, alternative means of initial reperfusion for acute STEMI.
Born out of this recognition have been attempts to shorten door-to-device (D2D) times by instituting and improving on a comprehensive systems approach, including emergency department physician activation, streamlined transfer processes, early activation of the catheterization team, and a clear chain of coordinated communication throughout.8,9 With a focused commitment to systems improvement, D2D times across the country have improved significantly since 2005.10 Despite these improvements, challenges remain in achieving timely reperfusion via PCI for certain patient populations, particularly for STEMI patients who require interhospital transfer to a PCI-capable facility.11
The Reperfusion in Acute Myocardial Infarction in North Carolina Emergency Departments (RACE) project has aimed to codify best system-based practices while simultaneously seeking novel ways to improve and streamline the current system of STEMI care delivery in an extensive network of North Carolina hospitals.9,12 Of the 119 hospitals in this network, 21 are equipped to perform primary PCI 24/7, with on-site presence of cardiac surgery back-up. For a patient presenting with an STEMI, a non-PCI center faces the time-sensitive decision of administering fibrinolytic therapy versus transferring the patient to a PCI center for emergent catheterization as a primary means of reestablishing coronary flow.
Our 18-month experience from July 2008 to December 2009 provided the opportunity to explore several important aspects of the transfer process, each with the potential to impact clinical decision making in our network: (1) whether transfers in our network from non-PCI centers to PCI centers result in favorable D2D times, (2) whether the outcome trends for patients transferred for primary PCI was associated with anticipated travel time to a PCI facility, and (3) whether the mode of transportation (ground versus air) is associated with improved reperfusion times among patients transferred for initial reperfusion via primary PCI. By virtue of the observational nature of our data, we are not attempting to reach firm conclusions about treatment effects, given the confounding inherent in these types of analysis.13 Instead, we aim to illustrate the practical implications of evidence-driven STEMI care and we aim to identify patterns in an effort to generate hypotheses about how to achieve improvements in STEMI systems of care.
Methods
Data were obtained using standard data collection from the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry. Data collection was designed to capture a comprehensive description of each patient presentation, including the following: (1) relevant elements of the medical history (ie, risk factor profiles, history of prior myocardial infarction, history of prior coronary artery bypass graft, or PCI); (2) important elements of the acute clinical presentation (ie, shock or heart failure on presentation); (3) key process times for reperfusion (onset of symptoms, first medical contact, first and subsequent ECG with ST elevation, first door, transport time, and reperfusion time—drug or device) of the air or ground transfer to a PCI-capable facility; and (4) important elements of the subsequent course of hospitalization (ie, mortality and other morbidities). The Table presents a summary of these various elements.
Table.
Characteristics of Our Study Populations
| Drive Time Categories of Transferred STEMI Patients (n=1537) for Primary PCI |
Direct Presenters (n=3908) |
|||
|---|---|---|---|---|
| ≤30 min (n=531) | 31–45 min (n=664) | ≥45 min (n=342) | ||
| Demographics | ||||
| Age, mean in y | 58.8 | 59.2 | 60.0 | 60.7 |
| Male gender | 403 (75.9%) | 466 (70.2%) | 234 (68.4%) | 2735 (70.0%) |
| *Race | ||||
| White | 451 (84.9%) | 575 (86.6%) | 286 (83.6%) | 3296 (84.3%) |
| Black or African-American | 62 (11.7%) | 70 (10.5%) | 49 (14.3%) | 532 (13.6%) |
| Hispanic or Latino | 20 (3.8%) | 6 (0.9%) | 6 (1.8%) | 59 (1.5%) |
| Clinical characteristics | ||||
| Diabetes mellitus | 116 (21.8%) | 153 (23.0%) | 77 (22.5%) | 850 (21.8%) |
| Tobacco use | 252 (47.5%) | 330 (49.7%) | 173 (50.6%) | 1845 (47.2%) |
| Hypertension | 333 (62.7%) | 408 (61.4%) | 210 (61.4%) | 2474 (63.3%) |
| Dyslipidemia | 299 (56.1%) | 315 (47.4%) | 186 (54.4%) | 2037 (52.1%) |
| Peripheral arterial disease | 17 (3.2%) | 27 (4.1%) | 17 (5.0%) | 201 (5.1%) |
| Prior stroke | 19 (3.6%) | 27 (4.1%) | 16 (4.7%) | 213 (5.5%) |
| Currently on dialysis | 1 (0.2%) | 5 (0.8%) | 5 (1.5%) | 42 (1.1%) |
| Prior coronary/cardiac history | ||||
| Prior MI | 73 (13.7%) | 107 (16.1%) | 60 (17.5%) | 851 (21.8%) |
| Prior PCI | 90 (16.9%) | 119 (17.9%) | 61 (17.8%) | 834 (21.3%) |
| Prior CABG | 28 (5.3%) | 25 (3.8%) | 17 (5.0%) | 291 (7.4%) |
| Prior heart failure | 9 (1.7%) | 22 (3.3%) | 14 (4.1%) | 205 (5.2%) |
| Means of transport to first facility | ||||
| Self/family | 440 (82.7%) | 437 (65.8%) | 203 (59.4%) | 1035 (26.5%) |
| Ambulance | 85 (16.0%) | 224 (33.7%) | 139 (40.6%) | 2785 (71.3%) |
| Mobile ICU | 6 (1.1%) | 2 (0.3%) | 0 (0%) | 25 (0.6%) |
| Air | 0 (0%) | 0 (0%) | 0 (0%) | 63 (1.6%) |
| Acute presentation | ||||
| †First ECG obtained in field | 42/91 (46.2%) | 86/226 (38.1%) | 57/139 (41.0%) | 2303/2873 (80.1%) |
| STEMI noted on first obtained ECG | 456 (85.9%) | 586 (88.3%) | 282 (82.5%) | 3486 (89.2%) |
| Cardiogenic shock on first medical contact | 53 (10.0%) | 54 (8.1%) | 33 (9.6%) | 373 (9.5%) |
| Heart failure on first medical contact | 29 (5.5%) | 41 (6.2%) | 29 (8.5%) | 308 (7.9%) |
STEMI indicates ST-segment–elevation myocardial infarction; MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; ICU, intensive care unit.
Due to overlap in self-identification, columnar breakdown may add to >100%.
Includes patients transported by ambulance, mobile ICU, or air; excludes self/family presenters.
Standardized, anticipated drive times were established for the trip from each non-PCI center to the nearest PCI center using a conventional, consistent on-line navigation tool.14 Each STEMI patient presentation to a non-PCI center subsequently fell into 1 of 3 categories based on the anticipated drive time for transfer to the nearest PCI center: transfer travel time ≤30 minutes (≤30 minutes), transfer travel time between 31 and 45 minutes (31–45 minutes), transfer travel time >45 minutes (>45 minutes). The first 30-minute cutoff for the ≤30 minutes group was based on the notion that the pretransfer phase at the non-PCI center could reasonably be expected to take 30 minutes, as might the post-transfer, predevice phase upon arrival to the PCI facility. This 30/30/30 goal allows for guideline goal achievement in a well-functioning system. Within each of these 3 transfer time categories, STEMI patient presentations were further sorted into those transferred by ground and those transferred by air.
Statistical Methods
Descriptive statistics for continuous and categorical variables are presented as median (interquartile range) and number, respectively. For the key time-based variables in our analysis (D2D, door-in door-out [DIDO], door-out-second-door-in, second-door-in-to-device), we compared median times.
For patient characteristics, the statistical comparisons were based on Fisher exact test for statistical significance. P<0.05 was considered statistically significant. SAS version 8.2 (SAS Institute Inc, Cary, NC) was used for all analyses.
Results
During the 18-month period between July 2008 and December 2009, 6841 acute STEMI patients were treated in our system, 2933 of whom underwent transfer from a non-PCI center to a PCI center. Of the 2933 transferred patients, 1537 were transferred for primary PCI as an initial, emergent reperfusion therapy. During this same 18-month period, there were 3908 STEMI patients who, by virtue of their initial presentations to PCI-capable centers, did not require interhospital transfer. Demographic and clinical characteristics of the 1537 transferred primary PCI patients and of the 3908 direct presenters are outlined in the Table. The transferred population is further divided by drive time duration in 3 groups, as defined in the Methods section.
The Table provides demographic characteristics including age, race, medical history, and presenting features between the transferred and nontransferred patients. The transferred patients are further divided by transfer distances into 3 groups: ≤30 minutes, 31 to 45 minutes, and >45 minutes. In all groups, median age at presentation was ≈60 years, 68% to 76% of patients were men, and 84% to 87% of patients were identified as white. Overall, the groups had similar cardiovascular and coronary histories.
There are notable differences in the manner of initial presentation between the transferred patients and direct presenters. More than two thirds (1080/1537 or 70%) of our 1537 transferred patients were self-presenters to the initial non-PCI facility, with only 30% arriving to the first facility by ambulance or mobile intensive care unit. In contrast, 72% (2810/3908) of direct presenters to PCI centers arrived via ambulance or mobile intensive care unit, with only 26% arriving as self-presenters, yielding a statistically significant difference in the manner of initial presentation between transfer patients and direct presenters (P<0.001). Focusing on patients brought to the first hospital by trained emergency personnel (ie, excluding self-presenters), there was a substantial difference in the proportion who had prehospital ECGs between transfers and direct presenters. Only 41% (185/456) of emergency medical services -transported patients presenting initially to non-PCI facilities reportedly had a prehospital ECG compared with 80% (2303/2873) of emergency medical services -transported patients presenting initially to PCI facilities (P<0.001). Among transfers, patients in the ≤30 minutes group was numerically more likely to have had a prehospital ECG (46%) than patients in the more distant groups (38% for 31–45 minutes group; 41% for the >45 minutes group), although these differences did not reach the threshold for statistical significance (P=0.21 and P=0.50, respectively).
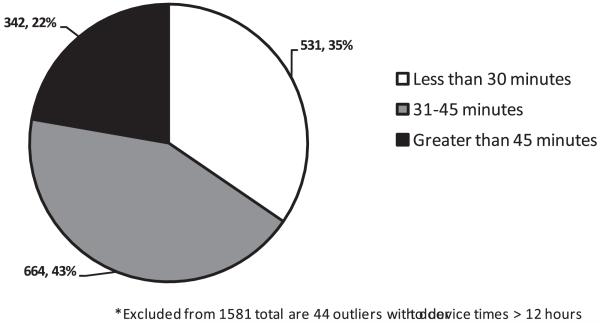
D2D Times
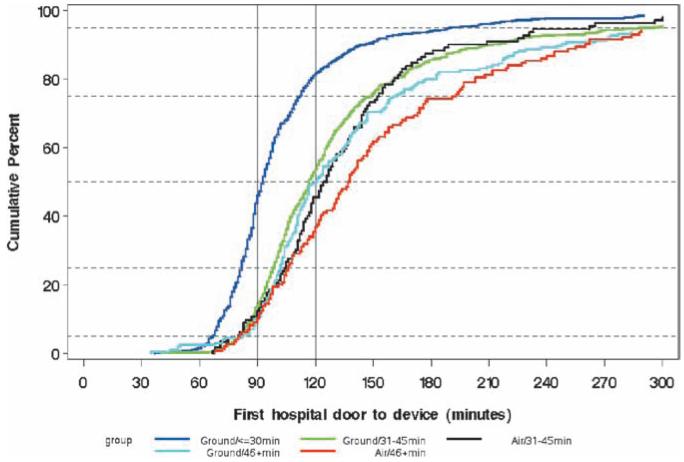
For the 1537 STEMI patients transferred for initial reperfusion via primary PCI, Figure 1 highlights the numeric breakdown of patients by drive time category, whereas Figure 2 presents median D2D times. These observed times were categorized by transfer drive time category (≤30 minutes, 31–45 minutes, or >45 minutes) and by mode of transport (ground versus air). For patients transferred by ground, median D2D times increased from 93 minutes (25th percentile [Q1], 82 minutes; 75th percentile [Q3], 112 minutes) in the ≤30 minutes group to 117 minutes (Q1, 98 minutes; Q3, 149 minutes) in the 31 to 45 minutes group to 121 minutes (Q1, 102 minutes; Q3, 161 minutes) in the >45 minutes group. For patients transferred by air, median D2D times increased from 125 minutes (Q1, 105 minutes; Q3, 153 minutes) in the 31 to 45 minutes group to 138 minutes (Q1, 106 minutes; Q3, 192 minutes) in the >45 minutes group. Only 2 patients in the ≤30 minutes group were transferred by air, thus their omission from Figure 2.
Figure 1.
Drive time categories for transfers for primary percutaneous coronary intervention.
Figure 2.
Median first door to device times by drive time and transport mode.
Figure 3 depicts the achievement of D2B time for ground-transported versus air-transported patients in the ≤30 minutes, 31 to 45 minutes, and >45 minutes groups. The ≤30 minutes group patients transferred by air (n=2) are omitted from this graphic representation. With the recent evolution in the PCI guidelines, an evolution that significantly impacts how we think about regional systems, we look at both the 90-minute mark and the 120-minute mark. This is motivated by the uncontroversial notion that faster-is-still-better and the notion that 90 minutes can still be a goal to which systems can strive. With a 90-minute, guideline-driven standard for D2D time, Figure 3 highlights the fact that approximately half of ground transfers in the ≤30 minutes group met the guideline goal. However, <20% of patients in the 31 to 45 minutes and >45 minutes groups met the 90-minute goal, regardless of whether transfer occurred by air or by ground. With employment of a 120-minute threshold, >80% of ground transfers in the ≤30 minutes group achieved satisfactory D2D times. More than half of ground transfers in the 31 to 45 minutes group achieved D2D within 120 minutes. Nearly half of ground transfers in the >45 minutes group and of air transfers in the 31 to 45 minutes group achieved D2D within 120 minutes. For the most distant air transfers (those in the >45 minutes group), only ≈35% achieved D2D within 120 minutes.
Figure 3.
Cumulative distribution of first door to device times by transport mode and drive time category.
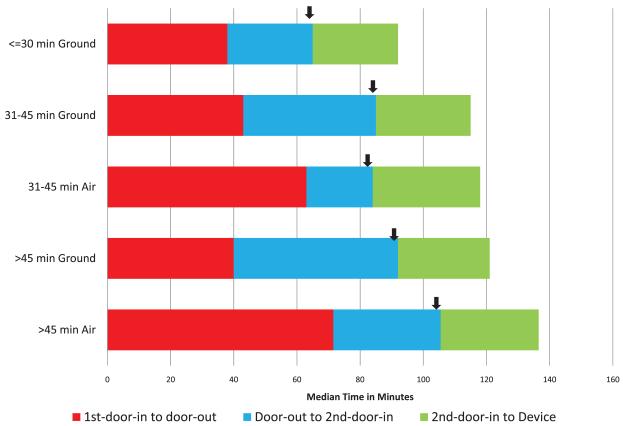
Anatomy of a Transfer
Our data permit a closer examination of the time-based elements of D2D time for transferred patients. D2D time can be dissected into its key components: DIDO, door-out-second-door-in, and second-door-in-to-device. Figure 4 presents the median time for each of these components of D2D time for patients transferred either by ground or by air in each of our 3 transfer distance groups. Data are not presented for the 2 patients transferred by air in the ≤30 minutes group.
Figure 4.
Temporal anatomy of a transfer by drive time and transport mode.
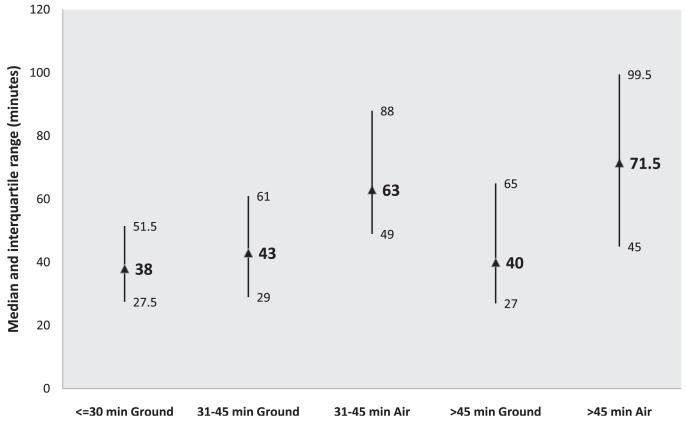
Evident from Figure 4 are several important time trends. First, median door-out to second-door-in times predictably increased by distance category for ground transfers: 27 minutes (Q1, 21 minutes; Q3, 34 minutes) in the ≤30 minutes group, 42 minutes (Q1, 35 minutes; Q3, 50 minutes) in the 31 to 45 minutes group, and 52 minutes (Q1, 44 minutes; Q3, 61 minutes) in the >45 minutes group. Median door-out to second-door-in times similarly increased by distance category for air transfers: 21 minutes (Q1, 15 minutes; Q3, 33 minutes) in the 31 to 45 minutes group and 34 minutes (Q1, 26 minutes; Q3, 42 minutes) in the >45 minutes group. Second, once patient transport was underway, the trip by air tended to occur faster than the trip by ground: 21 minutes versus 42 minutes in the 31 to 45 minutes group, 34 minutes versus 52 minutes in the >45 minutes group. Third, once patients arrived to PCI facilities, the subsequent time to device deployment was fairly consistent across all 5 groups. Fourth, and perhaps most notable, median DIDO times at the initial non-PCI facilities were significantly lengthier for air transfers (63 minutes [Q1, 49 minutes; Q3, 88 minutes] for 112 patients in the 31–45 minutes group, 72 minutes [Q1, 45 minutes; Q3, 100 minutes] for 144 patients in the >45 minutes group) than for ground transfers (38 minutes [Q1, 28 minutes; Q3, 52 minutes] for the 521 patients in the ≤30 minutes group, 43 minutes [Q1, 29 minutes; Q3, 61 minutes] for the 538 patients in the 31 to 45 minutes group, and 40 minutes [Q1, 27 minutes; Q3, 65 minutes] for the 196 patients in the >45 minutes group). The distribution variability in DIDO times is depicted in Figure 5.
Figure 5.
Distribution of door-in door-out times by drive time and transport mode.
Mortality
It is important to acknowledge that any comparison or inference of comparative treatment effects is significantly limited by the observational nature of our registry-based data. Mortality was numerically higher in PCI patients in the >45 minutes group (5.3%, 18/342) compared with PCI patients falling into either the ≤30 minutes group (3.8%, 20/531) or the 31 to 45 minutes group (3.9%, 26/664) (P=0.31). The difference was not statistically significant, and even with attempts to risk adjust, these observational results remain inescapably confounded.
Discussion
Our results offer important insights into the impact of transfer time and mode of transport on achievement of guideline goals for D2D time in the treatment of STEMI patients.
In our North Carolina RACE network, we observed a substantial decline in the achievement of D2D time <120 minutes (or the 90 minutes systems goal) as driving distance increased. For STEMI patients transferred from non-PCI facilities located 31 to 45 minutes from the nearest PCI center, a small minority experienced reperfusion via PCI within 90 minutes of their initial presentation. For STEMI patients transferred from the most distant non-PCI facilities (the >45 minutes group), an even smaller minority were reperfused via PCI within the guideline-recommended 90 minutes. The 120-minute threshold suggested by the updated PCI guidelines yields more promising D2D achievements but still with significant room remaining for improvement.
Air transport from a non-PCI facility to a PCI facility theoretically offers the opportunity to expedite the transfer process with the hope of achieving shorter overall D2D times. This advantage presumably should result from reduced travel time between facilities when traveling by helicopter. One of the more notable findings is the failure to translate this theory into practice as measured by overall D2D time. For patients in the 31 to 45 minutes group, median D2D time for those transferred by air was in fact 8 minutes longer than for those transferred by ground. For patients in the >45 minutes group, median D2D time for air transfers was 17 minutes longer than ground transfers. Longer overall D2D times for air transfers occurred, despite the demonstrably shorter trip duration (as captured by our door-out second-door-in data) and despite relatively uniform second-D2D times across all 5 subgroups. Although air transport may be a faster option for longer transport distances, air transport did not achieve guideline goals for time to reperfusion, as measured by median times, no matter the transport time category (31–45 minutes, >45 minutes).
Our data clearly suggest that advantages of air transport (shorter door to door time) were outweighed by the extra time spent by these patients at the initial non-PCI facility, at least as conducted in North Carolina. Several potential explanations exist for our findings, including but not limited to: (1) the time associated with preparation and deployment of air transportation to the initial facility, and (2) the potential selection of air transport cases with more complexity and associated clinical time consumption in the pretransport phase.
From our findings stem potential policy prescriptions for improvements in D2D times for transferred STEMI patients in the RACE network, with specific focus on how to improve the efficiency of air transfers. This is particularly important because air transport has been successfully implemented in other regions with median first D2D times of ≈100 minutes.15
Maintaining the safety of patients, our emergency medical personnel and the general public are of critical, non-negotiable importance. Therefore, trip duration (as captured in our data as door-out second-door-in), whether by highway or by air, cannot and should not be considered an area for significant time savings. Although time gains might be achievable by streamlining PCI center processes that occur once a transfer lands on the helipad or arrives in the ambulance bay (as captured in our data by second-door-in-to-device), our data suggest that any potential gains would be modest at best. Our focus on shortening overall D2D times must, therefore, center on the initial DIDO phase, as others have suggested as well,16 particularly on the lengthy period of time air transfers spent in the first hospital. Shortening this initial time element may require review of helicopter deployment processes, including an emphasis on faster helicopter dispatch and parallel processes, review of how air versus ground decisions are systematically made, and a focus on how to improve the systematic use of emergency medical services (and thus improve access to earlier, prehospital ECG) by patients in more rural communities.
Our door-to-device and mortality data suggest the need for continued efforts aimed at systems improvement in the care of transferred STEMI patients, with particular focus on how to streamline overall air transfer processes. Work done by Geisinger-based investigators highlights the potential improvements that can be made to the STEMI transfer process, albeit at a single, rural PCI center.17 If significant improvements in DIDO times are deemed not feasible or logistically insurmountable, then our transfer data suggest a potentially narrower role for air transportation in our North Carolina STEMI network. It may also suggest the need for greater emphasis on the role of fibrinolysis as an initial reperfusion therapy for carefully selected STEMI patients presenting to more distant non-PCI facilities.
By extension, our results may also inform how we approach initial reperfusion in acute STEMI patients presenting to non-PCI centers located within closer reach of PCI centers. If for any identifiable reason, a specific transfer is predicted to take significantly longer than ordinarily anticipated (due, for example, to weather, traffic, equipment, deployment), our data suggest a potential need to carefully consider fibrinolytic therapy as an initial strategy.
Limitations
The manner in which we stratified our data into transfer distance categories is based on estimated drive time, rather than by actual drive time duration of each individual transfer. These estimates for transfer duration serve as consistent standards, incorporating road type (ie, highway versus local) and speed limits. However, these standard estimates do not account for the real-life variability in travel time for a given distance between the same points of origin and destination. This inescapable travel time variability stems from, but is not limited to, variability inherent in weather, traffic, equipment, and operators. Our methods for distance stratification and subsequent analysis nevertheless serve as a consistent guide for thinking about the optimal manner for delivering reperfusion therapy in a statewide network of non-PCI and PCI centers.
Our data are observational, registry-based in nature and, therefore, do not offer the clarity of control that randomization affords. Our data similarly lack the granularity to address important questions and confounders in assessing in the transfer process, including: how often did weather and other system issues affect the air versus ground transport decision? Future data collection and analyses might attempt to identify the impact of second-choice transport mode on the overall air versus ground comparison. Nevertheless, the current data form the basis for our best insight into the functioning of a highly integrated STEMI network and into the areas for potential improvement therein.
Finally, the RACE network represents an evolving system with continuous learning curves, including during the 18-month period examined in this article. Further data, as it becomes available, will help to confirm and clarify the trends and lessons highlighted in our current discussion.
Conclusions
In a well-developed statewide STEMI treatment system, achieving first D2D times within a 90-minute systems goal, or within the guideline-acceptable window of 120 minutes, is a significant challenge in cases where an interhospital transfer is required. Achievement of timely reperfusion via PCI appears most feasible when the non-PCI hospital is located within a 30-minute drive of the nearest PCI center. Helicopter transport was associated with longer DIDO times and was not associated with better overall D2D times for STEMI patients initially presenting to more distant non-PCI hospitals in the RACE network. Our findings suggest the need for continued systems improvement with an aim of reducing first medical contact to device times, with further examination of how to reduce DIDO times and reexamination of how to make the best air versus ground transport decision. There also exists the potential need to reemphasize the role of timely fibrinolytic therapy for appropriately selected STEMI patients who present to more distant non-PCI centers.
WHAT IS KNOWN
There are multiple components to the interhospital transfer process for ST-segment–elevation myocardial infarction patients that make the process challenging.
Achieving timely reperfusion requires an integrated well-developed regional system of ST-segment–elevation myocardial infarction care.
Interhospital transfer can be achieved via different modes, namely ground versus air transport.
WHAT THE STUDY ADDS
Significant challenges remain in achieving guideline-based reperfusion goals for ST-segment–elevation myocardial infarction patients initially presenting to more distant non-PCI hospitals.
Air transfer may not necessarily be associated with faster reperfusion times, perhaps as a result of lengthier door-in door-out times at the transferring hospital.
Acknowledgments
Sources of Funding
This work was supported by an award from the American Heart Association Pharmaceutical Roundtable and David and Stevie Spina.
Footnotes
Disclosures
Dr Jollis has a working relationship (ie, consulting, research, and educational services) with the following companies: Blue Cross Blue Shield North Carolina, Medtronic Foundation, Sanofi-Aventis, and United Healthcare. Dr Granger has a working relationship (ie, consulting, research, and educational services) with the following companies: American College of Cardiology Foundation, Astellas Pharma Inc, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Elsevier, GlaxoSmithKline, Hoffman LaRoche (Roche Holding), McGraw-Hill Publishing, Medtronic Inc, Merck Sharpe & Dohme (Merck & Co, USA), Otsuka, Pfizer Inc, Sanofi-Aventis, UpToDate, Inc, and WebMD. The other authors have no conflicts to report.
References
- 1.Antman EM. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52:1216–1221. doi: 10.1016/j.jacc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Gibson CM, de Lemos JA, Antman EM, TIMI Study Group Time is muscle in primary PCI: the strength of the evidence grows. Eur Heart J. 2004;25:1001–1002. doi: 10.1016/j.ehj.2004.04.029. [DOI] [PubMed] [Google Scholar]
- 3.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 4.De Luca G, Suryapranata H, Zijlstra F, van ‘t Hof AW, Hoorntje JC, Gosselink AT, Dambrink JH, de Boer MJ. ZWOLLE Myocardial Infarction Study Group. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42:991–997. doi: 10.1016/s0735-1097(03)00919-7. [DOI] [PubMed] [Google Scholar]
- 5.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction–executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction) Circulation. 2004;110:588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 6.Kushner FG, Hand M, Smith SC, Jr, King SB, 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Jr, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 7.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:e574–e651. doi: 10.1161/CIR.0b013e31823ba622. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs AK, Antman EM, Ellrodt G, Faxon DP, Gregory T, Mensah GA, Moyer P, Ornato J, Peterson ED, Sadwin L, Smith SC, American Heart Association’s Acute Myocardial Infarction Advisory Working Group Recommendation to develop strategies to increase the number of ST-segment-elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation. 2006;113:2152–2163. doi: 10.1161/CIRCULATIONAHA.106.174477. [DOI] [PubMed] [Google Scholar]
- 9.Jollis JG, Roettig ML, Aluko AO, Anstrom KJ, Applegate RJ, Babb JD, Berger PB, Bohle DJ, Fletcher SM, Garvey JL, Hathaway WR, Hoekstra JW, Kelly RV, Maddox WT, Jr, Shiber JR, Valeri FS, Watling BA, Wilson BH, Granger CB, Reperfusion of Acute Myocardial Infarction in North Carolina Emergency Departments (RACE) Investigators Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA. 2007;298:2371–2380. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 10.Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW, Curtis JP. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124:1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang TY, Peterson ED, Ou FS, Nallamothu BK, Rumsfeld JS, Roe MT. Door-to-balloon times for patients with ST-segment elevation myocardial infarction requiring interhospital transfer for primary percutaneous coronary intervention: a report from the national cardiovascular data registry. Am Heart J. 2011;161:76–83.e1. doi: 10.1016/j.ahj.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Jollis JG, Mehta RH, Roettig ML, Berger PB, Babb JD, Granger CB. Reperfusion of acute myocardial infarction in North Carolina emergency departments (RACE): study design. Am Heart J. 2006;152:851.e1–851.11. doi: 10.1016/j.ahj.2006.06.036. [DOI] [PubMed] [Google Scholar]
- 13.Muñoz D, Granger CB. ST-segment-elevation myocardial infarction treatment and the seductive lure of observational analyses. Circulation. 2011;124:2477–2479. doi: 10.1161/CIRCULATIONAHA.111.068676. [DOI] [PubMed] [Google Scholar]
- 14.Mapquest, inc . [Accessed May 2011]. 2011. Available at: http://www.Mapquest.Com. [Google Scholar]
- 15.Henry TD, Sharkey SW, Burke MN, Chavez IJ, Graham KJ, Henry CR, Lips DL, Madison JD, Menssen KM, Mooney MR, Newell MC, Pedersen WR, Poulose AK, Traverse JH, Unger BT, Wang YL, Larson DM. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 16.Miedema MD, Newell MC, Duval S, Garberich RF, Handran CB, Larson DM, Mulder S, Wang YL, Lips DL, Henry TD. Causes of delay and associated mortality in patients transferred with ST-segment-elevation myocardial infarction. Circulation. 2011;124:1636–1644. doi: 10.1161/CIRCULATIONAHA.111.033118. [DOI] [PubMed] [Google Scholar]
- 17.Blankenship JC, Scott TD, Skelding KA, Haldis TA, Tompkins-Weber K, Sledgen MY, Donegan MA, Buckley JW, Sartorius JA, Hodgson JM, Berger PB. Door-to-balloon times under 90 min can be routinely achieved for patients transferred for ST-segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol. 2011;57:272–279. doi: 10.1016/j.jacc.2010.06.056. [DOI] [PubMed] [Google Scholar]