Abstract
Background:
Subvastus approach in total knee arthroplasty (TKA) spares the quadriceps and may assist in faster rehabilitation. The present randomised controlled study was conducted to determine if the subvastus approach results in early recovery, faster mobilization, shorter hospital stay, and improved function.
Materials and Methods:
100 patients undergoing simultaneous bilateral TKA were randomized into two groups: subvastus group and medial parapatellar group. The patients were assessed clinically using VAS, time to straight leg raise, ability to stand with walker, ability to use a commode chair, ability to climb stairs, flexion at discharge, and day of discharge. Perioperative blood loss and duration of surgery were also compared. The patient were kept on same pain management and physiotherapy protocol. The evaluation was done at day 0,1,3 and at discharge. Statistical analyses tested the null hypotheses of no differences in patients treated with either group at 95% significance level (P < 0.05).
Results:
The VAS score was significantly lower in subvastus group on day 1 and day 3. Also mean hospital stay was 2.04 days less in subvastus group. Patients with subvastus approach were able to perform straight leg raising 0.44 days earlier. Though time to stand with walker was same for both groups, the ability to use commode chair, and climb stairs was significantly early (P < 0.05) in the subvastus group. The average flexion at the time of discharge in subvastus and parapatellar group were 100.8 and 96.8°, respectively. The mean perioperative blood loss in subvastus group and parapatellar group were 343 ml and 372 ml, respectively. Average surgical time required for subvastus approach and parapatellar approach were 108.5 and 94.3 min, respectively.
Conclusions:
Subvastus approach produce appreciably less pain and faster mobilization due to lesser insult to quadriceps, thus assisting in early rehabilitation, shorter hospital stay, less expenditure, and more patient satisfaction.
Keywords: Parapatellar approach, subvastus approach, total knee arthroplasty
INTRODUCTION
The two main concerns for patients prior to total knee arthroplasty (TKA) are pain and length of recovery.1–3 Obtaining satisfactory results with standard parapatellar approach may require a long recovery period. The ultimate functional result may be good but still fall short of the patient's expectations for early return to full activity. Though long term functional outcomes of both subvastus and medial parapatellar approaches are comparable in the literature,4–6 studies concerning early functional outcomes of both approaches show variable results with some studies showing favorable results of the subvastus approach4,5,7,8 while others do not.6,9 Very few randomized controlled trials comparing early results of both approaches have been published in the literature.6,8 In this study we compared the early functional outcome of subvastus approach with medial parapatellar approach in elderly, nonobese patients undergoing bilateral simultaneous TKA.
MATERIALS AND METHODS
Only elderly patients (>70 years of age) with body mass index (BMI) of less than 30, knee deformity less than 20° in any plane and undergoing bilateral simultaneous TKA for osteoarthritis were included in the study. Those with revision or unilateral surgery or with any previous knee surgery or arthritis due to any cause other than primary osteoarthritis were excluded. First 100 patients satisfying the inclusion criteria were studied. These patients were randomized into two groups of 50 patients each, group A (subvastus group) and group B (medial parapatellar group). A computer-generated variable block schedule was used for randomization. Patients underwent a single stage total knee arthroplasty with either a subastus approach in both lower limbs, or a medial parapatellar approach in both lower limbs. The randomization list was generated by an independent statistician and the resulting treatment allocations were stored in sealed opaque envelopes. Randomization occurred at the outpatient consultation by the orthopedic surgeon. The surgeries were performed by a single experienced arthroplasty surgeon (SJ) during September 2010 to July 2011. Inclusion and subsequent followup of patients are summarized in the consort statement [Figure 1].
Figure 1.
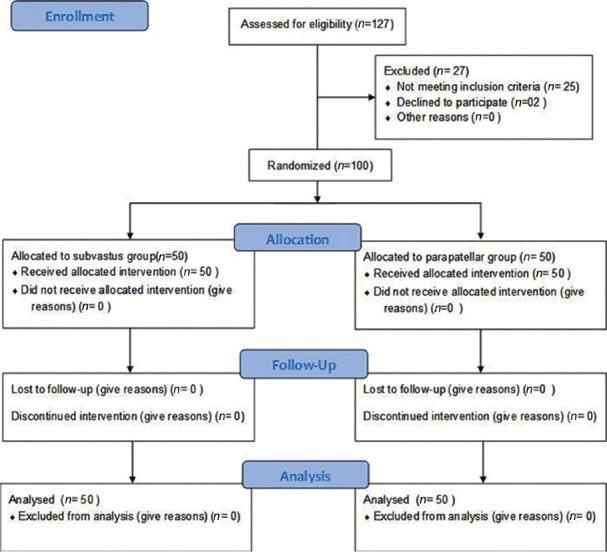
CONSORT statement: Flow chart of participants throughout the study
Approval from the institutional ethics committee was obtained. All patients agreed to sign an informed consent. There were no significant differences between both groups for age, gender, and BMI [Table 1]. There were 38 females and 12 males in “subvastus” group while 40 females and 10 males in “parapatellar” group. The mean age of the patients in “subvastus” group was 76.4 years (range70-82 years) and in “parapatellar” group was 75.8 years (range70-83 years). Both the groups received a preoperative physiotherapy consultation to educate them about the physiotherapy protocol. Similar regional anaesthesia (combined spinal epidural), pain management, and physiotherapy protocols consisting of active flexion and extension of the knee, straight leg raising exercises as tolerated, on day of surgery. Bed side mobilisation and walking with walker on postop day 1. Commode chair training on day 2, stairs climbing on day 3 and so on. All these protocols were followed depending upon the pain tolerance of these patients, and were delayed in case of increased pain and intolerance. Patients in both the groups received cruciate retaining mobile bearing prosthesis (Sigma CR 150 Depuy). Surgical technique was similar in all patients with only difference being the approach [Figures 2 and 3]. Computer navigation was used in all the patients for better alignment. Patella was not everted in any of the cases. Patella denervation and patelloplasty were done in all the patients. All surgeries were performed in the morning from 8 am to 12 pm. Operative day was considered as day 0, the next day as day 1 and so on. The day 0 assessment was performed 8 h after surgery for all patients. Paracetamol 1 gm twice a day (8 am and 8 pm) was given as an analgesic postoperatively. The VAS scores were recorded on a scale of 0 to 10 on day 0, 1, 3 and at discharge. Time of straight leg raising (one leg at a time), ability to stand with walker, ability to use a commode chair, ability to climb stairs, and day of discharge were also compared in both the groups. All these parameters were recorded prior to evening dose of paracetamol. Ability to use commode chair comfortably and VAS below two were considered as end points for patients discharge in this study. Perioperative blood loss and duration of surgery were also compared. Postoperative blood loss was assessed at the time of removal of drain (24 h after surgery). The parameters were recorded by a blinded research fellow and the results were analyzed by an independent statistician, both being unaware of the actual intervention.
Table 1.
Demographic data of the patients in each group

Figure 2.
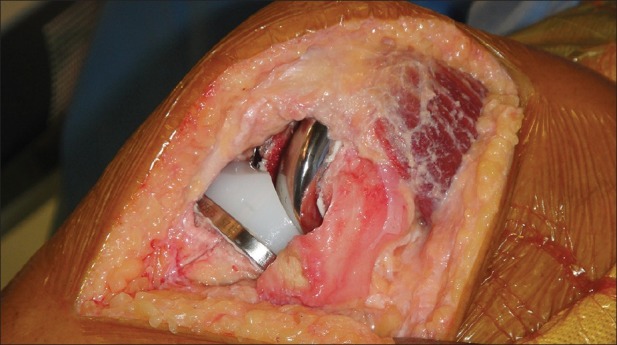
Clinical photograph showing subvastus approach total knee arthroplasty with CR 150 prosthesis
Figure 3.
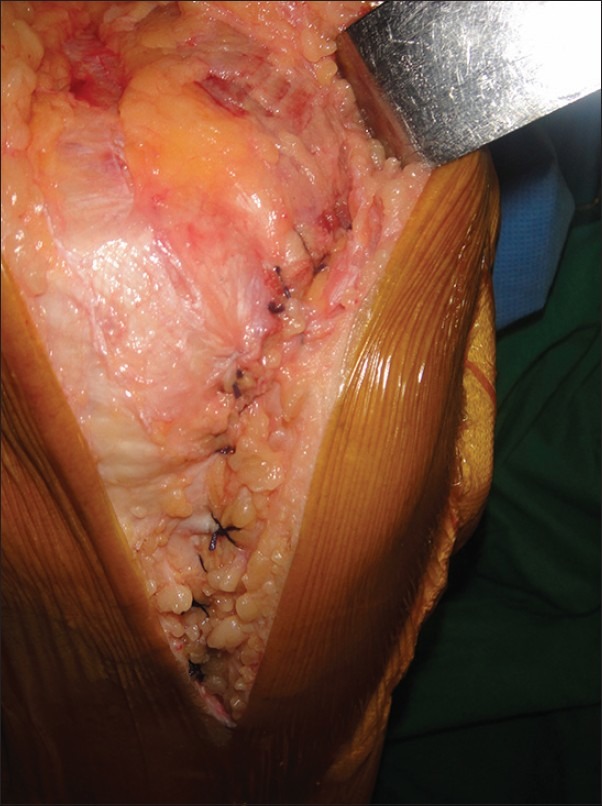
Clinical photograph showing closure of the subvastus approach
Statistical analysis
The statistical analysis was carried out using SPSS 16.0 and MS Excel 2003. Statistical analyses tested the null hypotheses of no differences in patients treated with either group at 95% significance level (P < 0.05). Unpaired t-test was used to evaluate possible statistical differences of values within and between groups.
RESULTS
The mean VAS scores in Group A (subvastus group) on day 0, day 1, day 3, and at discharge were 5.4, 3.8, 1.8, and 1.48, respectively [Table 2 and Figure 4]. Similarly, the mean VAS scores in Group B (parapatellar group) on day 0, day 1, day 3, and at discharge were 5.28, 4.6, 3.12, and 1.52, respectively [Table 2]. The difference in mean VAS score on day 0 between both the groups was not statistically significant (P value 0.676). The differences in mean VAS scores on day 1 and day 3 were statistically significant (P < 0.05). At discharge the differences in mean VAS scores were not statistically significant but more importantly, the discharge in subvastus group was 2.04 days earlier than the parapatellar group [Table 3 and Figure 5]. The ability to perform straight leg raise [Table 3] postoperatively was earlier in the subvastus group (1.64 as compared to 2.08 in parapatellar group) which was statistically significant (P < 0.01). Though time to stand with walker was same for both groups, the ability to use commode chair and climb stairs was significantly early (P < 0.05) in the subvastus group compared to parapatellar group [Table 3]. The average flexion at the time of discharge in subvastus and parapatellar group were 100.8 and 96.8°, respectively and the difference was statistically not significant [Table 3].
Table 2.
VAS scores
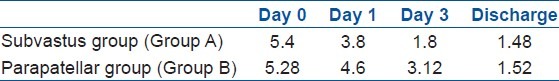
Figure 4.
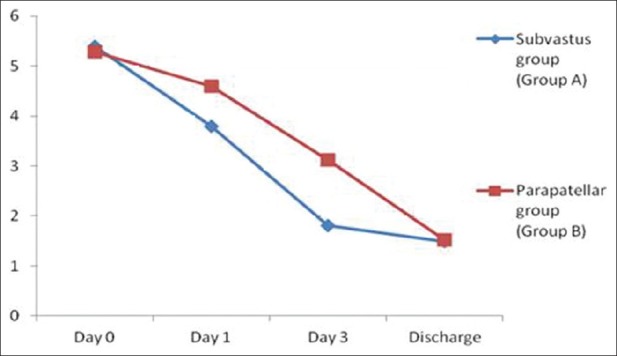
Graph showing VAS scores between parapatellar and subvastus group
Table 3.
Early functional results
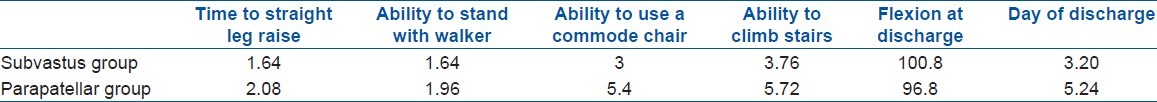
Figure 5.
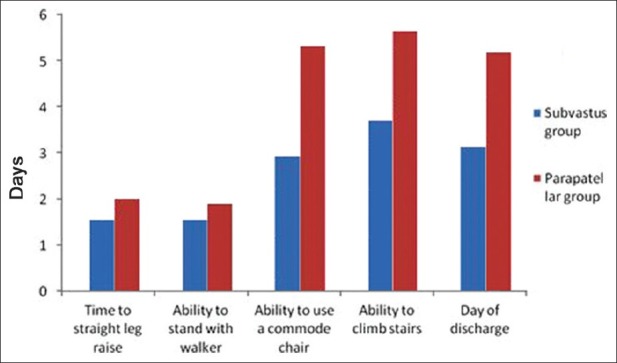
Bar diagram showing early function results between parapatellar and subvastus group
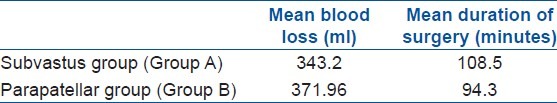
The mean perioperative blood loss in Group A (subvastus group) and Group B (parapatellar group) were 343.20 and 371.96 mL, respectively [Table 4] and the difference was not statistically significant (P-value 0.83). Average surgical time required for subvastus approach and parapatellar approach were 108.5 and 94.3 min, respectively [Table 4]. There were no early complications noted in both the groups during the study period.
Table 4.
Mean blood loss and duration of surgery
DISCUSSION
Early rehabilitation after a total knee arthroplasty (TKA) is desirable for patient satisfaction and to minimize the postoperative complications. Though there are many approaches for TKA, medial parapatellar approach is the most common approach. It is an extensile approach and provides adequate working space, but breach in the quadriceps mechanism has been considered a major disadvantage. The impairment of the blood supply to patella has also been mentioned as a disadvantage by Holtby et al.10 This problem may be further accentuated by lateral retinacular release for patellar tracking. Impairment of blood supply of patella may lead to avascular necrosis which can cause fracture or persistent anterior knee pain.10,11 Subvastus approach was described by Hoffman in 1991 as an alternative approach to TKA.12 Several advantages of subvastus approach have been highlighted in literature. It preserves the integrity of the quadriceps muscle as well as the patellar blood supply thus allowing better patellar tracking, less need for lateral retinacular release, and faster rehabilitation.13–15 The other advantages are decreased postoperative analgesics requirement and reduced hospital stay.4,13 Faure et al., in a comparative study concluded that the subvastus group had better muscle strength than the parapatellar group in the immediate postoperative period.5 Rehabilitation in early postoperative period has been shown to be better by subvastus approach as compared to medial parapatellar approach.8,13 The early strength advantage, potential anatomic, and vascular benefits of subvastus approach make it a viable alternative to the traditional parapatellar approach.
Major disadvantage of subvastus approach is that patellar eversion may be difficult and knee exposure may be inadequate.12 The technique is demanding and has a long learning curve. Other relative contraindications for subvastus approach are significant patella baja, previous high tibial osteotomy, and previous arthrotomy with the medial parapatellar approach.16,17 Though controversial, obesity, or excessive thigh girth have also been reported to limit the exposure in the subvastus approach.17,18 Considering the advantages and the disadvantages of this approach we believe that the most ideal candidates for this approach would be nonobese elderly individuals as early rehabilitation is of utmost importance in these patients.
Although the VAS scores on day 0 was the same in both groups, it was significantly lower in subvastus group than the parapatellar group from day 1 onwards till discharge. Active straight leg raise in bed, ability to use commode chair, and stair climbing was also significantly earlier in subvastus group than the parapatellar group. The average time of discharge of the patient was 2.04 days earlier in subvastus group as compared to the parapatellar group. The quadriceps strength was better in subvastus group than in parapatellar group as evidenced by early ability to climb stairs and use commode chair. This faster rehabilitation can also be attributed to less pain in subvastus approach group as the quadriceps mechanism remains intact. Other advantage of subvastus approach was shorter hospital stay, which significantly cuts down the expenses for the patient (approx. 10-15% less in our hospital) and add to overall patient satisfaction.
To the best of our knowledge, this is the only study performed on single stage bilateral simultaneous TKA. The similar procedure was done in both knees since we consider that functions like using commode chair, stair climbing, walking with walker, and pain can be better quantified if patients undergo the same procedure on both sides.5,6 These features were lacking in all of previously known studies.8,9,13
The limitation of this study is that the quadriceps power was not measured objectively with a tool like a Cybex test or any other similar device. However, these results can really be tested in postoperative patients is a question of debate, because of pain and apprehension after surgery.
To conclude, one of the main factors which limit the postoperative rehabilitation in elderly patients undergoing bilateral simultaneous TKA with parapatellar approach is pain and delayed mobilization. This study shows that subvastus approach produce appreciably less pain and faster mobilization as compared to parapatellar approach and shorter hospital stay, and more patient satisfaction. Therefore, this approach could be recommended in this patient group.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP. Patient satisfaction after total knee arthroplasty: A comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16:740–7. doi: 10.1054/arth.2001.23922. [DOI] [PubMed] [Google Scholar]
- 2.Trousdale RT, McGrory BJ, Berry DJ, Becker MW, Harmsen WS. Patients concerns prior to undergoing total hip and total knee arthroplasty. Mayo Clin Proc. 1999;74:978–82. doi: 10.4065/74.10.978. [DOI] [PubMed] [Google Scholar]
- 3.Dickstein R, Heffes Y, Shabtai EI, Markowitz E. Total knee arthroplasty in the elderly: Patients’ self-appraisal 6 and 12 months postoperatively. Gerontology. 1998;44:201–10. doi: 10.1159/000022011. [DOI] [PubMed] [Google Scholar]
- 4.Cila E, Güzel V, Ozalay M, Tan J, Simsşek SA, Kanatli U, et al. Subvastus versus medial parapatellar approach in total knee arthroplasty. Arch Orthop Trauma Surg. 2002;122:65–8. doi: 10.1007/s004020100319. [DOI] [PubMed] [Google Scholar]
- 5.Fauré BT, Benjamin JB, Lindsey B, Volz RG, Schutte D. Comparison of the subvastus and paramedian surgical approaches in bilateral knee arthroplasty. J Arthroplasty. 1993;8:511–6. [PubMed] [Google Scholar]
- 6.Bourke MG, Jull GA, Buttrum PJ, Fitzpatrick PL, Dalton PA, Russell TG. Comparing outcomes of medial parapatellar and subvastus approaches in total knee arthroplasty a randomized controlled trial. J Arthroplasty. 2012;27:347–53.e1. doi: 10.1016/j.arth.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Dutka J, Skowronek M, Sosin P, Skowronek P. Subvastus and medial parapatellar approaches in TKA: Comparison of functional results. Orthopedics. 2011;34:148. doi: 10.3928/01477447-20110427-05. [DOI] [PubMed] [Google Scholar]
- 8.Roysam GS, Oakley MJ. Subvastus approach for total knee arthroplasty: A prospective, randomized, and observer-blinded trial. J Arthroplasty. 2001;16:454–7. doi: 10.1054/arth.2001.22388. [DOI] [PubMed] [Google Scholar]
- 9.Weinhardt C, Barisic M, Bergmann EG, Heller KD. Early results of subvastus versus medial parapatellar approach in primary total knee arthroplasty. Arch Orthop Trauma Surg. 2004;124:401–3. doi: 10.1007/s00402-004-0692-3. [DOI] [PubMed] [Google Scholar]
- 10.Holtby RM, Grosso P. Osteonecrosis and resorption of the patella after total knee replacement: A case report. Clin Orthop Relat Res. 1996;328:155–8. doi: 10.1097/00003086-199607000-00024. [DOI] [PubMed] [Google Scholar]
- 11.Scapinelli R. Blood supply of the human patella.Its relation to ischaemic necrosis after fracture. J Bone Joint Surg Br. 1967;49:563–70. [PubMed] [Google Scholar]
- 12.Hofmann AA, Plaster RL, Murdock LE. Subvastus (southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;269:70–7. [PubMed] [Google Scholar]
- 13.Matsueda M, Gustilo RB. Subvastus and medial parapatellar approaches in total knee arthroplasty. Clin Orthop Relat Res. 2000;371:161–8. doi: 10.1097/00003086-200002000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Scuderi GR, Tenholder M, Capeci C. Surgical approaches in mini-incision total knee arthroplasty. Clin Orthop Relat Res. 2004;428:61–7. doi: 10.1097/01.blo.0000148574.79874.d0. [DOI] [PubMed] [Google Scholar]
- 15.Boerger TO, Aglietti P, Mondanelli N, Sensi L. Mini-subvastus versus medial parapatellarapproach in total knee arthroplasty. Clin Orthop Relat Res. 2005;440:82–7. doi: 10.1097/01.blo.0000185755.09777.2d. [DOI] [PubMed] [Google Scholar]
- 16.Engh GA. Midvastsus approach. In: Scuderi GR, Tria AJ Jr, editors. Surgical Techniques in Total Knee Arthroplasty. New York: Springer-Verlag; 2002. pp. 127–30. [Google Scholar]
- 17.Kim JM, Choi NY, Kim SJ. Large thigh girth is a relative contraindication for the subvastus approach in primary total knee arthroplasty. J Arthroplasty. 2007;22:569–73. doi: 10.1016/j.arth.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Shah N, Nilesh G, Patel N. Mini-subvastus approach for total knee arthroplasty in obese patients. Indian J Orthop. 2010;44:292–9. doi: 10.4103/0019-5413.65157. [DOI] [PMC free article] [PubMed] [Google Scholar]


