Abstract
Background:
Incorrect positioning of the implant and improper alignment of the limb following total knee arthroplasty (TKA) can lead to rapid implant wear, loosening, and suboptimal function. Studies suggest that alignment errors of > 3° are associated with rapid failure and less satisfactory function. Computer navigated systems have been developed to enhance precision in instrumentation during surgery. The aim of the study was to compare component alignment following computer assisted surgery (CAS) and jig based TKA as well as functional outcome.
Materials and Methods:
This is a prospective study of 100 knees to compare computer-assisted TKA and jig-based surgery in relation to femoral and tibial component alignment and functional outcome. The postoperative x-rays (anteroposterior and lateral) of the knee and CT scanogram from hip to foot were obtained. The coronal alignment of the femoral and tibial components and rotational alignment of femoral component was calculated. Knee society score at 24 months was used to assess the function.
Results:
Results of our study show that mean placement of the tibial component in coronal plane (91.3037°) and sagittal planes (3.6058°) was significantly better with CAS. The difference was statistically insignificant in case of mean coronal alignment of the femoral components (90.34210° in navigation group and 90.5444° in jig group) and in case of the mean femoral condylar twist angle (external rotation 2.3406° in navigation group versus 2.3593° in jig group).
Conclusions:
A significantly improved placement of the component was found in the coronal and sagittal planes of the tibial component by CAS. The placement of the components in the other planes was comparable with the values recorded in the jig-based surgery group. Functional outcome was not significantly different.
Keywords: Component alignment, computer assisted surgery, jig based knee replacement, navigation
INTRODUCTION
Total knee arthroplasty (TKA) has been reported as one of the most successful procedures with survival rates greater than 90% after 15 years.1 Success depends on the preoperative condition of the patient, the design and materials of the components, surgical technique and surgeon's ability to properly align the extremity and position the components.1–8 It is important to position the femoral and tibial components accurately and to balance the soft tissues correctly as component mal alignment is the principle cause of early failure.9 This has been attributed to instability and patello-femoral complications. It is also a contributing factor in later failures due to polyethylene wear or fixation failure.10
Optimal alignment and adequate positioning can be achieved using traditional jigs and alignment guides, or by the use of computer navigation. It is recommended that in the coronal plane, the femoral and tibial components be positioned with less than 3° of error.2 Such placement has been achieved in 70% to 80% of patients using intramedullary or extramedullary alignment guides.3,4 Entry point of the intramedullary alignment guide is critical as it can change both the coronal and the sagittal alignment.5 For rotational alignment of the femoral component, use of the Whiteside line, the transepicondylar axis, and posterior femoral condyles is recommended to avoid problems of patellar maltracking.7 However, the transepicondylar axis can be identified visually within 3° in only 75% of arthritic knees and there may be errors in its identification when using a mini-invasive approach.11 A high degree of accuracy cannot be expected using conventional techniques for rotational alignment by palpating anatomical landmarks. CAS has been developed to improve accuracy of the alignment and orientation of the components in TKA. Some studies have indicated that there was no significant difference between CAS and conventional TKA.12 Others found a clear tendency toward improved alignment of the limb with CAS.13–15
The aim of our study was to compare CAS and jig-based TKA with respect to the component alignment in the coronal and sagittal plane of tibial component, and to assess the accuracy of the rotational alignment of the femoral components. We also aimed to study the functional outcome after each surgery in both techniques.
MATERIALS AND METHODS
After Institutional Ethical Committee approval and patient's written informed consent, we conducted a prospective study. We included 100 consecutive knees meeting the inclusion criteria, undergoing primary TKA in a 1 year period, which were at random alternately placed into two groups of 50 each. In total there were 46 left knees and 54 right knees. Group 1 consisted of surgeries performed using computer-assisted navigation. Group 2 consisted of surgeries using conventional jig-based methods. The patients who underwent primary TKA for tri-compartmental osteoarthritis were included in the study. Exclusion criteria consisted of those knees with more than 30° valgus and revision TKA's.
Implants used included NexGen LPS (Zimmer, USA), PFC Sigma DePuy (Johnson and Johnson, USA), and INOR Total Condylar System (INOR Orthopedics, Mumbai, India), selection of which was determined by the socioeconomic status of the patient [Figure 1]. The bilateral TKA's were performed one week apart. Single surgeon (JT) performed all the cases.
Figure 1.
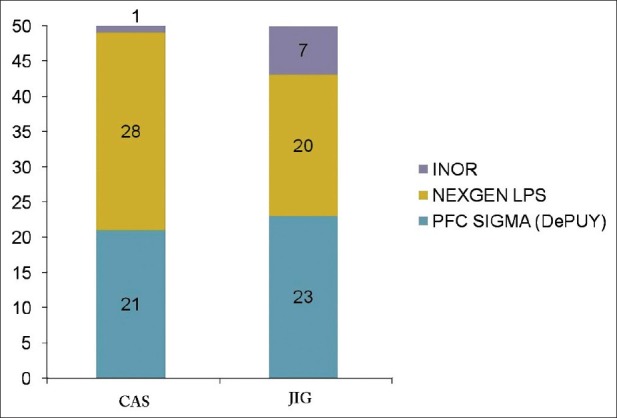
Bar diagram showing depicting the implants used
A standard midline approach with a medial parapatellar arthrotomy was used. The tibial cut was made first. The posterior slope of the tibial component varied with the implant selected as per the implant specific guidelines.
In the CAS group (Group 1), a navigation system (Vector Vision CT-free Knee; Brain LAB, Munich, Germany) with an optical tracking unit was used. Bone cuts were made as per the image reconstructed by the computer. In the Group 2, intramedullary jig was used for the distal femoral cut and an extramedullary alignment guide was used for cutting the proximal tibia.
Postoperative protocol consisted of 3 days intravenous antibiotics, deep vein thrombosis prophylaxis of injection Fondaparinaux 2.5 ml subcutaneously OD on day of surgery, and tablet Aspirin 300 mg OD for 6 weeks at discharge. Patients were ambulated the next day post surgery and discharged by the fifth day.
Prior to discharge, patients underwent anteroposterior and lateral radiographs of the knees and a CT scanogram from the hip to the foot [Figure 2]. A protocol for the scan was submitted to the radiology department for standardization of the images. Anatomical landmarks determined as per the Perth protocol included the center of the femoral head, the center of the talus, midpoint of the intercondylar notch, and center of the polyethylene insert/tibial plateau [Figure 3a]. On axial cuts, the lowest point of the sulcus between the attachments of superficial and deep medial collateral ligaments was marked, as was the tip of lateral epicondyle. The mechanical and anatomical axes were identified. The alignment of the prosthesis was then measured against the mechanical axis in both AP and lateral planes. The medial angles thus formed was to yield the coronal alignment of the femoral component and tibial components [Figures 3b,c]. The coronal alignment angle was measured against the target alignment of 90°. An angle of <90° was classified as varus alignment of the component, angle of >90° was classified as valgus. The rotation of the femoral component was measured relative to the axis between the medial sulcus and lateral epicondyle.
Figure 2.

Postoperative CT scanogram of the lower extremity from hip to foot showing implant in situ
Figure 3.
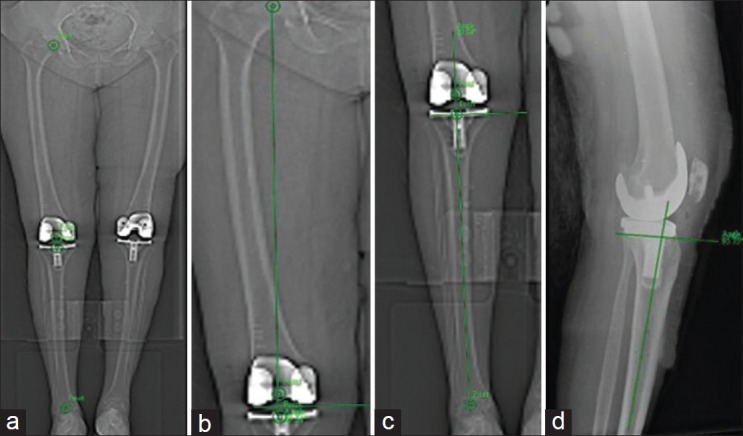
(a) CT scanogram showing center of the femoral head, talus, intercondylar notch, and polyethylene insert as marked, (b) Center of femur head is joined with a line to the center of the intercondylar notch. A tangent is drawn to the articular surface of the femoral condyles. The medial angle thus formed represents the coronal alignment of the femoral component, (c) Center of the tibial base plate is joined to the center of the AQ4 ankle. A second line is drawn parallel to the undersurface of the tibial component. The medial angle thus formed represents the coronal alignment of tibial component, (d) Center of the talus is joined to the center of the proximal tibia on lateral radiograph. The angle formed between this line and the line drawn parallel to the undersurface of the tibia gives the posterior slope of tibial component
Lateral radiographs were considered satisfactory if the knee was well centered without substantial limb rotation. The alignment of the femoral pegs on the lateral radiograph was used to determine limb rotation when such pegs were present. A complete overlap between the two pegs denotes no limb rotation relative to the radiographic plate. A partial overlap was accepted. The posterior angle formed by the undersurface of the tibial component and the tibial axis was measured [Figure 3d]. The target implantation was set between 3° and 7° posterior slope in this study keeping in mind the different implants being used. The rotational deviation of the femoral component from the referenced axis was determined by the angle between the line connecting the posterior femoral condyles and the line connecting the sulcus and lateral epicondyle [Figure 4].
Figure 4.
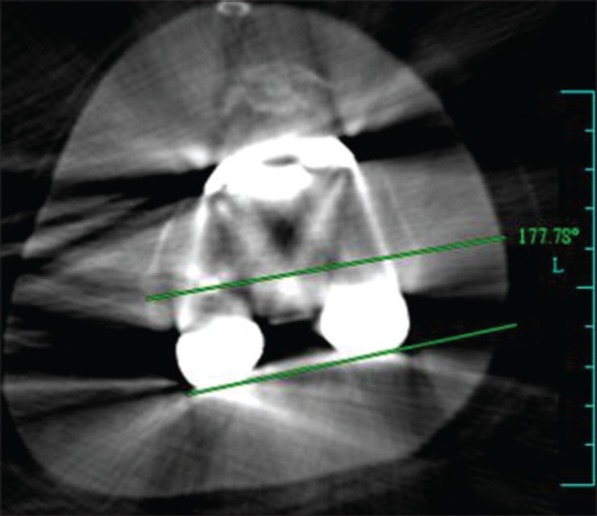
Axial CT shows angle between the line connecting the posterior femoral condyles and the line connecting the medial sulcus and lateral epicondyle measures the femoral condylar twist angle
The data was recorded by two independent observers, on two identical master charts, collaborated at the end of the study. The mean of two measurements was recorded for each evaluated film. 24 month followup Knee Society Scores were used.
Data was analyzed using SPSS, using an unpaired t-test to assess inter-observer variability for the mechanical axis of the tibia. The Wilcoxon signed rank test was used for the other parameters. The error, i.e., deviation away from the acceptable limits, was assessed with the Mann–Whitney test. The level of significance was set at P = 0.05 for the radiographic parameters and P = 0.001 for the functional outcome.
RESULTS
In Group 1 (CAS), there were 27 patients–17 women (32 knees) and 10 men (18 knees) with a mean age of 66.84 years (SD 5.912 yrs, range: 56–81 years). A mean preoperative deviation of the axis of the leg assessed on weight bearing radiographs was 6.17° varus (SD 8.216, range 21.37° varus to 24.43° valgus on right and 17.11° varus to 6.16° valgus on left).
In Group 2, there were 31 patients-26 women (43 knees) and 5 men (7 knees) with a mean age of 64.86 years (SD 8.204 years, range 56 to 80 years) and a mean preoperative deviation of 7.77° varus (SD 12.071, range 34.09° varus to 17.99° valgus on right and 43.1° varus to 20.91° valgus on left). There is no statistically significant difference in the outcomes based on the preoperative axis deviation (Fisher's Exact test; P = 0.156). No significant inter-observer variability for any of the parameters was observed.
Mean coronal alignment of the femoral component was found to lie within the 3°of acceptable deviation from midline. In Group 1, the mean angle was 90.34210° (SD: 94.355° valgus–86.725° varus) while in Group 2 mean angle was 90.5444° (SD: 97.15° valgus–86.025° varus). Hence, there was greater variability in the component positioning in Group 2. However, there was no significant difference in the overall coronal femoral component alignment (P = 0.777; Mann–Whitney test). Further, there were a greater number of outliers in Group 2, but this was statistically insignificant (P = 0.286; Mann–Whitney Test).
Mean coronal alignment of the tibial component in Group 1 was 91.3037° (95.69°-87.62°), while that in Group 2 was 90.2663° (98.405°-86.265°). The variation from the mean value was significantly greater in group 2 (P = 0.008; two-tailed t test). This variation from the 3° of acceptability was found to be statistically insignificant (P = 0.229; two-tailed t test). Hence, within the acceptable limits, the values in Group 1 were found to be closer to the target value of 90°. Statistically, there was significant difference in the variability of tibial component alignment in the coronal plane with respect to deviation from 90° (P = 0.008; t-test). We deduced that CAS helps increase the accuracy of the tibial component alignment in the coronal plane.
Femoral condylar twist angle was ideally set for 3° external rotation. Up to 3°of rotation on either side of this value was deemed acceptable. Our study showed that the mean value for both groups fell within the limits of acceptability–Group 1 had a mean of 2.3406° of external rotation (10.065°-0.32°), whereas Group 2 demonstrated a mean value of 2.3593° of external rotation (6.29°-0.143°). When the outliers from the 3° mark were tested statistically, there was no difference between the two groups (P < 0.157; two-tailed t test). A significant difference in favor of Group 1 was detected with respect to variation from the mean of the posterior slope (P = 0.002; two-tailed t test). The mean was 3.6058°(0.98°–8 - 94°) in Group 1, while it was 4.9491° (0.85°-9.79°) in Group 2. When the outliers from the acceptable was compared though, there was no significant difference between the two groups (P = 0.571, Mann–Whitney Test). Knee score had a mean of 90.94 in Group 1 (82-98) and 88.90 (80-100) in Group 2 (P = 0.013; two-tailed t test). There was no significant difference in the functional scores either; Mean: 91.90 (75-100) for Group 1 and 89.90 for Group 2 (80-100) (P = 0.026; Mann–Whitney Test). An average of 90 min tourniquet time was observed in both groups.
On followup of 24 months two cases in Group 2 developed deep vein thrombosis (DVT) while no Group 1 cases presented with DVT. There have been no cases of revision TKA for implant loosening or failure in either of the groups. There have been two cases of infection, one in each group, both of which settled after a debridement and insert change.
DISCUSSION
The number of TKAs is increasing annually, while the mean age of patients undergoing this procedure is decreasing. Thus, attention has been drawn to the longevity of the TKA.16 The optimal positioning and alignment of prosthetic components are critical to long term success of TKA.17,18 Unfavorable outcomes include pain, instability,19 limited range of motion, polyethylene wear, and implant loosening.10 These are perpetuated with improper positioning of implants. Postoperative mechanical axis within 3° valgus or varus is associated with an improved outcome.19 Malalignment of the prosthesis may lead to deleterious stresses on implanted components and to increased wear rates, which are reflected in poor short and long term results and in higher failure and revision rates.7,8,20,21
Mahaluxmiwala et al.3 have reported that in 25% of 654 knees, surgeons irrespective of their experience level failed to achieve alignment within ±3° of the mechanical axis. Petersen and Engh5 have shown that there was a 26% failure to achieve alignment to within 3° of varus or valgus. Varied reasons have been proposed for the inaccuracy on the femoral side such as bowed femora, wide medullary canals, and incorrect entry point. Nagamine et al.22 have also shown anatomical variations to occur in osteoarthritic patients that are generally not considered in conventional TKA. These drawbacks can be circumvented with extramedullary guide jigs for the tibia. Extramedullary instrumentation is less accurate for the femoral side and inaccuracies are heightened in obese patients.18
Malalignment of the tibial component alters the distribution of tibial loading and can increase shear forces at the tibio-femoral interface, resulting in increased wear. A threshold of 3° of varus malalignment has been reported to significantly increase the risk of medial bone collapse.23 Aglietti and Buzzi reported a statistically significant increase in radiolucent lines and in probable loosening if tibio-femoral varus or tibial component varus of more than 2° was present. Vince et al. noted that all cases in their series with tibial loosening were aligned in varus, and 80% of the knees placed in varus required a revision.24
In this study, the findings for coronal alignment of the components were the same as with the findings of Mullaji et al.25 and Jean-Yves Jenny et al.13 On the other hand, Anderson et al.26 reported a significant difference between the two groups (P < 0.001). Only a few studies have demonstrated any advantage of the navigation system with respect to rotational alignment. Using the image-free system, it is uncertain whether digitizing the bony landmarks is precise, and the accuracy of the rotational alignment is still in question.26–29
Many authors17,30,31 have reported variability in the identification of the transepicondylar axis. We have used the medial sulcus for the medial landmark in this study.
In this study, 75% of the femoral components were implanted within 3° of the ideal rotational alignment. 20% cases in Group 1 were outside the 3° cut-off mark (mean 2.3406°), while 30% of cases in the Group 2 fell outside the acceptable limit (mean 2.3593°); however, there was no statistically significant difference in this condylar twist angle when using the navigation technique, which is in keeping with most of the studies done for assessing the rotational alignment of the components including the study by Choong et al.32 In contrast, Chauhan et al.33 and Stockl et al.34 have reported improved rotational alignment of the components after navigated TKA.
Anderson et al.35 reported that the tibial posterior slope was 3.98 in the control group and 3.08 in the navigation group (P < 0.03). Our study, on the contrary, showed a significantly improved outcome in those cases treated with navigation. Both the groups drew mean values within the acceptable range, but the range and deviation from the mean were significantly higher in Group 2 (P < 0.002, Mann–Whitney Test).
It is difficult for a patient who has undergone bilateral TKA to separate the function of each knee. Although this is a problem when assessing function after bilateral TKA, we believe that we were able to obtain fairly accurate information after careful assessment of the performance of each knee. Since long term implant survival of conventional TKA has been shown to be excellent, functional assessment and overall quality of life are becoming more critical issues in the evaluation of success in TKA.12,36 In our study, the knee score in terms of measurements, range of movement, and pain levels was contrary to the findings in the paper published by Choong et al.32 who suggested better function and quality of life for patients following navigation surgery.
Limitations of our study are that, due to varying socioeconomic status between patients we had to use different implants. This may be considered a confounding factor.
There were also huge variations in the preoperative deformities of the knees ranging from 34.09° varus to 24.43° valgus, which may present as a confounding factor in the accuracy of placement of components as well as soft tissue balancing. However, our results between the final operative outcomes showed acceptable degrees of correction in all the patients. The preoperative wide range of varus and valgus, though present, were equally distributed in both groups. And since we were comparing outcome of two techniques, and not surgical methods, it was not relevant or beneficial to our study to exclude those patients.
We had two cases of complications of DVT in Group 2. However, since tourniquet time was not significantly prolonged in either group, the 2 cases of DVT were incidental observations, and cannot be attributed to increasing time for venous stasis.
In conclusion, coronal alignment of femoral component is comparable in both groups; however, coronal and sagittal plane alignment of tibial component is statistically significantly better in the CAS group (Group 1). CAS also demonstrates its fair share of errors, which however are comparable with those made in the conventional jig-based surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Rodricks DJ, Patil S. Press-fit condylar design total knee arthroplasty: Fourteen to seventeen-year followup. J Bone Joint Surg Am. 2007;89-A:89–95. doi: 10.2106/JBJS.E.00492. [DOI] [PubMed] [Google Scholar]
- 2.Jeffery RS, Morris RW. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–14. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 3.Mahaluxmivala J. The effect of surgeon experience on component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty. 2001;16:635–40. doi: 10.1054/arth.2001.23569. [DOI] [PubMed] [Google Scholar]
- 4.Petersen TL, Engh GA. Radiographic assessment of knee alignment aftertotal knee arthroplasty. J Arthroplasty. 1988;3:67–72. doi: 10.1016/s0883-5403(88)80054-8. [DOI] [PubMed] [Google Scholar]
- 5.Mihalko WM, Boyle J. The variability of intramedullary alignment of the femoral component during total knee arthroplasty. J Arthroplasty. 2005;20:25–8. doi: 10.1016/j.arth.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 6.Matsuda S, Miura H, Nagamine R, Urabe K, Mawatari T, Iwamoto Y. A comparison of rotationallandmarks in the distal femur and the tibial shaft. Clin Orthop Relat Res. 2003;414:183–8. doi: 10.1097/01.blo.0000072904.36018.79. [DOI] [PubMed] [Google Scholar]
- 7.D’Lima DJ, Patil S. Dynamic intraoperative ligament balancing for total knee arthroplasty. Clin Orthop Relat Res. 2007;463:208–12. [PubMed] [Google Scholar]
- 8.Griffin WL, Fehring TK. Sterilization and wear-related failure in first- and second generation press-fit condylar total knee arthroplasty. Clin Orthop Relat Res. 2007;464:16–20. [PubMed] [Google Scholar]
- 9.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–8. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 10.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Why are total knee arthroplastiesfailing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Yau WP, Leung A, Liu KG, Yan CH, Wong LS, Chiu KY. Errors in the identification of the transepicondylar and anteroposterior axes of the distal femur in total knee replacement using minimally- invasive and conventional approaches: A cadaver study. J Bone Joint Surg Br. 2008;90:520–6. doi: 10.1302/0301-620X.90B4.19841. [DOI] [PubMed] [Google Scholar]
- 12.Kim YH, Kim JS. Alignment and orientation of the components in total knee replacement with and without navigation support a prospective, randomized study. J Bone Joint Surg Br. 2007;89:471–6. doi: 10.1302/0301-620X.89B4.18878. [DOI] [PubMed] [Google Scholar]
- 13.Jenny HY, Mielke RK, Kohler S, Kiefer H, Konermann K, Boeri C, et al. Total knee prosthesis implantation with a non image based navigation system a multicentric analysis. Proceedings from the 70th Annual Meeting of the American Academy of Orthopedic Surgeons. Rosemont III. Am Acad Orthop Surg. 2003;96 [Google Scholar]
- 14.Bäthis H, Perlick L, Tingart M, Lüring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty: comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682–87. doi: 10.1302/0301-620x.86b5.14927. [DOI] [PubMed] [Google Scholar]
- 15.Insall JN, Ranawat CS. A comparison of four models of total knee- replacement prosthesis. J Bone Joint Surg Am. 1976;58-A:754–65. [PubMed] [Google Scholar]
- 16.Victor J, Hoste D. Image-based computer-assisted total knee arthroplasty lead to lower variability in coronal alignment. Clin Orthop Relat Res. 2004;428:131–9. doi: 10.1097/01.blo.0000147710.69612.76. [DOI] [PubMed] [Google Scholar]
- 17.Ritter MA, Farris PM. Postoperative alignment of total knee replacement: Its effect on survival. Clin Orthop Relat Res. 1994;299:153–6. [PubMed] [Google Scholar]
- 18.Weng YJ, Hsu RW, Hsu WH. Comparison of computer assisted navigation and conventional instrumentation for bilateral total knee arthroplasty. JArthroplasty. 2009;245:668–73. doi: 10.1016/j.arth.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Kumar PJ, Dorr LD. Severe malalignment and softtissue imbalance in total knee arthroplasty. Am J Knee Surg. 1997;10:36–41. [PubMed] [Google Scholar]
- 20.Spencer JM, Chauhan SK. Computer navigation versus conventional total knee replacement: No difference in functional results at two years. J Bone Joint Surg Br. 2007;89:477–80. doi: 10.1302/0301-620X.89B4.18094. [DOI] [PubMed] [Google Scholar]
- 21.Patil S, D’Lima DD. Improving tibial component coronal alignment during total knee arthroplasty with use of a tibial planing device. J Bone Joint Surg Am. 2007;89:381–7. doi: 10.2106/JBJS.F.00204. [DOI] [PubMed] [Google Scholar]
- 22.Nagamine R, Miura H, Bravo CV, Urabe K, Matsuda S, Miyanishi K, et al. Anatomic variations should be considered in total knee arthroplasty. J Orthop Sci. 2000;5:232–7. doi: 10.1007/s007760050157. [DOI] [PubMed] [Google Scholar]
- 23.Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, et al. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 24.Kim SJ. Computer assisted navigation in total knee arthroplasty improved coronal alignment. J Arthroplasty. 2005;20:123–31. doi: 10.1016/j.arth.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Mullaji A, Kanna R, Marawar S, Kohli A, Sharma A. Comparison of limb and component alignment using computer-assisted navigation versus image intensifier guided total knee arthroplasty-a prospective, randomized, single-surgeon study of 467 knees. J Arthroplasty. 2007;22:953–9. doi: 10.1016/j.arth.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 26.Kansara D, Markel DC. The effect of posterior tibial slope on the range of motion after total knee arthroplasty. J Arthroplasty. 2006;21:809–13. doi: 10.1016/j.arth.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 27.Lesh ML, Schneider DJ, Deol G, Davis B, Jacobs CR, Pellegrini VD., Jr The consequences of anterior femoral notching in total knee arthroplasty: A biomechanical study. J Bone Joint Surg Am. 2000;82A:1096–101. doi: 10.2106/00004623-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Lachiewicz PF, Soileau ES. Patella mal tracking in posterior-stabilized total knee arthroplasty. Clin Orthop Relat Res. 2006;452:155–8. doi: 10.1097/01.blo.0000238803.97713.7d. [DOI] [PubMed] [Google Scholar]
- 29.Dutton AQ, Yeo SJ. Computer assisted minimally invasivetotal knee arthroplasty compared with standard total knee arthroplasty. J Bone Joint Surg Am. 2009;91:116–30. doi: 10.2106/JBJS.H.01549. [DOI] [PubMed] [Google Scholar]
- 30.Mizu-uchi H, Matsuda S, Miura H, Higaki H, Okazaki K, Iwamoto Y. The effect of ankle rotation on cutting of the tibia in total knee arthroplasty. J Bone Joint Surg Am. 2006;88A:2632–6. doi: 10.2106/JBJS.E.01288. [DOI] [PubMed] [Google Scholar]
- 31.Windsor RE, Scuderi GR. Mechanisms of failur of the femoral and tibial components in total knee arthroplasty. Clin Orthop Relat Res. 1989;248:15–9. doi: 10.1097/00003086-198911000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Choong PF. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24:560–9. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 33.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer assisted knee arthroplasty versus a conventional jig based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004;86:372–7. doi: 10.1302/0301-620x.86b3.14643. [DOI] [PubMed] [Google Scholar]
- 34.Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2004;426:180–6. doi: 10.1097/01.blo.0000136835.40566.d9. [DOI] [PubMed] [Google Scholar]
- 35.Anderson KC, Buehler KC, Markel DC. Computer assisted navigation in total knee arthroplasty: Comparison with conventional methods. J Arthroplasty. 2005;20:132–8. doi: 10.1016/j.arth.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 36.Decking R, Markmann Y. Leg axisafter computer-navigated total knee arthroplasty-a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20:282–8. doi: 10.1016/j.arth.2004.09.047. [DOI] [PubMed] [Google Scholar]


