Abstract
Background:
Arthroscopic debridement with continuous irrigation system was used with success in treating infective arthritis. We evaluated the effectiveness of arthroscopic debridement coupled with antibiotic continuous irrigation system in acute presentation of late infected total knee arthroplasty.
Materials and Methods:
We performed a retrospective review of medical record of patients with acute presentation of late infected total knee arthroplasty who were treated by arthroscopic debridement coupled with continuous postoperative antibiotic irrigation system.
Results:
Seventeen patients were included in our study. 15 (88%) patients preserved their total knee prosthesis at mean of followup of 27.5 months (range, 14-28 months). Two (12%) patients failed arthroscopic protocol and finally needed two stages revision. Our study showed an 88% prosthesis retention rate in patients with acute presentation of late prosthetic knee infection. No complication was associated with use of antibiotic irrigation system.
Conclusion:
Arthroscopic debridement combined with continuous antibiotic irrigation and suction is an effective treatment for patients with acute presentation of late infected total knee arthroplasty.
Keywords: Arthroscopic debridement, infected total knee arthroplasty, irrigation
INTRODUCTION
Infection is the most disastrous complication of total knee arthroplasty (TKA) with reported rate of 1-5% in early studies,1–3 although this rate has declined to 0.5-1% in recent studies.2,4–6 The options for treatment of an infection of the prosthesis includes two stage reimplantation, exchange arthroplasty, or open debridement with prosthesis retention.7–11 Two stage reimplantation is 97% successful, although it involves significant morbidity and can cause extensor weakness and rupture.11 Open debridement with component retention is a reasonable alternative to a two stage revision. However, the results of open debridement with component retention vary widely: The success rate is 29-83%.9,11 The success of open debridement with component retention depends on the duration of symptoms, onset of treatment, and virulence of the organisms.12,13 Arthroscopic debridement for septic knee appears to be an attractive alternative to the two methods mentioned above because of its low morbidity and faster recovery.14
Flood et al. first reported two cases of infected total knee arthroplasty treated by arthroscopic irrigation and debridement and component retention.15 A larger series by Waldman et al. reported a low rate of successful infection elimination and component retention (38%).14 Although the treatment results of arthroscopic debridement and component retention are variable, faster recovery and minimal disruption to the extensor mechanisms make it an attractive alternative. Our hypothesis is that continuous irrigation with high dose vancomycin increases the success rate of infection eradication when used with arthroscopic debridement in strictly selected patients. We performed a retrospective review of the patients of acute presentation of late infection following total knee arthroplasty and were treated with arthroscopic debridement with continuous high-dose vancomycin irrigation postoperatively.
MATERIALS AND METHODS
The patients who developed infection following TKA, treated by three senior surgeons from 2000 to 2008 were retrospectively reviewed.
The inclusion criteria were patients with (1) primary total knee arthroplasty, (2) the absence of radiographic evidence of prosthetic loosening, (3) athroscopic surgery performed within 7 days after the onset of symptoms of infection, (4) deep infection of the prosthesis identified by initial aspiration and bacterial culture, and (5) who completed the outpatient followup for at least one year after debridement. We excluded patients with immune compromised conditions such as diabetes and steroid use.
Diagnosis of septic arthritis was suspected based on the patient's symptoms, including pain, effusion, swelling, and fever, and was confirmed by aspiration and culture. Seventeen patients who met the above criteria were included in the study. All patients received empirical antibiotic treatment (vancomycin) after the initial aspiration and culture sensitivity, and the use of the antibiotic was adjusted by an infection specialist according to the culture results and sensitivity test. Patients received arthroscopic treatment as soon as possible after admission.
Operative procedure
Arthroscopic debridement was performed through anteromedial, anterolateral, and superolateral portals; the superomedial portal was sometimes added to maximize visualization. The synovectomy was performed as completely as possible in the suprapatellar pouch, lateral and medial gutters, intercondylar notch, and infrapatellar fat pad. A high speed, motorized shaver was used to perform the debridement of fibrous debris, necrotic synovium, loose fragments, or loculated pockets of adhesive compartments. We restricted use of electrocauterization and thermal shrinkage to limit thermal damage and necrotic debris in the joint.
During the procedure, the joint was irrigated with at least 12 litres of normal saline. Following debridement, a closed continuous irrigation–suction system was established. The inflow tube was established using a Hemovac drainage tube (size 1/4 inch or 6.4 mm) through a lateral thigh entering into the suprapatellar pouch. Outflow was established on the inferomedial aspect of the knee using a chest tube (24 FG). The tubes were fixed with suture stitches. The outflow chest drainage tube was connected to a Gomco suction machine [Figure 1] set at intermittent (time on: time off, 60:15 s) and vacuum suction (150 mmHg) to allow distention and suction. The amounts of inflow and outflow of the closed circuit system were monitored carefully. The inflow saline amount was 12 litres per day on average. Normal saline solution was used in the irrigation-suction system. Vancomycin at a dose of 500 mg in 2 liter of normal saline was used in the irrigation-suction systems for 2 days. The inflow tube was removed on the third postoperative day, and the outflow tube was retained for 2 more days to monitor joint effusion. If the joint effusion was less than 50 ml per day and the color normalized, the tube was removed.
Figure 1.
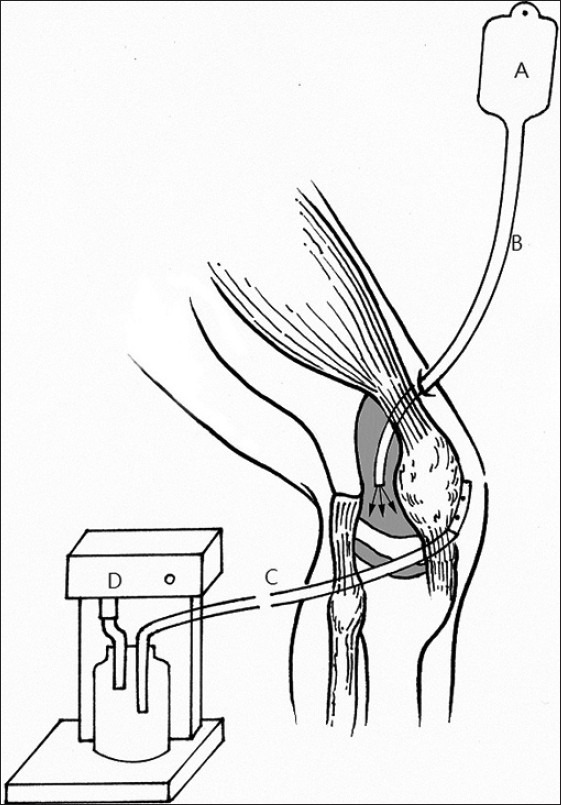
Line diagramme showing continuous antibiotic irrigation–suction system of the knee joint. Antibiotics in Normal saline (a) is hung above and fed into the joint by gravity inflow with ¼” Hemovac drainage tube. (b) At the same time, 24FG chest tube is positioned from the standard anterolateral portal. (c) A Gomco suction machine. (d) provides intermittent vacuum suction
Our decision to repeat the debridement was based on clinical and laboratory results. We reevaluated each patient on the fifth day after the index procedure. If the knee appeared hot, red, and swollen, and if the C-reactive protein (CRP) level remained constant or decreased slightly, we performed one repeat operation. If the drainage amount and color failed to normalize after the second debridement, the result was counted as a failure and open debridement ensued.
The decision to use antibiotic therapy was based on the suggestion by the infectious disease specialist according to the final microbiology culture and sensitivity report. Intravenous antibiotics were continued for 6 weeks and were changed to oral antibiotics as the CRP level normalized and the clinical symptoms improved.
Full functional rehabilitation was started immediately after removal of the drains. The initial physical therapy program comprised continuous passive motion (CPM) exercises within pain limits, followed by a knee strengthening program. Partial weight bearing with crutches support was allowed in the involved extremity. The followup included clinical examination, CRP and radiographic imaging every month for 3 months and then every 3 months. Successful treatment was defined as no clinical symptoms and the level of CRP <0.5 mg/dL at every outpatient followup. The Knee Society scoring was performed at least 1 year after the indexed arthroscopic protocol.15 The clinical examination for symptoms of infection such as redness, heat, and swelling and radiographic interpretation for prosthesis loosening were performed by the senior authors.
RESULTS
Seventeen patients were included in the study [Table 1]. No patient was lost to followup in an average 27.5 months followup (range 14-38 months). Except for infection in the patient (number 17) who was diagnosed with an early deep postoperative infection, the infections in the rest of the patients were classified as the late hematogenous type.16 The surgeries were performed on average 4 days after onset of symptoms (average 42.2 months, range 8-71 months after initial TKA). Five of 17 patients (29%) underwent second arthroscopic debridement because of sustained heat and bloody, turbid reddish drainage color after 2 days of continuous irrigation The procedure was considered a failure in two of five (40%) patients who underwent repeated arthroscopic debridement because of persistent knee swelling and a high CRP level (>0.5 mg/dL).
Table 1.
Clinical details of patients with acute presentation of late infection following total knee arthroplasty (TKA)
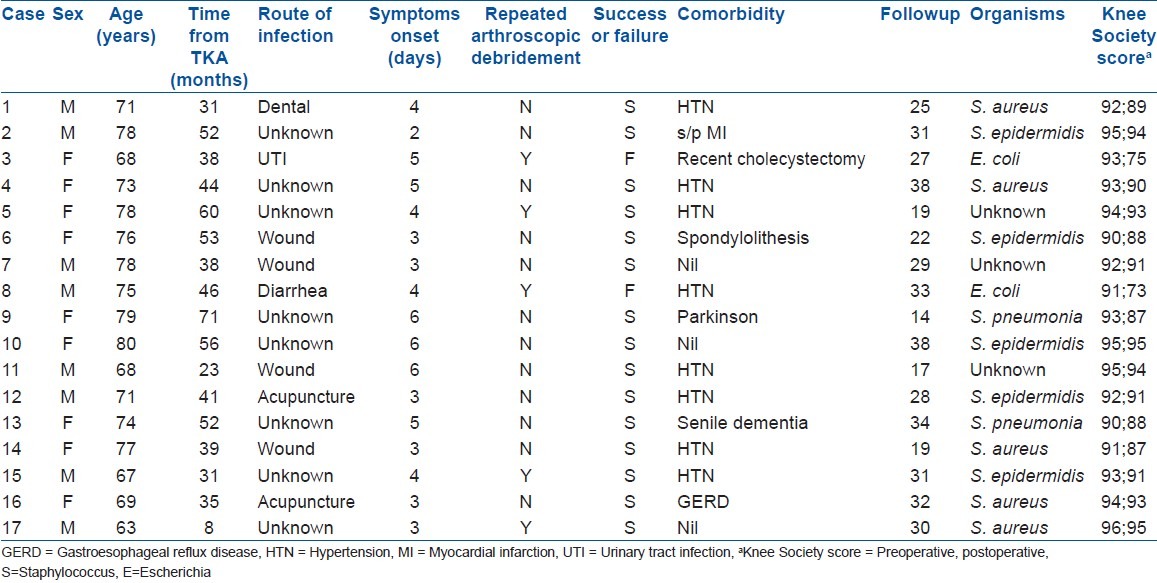
Ten of 17 patients were staphylococcal infection and five of them were oxacillin resistant. The rest of the 7 patients developed streptococcal infection (n = 2), Escherichia coli infection (n = 2), and infection of unknown pathogen (n = 3). The procedures considered a failure after two arthroscopic debridements were in two patients with Escherichia coli infection. They were treated with open debridement. These two patients finally received a two-stage revision total knee arthroplasty after component removal.
Overall infection could be controlled in 15 patients thus the success rate of infection eradication was 88%. The postoperative Knee Society score was worse in patients whose arthroscopic protocol failed and who underwent the two-stage revision (preoperative average: 92; postoperative average: 74) compared with the patients who underwent a successful arthroscopic protocol (preoperative average: 93; postoperative average: 89; P < 0.02). The data is too less for statistical analysis.
DISCUSSION
The treatment of infected TKA usually involves removing the prosthesis and reimplanting a new one. A two stage revision is the gold standard in the treatment of an infected total knee prosthesis, although an infection eradication rate of 97% was reported by Windsor et al.17 The two stage reimplantation method is a long and costly procedure that requires removal of the components, replacement with antibiotic eluting cement, and reimplantation of the prosthesis after 6 weeks of intravenous antibiotic therapy. Complications such as extensor lag11 and late rupture of the extensor18 mechanisms have been reported. Loss of bone stock is also an important issue after component removal.
Component retention with open debridement has an 83% infection eradication rate.9 Open debridement and component retention has the advantage of preservation of bone stock while providing thorough synovectomy and component cleansing, especially of the polyethylene insert.9 Component retention with arthroscopic debridement is another reasonable alternative for treating total knee prosthesis infection. After arthroscopic procedures, patients return to full function sooner. If the arthroscopic procedure finally fails, a two-stage revision total knee arthroplasty may still be required.
Waldman et al. (n = 16) reported a 38% overall success rate in eradication after arthroscopic debridement of infection,14 a rate that is less than their previously reported 83% success rate for open debridement procedures. They concluded that the inferior outcomes of arthroscopic debridement reflect inadequate synovectomy and incomplete debridement of the prosthetic knee including the posterior aspect of the knee joint, polyethylene insert, and bone cement interfaces. Ilahi et al. reported five cases of infected total knee prosthesis treated with an arthroscopic procedure19; the infection was eradicated in all five patients after arthroscopic debridement and intravenous antibiotics treatment. They concluded that strict patient selection (less than 7 days after symptom onset and no immune-compromised patients), a radiologically stable prosthesis, and profuse irrigation with intraoperative saline containing antibiotics were crucial for success in their arthroscopic treatment. However, the case number was very small in their study.
Our study used similar inclusion criteria as those used in previous studies,14,15,19 and we used a multiportal arthroscopic approach to perform a adequate subtotal synovectomy. We performed arthroscopic debridement through up to four portals (anterolateral, anteromedial, superolateral, superomedial). The synovectomy was performed as thoroughly as possible. We found that performing the arthroscopic procedure under the reflexive prosthesis surface was difficult in the beginning, but by exchanging viewing portals and working portals, we found that synovectomy can still be performed completely except for the posterior aspect of the knee. In arthroscopic debridement of a total knee infection, dead space lies under the space between the polyethylene insert and tibial component. The area comprises an avascular area, which lacks self-defense immune mechanisms and is inaccessible to the arthroscope.14,15,19 We believe that our procedure solves these problems with continuous irrigation with normal saline and antibiotics.
Continuous antibiotics irrigation after arthroscopic debridement has not been reported in the treatment of total knee prosthetics infection. However, several studies have investigated the treatment of infective arthritis of the knee. Jackson reported good results using a distension–irrigation technique in a small number of patients with infective arthritis of the knee.20 Continuous irrigation has also been reported to improve the outcome of arthroscopic debridement in infective arthritis of the knee.21 The continuous closed irrigation–suction system with a persistent irrigation circuit of the knee joint has the following theoretical advantages: (a) dilutes the enzymatically active material, (b) dilutes concentration of the causative microorganism and increases the efficiency of systemic antibiotics; and removes the necrotic material.21 The supplement of antibiotics in our method (vancomycin 250 μg/ml) for 2 days provides a high local concentration, which is more than 50 times the serum trough level under intravenous vancomycin treatment. This method gives a stable supply of vancomycin at a bactericidal concentration, which may help eliminate bacteria in avascular areas that are inaccessible to arthroscopic debridement.
We used vancomycin as an empirical antibiotic for intraarticular irrigation in all patients before the culture and sensitivity report was available to us. Intraarticular antibiotic irrigation usually stopped before the culture and sensitivity reports were known. In two of our patients, the final arthroscopic protocol was considered a failure. Patients number 3 and 8 were found to be infected with E. coli species. These two patients required a two-stage revision and intravenous third-generation cephalosporin treatment. The failure was caused partly by the insensitivity of possible Gram-negative bacteria species to the initial vancomycin treatment. These results made us reconsider the use of broad spectrum antibiotics as an empirical treatment before the culture results are known.
Antibiotic concentration many times higher than the minimal bactericidal concentration can be achieved through prolonged direct antibiotic irrigation. The method gives a more constant supply of antibiotics, unlike in antibiotic cement implantation, in which the concentration decreases rapidly after the first 24 h.3,22–25
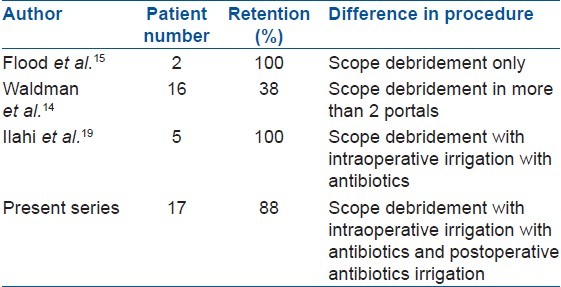
The weaknesses of our study are that it was a retrospective case series and no control group was established for comparison. However, we have compared our infection eradication results with those of previous studies [Table 2]. Further the sample size is too small to give statistically significant results. The results show that intraoperative irrigation with antibiotics improves the success rate markedly. We extended the bactericidal treatment in the postoperative period through direct high dose vancomycin irrigation, which further decreased the formation of a biofilm of the remaining bacteria and possibly decreased the formation of a resistant bacterial strain.25 Our continuous antibiotic irrigation-suction system may be added as an adjunct treatment in postoperative arthroscopic debridement to improve the success rate of infective elimination.
Table 2.
Summary of previous literature about athroscopic debribement
To conclude the arthroscopic debridement combined with continuous antibiotic irrigation and suction can be an alternative treatment for patients with early diagnosed knee prosthesis infection. This treatment provides the patient with better postoperative knee function and fewer postoperative comorbidities such as extensor dysfunction.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Kettlekamp DB. Infected total knee replacement (editorial) Arch Surg. 1977;112:552–3. doi: 10.1001/archsurg.1977.01370050012002. [DOI] [PubMed] [Google Scholar]
- 2.Wilson MG, Kelley K, Thornhill TS. Infection as a complication of total knee-replacement arthroplasty. Risk factors and treatment in sixty-seven cases. J Bone Joint Surg Am. 1990;72:878–83. [PubMed] [Google Scholar]
- 3.Anguita-Alonso P, Rouse MS, Piper KE, Jacofsky DJ, Osmon DR, Patel R. Comparative study of antimicrobial release kinetics from polymethylmethacrylate. Clin Orthop Relat Res. 2006;445:239–44. doi: 10.1097/01.blo.0000201167.90313.40. [DOI] [PubMed] [Google Scholar]
- 4.Jamsen E, Huhtala H, Puolakka T, Moilanen T. Risk factors for infection after knee arthroplasty. A register-based analysis of 43, 149 cases. J Bone Joint Surg Am. 2009;91:38–47. doi: 10.2106/JBJS.G.01686. [DOI] [PubMed] [Google Scholar]
- 5.McCleery MA, Leach WJ, Norwood T. Rates of infection and revision in patients with renal disease undergoing total knee replacement in Scotland. J Bone Joint Surg Br. 2010;92:1535–9. doi: 10.1302/0301-620X.92B11.23870. [DOI] [PubMed] [Google Scholar]
- 6.Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ. The incidence of deep prosthetic infections in a specialist orthopaedic hospital: A 15-year prospective survey. J Bone Joint Surg Br. 2006;88:943–8. doi: 10.1302/0301-620X.88B7.17150. [DOI] [PubMed] [Google Scholar]
- 7.Estes CS, Beauchamp CP, Clarke HD, Spangehl MJ. A two-stage retention debridement protocol for acute periprosthetic joint infections. Clin Orthop Res. 2010;468:2029–38. doi: 10.1007/s11999-010-1293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Insall JN, Thompson F, Brause BD. Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am. 1983;65:1078–98. [PubMed] [Google Scholar]
- 9.Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty A two-stage retention debridement protocol for acute periprosthetic joint infections. J Arthroplasty. 1997;12:426–33. doi: 10.1016/s0883-5403(97)90199-6. [DOI] [PubMed] [Google Scholar]
- 10.Morrey BF, Westholm F, Schoifet S, Rand JA, Bryan RS. Long term results of various treatment options for infected total knee arthroplasty. Clin Ortho Res. 1989;248:120–8. [PubMed] [Google Scholar]
- 11.Rand JA. Alternatives to reimplantation for salvage of the total knee arthroplasty complicated by infection. J Bone Joint Surg Am. 1993;75:282–9. doi: 10.2106/00004623-199302000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Deirmengian C, Greenbaum J, Stern J, Braffman M, Lotke PA, Booth RE, Jr, et al. Open debridement of acute gram-positive infections after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:129–34. doi: 10.1097/01.blo.0000092996.90435.35. [DOI] [PubMed] [Google Scholar]
- 13.Choi HR, von Knoch F, Zurakowski D, Nelson SB, Malchau H. Can implant retention be recommended for treatment of infected TKA? Clin Orthop Relat Res. 2011;469:961–9. doi: 10.1007/s11999-010-1679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waldman BJ, Hostin E, Mont MA, Hungerford DS. Infected total knee arthroplasty treated by arthroscopic irrigation and debridement. J Arthroplasty. 2000;15:430–6. doi: 10.1054/arth.2000.4637. [DOI] [PubMed] [Google Scholar]
- 15.Flood JN, Kolarik DB. Arthroscopic irrigation and debridement of infected total knee arthroplasty: Report of two cases. Arthroscopy. 1988;4:182–6. doi: 10.1016/s0749-8063(88)80024-0. [DOI] [PubMed] [Google Scholar]
- 16.Kim YH, Choi Y, Kim JS. Treatment based on the type of infected TKA improves infection control. Clin Orthop Relat Res. 2011;469:977–84. doi: 10.1007/s11999-010-1425-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Windsor RE, Insall JN, Urs WK, Miller DV, Brause BD. Two-stage reimplantation for the salvage of total knee arthroplasty complicated by infection. Further followup and refinement of indications. J Bone Joint Surg Am. 1990;72:272–8. [PubMed] [Google Scholar]
- 18.Rand JA, Bryan RS. Reimplantation for the salvage of an infected total knee arthroplasty. J Bone Joint Surg Am. 1983;65:1081–6. [PubMed] [Google Scholar]
- 19.Ilahi OA, Al-Habbal GA, Bocell JR, Tullos HS, Huo MH. Arthroscopic debridement of acute periprosthetic septic arthritis of the knee. Arthroscopy. 2005;21:303–6. doi: 10.1016/j.arthro.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Jackson RW, Parsons CJ. Distension-irrigation treatment of major joint sepsis. Clin Orthop Relat Res. 1973;96:160–4. [PubMed] [Google Scholar]
- 21.Kuo CL, Chang JH, Wu CC, Shen PH, Wang CC, Lin LC, et al. Treatment of septic knee arthritis: Comparison of arthroscopic debridement alone or combined with continuous closed irrigation-suction system. J Trauma. 2010;71:454–9. doi: 10.1097/TA.0b013e3181ec4734. [DOI] [PubMed] [Google Scholar]
- 22.McLaren Rl, McLaren AC, Vernon BL. Generic tobramycin elutes from bone cement faster than proprietary tobramycin. Clin Orthop Relat Res. 2008;466:1372–6. doi: 10.1007/s11999-008-0199-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salvati EA, Callaghan JJ, Brause BD, Klein RF, Small RD. Reimplantation in infection. Elution of gentamicin from cement and beads. Clin Orthop Relat Res. 1986;207:83–93. [PubMed] [Google Scholar]
- 24.van de Belt H, Neut D, Schenk W, van Horn JR, van der Mei HC, Busscher HJ. Gentamicin release from polymethylmethacrylate bone cements and Staphylococcus aureus biofilm formation. Acta Orthop Scand. 2000;71:625–9. doi: 10.1080/000164700317362280. [DOI] [PubMed] [Google Scholar]
- 25.Whiteside LA, Peppers M, Nayfeh TA, Roy ME. Methicillin-resistant Staphylococcus aureus in TKA treated with revision and direct intraarticular antibiotic infusion. Clin Orthop Relat Res. 2011;469:26–33. doi: 10.1007/s11999-010-1313-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


