Abstract
Objectives
To investigate the association between psychological distress and obesity among law enforcement officers (LEOs) in the United States.
Methods
Self-reported data on psychological distress based on six key questions were obtained from LEOs who participated in the National Health Interview Survey (2004-2010). We used Prochaska's cut-point of a Kessler 6 score ≥ 5 for moderate/high mental distress in our analysis. Mean levels of body mass index (BMI) were compared across three levels of psychological distress.
Results
The average age of LEOs (n = 929) was 39.3 years; 25% were female. Overall, 8.1% of LEOs had moderate or high psychological distress; 37.5% were obese (BMI ≥ 30). Mean BMI increased with increasing psychological distress (no distress, BMI = 27.2 kg/m2; mild distress, 27.6 kg/m2; and moderate/high distress, 33.1 kg/m2; p = 0.016) after adjustment for age, race, income, and education level among female officers only. Physical activity modified the association between psychological distress and BMI but only among male LEOs (interaction p = 0.002). Among male LEOs reporting low physical activity, psychological distress was positively associated with BMI (30.3 kg/m2 for no distress, 30.7 for mild distress, 31.8 for moderate/high distress; p = 0.179) after adjustment, but not significantly. This association was not significant among males reporting high physical activity.
Conclusion
Mean BMI significantly increased as psychological distress increased among female LEOs. A longitudinal study design may reveal the directionality of this association as well as the potential role that physical activity might play in this association.
Keywords: Psychological distress, Law enforcement officers, Adiposity
Introduction
The law enforcement profession is a highly stressful occupation. Law enforcement officers (LEOs) include police officers, detectives and criminal investigators, correctional officers, bailiffs, fish and game wardens, and parking enforcement workers. Police officers are required to be constantly on alert because they are likely to experience unexpected situations at any moment such as confrontation by criminals. In addition, they commonly work overtime and various shift schedules, and they experience administrative and organizational pressure and demands. These stressors could adversely affect their health and their lifestyle resulting in conditions such as posttraumatic stress disorder (PTSD) [1,2], metabolic syndrome [3], cardiovascular disease [4], and alcoholism and anxiety [5]. Collins and Gibbs [6] reported that police organizational culture and workload were the key issues in officer stress in one county police force. A study on police officers in the United Kingdom showed that the prevalence of PTSD in officers was six or more times the prevalence for the community [7].
Protective service workers, police officers and firefighters, had the second highest obesity prevalence (29.8%) among 41 occupational categories, and the annual change in obesity prevalence (2.1% ± 0.8) was two times higher than that for the United States population (0.95% ± 0.11) in the period from 1997 to 2002 [8]. A recent study showed that, in an urban police population, the prevalence of obesity for male officers was 47.4%, while for female officers it was only 16.0% [9]. Obesity has been shown to be associated with certain chronic diseases and injuries (e.g., cardiovascular disease, musculoskeletal disorders, vibration-induced injury, and sleep-disorders) and with occupational safety [10].
Several studies have reported that psychological distress is associated with obesity. Psychological distress elevated body mass index (BMI) [11,12] and central obesity [13]. Many studies have reported the positive relationship between job stress and obesity in workers [13-16]. Other studies have found that stress from family concerns correlated with depression and obesity [17,18]. Very few studies have examined the association between psychological distress and obesity in law enforcement workers or military personnel. In a study conducted among Afghanistan and Iraq War veterans, Barber and colleagues [19] found that PTSD and depression were not associated with increased weight. Another study showed that depressive symptoms were associated with the metabolic syndrome among police officers [9].
Psychological factors like depression, anxiety, fatigue, and psychological trauma might be risk factors for obesity. The objective of this paper is to investigate the association between psychological distress and obesity among a cross-section of LEOs who responded over a seven-year period in the United States.
Materials and Methods
Source of data
The National Health Interview Survey (NHIS), developed and administered by National Center for Health Statistics in the Centers for Disease Control and Prevention, is a nationwide survey on the health of the civilian non-institutionalized United States population [20]. The NHIS is a nationally representative in-person household interview conducted annually and based on a multi-stage clustered area probability sample. Individuals who belong to minority racial/ethnic backgrounds (e.g., Blacks, Hispanics, and Asians) and adults aged ≥ 65 years are oversampled to allow for the precise estimation of health in minority populations and elders. Data from the NHIS core questionnaires (Sample Adults, Family, Household) in 2004-2010 were analyzed for this study. Data prior to 2004 were not included since a specific occupation, law enforcement workers, was not available. Merging NHIS data files to Sample Adults file and combining NHIS data across years were performed using the NHIS guidelines: Variance Estimation and Other Analytic Issues, NHIS 1995-2005; Variance Estimation and Other Analytic Issues, NHIS 2006-2010. The total initial sample size from the Sample Adults survey (aged 18 years or older) in 2004-2010 was 187,091, with an average response rate of 79.5%. The final sample size used in our analyses was 105,862 working adults, after removing those who were not employed during the last week of the interview (n = 75,166) and those who were pregnant or missing any of the psychological distress and BMI variables (n = 6,063). This study focused on LEOs (n = 929) among the United States working adults (n = 105,862).
Outcome variable: BMI
In the Sample Adults questionnaire, participants were asked their height in inches ("How tall are you without shoes?") and their weight in pounds ("How much do you weigh without shoes?"). BMI was used to assess obesity, and was calculated as weight in kilograms divided by height in meters squared. We used BMI as both a continuous variable and a categorical variable (BMI < 25 kg/m2 for underweight/normal, 25 to < 30 kg/m2 for overweight, and ≥ 30 kg/m2 for obese).
Exposure variable: psychological distress
There were six psychological distress questions for assessing the presence of a possible mental health condition that were designed for the United States NHIS, which are referred to as Kessler 6 (K6) [21]. The standard K6 has the following six questions: "During the past 30 days, how often did you feel 1) so sad that nothing could cheer you up? 2) nervous? 3) restless or fidgety? 4) hopeless? 5) that everything was an effort? 6) worthless?" Response categories are "All of the time" (score = 4), "Most of the time" (score = 3), "Some of the time" (score = 2), "A little of the time" (score = 1), and "None of the time" (score = 0). The total psychological distress score was the sum of the six items with a range of 0-24. Since the number of participants in the serious psychological distress category (K6 ≥ 13) for the LEOs was very small, we used Prochaska's cut-point of K6 ≥ 5 as moderate/high mental distress in our analyses [22].
Covariates
The NHIS Sample Adult module collected socio-demographic information including age (≥ 18 years), gender, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic all other race groups), marital status (single/never married, married, separated/divorced/widowed), highest level of education completed (from never attended/kindergarten to doctoral degree), income earned last year (11 levels from USD 0 to USD 75,000 or more), having more than one job (yes, no), and number of years in the law enforcement profession. Lifestyle information included smoking status (never, former, current), alcohol status (never/former, current [≤ 3 drinks/week], current [> 3 drinks/week]), hours of sleep per day, and leisure-time physical activity (hours per week). To assess leisure-time physical activity, participants were asked to summarize their usual physical activity both in terms of frequency and duration while engaging in aerobic physical activity or muscle-strengthening activity. Hours of leisure-time physical activity per week was calculated based on the frequency and duration. The term "physical activity" in our study refers to leisure-time physical activity. After we assessed effect modification by physical activity and found that it was significant, we examined the association between psychological distress and obesity while stratifying on physical activity which was dichotomized at the median.
Statistical analysis
In order to more accurately represent the population of the United States, all analyses were performed using a weighting variable, which was divided by seven to take into consideration the seven survey years 2004-2010. Statistical comparisons of cross-tabulated prevalence and mean estimates were analyzed using chi-square tests or the Student's t-tests, respectively. We also investigated whether characteristics of the LEOs varied by survey year. After performing bivariate analysis, regression analyses were used to determine if psychological distress was associated with obesity. We assessed effect modification by gender due to the fact that women and men may process psychological distress in different ways and also tend to have different levels of BMI. We also assessed effect modification by physical activity because physical activity may influence both psychological distress and obesity. Since age, race, annual income, and education level were strongly associated with both psychological distress and BMI, we included them in the multivariate analysis as confounders. We also included age as confounder because it has been strongly related to psychological distress and BMI in previous studies [23,24]. All data that we used met the standard of statistical reliability, i.e., relative standard error (standard error/mean) < 30% which is found in the guidelines of the National Center for Health Statistics [25]. To attain unbiased estimates from the NHIS data, all analyses were weighted to account for the complex survey design and survey non-response using the SAS-callable SUDAAN 10.0 software (Research Triangle Institute, Research Triangle Park, NC, USA) with Taylor series linearization methods for NHIS variance estimation. The cut point for statistical significance was p < 0.05.
Results
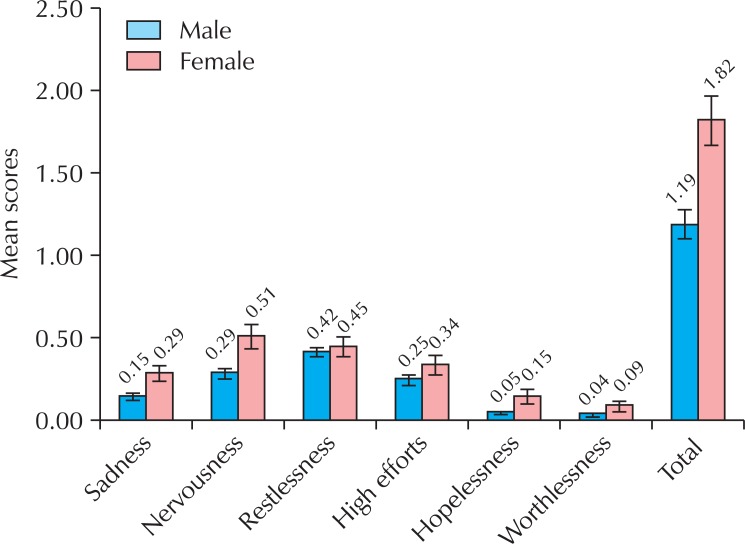
Table 1 shows descriptive statistics for demographics and other selected characteristics for LEOs and the United States workers. The average age of all LEOs (n = 929) was 39.3 years. The prevalence of current smoking was higher (though not statistically significant) in women than in men (20.4% vs. 13.5%). As expected, male and female LEOs differed with respect to BMI (p < 0.001). For example, the prevalence of being overweight (25 ≤ BMI < 30 kg/m2) or obese (BMI ≥ 30) was significantly higher among male LEOs than among female LEOs (83.9% vs. 71.7%), however, male officers spent more time in physical activity compared to female officers (5.1 hours/week vs. 3.6 hours/week; p < 0.001). The mean total psychological distress score among all LEOs was 1.32. Female LEOs had significantly higher mean levels of psychological distress score than male LEOs (1.82 vs. 1.19; p = 0.020). The score for "restlessness" was highest among the male LEOs, followed by "nervousness" and "high effort" (Fig. 1). Among female LEOs, "nervousness" had the highest score. The mean level of "nervousness" was almost twice as high in female compared with male LEOs, and female LEOs also reported higher scores for "sadness", "hopelessness", and "worthlessness" than the male LEOs.
Table 1.
Descriptive statistics for demographic and other characteristics of law enforcement officers by gender; NHIS (2004-2010)
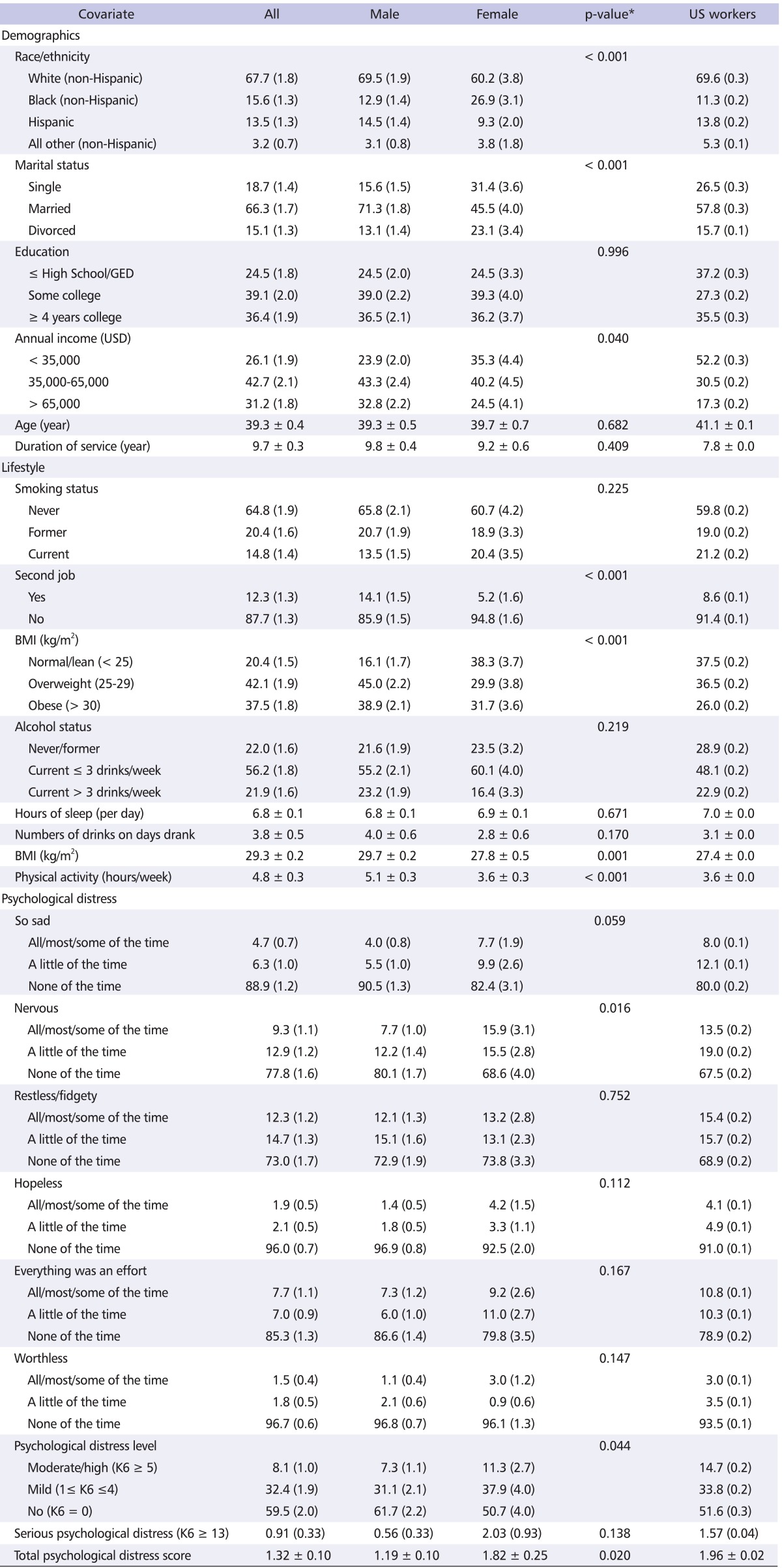
Values are presented as percentage (standard error) or mean ± standard error.
Sample number/estimated population: all, 929/1,180,440; male, 698/950,237; female, 231/237,203; US workers, 105,862/131,822,554.
*p-values are for differences between women and men from Student's t-tests or χ2 tests for independence.
NHIS: National Health Interview Survey, GED: General Educational Development Test, BMI: body mass index; K6: Kessler 6.
Fig. 1.
Mean psychological distress scores in law enforcement officers by gender. "I" bar indicates the standard error.
The association between selected characteristics and psychological distress is presented in Table 2. There was a slightly higher prevalence of officers with less education in the highest distress category. Similarly, a larger proportion of officers in the moderate and high distress group had low annual income (< USD 35,000) than for those in the mild and no distress categories. Officers with high distress reported a significantly lower mean sleep duration compared to those with mild and no distress (6.5 hours/week, 6.8 hours/week, 6.9 hours/week respectively; p = 0.003).
Table 2.
Associations between psychological distress and selected characteristics in law enforcement officers: NHIS (2004-2010)
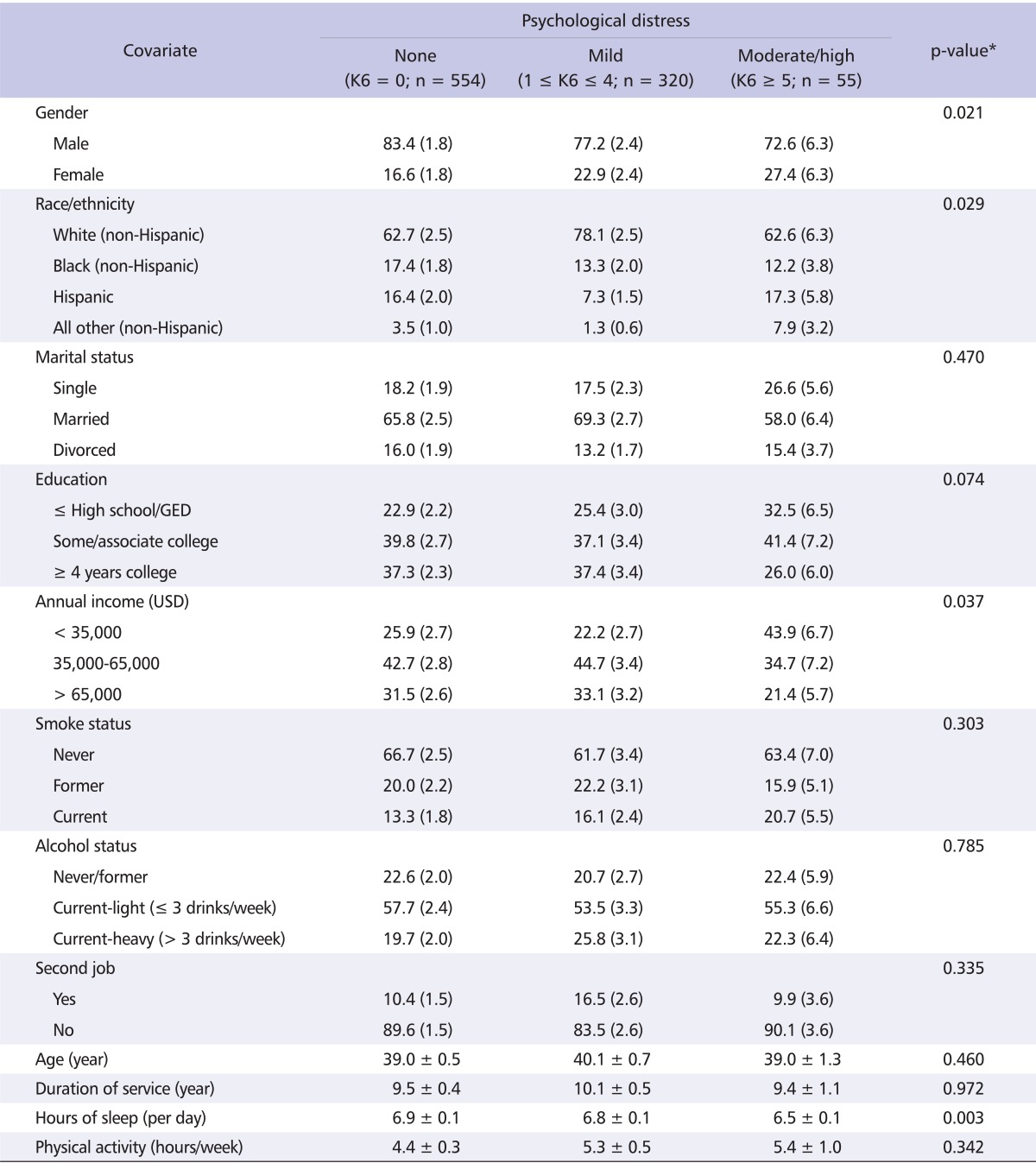
Values are presented as percentage (standard error) or mean ± standard error.
NHIS: National Health Interview Survey, K6: Kessler 6, GED: General Educational Development Test.
*For nominal variables (gender, race, marital status, smoke status, alcohol status, second job), the p-values were obtained from Cochran-Mantel-Haenszel analysis of variance-type test (SUDAAN 10 Example Manual, 2008). For continuous or ordinal variables (age, education, income, years of service, sleep duration, physical activity), the p-values were obtained from linear association.
Table 3 shows the association between psychological distress and BMI, stratified by gender. Among female officers, mean BMI increased significantly with increasing psychological distress (no distress, BMI = 27.2 kg/m2; mild distress, 27.6 kg/m2; and moderate/high distress, 33.1 kg/m2; p = 0.016) after adjustment for age, race, annual income, and education level. There was no association between psychological distress and BMI among male officers. Survey year was not shown to be a confounder so it was excluded from the final models of Tables 3, 4.
Table 3.
Mean BMI by psychological distress and gender; NHIS (2004-2010)
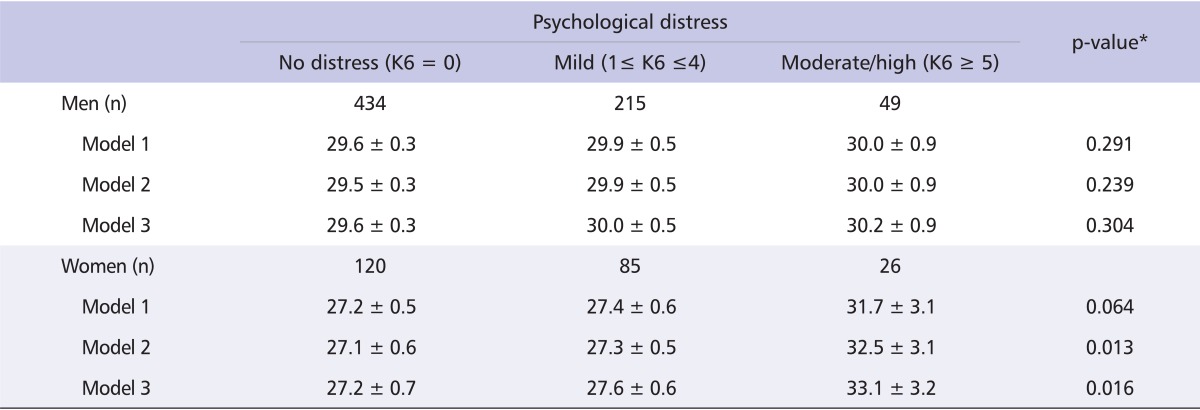
Values are presented as mean ± standard error.
Model 1: unadjusted; Model 2: adjusted for age, race/ethnicity; Model 3: adjusted for age, race/ethnicity, annual income, and education.
*The p-values are from linear regression.
Interaction p-value = 0.192 for psychological distress*gender.
BMI: body mass index, NHIS: National Health Interview Survey, K6: Kessler 6.
Table 4.
Unadjusted and adjusted mean BMI across psychological distress categories stratified by physical activity among male law enforcement officers, NHIS (2004-2010)
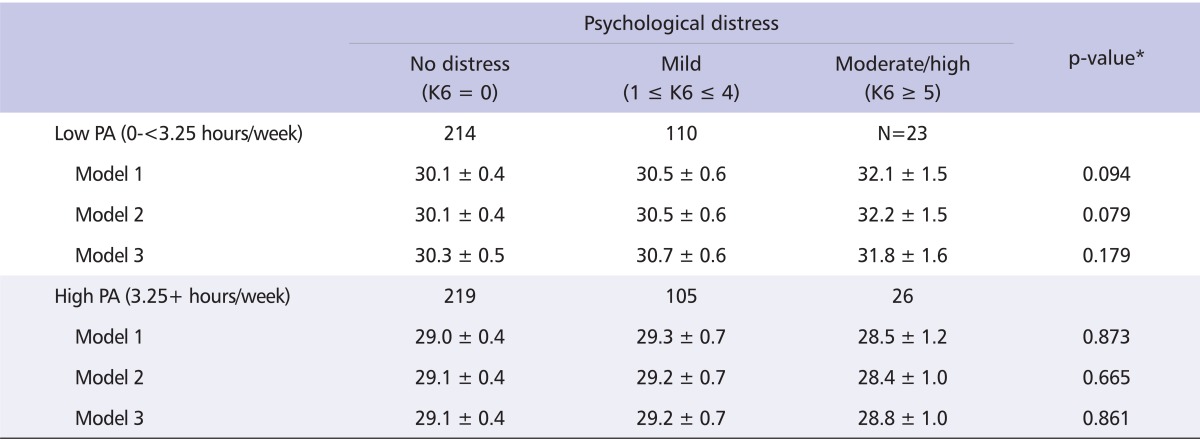
Values are presented as number or mean ± standard error.
Model 1: unadjusted; Model 2: adjusted for age, race/ethnicity; Model 3: adjusted for age, race/ethnicity, annual income, and education.
*The p-values are from linear regression models.
Interaction p-value <0.002 for psychological distress*physical activity among male law enforcement officers.
BMI: body mass index, NHIS: National Health Interview Survey, K6: Kessler 6, PA: Physical Activity.
Physical activity was a significant effect modifier in the relationship between the psychological distress and obesity among male LEOs (interaction p-value = 0.002) but not among female LEOs (interaction p-value = 0.860). Table 4 shows the association between psychological distress and BMI, stratified by physical activity for male LEOs. Among male officers reporting low physical activity, mean levels of BMI slightly increased as levels of psychological distress increased, but the trend was not statistically significant. This association was less striking and also not significant among male officers who reported high physical activity.
Discussion
This study shows that psychological distress was positively associated with BMI in female LEOs. There are few published studies that have investigated the association between psychological distress and obesity among LEOs. However, many more studies have been identified that have investigated the association between work-related stress and obesity. Findings regarding the association between high work distress and obesity among workers show mixed results. One study found no significant association between work stress and obesity [26]. Authors of a British cohort study [14] reported that job stress was a risk factor for weight gain depending on the baseline weight. Among workers with a BMI of < 22 kg/m2 at baseline, job stress resulted in weight loss, whereas among workers with a BMI of > 27 kg/m2 at baseline, it was associated with weight gain [14]. A longitudinal study conducted in the United States showed that increased psychosocial stress related to job-related demands was a risk factor for weight gain among adult males [11]. Other studies have reported that workplace stress is associated with higher uncontrolled eating [16] and increased obesity [13,27].
The current study found that the prevalence of serious psychological distress (K6 ≥ 13) among all LEOs was much lower (0.91%) compared to the average prevalence of United States working adults (1.57%). This result may suggest that LEOs are mentally healthy because good mental and physical health are pre-requisites for acceptance into the profession. Our study showed that female LEOs had more than triple the prevalence of serious psychological distress (i.e., K6 > 13) than male LEOs (2.03% vs. 0.56%, respectively) although overall prevalence was low. It is possible that female LEOs may experience greater occupational stress in the male-dominated profession of law enforcement [28-30]. Yoo and Franke [28] reported that female officers had significantly higher scores on perceived stress, job strain, vital exhaustion, and effort reward imbalance than male officers. Examples of work-related stressors that may be more likely to affect female officers are confronting death, violence, work schedule, gender discrimination, relationship with coworkers, and workload [29,30]. Recent studies [9,28] have reported that stressors among female officers, such as organizational problems and lack of support, were associated with more adverse cardiovascular risk factor levels and certain chronic diseases (metabolic syndrome, hypercholesterolemia, and diabetes). In our study, nervousness, restlessness/fidgeting, and high effort were associated with the most psychological distress regardless of gender. Our study also showed that female officers had a higher prevalence of nervousness than male officers. Psychological distress may operate through various factors (including several lifestyle behaviors such as levels of physical activity, dietary habits, and sleep habits) to influence weight. According to the American Psychological Association [31], sedentary behaviors (e.g., watching television, drinking, smoking, playing too many video games and surfing the internet) could have serious implications for weight gain. After stratification by physical activity, mean BMI increased with increasing psychological distress among male LEOs with low levels of physical activity, but the association was not significantly significant.
Some individuals may use food as a means of coping with distress. Those with high levels of distress may change their food choices from healthy foods (e.g., low fat) to unhealthy foods (e.g., high hydrogenated fat) and may also increase their food consumption [32,33]. Torres and Nowson [34] reviewed several studies and concluded that chronic stress was associated with higher consumption of high-sugar and high-fat foods and was related to weight gain in men. Fernandez and colleagues [15] reported that chronic and acute occupational stressors increased BMI among workers in upstate New York. We were unable to find published studies that investigated the association of distress with dietary changes or food intake among LEOs. However, a study conducted among transit workers suggest that dietary changes may be related to long work hours and shift work [35]. Persons who are scheduled to work on the night shift are known to have limited access to healthy restaurants, and they may be more likely to eat fast foods which contain high levels of fat and sugar [35]. Emotional and stress-related eating is associated with increased food intake which can lead to overweight and obesity [27,36,37].
Some officers may drink alcohol to cope with the strains and pressures of their work or in socialization with coworkers. Davey et al. [38] reported that 30% of officers in an Australian state police service were at risk of harm from excessive alcohol consumption. Heavy alcohol drinking, which is associated with increased caloric intake, has been linked to an increased BMI [39,40]. Previous research [41], however, found that among police officers in Mississippi, those with the greatest risk of drinking problems were young, white, and unmarried day-shift officers. Also, the prevalence of drinking among Mississippi officers was similar to that of the United States general population [41]. Our study confirmed that the prevalence of drinking > 3 drinks/week (21.9%) among LEOs was similar to that of NHIS United States workers (22.9%), but the average number of drinks per occasion (3.8) for LEOs was slightly higher than that of United States workers (3.1). Studies have shown that those with hazardous drinking behaviors had fewer occasions for drinking than the non-hazardous group, but consumed more drinks per occasion [39,41]. Lindsay [41] also reported that officers on the day shift were at greater risk for alcohol problems since most alcohol drinking occurs during the evenings. Gu and colleagues [42] showed alcohol drinking was positively correlated with waist circumference and abdominal height. Therefore, if officers drink excessively to cope with the challenges of their duties, this practice may adversely affect body weight and BMI.
A recent study conducted on a sample of the United States police officers reported significant inverse associations between perceived stress and sleep duration [43]. The authors also found that, in the fourth quartile of perceived stress, female officers were almost four times more likely and male officers were about six times more likely to experience poor sleep quality compared to officers in the first quartile of perceived stress. These findings have public health implications for obesity since studies have shown short sleep duration to be positively associated with metabolic syndrome and obesity [44,45].
One biological mechanism through which psychological stress may be associated with obesity is through increased cortisol production. Cortisol, a hormone which is secreted by the adrenal glands and is responsible for maintaining homeostasis, may be a physiological measure of stress. Chronic psychological stress prolongs high levels of cortisol, which have negative health effects such as hyperglycemia [46], elevated blood pressure and diminished heart rate variability [47], increased abdominal obesity [48,49], and metabolic syndrome [50]. Dallman [36] reported that persons who experience stress typically choose foods with high fat and sugar content even if they are neither hungry nor have a homeostatic need for calories, and concluded that stress and the brain stress networks promoted personal eating behaviors that may lead to obesity. Police studies reported that officers with post-traumatic stress disorder had higher awakening salivary cortisol levels [51], and cortisol dysregulation was apparent in male officers with metabolic syndrome [52]. In the highly stressful work environment of law enforcement, it is quite possible that LEOs may be experiencing chronic stress. Therefore the higher levels and prolonged elevation of cortisol may result in increased blood sugar and body fat.
Limitations and strengths
There are several limitations in this study. First, information bias may be present regarding BMI values due to the fact that height and weight were self-reported. Under-reporting weight and over-reporting height in the survey may have caused BMI to be underestimated, especially among obese women [53]. However, this type of bias would tend to influence the results toward the null (i.e., weaker or no significant association). In addition, use of self-reported information for BMI has been shown to be highly correlated with measured BMI in a previous study [54]. Second, this cross-sectional study design precludes inferences of cause and effect. For instance, the statement that the higher psychological distress was associated with higher BMI does not imply causality nor does it indicate the temporal nature of the association. It is not possible to determine the temporal sequence with this study design. Although we do not know the temporal relationship between psychological distress and obesity, we have analyzed psychological distress as though it were the exposure and obesity as the outcome based on previous studies. Two studies [55,56] have shown that psychological stress or worksite stress had a negative influence on obesity. Another study [57] found that psychological well-being was associated with weight loss and with improved nutritional behaviors. Third, since the psychological distress questionnaires were designed for the national survey, the six items (i.g., sadness, nervousness, restlessness, high efforts, hopelessness, and worthlessness) may not be sufficient to cover all stressors inherent in the law enforcement profession. In addition these questionnaires were used to assess general psychological distress and were not designed to measure work-related stress specifically.
There are also strengths to this study. To our knowledge, this study is the first to investigate the association between psychological distress and obesity in current LEOs. The sample size allowed for adequate power even after stratification by gender and physical activity. Another major strength of this study is that it was conducted in a nationally representative sample of the United States population.
In summary, our study showed that psychological distress was positively associated with BMI in female LEOs. In the highly stressful work environment of law enforcement, it is quite possible that LEOs may be experiencing chronic stress. Identifying interventions to control stress or decrease its effect on overweight and obesity may be critical in female LEOs. A longitudinal study design may reveal the directionality of the association between psychological distress and BMI as well as the potential role that physical activity might play in this association.
Footnotes
No potential conflict of interest relevant to this article was reported. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.Violanti JM, Fekedulegn D, Hartley TA, Andrew ME, Charles LE, Mnatsakanova A, Burchfiel CM. Police trauma and cardiovascular disease: association between PTSD symptoms and metabolic syndrome. Int J Emerg Ment Health. 2006;8:227–237. [PubMed] [Google Scholar]
- 2.Rasmusson AM, Schnurr PP, Zukowska Z, Scioli E, Forman DE. Adaptation to extreme stress: post-traumatic stress disorder, neuropeptide Y and metabolic syndrome. Exp Biol Med (Maywood) 2010;235:1150–1162. doi: 10.1258/ebm.2010.009334. [DOI] [PubMed] [Google Scholar]
- 3.Hartley TA, Burchfiel CM, Fekedulegn D, Andrew ME, Knox SS, Violanti JM. Associations between police officer stress and the metabolic syndrome. Int J Emerg Ment Health. 2011;13:243–256. [PMC free article] [PubMed] [Google Scholar]
- 4.Franke WD, Kohut ML, Russell DW, Yoo HL, Ekkekakis P, Ramey SP. Is job-related stress the link between cardiovascular disease and the law enforcement profession? J Occup Environ Med. 2010;52:561–565. doi: 10.1097/JOM.0b013e3181dd086b. [DOI] [PubMed] [Google Scholar]
- 5.Harpold JA, Feemster SL. Negative influences of police stress. FBI Law Enforc Bull. 2002;71:1–7. [Google Scholar]
- 6.Collins PA, Gibbs AC. Stress in police officers: a study of the origins, prevalence and severity of stress-related symptoms within a county police force. Occup Med (Lond) 2003;53:256–264. doi: 10.1093/occmed/kqg061. [DOI] [PubMed] [Google Scholar]
- 7.Green B. Post-traumatic stress disorder in UK police officers. Curr Med Res Opin. 2004;20:101–105. doi: 10.1185/030079903125002748. [DOI] [PubMed] [Google Scholar]
- 8.Caban AJ, Lee DJ, Fleming LE, Gómez-Marín O, LeBlanc W, Pitman T. Obesity in US workers: The National Health Interview Survey, 1986 to 2002. Am J Public Health. 2005;95:1614–1622. doi: 10.2105/AJPH.2004.050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartley TA, Knox SS, Fekedulegn D, Barbosa-Leiker C, Violanti JM, Andrew ME, Burchfiel CM. Association between depressive symptoms and metabolic syndrome in police officers: results from two cross-sectional studies. J Environ Public Health. 2012;2012:861219. doi: 10.1155/2012/861219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schulte PA, Wagner GR, Ostry A, Blanciforti LA, Cutlip RG, Krajnak KM, Luster M, Munson AE, O'Callaghan JP, Parks CG, Simeonova PP, Miller DB. Work, obesity, and occupational safety and health. Am J Public Health. 2007;97:428–436. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170:181–192. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kubzansky LD, Gilthorpe MS, Goodman E. A prospective study of psychological distress and weight status in adolescents/young adults. Ann Behav Med. 2012;43:219–228. doi: 10.1007/s12160-011-9323-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. Am J Epidemiol. 2007;165:828–837. doi: 10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- 14.Kivimäki M, Head J, Ferrie JE, Shipley MJ, Brunner E, Vahtera J, Marmot MG. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes (Lond) 2006;30:982–987. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- 15.Fernandez ID, Su H, Winters PC, Liang H. Association of workplace chronic and acute stressors with employee weight status: data from worksites in turmoil. J Occup Environ Med. 2010;52(Suppl 1):S34–S41. doi: 10.1097/JOM.0b013e3181c88525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nevanperä NJ, Hopsu L, Kuosma E, Ukkola O, Uitti J, Laitinen JH. Occupational burnout, eating behavior, and weight among working women. Am J Clin Nutr. 2012;95:934–943. doi: 10.3945/ajcn.111.014191. [DOI] [PubMed] [Google Scholar]
- 17.Dong C, Sanchez LE, Price RA. Relationship of obesity to depression: a family-based study. Int J Obes Relat Metab Disord. 2004;28:790–795. doi: 10.1038/sj.ijo.0802626. [DOI] [PubMed] [Google Scholar]
- 18.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 19.Barber J, Bayer L, Pietrzak RH, Sanders KA. Assessment of rates of overweight and obesity and symptoms of posttraumatic stress disorder and depression in a sample of Operation Enduring Freedom/Operation Iraqi Freedom veterans. Mil Med. 2011;176:151–155. doi: 10.7205/milmed-d-09-00275. [DOI] [PubMed] [Google Scholar]
- 20.NHIS Survey Description [Internet] Hyattsville (MD): National Center for Health Statistics (NCHS); 2011. [cited 2012 Mar 29]. 2010 National Health Interview Survey (NHIS) public use data release. Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2010/srvydesc.pdf. [Google Scholar]
- 21.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 22.Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. 2012;21:88–97. doi: 10.1002/mpr.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jorm AF, Windsor TD, Dear KB, Anstey KJ, Christensen H, Rodgers B. Age group differences in psychological distress: the role of psychosocial risk factors that vary with age. Psychol Med. 2005;35:1253–1263. doi: 10.1017/S0033291705004976. [DOI] [PubMed] [Google Scholar]
- 24.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 25.Klein RJ, Proctor SE, Boudreault MA, Turczyn KM. Statistical Notes, No. 24 (2002 Jun) Hyattsville (MA): National Center for Health Statistics; 2002. Healthy people 2010 criteria for data suppression. [PubMed] [Google Scholar]
- 26.Overgaard D, Gyntelberg F, Heitmann BL. Psychological workload and body weight: is there an association? A review of the literature. Occup Med (Lond) 2004;54:35–41. doi: 10.1093/occmed/kqg135. [DOI] [PubMed] [Google Scholar]
- 27.Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26:37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- 28.Yoo H, Franke WD. Stress and cardiovascular disease risk in female law enforcement officers. Int Arch Occup Environ Health. 2011;84:279–286. doi: 10.1007/s00420-010-0548-9. [DOI] [PubMed] [Google Scholar]
- 29.Violanti JM, Aron F. Ranking police stressors. Psychol Rep. 1994;75:824–826. doi: 10.2466/pr0.1994.75.2.824. [DOI] [PubMed] [Google Scholar]
- 30.Gershon RR, Lin S, Li X. Work stress in aging police officers. J Occup Environ Med. 2002;44:160–167. doi: 10.1097/00043764-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 31.2010 stress in American findings [Internet] Washington, DC: American Psychological Association; 2010. [cited 2012 Apr 23]. Available from: http://www.apa.org/news/press/releases/stress/national-report.pdf. [Google Scholar]
- 32.Zellner DA, Loaiza S, Gonzalez Z, Pita J, Morales J, Pecora D, Wolf A. Food selection changes under stress. Physiol Behav. 2006;87:789–793. doi: 10.1016/j.physbeh.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 33.Wallis DJ, Hetherington MM. Emotions and eating. Self-reported and experimentally induced changes in food intake under stress. Appetite. 2009;52:355–362. doi: 10.1016/j.appet.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 34.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23:887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 35.Escoto KH, French SA, Harnack LJ, Toomey TL, Hannan PJ, Mitchell NR. Work hours, weight status, and weight-related behaviors: a study of metro transit workers. Int J Behav Nutr Phys Act. 2010;7:91. doi: 10.1186/1479-5868-7-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21:159–165. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mullane CN. Distress tolerance, experiential avoidance, and negative affect: Implications for understanding eating behavior and BMI [PhD dissertation] Knoxville (TN): University of Tennessee; 2011. Available from: http://trace.tennessee.edu/utk_graddiss/1103. [Google Scholar]
- 38.Davey JD, Obst PL, Sheehan MC. It goes with the job: officers' insights into the impact of stress and culture on alcohol consumption within the policing occupation. Drug Educ Prev Policy. 2001;8:141–149. [Google Scholar]
- 39.Breslow RA, Smothers BA. Drinking patterns and body mass index in never smokers: National Health Interview Survey, 1997-2001. Am J Epidemiol. 2005;161:368–376. doi: 10.1093/aje/kwi061. [DOI] [PubMed] [Google Scholar]
- 40.Yeomans MR. Alcohol, appetite and energy balance: is alcohol intake a risk factor for obesity? Physiol Behav. 2010;100:82–89. doi: 10.1016/j.physbeh.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 41.Lindsay V. Police officers and their alcohol consumptionshould we be concerned? Police Quart. 2008;11:74–87. [Google Scholar]
- 42.Gu JK, Charles LE, Burchfiel CM, Fekedulegn D, Sarkisian K, Andrew ME, Ma C, Violanti JM. Long work hours and adiposity among police officers in a US Northeast City. J Occup Environ Med. 2012;54:1374–1381. doi: 10.1097/JOM.0b013e31825f2bea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Charles LE, Slaven JE, Mnatsakanova A, Ma C, Violanti JM, Fekedulegn D, Andrew ME, Vila BJ, Burchfiel CM. Association of perceived stress with sleep duration and sleep quality in police officers. Int J Emerg Ment Health. 2011;13:229–241. [PMC free article] [PubMed] [Google Scholar]
- 44.Wu MC, Yang YC, Wu JS, Wang RH, Lu FH, Chang CJ. Short sleep duration associated with a higher prevalence of metabolic syndrome in an apparently healthy population. Prev Med. 2012;55:305–309. doi: 10.1016/j.ypmed.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 45.Al-Hazzaa HM, Musaiger AO, Abahussain NA, Al-Sobayel HI, Qahwaji DM. Prevalence of short sleep duration and its association with obesity among adolescents 15- to 19-year olds: A cross-sectional study from three major cities in Saudi Arabia. Ann Thorac Med. 2012;7:133–139. doi: 10.4103/1817-1737.98845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCowen KC, Malhotra A, Bistrian BR. Stress-induced hyperglycemia. Crit Care Clin. 2001;17:107–124. doi: 10.1016/s0749-0704(05)70154-8. [DOI] [PubMed] [Google Scholar]
- 47.Vrijkotte TG, van Doornen LJ, de Geus EJ. Effects of work stress on ambulatory blood pressure, heart rate, and heart rate variability. Hypertension. 2000;35:880–886. doi: 10.1161/01.hyp.35.4.880. [DOI] [PubMed] [Google Scholar]
- 48.Epel ES, McEwen B, Seeman T, Matthews K, Castellazzo G, Brownell KD, Bell J, Ickovics JR. Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med. 2000;62:623–632. doi: 10.1097/00006842-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 49.Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 50.Branth S, Ronquist G, Stridsberg M, Hambraeus L, Kindgren E, Olsson R, Carlander D, Arnetz B. Development of abdominal fat and incipient metabolic syndrome in young healthy men exposed to long-term stress. Nutr Metab Cardiovasc Dis. 2007;17:427–435. doi: 10.1016/j.numecd.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 51.Violanti JM, Andrew ME, Burchfiel CM, Hartley TA, Charles LE, Miller DB. Post-traumatic stress symptoms and cortisol patterns among police officers. Policing. 2007;30:189–202. [Google Scholar]
- 52.Austin-Ketch TL, Violanti JM, Fekedulegn D, Andrew ME, Burchfiel CM, Vena JE. Metabolic syndrome and salivary cortisol: is there dysregulation among a group active duty urban police officers? Diabetes Metab Syndr. 2010;4:82–88. [Google Scholar]
- 53.Nawaz H, Chan W, Abdulrahman M, Larson D, Katz DL. Self-reported weight and height: implications for obesity research. Am J Prev Med. 2001;20:294–298. doi: 10.1016/s0749-3797(01)00293-8. [DOI] [PubMed] [Google Scholar]
- 54.McAdams MA, Van Dam RM, Hu FB. Comparison of self-reported and measured BMI as correlates of disease markers in US adults. Obesity (Silver Spring) 2007;15:188–196. doi: 10.1038/oby.2007.504. [DOI] [PubMed] [Google Scholar]
- 55.Moore CJ, Cunningham SA. Social position, psychological stress, and obesity: a systematic review. J Acad Nutr Diet. 2012;112:518–526. doi: 10.1016/j.jand.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 56.Buss J. Associations between obesity and stress and shift work among nurses. Workplace Health Saf. 2012;60:453–458. doi: 10.1177/216507991206001007. [DOI] [PubMed] [Google Scholar]
- 57.Braun TD, Park CL, Conboy LA. Psychological well-being, health behaviors, and weight loss among participants in a residential, Kripalu yoga-based weight loss program. Int J Yoga Therap. 2012;(22):9–22. [PubMed] [Google Scholar]