Abstract
Background:
Posterior tibial slope (PTS) is an important factor affecting postoperative range of motion (ROM) following total knee arthroplasty (TKA). Metaphysio-diaphyseal angle (MDA) is a new entity defined as angle between proximal anatomical axis and metaphyseal axis of tibia. This study was undertaken to determine PTS in Indian patients and find its correlation with MDA of tibia. Accuracy of extramedullary jigs and the influence of MDA on the accuracy was also evaluated. This study is a retrospective analysis of prospectively collected data in a tertiary healthcare center.
Materials and Methods:
Data of 100 consecutive patients undergoing TKA in a single center by a single surgeon was analyzed. Posterior cruciate ligament (PCL) substituting TKA was done with same jig to achieve different PTS in different patients. MDA, preoperative PTS and postoperative PTS were calculated. The data was analyzed using appropriate statistical analysis.
Results:
Mean preoperative PTS was 11.64° and mean MDA was 23.76° with a strong correlation between them (Pearson's coefficient 0.72). Extramedullary jigs were accurate in 53% cases. In remaining 47%, postoperative PTS was less than planned PTS in 30%, and more in 17%. Mean postoperative PTS was 2.54°. In patients with MDA < 20°, postoperative PTS was significantly less (P = 0.0176) compared with those with MDA > 20°.
Conclusions:
The study establishes the positive correlation between MDA and PTS in Indians; and that MDA is an independent factor affecting accuracy of extramedullary jigs in TKA.
Keywords: Extramedullary Jigs in total knee arthroplasty, metaphysio-diaphyseal angle, posterior tibial slope, total knee arthroplasty
INTRODUCTION
Total knee arthroplasty (TKA) is one of the most successful operations yet devised with an average survival of more than 90% at 15 years.1,2 The patients require an average of 67° of flexion for swing phase of gait, 83° for climbing stairs, 90° for descending stairs, and 93° to rise from a seated position.3,4 In the eastern hemisphere and in the Indian subcontinent, flexion greater than 105° is required for kneeling and squatting during activities of daily living and religious activities.5 Among the numerous factors affecting the postoperative flexion in a total knee replacement posterior tibial slope (PTS) is important, which decides about the sagittal alignment of tibia.5
The coronal alignment of the knee has been studied extensively, there are very few studies on the sagittal anatomy. Almost all studies in this field have been done in the Caucasian population. Studies done in the Chinese, Japanese, and Pakistani populations (Asians) have documented a difference in the PTS in their respective population from the Caucasians.6–8 Considering these racial differences in the anatomy of the knee, the postoperative outcome and the need for a difference in the prosthesis according to racial variations, a study was needed to bring out the characteristics of Indian population, which would help in designing prosthesis suited for Indian population. The present study accomplishes this partly by studying the sagittal anatomy of the tibia. It is well known that in TKA, proper alignment of the components is critical to patient satisfaction and long term survival of the implants.8 We postulate that any variations in sagittal anatomy and sagittal Metaphysio-Diaphyseal Angle (MDA) may affect the intraoperative achieved PTS and in turn, the outcome of the surgery.
MDA is a new entity defined in this study. This angle is formed between two lines: first line is the proximal anatomical axis of the tibia and the second is the axis of the metaphysis. First, in a lateral view radiograph, the proximal anatomical axis of tibia (i.e. the first line) is drawn by connecting midpoints of outer cortical diameter of tibia at 5 and 15 cm distal to the knee joint. Then, the axis of metaphysis (i.e. the second line) was drawn by defining two points each on anterior and posterior cortices of tibial metaphysis in a lateral film and joining the midpoints [Figure 1]. Finally, the angle between these two lines (i.e. the MDA) was measured.
Figure 1.

X-ray knee joint with leg (lateral view) showing calculation of metaphysio-diaphyseal angle
The aim of the present study is to find the mean preoperative PTS and MDA in the Indian population and to find a correlation between them to find whether the MDA influences the accuracy of PTS taken with extramedullary jigs.
MATERIALS AND METHODS
A retrospective analysis of prospectively collected data was done for 100 patients (with Ahlback grade 4 and 5 osteoarthrosis of knee) who underwent TKA in a tertiary care centre from June 2001 till January 2010. The average followup was 4.5 years (range 2-8.5 years). All the patients were operated by a single surgeon using posterior cruciate ligament substituting design (with semi-congruent insert) of one make of a particular manufacturer (Zimmer, Inc., USA) using a single type of jig with provision to give different PTS. Patients with extra articular deformity and bone defects requiring build up on tibia were excluded from the study. The average age was 62.4 years (range 58-74 years). Full weight bearing standard radiographs were taken in both anteroposterior and lateral views. Lateral views were taken with both the tibia and femoral condyles overlapping with at least 15 cm of shaft of tibia and femur visible for calculation of the anatomical axes.9
Preoperative PTS [Figure 2] was defined as the angle formed by two lines in the lateral radiograph. The first line was the line perpendicular to the anatomical axis of the tibia. The second line formed by joining the most proximal points on the tibia plateau on the lateral radiograph as defined by Massin et al.,9 avoiding osteophytes. Although previously, there was no consensus on the ideal anatomical axis to measure PTS, the proximal anatomical axis, i.e. the line connecting midpoints of outer cortical diameter at 5 and 15 cm distal to the knee joint (Yoo et al8), is now recommended because it is most parallel to the sagittal mechanical axis.8 Hence this axis was assumed to be the anatomical axis in our study.
Figure 2.

X-ray knee with leg (lateral view) showing calculation of preoperative posterior tibial slope
The polyethylene insert of the implant used (Zimmer Nexgen) in this study had no in-built tibial slope in its design. We did not try to impose a constant slope. The planned PTS was decided according to the native tibial slope of the patient. We did not reproduce the native slope, but the planned slope was decided by the operating surgeon keeping in mind the native slope and varying within a range from 0° to 7°. In the postoperative radiograph the PTS [Figure 3] was calculated by joining two lines. The first line was the line perpendicular to anatomical axis of tibia. The second line is formed by joining the two most proximal points along the region of the tibial bone cut. All measurements were taken by three different authors, and after concluding that there is a high interclass correlation coefficient (Single Measures Interclass Correlation Coefficient of 0.984) on agreement of measurements, the values measured by the senior surgeon were considered for the calculations.
Figure 3.

Postoperative x-ray knee (lateral view) showing calculation of the postoperative tibial slope
Appropriate statistical analyses were applied depending upon the distribution of the data with Microsoft Excel software. For finding correlation, as the data was quantitative and normally distributed with n > 30, Pearson's correlation coefficient was used to define the correlation between PTS and MDA. For comparing two groups defined on the basis of MDA, student's unpaired t-test was used with an alpha level of 0.05 and beta 0.2, that is, power (1-beta) of 80%.
RESULTS
Among the 100 patients studied the mean preoperative PTS was 11.64 with a standard deviation of 4.54° (range: 2-25°). The mean MDA was found to be 23.76° with a standard deviation of 5.50° (range: 8-38°) [Table 1]. There was a strong correlation between the PTS and the MDA (Pearson's coefficient of 0.72) [Figure 4].
Table 1.
Observed values of preoperative PTS and MDA
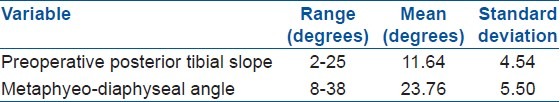
Figure 4.
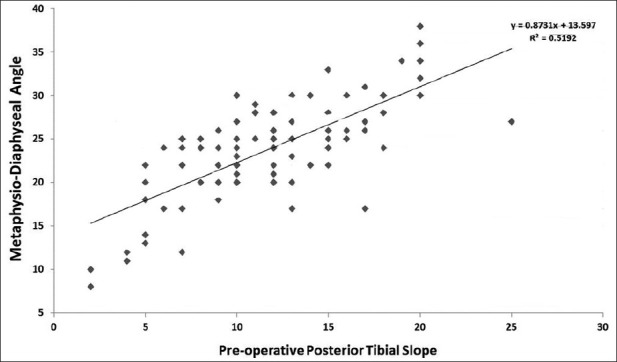
Scattered diagram showing relation between metaphysio-diaphyseal angle and preoperative posterior tibial slope
The accuracy of the mechanical jig provided for taking the posterior tibial cuts was also studied. The jig was of single manufacturer with provision to take cuts at different angles of PTS as desired by the surgeon. On analyzing post surgery radiographs, in 53 out of the total 100 patients (i.e. 53%) the achieved postoperative PTS was equal to the planned PTS [Table 2]. Out of the remaining 47% cases, 30 patients had a postoperative PTS, which was less than the planned PTS and 17 patients had postoperative PTS, which was more than the planned PTS. The mean planned PTS was 3.02° with a standard deviation of 2.76° (range: 0-7°). The mean postoperative PTS was 2.54 with a standard deviation of 2.90° (range: 5-7°). It was noted that there were two distinct groups [Table 3]. The group with MDA ≤20° were labeled group 1 (n = 26) and MDA >20° as group 2 (n = 74).
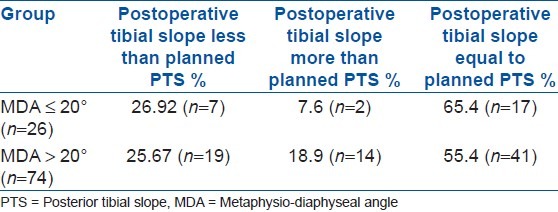
Table 2.
Variation in the postoperative PTS due to inaccuracy of cutting jig
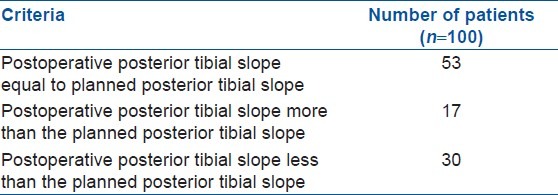
Table 3.
Postoperative PTS in the two groups defined by MDA
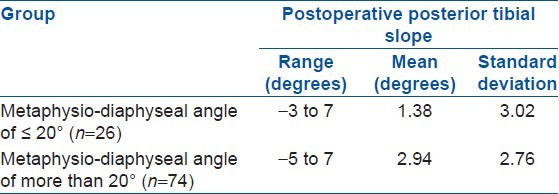
The planned PTS was different for each patient, which was decided during the preoperative planning. While comparing via unpaired t-test; although there was no statistically significant difference in between the two groups with regard to the planned PTS (with a P value of 0.71, i.e., P > 0.05), the difference in achieved postoperative tibial slope between the two groups was significant (P value for the difference was 0.0176, i.e., P < 0.05). Hence, the postoperative PTS in the group of patients with a MDA ≤20° was significantly less than the postoperative PTS in the group of patients with a MDA >20°. The difference between the postoperative PTS with respect to planned PTS is given in Table 4.
Table 4.
Relation between postoperative PTS and planned PTS in the two groups defined by MDA
DISCUSSION
The study highlights the ethnic differences in the PTS. Whereas the normal PTS has been quoted as 5-10°; racial differences in the PTS have been found.6–8,10,11 Asian population has been found to have an increased PTS as compared with Caucasian population. Moreover, it has been found that the PTS increases with the onset of osteoarthritis.7,12,13 The average PTS in our study was 11.64 with a standard deviation of 4.54. These values are similar to the values reported in literature by Khattak et al. (2010) in Pakistani population (12.5° in males and 14.2° in females),6 Chiu et al. (2000) in the Chinese population (13.1° in osteoarthritic knees and 10.8° in normal knees on radiographs)7 and Yoo in the Japanese population (10.6°).8 At the same time some other authors have reported lower PTSs in the Asian population.12,14 These variations in the PTS reported in the same population may be due to the difference in the reference axis and the methodology used in the calculation of the PTS.6–8,12–14
It was postulated in this study that the MDA might affect the PTS and hence affect the overall sagittal alignment of the proximal tibia. This has been confirmed by our present study where a strong Pearson's coefficient of correlation of 0.72 was found between the preoperative PTS and MDA. As the MDA affects the postoperative PTS independent of other factors as shown in our study, this entity holds potential for a new value to be taken into consideration while planning for sagittal anatomy in TKA.
It appears that the MDA affect the mechanical axis in the sagittal plane, because it brings the center of the knee backward. Therefore, it is susceptible to increase the difference between the anatomical axis obtained from an extramedullary jig (aligned on the diaphysis and the anterior cortical line8 ) and the mechanical axis: the greater the MDA, the greater the difference between the diaphyseal axis and the mechanical axis in the sagittal plane. Therefore, the surgeon, who bases himself on the diaphyseal axis, will restore the PTS based on the wrong axis, overestimating the real tibial slope in tibias with a great MDA. This could even lead surgeons to invert the tibial slope in tibias with low native PTS if any.
Second it appears, based on geometrical considerations, that, for a given PTS, the error between the mechanical axis and the anterior cortical line8 is increased when the MDA increases and vice versa. Therefore, it is important to investigate the relation between the MDA and the PTS.
Consequently, we
-
(1)
looked for the relation, if any, that might exist between the MDA and the PTS;
-
(2)
evaluated the potential error that might result from variations of the MDA, to finally evaluate the potential clinical relevance when performing a TKR.
We hypothesized that high MDAs could potentially lead surgeons to overestimate the PTS using extramedullary jigs and that it would require a substantial correction depending of the native MDA and PTS. We have attached a drawing to illustrate the hypothesis [Figure 5].
Figure 5.
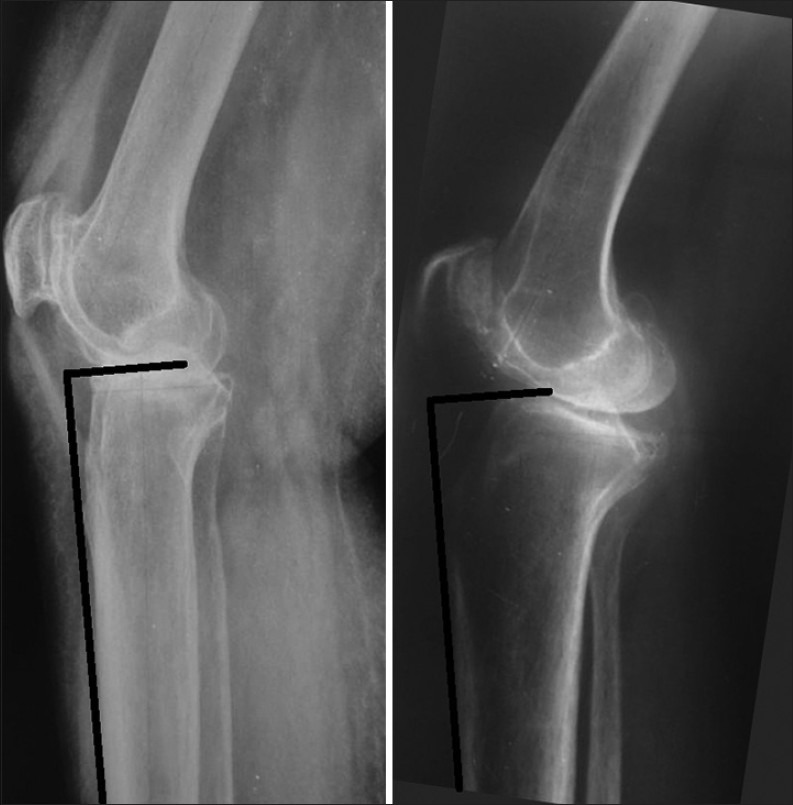
X-ray knee joint (lateral view) showing variation in cuts of extramedullary jig in cases with different MDAs
It was also found the MDA affects the accuracy of the extramedullary jig used for achieving the PTS and the PTS achieved intraoperatively. With all the other variables having no significant differences between the two groups; the group with a MDA less than 20° had a significantly decreased PTS than the group with a MDA more than 20° (P = 0.017). The angle of 20° was chosen because that particular demarcation showed a significant difference in the achieved postoperative PTS between the two groups. The variation in the achieved PTS could be explained by the altered proximal tibial anatomy in between cases with different MDA. As per the study by Yoo et al., (2008) the anterior cortical line of tibia can differ from the mechanical axis of tibia by as high as 6.2° (mean 3.2, SD 1.3).8 Thus, the extramedullary jig, which is kept parallel to the anterior cortical line, will not compensate for any change in the MDA and hence will lead to a different tibial cut depending on the MDA [Figure 5].
Kansara et al. (2006)15 did a clinical study on 61 patients undergoing TKA. The tibial cutting guides accurately achieved the intended posterior slope, but increasing posterior slope from 0° to 5° did not result in a significant increase in range of movement or Hospital for Special Surgery functional score. In addition, in some cases attempting a 0° slope gave rise to a negative slope, which was not seen with a 5° intended slope.15
There are some limitations of the study. Studies have shown that the most accurate method to measure the PTS is computed tomography (CT) scan.12,14 Besides medial tibial slope and lateral tibial slope vary in a single patient.7,12,13 However, Chiu et al., found a good agreement between the PTS measured on radiographs and the actual tibial slope measured on cadaveric tibia.7 Other anatomical aspects of the knee such as the coronal plane alignment of tibia and its variations with the age, sex, and the onset of osteoarthritis, the medio-lateral and antero-posterior dimensions of the tibia and the correlation between these variables were not considered. Further studies are needed to complete our knowledge regarding the anatomical variations in the Indian population. The study has been carried out in patients undergoing TKA with knees deformed due to osteoarthritis.
The gender of the patient has not been considered in this study. In a systematic review by Merchant et al. (2008)16 and study of 60 cadaveric knees by Dargel et al. (2011)17 observed that the male dimensions of knee are larger than their female counterparts; when adjusted for patients’ height and femoral length and on matched pair analysis there is no significant difference in the morphometric variables in male and female sex.17 Khattak et al. and Didia et al. did find a significant difference in the PTSs between the two sexes.6,11
In spite of these limitations, considering the above facts, we conclude:
The average PTS in Indian patients with osteoarthritic knees is higher than the Caucasian population and is almost equal to the PTS of the oriental population.
There is a significant correlation between the preoperative PTS and the MDA.
Because PTS and MDA vary in the same direction, there is a substantial risk of error when cutting the tibia based on an extramedullary jig The MDA should be considered during the planning of a Total Knee Replacement.
This error is substantial in patients with a high MDA (>20°): Only 55% of patients with MDA > 20° had postoperative PTS equal to the desired cut. In a patient with a MDA of less than 20°, planned PTS less than 3° should be avoided as it risks giving a negative tibial slope or an anterior tibial slope, which is associated with an adverse biomechanics. Moreover, in cases with a MDA of more than 20° a planned PTS of more than 5° should be avoided.
We think a PTS of 3-5° should be safe in all cases. Further studies will help in better understanding of applied anatomy of knee in TKA and its role in functional improvement.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Rodricks DJ, Patil S, Pulido P, Colwell CW., Jr Press-fit condylar design total knee arthroplasty.Fourteen to seventeen-year followup. J Bone Joint Surg Am. 2007;89:89–95. doi: 10.2106/JBJS.E.00492. [DOI] [PubMed] [Google Scholar]
- 2.Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The chitranjan ranawat award: Long term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res. 2006;452:28–34. doi: 10.1097/01.blo.0000229356.81749.11. [DOI] [PubMed] [Google Scholar]
- 3.Kettelkamp DB. American Academy of Orthopaedic Surgeons: Symposium on reconstructive surgery of the knee. St Louis: CV Mosby; 1976. Gait characteristics of the knee: Normal, abnormal, and post reconstruction; p. 47. [Google Scholar]
- 4.Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972;52:34–43. doi: 10.1093/ptj/52.1.34. [DOI] [PubMed] [Google Scholar]
- 5.Kim JM, Moon MS. Squatting following total knee arthroplasty. Clin Orthop Relat Res. 1995;313:177–86. [PubMed] [Google Scholar]
- 6.Khattak MJ, Umer M, Davis ET, Habib M, Ahmed M. Lower limb alignment and posterior tibia slope in Pakistanis: A radiographic study. J Orthop Surg. 2010;18:22–5. doi: 10.1177/230949901001800105. [DOI] [PubMed] [Google Scholar]
- 7.Chiu KY, Zhang SD, Zhang GH. Posterior slope of tibial plateau in Chinese. J Arthroplasty. 2000;15:224–7. doi: 10.1016/s0883-5403(00)90330-9. [DOI] [PubMed] [Google Scholar]
- 8.Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK. Anatomical references to assess the posterior tibial slope in total knee arthroplasty: A comparison of 5 anatomical axes. J Arthroplasty. 2008;23:586–92. doi: 10.1016/j.arth.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Massin P, Gournay A. Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty. 2011;26:124–30. doi: 10.1016/j.arth.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Yoga R, Sivapathasundaram N, Suresh C. Posterior slope of the Tibia Plateau in Malaysian patients undergoing total knee replacement. Malays Orthop J. 2009;3:78–80. [Google Scholar]
- 11.Didia BC, Jaja BN. Posterior slope of tibial plateau in adult Nigerian subjects. Int J Morphol. 2009;27:201–4. [Google Scholar]
- 12.Han HS, Chang CB, Seong SC, Lee S, Lee MC. Evaluation of anatomic references for tibial alignment in total knee replacement. Knee Surg Sports Traumatol Arthrosc. 2008;16:373–7. doi: 10.1007/s00167-008-0486-1. [DOI] [PubMed] [Google Scholar]
- 13.Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC, Jr, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90:2724–34. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G. Differences of knee anthropometry between chinese and white men and women. J Arthroplasty. 2011;26:124–30. doi: 10.1016/j.arth.2009.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kansara D, Markel DC. The effect of posterior tibial slope on range of motion after total knee arthroplasty. J Arthroplasty. 2006;21:809–13. doi: 10.1016/j.arth.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 16.Merchant AC, Arendt EA, Dye SF, Fredericson M, Grelsamer RP, Leadbetter WB, et al. The female knee: Anatomic variations and the female-specific total knee design. Clin Orthop Relat Res. 2008;466:3059–65. doi: 10.1007/s11999-008-0536-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dargel J, Michael JW, Feiser J, Ivo R, Koebke J. Human knee joint anatomy revisited: Morphometry in the light of sex- specific total knee arthroplasty. J Arthroplasty. 2011;26:346–53. doi: 10.1016/j.arth.2009.12.019. [DOI] [PubMed] [Google Scholar]


