Abstract
Background:
Failed infected internal fixation produces significant pain and functional disability. In infected internal fixation of hip fractures with partial or complete head destruction, total hip arthroplasty (THA) can be technically challenging; however, it restores hip biomechanics. The present study is to evaluate the results and assess the complications of THA following failed infected internal fixation of these fractures.
Materials and Methods:
A retrospective review of prospectively collected data in a tertiary healthcare center was performed of 20 consecutive patients of THA following failed infected internal fixation operated between September 2001 and November 2007. There were 11 dynamic hip screw failures for intertrochanteric fractures, 6 failed osteotomies following transcervical fractures, and 3 failed screw fixations for transcervical fractures.
Results:
The average age of the patients was 48.5 years (range 28-70 years) and the average followup period was 6.5 years (range 3.5-10.5 years). An indigenously designed cement spacer was used in a majority of patients (n = 15). The custom-made antibiotic impregnated cement spacer was prepared on-table, with the help of a K-nail bent at 130°, long stem Austin Moore's prosthesis (n=1), Charnley's prosthesis (n=1), or bent Rush nail (n=1). The antibiotic mixed cement was coated over the hardware in its doughy phase and appropriately shaped using an asepto syringe or an indigenously prepared spacer template. Nineteen of the 20 patients underwent two-stage revision surgeries. The average Harris hip score improved from 35.3 preoperatively to 82.85 postoperatively at the last followup. A significant difference was found (P < 0.0001). None of the patients had recurrence of infection.
Conclusions:
The results were comparable to primary arthroplasty in femoral neck fractures. Thus, THA is a useful salvage procedure for failed infected internal fixation of hip fractures.
Keywords: Hip fracture, infection, failed internal fixation, antibiotic spacer, total hip arthroplasty
INTRODUCTION
Failed internal fixation of hip is a problem of varied etiology. The problems get compounded when there is the presence of infection around the hip implants.1 Deep infection after a hip fracture operation impairs functional outcome and increases mortality by 10.4%.2 Eradication of infection becomes necessary for any definitive procedure to be performed on the hip. The patients are distressed because of pain and functional disability.3
With the recent advances in orthopedic surgery, the indications for Girdlestone resection arthroplasty after failed operated fractures of the hip are very limited.4 The reported results of Girdlestone's arthroplasty are variable with satisfactory results reported by some studies,5–8 and poor outcome by others.9–12 Hence, this procedure remains viable only in medically suboptimal patients.4 Total hip arthroplasty (THA) for failed and infected internal fixation of hip fractures is a difficult procedure. The problems which are frequently encountered are poor bone stock, significant osteoporosis, distorted anatomy, contracted soft tissues, and also the severe deformities which may be present due to the fractures.1,3,13,14 The presence of screws also adds to the difficulties as they act as stress risers and also allow the cement to pass through screw holes. The management of these difficult conditions requires a thorough surgical debridement, proper antibiotic coverage, and precise preoperative planning and anticipation of the difficulties to be encountered. THA remains the only salvage procedure for this group of patients in order to provide a stable, mobile hip with restored biomechanics.
The present series encompasses all the fractures of the hip joint including trans-cervical and intertrochanteric fractures as well as osteotomies used to treat proximal femoral fractures. The aim of the present study is to evaluate the results and assess the complications of THA following failed infected internal fixation of these fractures.
MATERIALS AND METHODS
A retrospective analysis of prospective data collected from 20 consecutive patients of total hip arthroplasty following failed infected internal fixation operated between September 2001 and November 2007 was carried out [Table 1].
Table 1.
Clinical details of patients
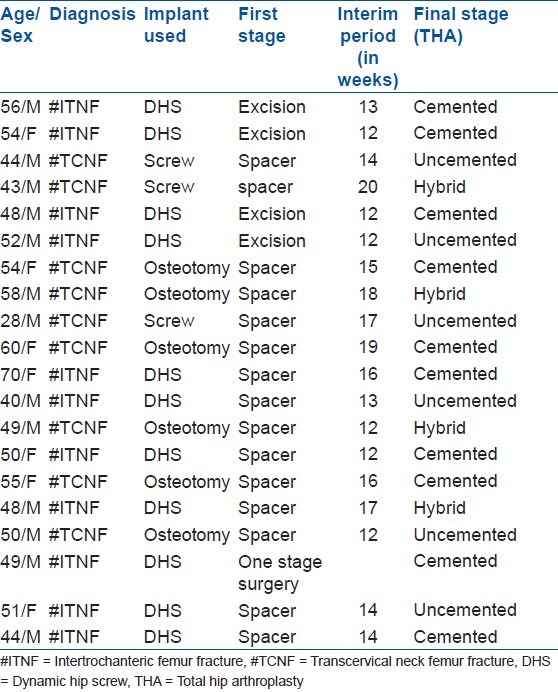
All patients were operated by a single senior surgeon (SSM). There were 13 males and 7 females. The average age of the patients was 48.5 years (range: 28-70 years) with the average followup period of 6.5 years (3.5 to 10.5 years). There were 11 dynamic hip screw failures for intertrochanteric fractures, 6 failed osteotomies following proximal femoral fractures, and 3 failed screw fixations for transcervical fractures. The duration between the index surgery for fracture fixation and the time of presentation ranged between 8 months and 3 years. All patients had undergone mean 2.05 previous surgeries per patient (range 1-4 surgeries). The diagnosis of infection was made on the basis of clinical criteria like persistent pain, local swelling, discharging sinus, as well as laboratory investigations like erythrocyte sedimentation rate (ESR) and C-reactive proteins (CRP). Radiology also aided in the diagnosis by the presence of osteolysis around the implants as well as periosteal reaction. Failed internal fixation was defined by nonunion at fracture site and/or implant failure. Preoperative aspiration of the joint fluid was done in all cases under strict aseptic precautions. A positive culture was a definite indicator of infection though a negative result did not rule out infection [Figures 1A & 1B].
Figure 1A.
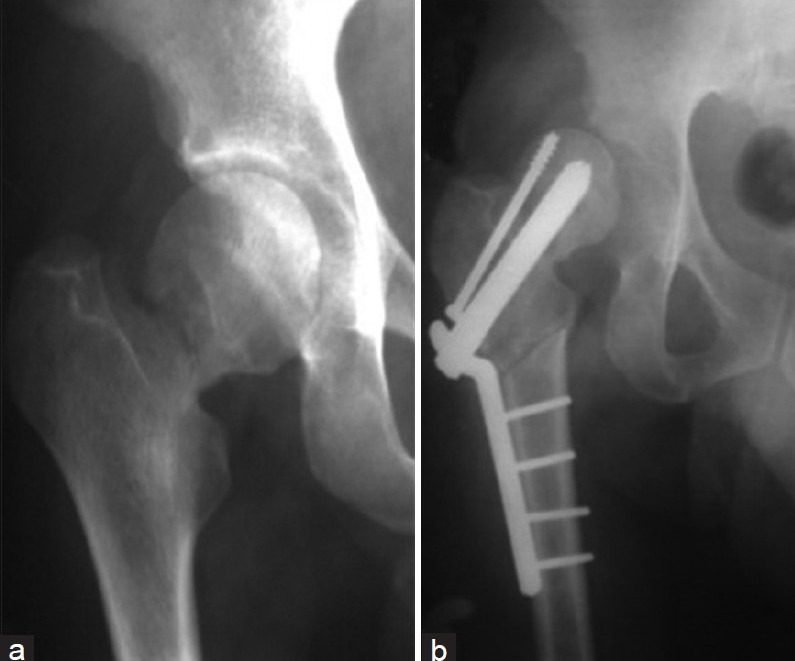
(a) Radiograph of right hip joint (anteroposterior view) of a 49 year-old male showing fracture neck femur (b) postoperative radiograph of right hip (anteroposterior view) of same patient showing osteotomy done for fracture neck femur after failed fixation
Figure 1B.
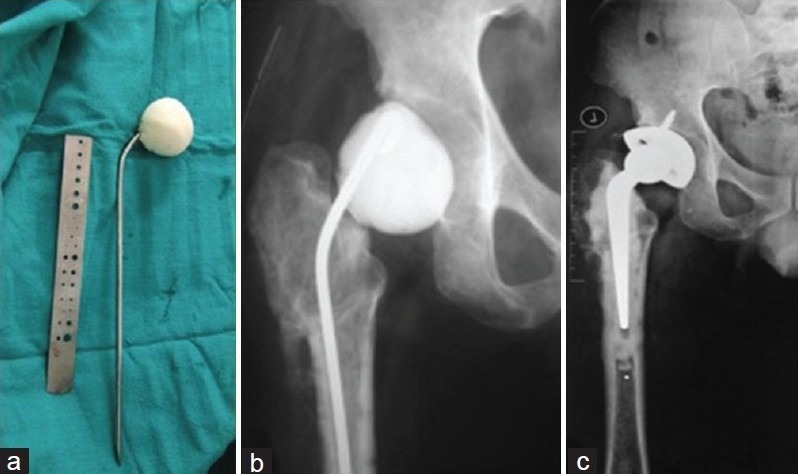
(a) Intraoperative photograph of a custom-made antibiotic cement spacer over bent rush nail (b) Radiograph of right hip (anteroposterior view) after first stage showing antibiotic cement spacer in situ (c) Final radiograph of the patient after re-implantation arthroplasty
Nineteen out of the 20 patients were treated with two-stage revision surgery while only 1 had a one-stage revision. Surgery was performed with the patient in the lateral position through a posterolateral approach. Wherever possible, the previous incision scar was included in incision. If not possible, an adequate gap was maintained in between old and new incision to prevent risk of flap necrosis and poor wound healing. The first stage included excision of the sinuses, removal of implants, foreign materials and all potentially infected tissues, thorough debridement and implantation of an antibiotic impregnated cement spacer. Intraoperative samples were taken from three different locations — subcutaneous tissues, from the hip joint, and from the femoral canal (intramedullary)— and were sent for histopathology as well as culture and antibiotic sensitivity. The implants were removed, head and neck of femur were excised, and canal was reamed till the appropriate diameter. The emphasis was on thorough and radical debridement and excision of all infected tissues. Copious normal saline pulse lavage wash was given.
In 15 patients, a custom-made antibiotic impregnated cement spacer was made on-table, the most common being made with the help of a K-nail (Kuntscher femur nail) (n = 12) bent at 130°. The others that were used were long stem Austin Moore's prosthesis (n = 1), Charnley's prosthesis (n = 1), and a bent Rush nail (n = 1). The choice of antibiotic used in the cement was determined by the organism isolated in preoperative cultures and its antibiotic sensitivity. If no organism could be isolated preoperatively, then 4 g of Vancomycin were added to two packets of 40 g Gentamicin impregnated cement. The cement was coated over the hardware in its doughy phase and appropriately shaped using an asepto syringe or an indigenously prepared spacer template [Figure 2]. The final adjustments were made according to the size of the femoral canal. Once the cement was set, the spacer was inserted into the femoral canal and the head reduced in the acetabulum. The wound was closed in layers over a negative suction drain. Among the remaining five patients, four underwent a Girdlestone like excision arthroplasty, while on one patient a single stage arthroplasty was performed. The decision to choose between excision arthroplasty vs spacer was taken based on technical difficulties faced intraoperatively. Spacer maintains soft tissue tension, avoids shortening, improves gait pattern, and provides local release of antibiotics. Hence, wherever possible, and especially in later cases of the series, (15 out of 20 cases), a spacer was chosen over excision arthroplasty.
Figure 2.

Clinical photograph showing indigenously prepared template for appropriate shaping of cement spacer
Postoperatively, the patients were given a third generation cephalosporin and an aminoglycoside (according to the hospital infection control committee protocol) till a definitive culture and antibiotic sensitivity report was obtained, after which the patients were shifted over to the antibiotics for which the organism was sensitive to. Duration of antibiotic was for 6 weeks, which is similar to most studies on two-stage revision for periprosthetic infection.15 The therapy was divided in to two injectable antibiotics for a period of 3 weeks, followed by oral antibiotics for 3 more weeks (similar to Younger et al.).16 The patients were then kept without antibiotics for 3-6 weeks after which they were reassessed. Systemic and local signs of infection were looked for; ESR and CRP levels were estimated weekly. A preoperative aspiration of the hip was performed before the second surgery. Only when all these investigations were within normal limits, the patient was taken up for the second surgery. The average time-interval between the two surgeries was 10 weeks (range: 8-16 weeks). In this interim period, all patients (including excision arthroplasty cases) were ambulatory and relatively pain-free with partial weight borne on the affected limb after 5th postoperative day with the help of a walker or axillary crutches.
Re-implantation arthroplasty
Preoperative templating of the hip was done using radiographs of the pelvis with both hips anteroposterior and lateral views. A wide range of implants were kept ready during the revision surgery due to technical difficulties involved. At reimplantation, the pre-existing surgical approach used for first stage was utilised. The scar tissues as well as any unhealthy tissues were removed. Samples were obtained at various planes and sent for frozen section. On a frozen section, a polymorph count of >10/high power field was taken to be diagnostic of infection as recommended by Lonner et al., in their prospective study on reliability of analysis of intraoperative frozen sections.17 The frozen sections in 19 of 20 patients turned out to be negative (less than 5 polymorphs per high power field) and we could proceed for the reimplantation.
One patient who had a positive frozen section, a new spacer was inserted, and definitive arthroplasty was done at the third stage. After this, the spacer was removed and the definitive prosthesis was inserted. The decision about the type of prosthesis to be used was made according to the age, bony architecture, canal flare index as well as the residual bone stock of the patient. If bone cement was used for fixation at the time of reimplantation, antibiotic impregnated cement was preferred. None of the patients with failed osteotomies required reosteotomies to negotiate the femoral canal. All patients received intravenous antibiotics for 5 days postoperatively.
All the patients were evaluated at 6 weeks, 12 weeks, 6 months and yearly thereafter. The presence of pain at rest as well as on ambulation and the range of motion of the hip were calculated. ESR and CRP levels were estimated at each followup till one year of followup. The patients were functionally evaluated according to Harris hip score before the surgery, in the interim period between the two surgeries and at every visit after the second surgery.
The data was analyzed using Microsoft Excel 2007 and PASW Statistics 18.0. The normality of the preoperative and postoperative Harris hip score was tested using the Kolmogorov-Smirnov test and the paired t-test was used for significance. The P value <0.05 was taken as significant.
RESULTS
The average followup period was 6.5 years (range 3.5-10.5 years). The mean duration between the index surgery for fracture fixation and presentation was about 1.4 years (range: 8 months to 3.2 years). Of the 20 patients, 14 of them had undergone more than one previous surgery, of which 4 were for revision of fracture fixation while the remaining 10 had undergone debridement with retention of fixation devices for the eradication of infection. The diagnosis of infection was made on the basis of discharging sinus in 14 and persistent pain with positive preoperative aspiration in the remaining 6 patients. ESR and CRP levels were correlating well with the presence of infection with all the patients showing high levels of both ESR and CRP preoperatively. A definite organism could be isolated in 19 patients of which 9 of them showed coagulase negative staphylococcus. The rest were staphylococcus aureus in five, methicillin-resistant staphylococcus aureus in one and gram negative organisms in five.
The duration between first and second surgery was of about 10 weeks (range: 8-16 weeks). Intraoperative samples taken during the second surgery were negative for organisms and had less than 5 polymorphs per high power field. Out of the 20 patients, 10 underwent cemented hip replacement with gentamicin impregnated cement, 4 with hybrid hip replacements (uncemented acetabular cups and cemented femoral stems) and 6 of them underwent uncemented hip replacements. The decision of implant was taken on basis of age, bone quality, bone loss, and affordability of the patient.
Thorough preoperative planning, appropriate antibiotic therapy, and meticulous attention to surgical detail had resulted in significant functional improvement in these patients. The Harris hip score of the patients had improved considerably from an average of 35.3 preoperatively to 49.6 after the first surgery and to 82.85 after the second definitive surgery at the time of last followup. It was found to be normally distributed by the Kolmogorov Smirnov test and thus analyzed using the paired t-test at 5% significance. A significant difference was found (P < 0.0001) [Figure 3].
Figure 3.
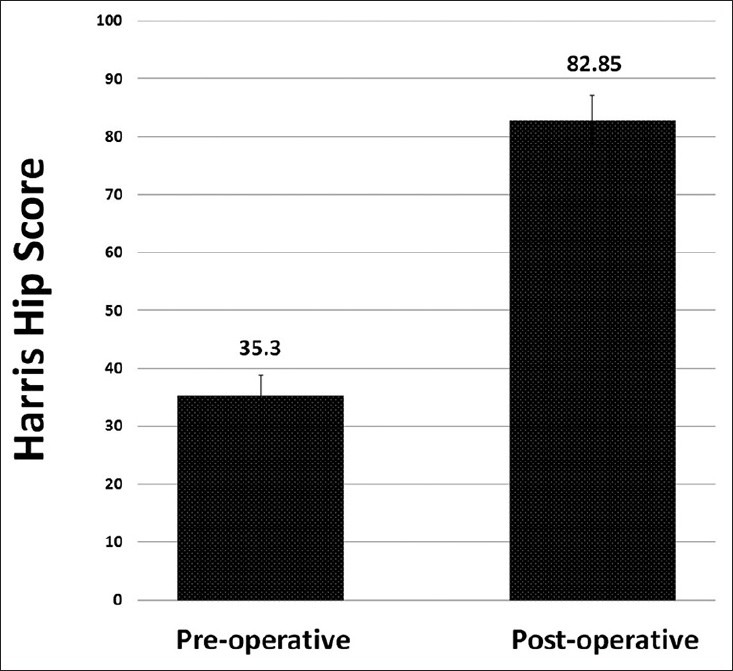
Bar diagram showing preoperative and postoperative Harris hip scores
There was one superficial reinfection, which was treated successfully with local debridement and oral antibiotics. The other patients showed complete healing of discharging sinuses and ESR and CRP levels were normal. There was one intraoperative fracture of the greater trochanter and was treated with tension band wiring. The fracture had completely united in about 8 weeks and the patient was ambulatory without any support or limp at the time of last followup. Sciatic nerve palsy occurred in one patient. It recovered partially one year after second surgey. Four of the patients showed evidence of limb length discrepancy ranging from 3cm shortening in one case, 1 cm shortening in two cases and 1 cm lengthening in one case.
DISCUSSION
The present series has used arthroplasty as an effective treatment for failed and infected implants for hip fractures. The advantage of this study and technique lies in its applicability in a heterogeneous series. Both intertrochanteric and trans-cervical fractures have been included along with osteotomies for hip fractures. While there are many recent studies18–20 on success of THA as a salvage procedure for failed internal fixation of hip, the literature on infected failed fixation is minimal. Pang-Hsin Hseih et al.,1 have described a series of only failed and infected intertrochanteric fracture fixation implants which have been treated with two-stage arthroplasty. Our series deals with all the fractures of the hip joint. Dean et al,21 have described use of Modular Endoprosthetic Tumour System (METS) for eight cases of failed internal fixation of which only two were infected. One was managed by single stage where as the second case required two-stage surgery (spacer of antibiotic-impregnated cement modeled around a guidewire for the first stage). Tzurbakis et al,22 reported a single case of deep wound infection after a trochanteric fracture internal fixation presenting with hip dislocation for which excisional arthroplasty was done as first stage and THA was done 6 weeks later. Our study has a series of 20 patients of failed infected internal fixation of hip.
The approach to such patients is all the more difficult due to the distorted anatomy, inadequate bone stock as well as the severe soft tissue changes encountered.13,14,23 We have endeavored to use the same principles of removal of all infected foreign material, good local concentration of antibiotics by the use of antibiotic impregnated cement and have shown good result with none of our patients showing any evidence of deep infection in recent followups.
There is some controversy regarding whether a single-stage or two-stage revision should be done. There are very few indications for a single-stage surgical procedure like brief duration of symptoms, gram-positive organisms sensitive to antibiotics, a well-fixed implant, and the absence of excessive soft-tissue scarring.24–26 This approach is usually associated with a significant failure rate.1,26,27 Hence, it was followed in just one of our patients who met with all the above-mentioned pre-requisites.
In 15 of 19 patients, we have used custom-made cement spacer for the interim period. This temporary cement spacer accelerates rehabilitation, maintains the patient's mobility, and preserves soft-tissue planes making the re-implantation procedure easier to perform.26,28 Dislocation of the spacer was supposed to be a common complication, with rates ranging from 1.8% to 18% in various studies.1,3,13 However, it was more related to the geometry of the spacer with geometric mismatch being a common cause for the dislocation. In our series, the exact shape and size of the femoral head was re-created by meticulous templating and hence we did not encounter any patient with dislocation of the spacer device. We have used a K-nail or a Rush nail bent at an appropriate angle (130°) coated with cement shaped with a custom-made mold in most of our patients while in others we have used a cement coated Austin Moore's prosthesis or a Charnley's prosthesis. The cement mold was made using an indigenously made, autoclavable template for three different sizes. This provided a cost-effective and easy method that was extremely useful in the present set-up.
The use and duration of antibiotic therapy in the interim period is a matter of considerable debate. McDonald et al,27 in a report on the results of 82 two-stage reconstructions that had been performed for the treatment of infection at the site of a hip arthroplasty, recommended at least 4 weeks of intravenous antibiotic therapy when antibiotic-impregnated material is not used. Nestor et al,29 evaluated 28 patients who had an infection at the site of a hip or knee arthroplasty and demonstrated comparable results between patients who were managed with the implantation of antibiotic-loaded cement beads in conjunction with less than 5 days of parenteral antibiotic therapy and those who were managed with 6 weeks of conventional intravenous antibiotic therapy. In the present series, we have used injectable antibiotics for 3 weeks and oral antibiotics for 3 weeks, which is similar to other studies on peri-prosthetic infection.15,16 Prophylactic antibiotic therapy, taking into consideration recommendations of the hospital infection committee, in the form of third-generation cephalosporin in combination with an aminoglycoside, was given when a definite organism could not be isolated.
The ESR and serum CRP level are not specific measures of infection.30 However, these tests are sensitive, readily available, most useful and prognostically significant when they are monitored serially.24 Hence, the method of using the ESR and serum CRP level to guide the timing of reimplantation is a more practical approach than selecting a fixed interval between procedures because the virulence of the causative pathogen, the severity of infection, and the host response to antimicrobial treatment may vary greatly among individuals.1,23
The patients in the present series have shown a significant improvement in their functional scores with the average Harris hip score being 82.8 postoperatively. This was found to be comparable with primary hip arthroplasty for femoral neck fractures. Narayan et al.,31 have found the average Harris hip score of patients of femoral neck fractures treated with total hip arthroplasty to be 83.8, while Patel et al.,32 have also reported similar results in their group of patients.
The only other series comparable to the present series was that of Pang-Hsin Hseih et al.,1 which has discussed the use of hip arthroplasty in infected intertrochanteric fractures. Similar results were obtained in this series with all the patients having significant improvement in their functional scores. In that series, all patients were treated with two-stage revision with either cement beads or cemented spacer in the interim period.
The strengths of the present study include a relatively high number of consecutive patients of this difficult problem with a high rate of followup. Also this study includes not just intertrochanteric fractures but also trans-cervical fractures and osteotomies for proximal femoral fractures.
The limitations of this study are its retrospective design and a relatively medium term followup. Although there were no deep re-infections in our patients till the last followup, it may still be early to comment on the long term re-infection rate in these patients.
To conclude we found that THA was very effective in restoring function in patients with deep hip sepsis after failed treatment of hip fractures. Complete and radical debridement in the first stage as well as proper antibiotic therapy helped in achieving a desirable outcome. The use of the indigenously prepared cement spacer template was a very inexpensive but effective method in shaping the femoral head component of the spacer device and providing a stable construct between the two surgeries.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Hsieh PH, Chang YH, Chen SH, Shih CH. Staged arthroplasty as salvage procedure for deep hip infection following intertrochanteric fracture. Int Orthop. 2006;30:228–32. doi: 10.1007/s00264-005-0059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Partanen J, Syrjälä H, Vähänikkilä H, Jalovaara P. Impact of deep infection after hip fracture surgery on function and mortality. J Hosp Infect. 2006;62:44–9. doi: 10.1016/j.jhin.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 3.Duncan CP, Beauchamp C. A temporary antibiotic-loaded joint replacement system for management of complex infections involving the hip. Orthop Clin North Am. 1993;24:751–9. [PubMed] [Google Scholar]
- 4.Sharma H, Kakar R. Outcome of Girdlestone's resection arthroplasty following complications of proximal femoral fractures. Acta Orthop Belg. 2006;72:555–9. [PubMed] [Google Scholar]
- 5.Campbell A, Fitzgerald B, Fisher WD, Hamblen DL. Girdlestone pseudarthrosis for failed total hip replacement. J Bone Joint Surg. 1978;60:441–2. [Google Scholar]
- 6.Ahlgren SA, Gudmundsson G, Bartholdsson E. Function after removal of a septic total hip prosthesis. A survey of 27 Girdlestone hips. Acta Orthop Scand. 1980;51:541–5. doi: 10.3109/17453678008990838. [DOI] [PubMed] [Google Scholar]
- 7.Böhler M, Salzer M. Girdlestone's modified resection arthroplasty. Orthopedics. 1991;14:661–6. doi: 10.3928/0147-7447-19910601-06. [DOI] [PubMed] [Google Scholar]
- 8.Castellanos J, Flores X, Llusà M, Chiriboga C, Navarro A. The Girdlestone pseudarthrosis in the treatment of infected hip replacements. Int Orthop. 1998;22:178–81. doi: 10.1007/s002640050236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bittar ES, Petty W. Girdlestone arthroplasty for infected total hip arthroplasty. Clin Orthop. 1982;170:83–7. [PubMed] [Google Scholar]
- 10.Clegg J. The results of the pseudarthrosis after removal of an infected total hip prosthesis. J Bone Joint Surg. 1977;59:298–301. doi: 10.1302/0301-620X.59B3.893508. [DOI] [PubMed] [Google Scholar]
- 11.Esenwein SA, Robert K, Kollig E, Ambacher T, Kutscha-Lissberg F, Muhr G. Long term results after resection arthroplasty according to Girdle- stone for treatment of persisting infections of the hip joint. Chirurg. 2001;72:1336–43. [PubMed] [Google Scholar]
- 12.McElwaine JP, Colville J. Excision arthroplasty for infected total hip replacements. J Bone Joint Surg. 1984;66:168–71. doi: 10.1302/0301-620X.66B2.6707049. [DOI] [PubMed] [Google Scholar]
- 13.Leunig M, Chosa E, Speck M, Ganz R. A cement spacer for two-stage revision of infected implants of the hip joint. Int Orthop. 1998;22:209–14. doi: 10.1007/s002640050244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Younger AS, Duncan CP, Masri BA. Treatment of infection associated with segmental bone loss in the proximal part of the femur in two stages with use of an antibiotic-loaded interval prosthesis. J Bone Joint Surg Am. 1998;80:60–9. doi: 10.2106/00004623-199801000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Fink B. Revision of late periprosthetic infections of total hip endoprostheses: pros and cons of different concepts. Int J Med Sci. 2009;6:287–95. doi: 10.7150/ijms.6.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Younger AS, Duncan CP, Masri BA, McGraw RW. The outcome of two-stage arthroplasty using a custom-made interval spacer to treat the infected hip. J Arthroplasty. 1997;12:615–23. doi: 10.1016/s0883-5403(97)90133-9. [DOI] [PubMed] [Google Scholar]
- 17.Lonner JH, Desai P, Dicesare PE, Steiner G, Zuckerman JD. The reliability of analysis of intraoperative frozen sections for identifying active infection during revision hip or knee arthroplasty. J Bone Joint Surg Am. 1996;78:1553–8. doi: 10.2106/00004623-199610000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Laffosse JM, Molinier F, Tricoire JL, Bonnevialle N, Chiron P, Puget J. Cementless modular hip arthroplasty as a salvage operation for failed internal fixation of trochanteric fractures in elderly patients. Acta Orthop Belg. 2007;73:729–36. [PubMed] [Google Scholar]
- 19.Hammad A, Abdel-Aal A, Said HG, Bakr H. Total hip arthroplasty following failure of dynamic hip screw fixation of fractures of the proximal femur. Acta Orthop Belg. 2008;74:788–92. [PubMed] [Google Scholar]
- 20.D’Arrigo C, Perugia D, Carcangiu A, Monaco E, Speranza A, Ferretti A. Hip arthroplasty for failed treatment of proximal femoral fractures. Int Orthop. 2010;34:939–42. doi: 10.1007/s00264-009-0834-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dean BJ, Matthews JJ, Price A, Stubbs D, Whitwell D, Gibbons CM. Modular endoprosthetic replacement for failed internal fixation of the proximal femur following trauma. Int Orthop. 2012;36:731–4. doi: 10.1007/s00264-011-1332-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tzurbakis M, Morakis E, Mouzopoulos G, Lasanianos N, Ioannis G. Deep wound infection after a trochanteric fracture internal fixation presenting with hip dislocation: A case report. Cases J. 2010;3:19. doi: 10.1186/1757-1626-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res. 1976;117:221–40. [PubMed] [Google Scholar]
- 24.Garvin KL, Hanssen AD. Infection after total hip arthroplasty. Past, present, and future. J Bone Joint Surg Am. 1995;77:1576–88. doi: 10.2106/00004623-199510000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Zilkens KW, Casser HR, Ohnsorge J. Treatment of an old infection in a total hip replacement with an interim spacer prosthesis. Arch Orthop Trauma Surg. 1990;109:94–6. doi: 10.1007/BF00439386. [DOI] [PubMed] [Google Scholar]
- 26.Ivarsson I, Wahlstrom O, Djerf K, Jacobsson SA. Revision of infected hip replacement. Two-stage procedure with a temporary gentamicin spacer. Acta Orthop Scand. 1994;65:7–8. doi: 10.3109/17453679408993707. [DOI] [PubMed] [Google Scholar]
- 27.McDonald DJ, Fitzgerald RH, Jr, Ilstrup DM. Two-stage reconstruction of a total hip arthroplasty because of infection. J Bone Joint Surg Am. 1989;71:828–34. [PubMed] [Google Scholar]
- 28.Hovelius L, Josefsson G. An alternative method for exchange operation of infected arthroplasty. Acta Orthop Scand. 1979;50:93–6. doi: 10.3109/17453677909024096. [DOI] [PubMed] [Google Scholar]
- 29.Nestor BJ, Hanssen AD, Ferrer-Gonzalez R, Fitzgerald RH., Jr The use of porous prostheses in delayed reconstruction of total hip replacements that have failed because of infection. J Bone Joint Surg Am. 1994;76:349–59. doi: 10.2106/00004623-199403000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Berbari E, Mabry T, Tsaras G, Spangehl M, Erwin PJ, Murad MH, et al. Inflammatory blood laboratory levels as markers of prosthetic joint infection: A systematic review and meta-analysis. J Bone Joint Surg Am. 2010;92:2102–9. doi: 10.2106/JBJS.I.01199. [DOI] [PubMed] [Google Scholar]
- 31.Narayan KK, George T. Functional outcome of fracture neck of femur treated with total hip replacement versus bipolar arthroplasty in a South Asian population. Arch Orthop Trauma Surg. 2006;126:545–8. doi: 10.1007/s00402-006-0182-x. [DOI] [PubMed] [Google Scholar]
- 32.Patel KK, Ashford RU, Frasquet-Garcia A, Booth C, Joseph SR, De Boer PG. Muller straight stem total hip arthroplasty for fractured neck of femur. Injury. 2006;37:727–33. doi: 10.1016/j.injury.2005.12.009. [DOI] [PubMed] [Google Scholar]


