Abstract
Objective:
To predict the validity of Watch-PAT (WP) device for sleep disordered breathing (SDB) among highway bus drivers.
Method:
A total number of 90 highway bus drivers have undergone polysomnography (PSG) and Watch-PAT test simultaneously. Routine blood tests and the routine ear-nose-throat (ENT) exams have been done as well.
Results:
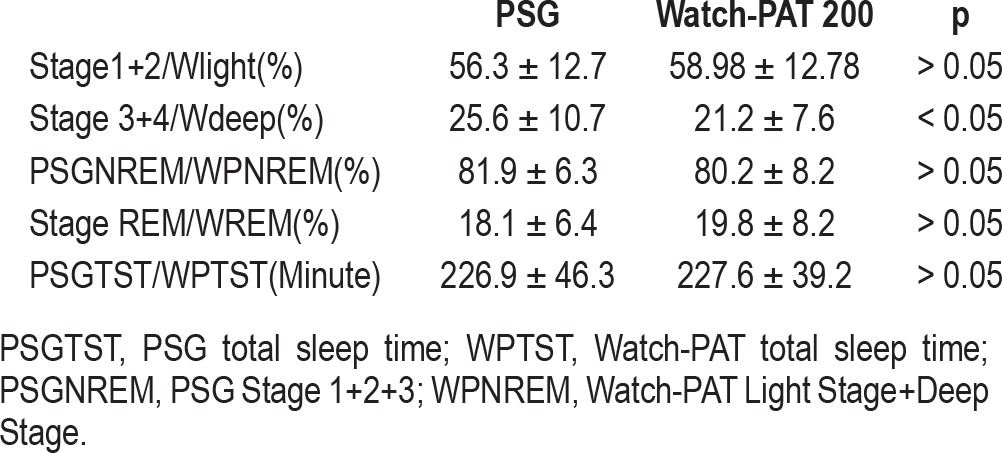
The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were 89.1%, 76.9%, 82% and 85.7% for RDI > 15, respectively. WRDI, WODI, W < 90% duration and Wmean SaO2 results were well correlated with the PSG results. In the sensitivity and specificity analysis, when diagnosis of sleep apnea was defined for different cut-off values of RDI of 5, 10 and 15, AUC (95%CI) were found as 0.84 (0.74-0.93), 0.87 (95%CI: 0.79-0.94) and 0.91 (95%CI: 0.85-0.97), respectively. There were no statistically significant differences between Stage1+2/Wlight and Stage REM/WREM. The percentage of Stage 3 sleep had difference significant statistically from the percentage of Wdeep. Total sleep times in PSG and WP showed no statistically important difference. Total NREM duration and total WNREM duration had no difference either.
Conclusion:
Watch-PAT device is helpful in detecting SDB with RDI > 15 in highway bus drivers, especially in drivers older than 45 years, but has limited value in drivers younger than 45 years old who have less risk for OSA. Therefore, WP can be used in the former group when PSG is not easily available.
Citation:
Yuceege M; Firat F; Demir A; Ardic S. Reliability of the Watch-PAT 200 in detecting sleep apnea in highway bus drivers. J Clin Sleep Med 2013;9(4):339-344.
Keywords: Ambulatory monitoring, sleep disordered breathing, highway driver, polysomnography
There have been many traffic accidents in our country, and the total number is constantly increasing. In 2002, there were 439,958 traffic accidents, and in 2011, there were 1,228,938 accidents reported in Turkey.1 Being sleepy and nonstop driving without sleeping are the most common factors (70.3%) related to these traffic accidents.1 Obstructive sleep apnea syndrome, insomnias, narcolepsy, periodic leg movements, jet lag, parasomnias, and depression may all lead to daytime sleepiness but are not routinely assessed in professional drivers.
In our country, an item published in the official register concerning polysomnography (PSG) indications for heavy-vehicle drivers states that any heavy vehicle driver applicant older than 45 years and those younger than 45 years with snoring, witnessed apnea, and/or daytime sleepiness with BMI > 25 should have a PSG before getting a license.2 However, the law is not in practical use because the number of applicants is substantially greater than the capacity of the sleep centers to test them; thus most of those who should have PSG testing cannot be tested.
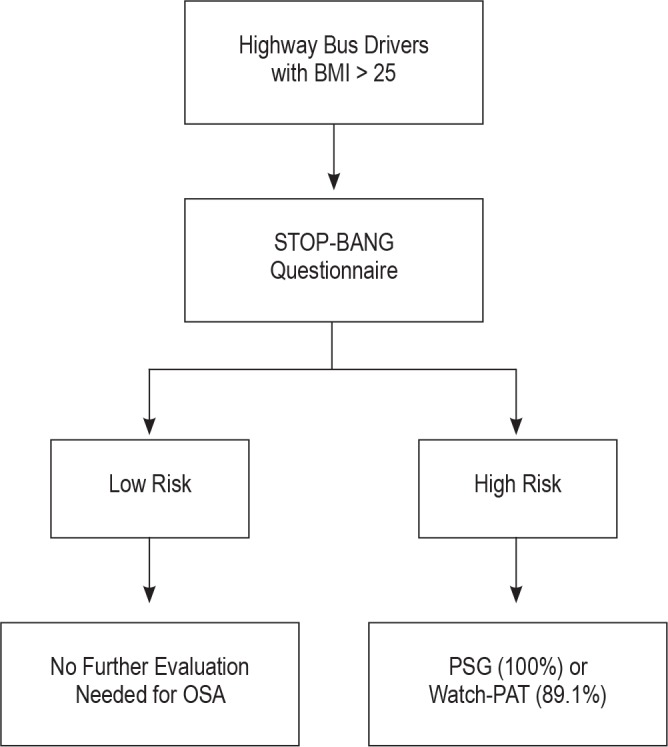
In a previous study (the first part of this study), we utilized four questionnaires to define drivers at high risk for sleep apnea and found that the STOP-BANG questionnaire is helpful and easy to use and can identify drivers at risk for OSA. We concluded it might be a potential alternative diagnostic pathway when portable monitoring or PSG are not accessible.3
High cost, long waiting lists, and the requirement of one night of hospitalization limit the usage of PSG. Less expensive and more practical unattended portable devices are now available in many sleep labs. In the current study, we aimed at validating such a device by simultaneously studying patients with a portable device and multichannel polysomnography. We hypothesized that the portable device, the Watch-PAT 200, would be accurate in diagnosing OSA in bus drivers.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Polysomnography is mandatory in drivers older than 45 years old and those with snoring, witnessed apnea and/or day time sleepiness who are younger than 45 years old, before getting a highway bus driver licence in Turkey, but the number of sleep centers are not enough to test all the applicants. This study has been done to test the accuracy of Watch-PAT device in detecting sleep disordered breathing among the highway bus drivers.
Study Impact: Watch-PAT device has been found to be helpful in detecting sleep disordered breathing especially in drivers older than 45 years old, thus it can be used to test sleep apnea before getting highway driver license, where polysomnography is not available.
METHOD
Subjects
We contacted two bus driver companies; 90 highway bus drivers willing to participate were enrolled to the study. The study was performed between September 2010 and December 2011. All participants underwent a simultaneous recording of PSG and the Watch-PAT 200.
PSG was performed for 5 h during the daytime after a full night's work (driving) without sleep. Fasting blood samples were taken for complete blood count, liver and renal function tests, spirometry, lipid panel, and thyroid function tests as routine tests for hospitalized patients. Drivers were analyzed for metabolic syndrome (according to ATPIII criteria). The results have previously been reported.3 Exclusion criteria were prior diagnosis of sleep apnea, α-blocker medication, bilateral sympathectomy, Raynaud disease, acrocyanosis, severe vasculopathy, neuropathy, and total sleep time < 180 min in PSG recordings. The study complied with the declaration of Helsinki and was approved by the local research ethics committee; all drivers gave written informed consent prior to participation.
Sleep Study
All drivers underwent daytime polysomnography using the Compumedics E series (Compumedics, Melbourne, Victoria, Australia); ≥ 5 h of recording was performed, and those with total sleep time < 180 min were excluded from the study. PSG recordings included 6-channel electroencephalography, 2-channel electrooculography, 2-channel submental electromyography, oxygen saturation by an oximeter finger probe, respiratory movements via chest and abdominal belts, airflow both via nasal pressure sensor and oro-nasal thermistor, electrocardiography, and leg movements via both tibial anterolateral electrodes. Sleep stages and respiratory parameters were scored according to the standard criteria of the American Academy of Sleep Medicine (AASM). Based on the guidelines of the AASM published in 2007, apnea was defined as ≥ 90% decrease in airflow persisting ≥ 10 s relative to the basal amplitude. Hypopnea was defined as ≥ 50% decrease in the airflow amplitude relative to the baseline value with an associated ≥ 3% oxygen desaturation or arousal, persisting ≥ 10 seconds.4
Apnea-hypopnea index (AHI) was calculated based on the following formula: total number of obstructive apneas + hypopneas / total sleep time (h). Patients with a sleep recording of < 5 h or total sleep time < 180 min were excluded. Sleep stage scoring was done by using software (Profusion PSG 3) in 30-s epochs by a certified registered polysomnographic technologist according to AASM criteria.4 The scoring technologist was blind to the Watch-PAT device result.
Watch-PAT 200
Watch-PAT 200 (Itamar Medical, Caesarea, Israel) is a 4-channel unattended home device, categorized as Level 3 device by the American Academy of Sleep Medicine. The channels are: (1) PAT (peripheral arterial tone), (2) pulse oximetry, (3) heart rate, and (4) actigraphy.
Peripheral arterial tone (PAT) signal measures the arterial pulsatile volume changes of the finger that are regulated by α-adrenergic innervation of the smooth muscles of the vasculature of the finger, and thus reflects sympathetic nervous system activity. This augmentation in sympathetic activity accompanies the increase in heart rate and desaturation at the termination of respiratory events. Thus, the WP indirectly detects apnea/hypopnea events by identifying surges of sympathetic activation associated with the termination of these events.5,6
Statistical Analysis
Descriptive statistics were provided as mean and standard deviation for numerical variables, and frequency and percentage for categorical variables. SPSS v 16.0 was used in the statistical analysis. Sensitivity, specificity, positive predictive value, negative predictive values, and 95%CI were calculated for different cutoff values of RDI and AHI (5, 10, and 15) selected to diagnose OSA. Receiver operating curves (ROCs) were drawn to evaluate the validity of WP for the diagnosis of OSA. Area under curve (AUC) and 95% CI was calculated. Pearson correlation analysis was performed to evaluate the correlation between PSG and WP. Agreement between the 2 methods was investigated with Bland-Altman plots for AHI, RDI, and ODI.7 The average of the findings of PSG and WP was graphed (x-axis) versus the difference between the PSG and WP (y-axis). Differences between the 2 methods were calculated as index measured with PSG minus index measured with WP. Differences were compared with 0 (no difference) and tested with one-sample t-test. A p value < 0.05 was considered as statistically significant in the two sided testing.
RESULTS
Of 90 highway bus drivers who were evaluated, 85 were included in the study; 5 were excluded due to short total sleep time (< 180 min). All participants were male; 23 were younger than 45 years, and 62 were older than 45 years. All of the drivers were shift workers; none of them were regular daily drivers. Fifty-two percent of the drivers had RDI > 15. Thirty-nine of 62 drivers (62.9%) older than 45 years and 7/23 (30.4%) drivers younger than 45 years old had RDI > 15. We performed routine blood examinations from these consecutive hospitalized patients and we evaluated their associated values (fasting glucose, triglyceride, and HDL level) for “metabolic syndrome.” The results were reported in our previous publication.3
The sensitivity, specificity, PPV and NPV were 89.1%, 76.9%, 82%, and 85.7% for RDI > 15, respectively. The specificity was 10% and sensitivity 96% for RDI > 5 (Table 1).
Table 1.
Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of Watch-PAT 200 for RDI > 5, RDI > 10, and RDI > 15 compared with polysomnography
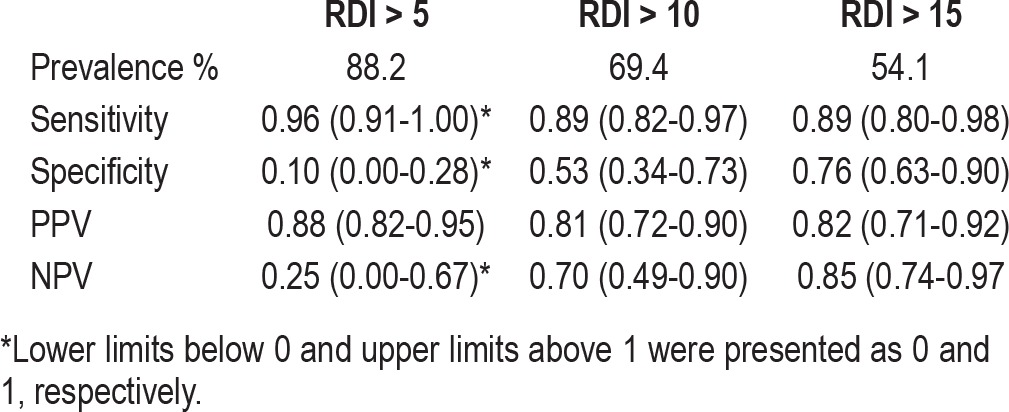
WRDI (RDI measured by Watch-PAT), WODI (Oxygen de-saturation index measured by Watch-PAT), W < 90% duration (< 90% saturation measured by Watch-PAT), and Wmean SpO2 (Mean SpO2 measured by Watch-PAT) results were well correlated with the PSG results (Table 2). As shown in the Table 3, age was relevant for the correct performance of Watch PAT. Scatter plot graphics and ROC curves of the PSG data and WP data are shown in Figures 1 and 2, respectively. In the sensitivity specificity analysis, when diagnosis of OSA was defined for different cutoff values of RDI of 5, 10, and 15, AUC (95%CI) were found as 0.84 (0.74-0.93), 0.87 (0.79-0.94), and 0.91 (0.85-0.97), respectively.
Table 2.
Correlation between polysomnographic data and Watch-PAT data
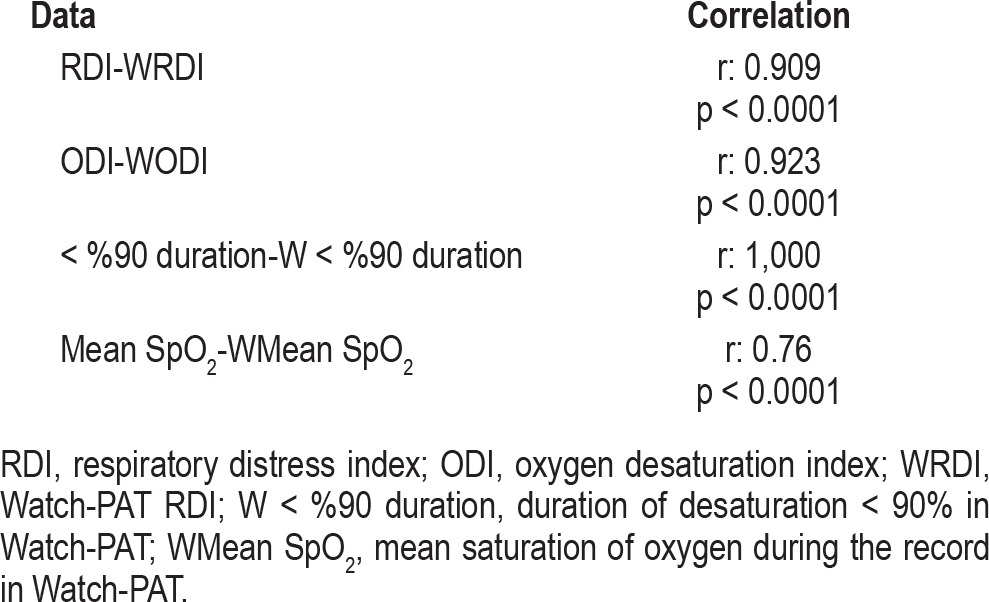
Table 3.
Validity of Watch-PAT 200 by age < 45 years old and > 45 years old

Figure 1. Scatter plots.

(A) AHI, (B) RDI, and (C) ODI recorded by PSG and WP. Pearson correlation coefficients were 0.96, 0.90, and 0.92, respectively (p < 0.001 for all).
Figure 2. Receiver-operator characteristic (ROC) analysis for the specificity and sensitivity for obstructive sleep apnea diagnosis of Watch-PAT for different cut-off values of PSG.
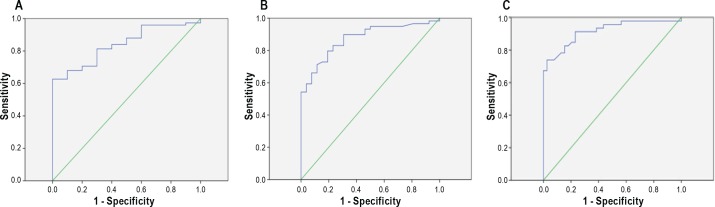
(A) RDI ≥ 5, (B) RDI ≥ 10, (C) RDI ≥ 15. Area under the curves and 95%CI's were 0.84 (0.74-0.93), 0.87 (0.79-0.94) and 0.91 (0.85-0.97), respectively.
Figure 3 shows the Bland-Altman plot of the comparison of 2 methods for AHI and RDI. The difference between the 2 methods was calculated as the index with PSG minus the index with WP. The difference had a mean (SD) -1.78 (4.18) for AHI, -1.43 (7.26) for RDI, and 0.54 (4.91) for ODI. WP AHIs were significantly larger than PSG AHIs. Differences for RDI and ODI were not significantly different from 0. Range of the differences (variance) increased with the mean value of the 2 methods, as illustrated in a funnel shaped graph. There was no systematic difference in RDI measurements.
Figure 3. Bland-Altman plot of the comparison of two methods.
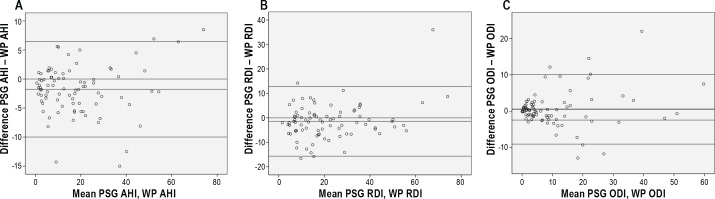
(A) AHI, (B) RDI, (C) ODI. Differences were calculated as index with PSG minus index with WP. Means of PSG and WP findings are on the x-axis, and differences are on the y-axis. Lines on the y-axis are drawn from 0, mean difference and mean ± 1.96 × SD of the differences. Statistical comparison of the differences with 0 gave p values of < 0.001 for AHI, 0.07 for RDI, and 0.30 for ODI.
There were no statistically significant differences between stage1+2/Wlight, stage REM/WREM. The percentage of stage 3 sleep differed significantly from the percentage of Wdeep. Total sleep times in PSG and WP showed no statistically significant difference. There were also no significant differences in total NREM duration and total WNREM duration (Table 4).
Table 4.
Sleep stages of PSG and Watch-PAT
DISCUSSION
We planned to evaluate the reliability of Watch-PAT 200 in detecting sleep apnea in highway bus drivers and found that polysomnographic values were well correlated with Watch-PAT values; r = 0.9, 0.92, 1, and 0.76 (p < 0.001) for RDI, ODI, < 90% duration, and mean oxygen saturation, respectively. Watch-PAT identified the drivers with RDI > 15 with 89.1% sensitivity and 76.9% specificity. There are studies confirming the validation of Watch-PAT device simultaneously with PSG,5,8–12 detection of the arousals,6,13 and assessment of CPAP efficacy.14,15 This is the first study evaluating the reliability of Watch-PAT in a particular group, in this case, highway bus drivers.
The statement from the Joint Task Force of the ACCP, American College of Occupational and Environmental Medicine and the National Sleep Foundation recommends in-service evaluation if the driver falls into one of five categories:
Sleep history suggestive of OSA,
- Two or more of the following:
- BMI > 35;
- neck circumference > 17 inches for men and > 16 inches for women;
- hypertension (new, uncontrolled, or unable to control with fewer than two medications)
Epworth Sleepiness Scale score > 10
Previously diagnosed sleep disorder, but recent medical visits/compliance data not available for immediate review
AHI > 5 but < 30 and no excessive daytime somnolence, no motor vehicle accidents, and no hypertension requiring ≥ 2 agents to control.16
In our previous study involving the same 85 highway bus drivers, the STOP-BANG questionnaire was shown to have the highest sensitivity and negative predictive value (87% and 76%, respectively) of the four questionnaires tested (Berlin, STOP, OSA50, and STOP-BANG) to assess risk of OSA.3 As a second procedure, the Watch-PAT 200 can be used to evaluate OSA in those drivers with high risk for OSA with 89.1% sensitivity (Figure 4). Low risk drivers (according to the STOP-BANG questionnaire) had a prevalence of 24% of RDI > 15, with 83% sensitivity and 84% specificity.
Figure 4. Algorithm for diagnosing OSA in highway bus drivers with BMI > 25 (in relation with our previous study with the same drivers in Firat et al.3).
The disadvantages of Watch-PAT 200 are: (1) It does not differentiate the type of respiratory event (obstructive apnea, mixed apnea, central apnea, or hypopnea) (2) The detection of the respiratory event relies on the augmented sympathetic activity. However, not all the arousals are the cause of the respiratory events. Other disorders (e.g., severe periodic limb movements) that cause arousal from sleep can cause sympathetic activation. Because of this reason, WP RDI results were higher than the PSG RDI results and this may explain why specificity was lower than the sensitivity.
The advantages of the Watch-PAT are5:
It does not require a sleep technician; adjustments can be learned and performed by any personnel.
Scoring is automated.
Hospitalization is not required.
Comparing the Watch-PAT and standard polysomnography, there were no significant differences in total sleep time, total NREM, light sleep stages, or REM, but there was a difference in estimation of deep sleep. Deep NREM sleep shifted partially to light stage of NREM in Watch-PAT in our study.
The association between sleep states and autonomic output has been studied extensively. The transition from wake to sleep is associated with decreasing sympathetic activity and increasing parasympathetic activity. REM sleep is characterized by increased variability of sympathetic activity with mild changes in parasympathetic activity.17–19 Light and deep sleep are differentiated by autonomic activations manifested predominantly as higher and more stable parasympathetic activity in deep sleep than light NREM sleep. Autonomic nervous system effects on heart rate, heart rate variability, or peripheral tone may be of significant importance in evaluating the quality of NREM sleep. The Watch-PAT recorder is based predominantly on recordings of peripheral arterial tone signal and pulse rate (two important outputs of the autonomic nervous system).18 In our study, the PAT signals helped to differentiate REM from NREM.
In Hedner's study,17 sleep stages were analyzed epoch by epoch with PSG; the authors reported accuracy of Watch-PAT as 0.475 Cohen κ in differentiating sleep stages. In their study, 14,351 deep stage epochs according to PSG were classified as deep stage in Watch-PAT, while 12,409 epochs classified as deep stage in PSG were classified as light sleep by the Watch-PAT. The statistical analyses showed moderate accuracy (Cohen κ coefficient 0.45). We were unable to analyze Watch-PAT epoch by epoch and calculate a Cohen κ coefficient.
Hypertension can be a cause of augmented sympathetic activity, and it is possible that this augmentation can lead to less deep sleep percentage in Watch-PAT, but this theory warrants further investigation.
We used Watch-PAT 200 in our study. Most of the studies are with Watch-PAT 100 device.5,6,8–15,18,19 Recently, Watch-PAT 200 has been shown to provide quick diagnosis in OSA and to be valid in the diagnosis of OSA during pregnancy.20,21
Our particular question was the reliability of this device in the diagnosis of obstructive sleep apnea in highway bus drivers. The feature of distinguishing sleep stages helps to augment the reliability of the device. Sleep staging and sleep architecture are important for understanding sleep pathology. In OSA patients, decreased REM continuity and deep sleep quantitity are hallmarks of the disease. Evaluating the patient as a whole with sleep structure, not with only AHI or RDI, helped to augment the diagnosis of OSA in our study group. The Watch-PAT had high sensitivity and specificity values when compared with PSG in the diagnosis of OSA in drivers with RDI > 15 and older than 45 years old, but the reliability of this device was limited especially in drivers with RDI < 15 (10% specificity, 25% NPV, Table 1) and younger than 45 years old (71% sensitivity 75% specificity, Table 3).
As all the drivers in the study were night drivers, we could not investigate the effect of sleep deprivation on PSG results. Some studies have shown that sleep deprivation may worsen the obstructive sleep apnea index.22,23
The major limitation of this study is that the comparison of the results of Watch-PAT and polysomnography were not performed epoch by epoch; total scores were compared because of the technical limitations of synchronizing PSG and Watch-PAT data. There are validation studies using epoch-by-epoch analysis.17,18 This limitation can have potential effect on defining sleep stages.
CONCLUSION
In our study, we found that the Watch-PAT 200 is helpful in detecting OSA in highway bus drivers, particularly in drivers older than 45, who have higher risk of OSA. The Watch-PAT 200 has limited value in diagnosing OSA in drivers younger than 45 years, who have less risk of OSA. Both polysomnography and Watch-PAT tests were performed during the same day which would be controlling the day-to-day variability of sleep study. Since the Watch-PAT test was performed in the sleep lab, it would be difficult to make inference about the clinical use of Watch-PAT in the ambulatory setting. We think that the Watch-PAT findings in the sleep lab and ambulatory setting would not be different, except for the changes in the quality of sleep due to sleeping in the lab. This should be investigated in further studies.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the Turkish Thoracic Society for providing financial support for this study.
REFERENCES
- 1.Turkish National Traffic Statistics of general Directorate of Security Affairs. 2012. Updated. Available from UTL: http//www.trafik.gov.tr/istatistikler/10_yil_istatistik.asp.
- 2.Official Register in Turkey with 26.09.2006 date and item no: 26301. Available from URL: http://www.resmigazete.gov.tr/2006/09/20060926-6.htm.
- 3.Firat H, Yuceege M, Demir A, Ardic S. Comparison of four established questionnaires to identify highway bus drivers at risk for obstructive sleep apnea in Turkey. Sleep Biol Rhythms. 2012. http://dx.doi.org/10.1111/j.1479-8425.2012.00566.x.
- 4.American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual. 2nd ed. Westchester IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 5.Bar AB, Pillar G, Dvir I, Sheffy J, Schnall RP, Lavie P. Evaluation of a portable device based on peripheral arterial tone for unattended home sleep studies. Chest. 2003;123:695–703. doi: 10.1378/chest.123.3.695. [DOI] [PubMed] [Google Scholar]
- 6.Pillar G, Bar A, Shlitner A, Schnall R, Shefy J, Lavie P. Autonomic arousal index detection based on peripheral arterial tonometry. Sleep. 2002;25:543–9. [PubMed] [Google Scholar]
- 7.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327:307–10. [PubMed] [Google Scholar]
- 8.Zou D, Grote L, Peker Y, Linblad U, Hedner J. Validation of a portable device for sleep apnea diagnosis in a population based cohort using synchronized home polysomnography. Sleep. 2006;29:367–74. doi: 10.1093/sleep/29.3.367. [DOI] [PubMed] [Google Scholar]
- 9.Pittman SD, Ayas NT, MacDonald MM, Malhotra A, Fogel RB, White DP. Using a wrist-worn device based on peripheral arterial tonometry to diagnose obstructive sleep apnea: in-laboratory and ambulatory validation. Sleep. 2004;27:923–33. doi: 10.1093/sleep/27.5.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ayas NT, Pittman S, MacDonald MM, White DP. Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med. 2003;4:435–42. doi: 10.1016/s1389-9457(03)00111-4. [DOI] [PubMed] [Google Scholar]
- 11.Kenny P. Pang, Christine G. Gourin, David J. Terris. A comparison of polysomnography and the WatchPAT in the diagnosis of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137:665–8. doi: 10.1016/j.otohns.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Hedner J, Pillar G, Pittman DS, Zou D, Grote L, White D. A Novel adaptive wrist actigraphy algorithm for sleep-wake assessment in sleep apnea patients. Sleep. 2004;27:1560–6. doi: 10.1093/sleep/27.8.1560. [DOI] [PubMed] [Google Scholar]
- 13.Pillar G, Bar A, Betito M, et al. An ambulatory device for detection of AASM defined arousals from sleep: the WP100. Sleep Med. 2003;4:207–12. doi: 10.1016/s1389-9457(02)00254-x. [DOI] [PubMed] [Google Scholar]
- 14.Pittman SD, Pillar G, Berry RB, Malhotra A, Macdonald MM, White DP. Follow-up assessment of CPAP efficacy in patients with obstructive sleep apnea using an ambulatory device based on peripheral arterial tonometry. Sleep Breath. 2006;10:123–31. doi: 10.1007/s11325-006-0058-x. [DOI] [PubMed] [Google Scholar]
- 15.Berry RB, Hill G, Thompson L, McLaurin V. Portable monitoring and auto-titration versus polysomnography for the diagnosis and treatment of sleep apnea. Sleep. 2008;31:1423–31. [PMC free article] [PubMed] [Google Scholar]
- 16.Hartenbaum N, Collop N, Rosen IM, et al. Sleep apnea and commercial motor vehicle operators. Statement from the Joint Task Force of the ACCP, American College of Occupational and Environmental Medicine and the National Sleep Foundation. Chest. 2006;130:902–5. doi: 10.1378/chest.130.3.902. [DOI] [PubMed] [Google Scholar]
- 17.Hedner J, White DP, Malhotra A, et al. Sleep staging based on autonomic signals: a multi-center validation study. J Clin Sleep Med. 2011;7:301–6. doi: 10.5664/JCSM.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bresler M, Sheffy K, Pillar G, Preiszler M, Herscovici S. Differentiating between light and deep sleep stages using an ambulatory device based on peripheral arterial tonometry. Physiol Meas. 2008;29:571–84. doi: 10.1088/0967-3334/29/5/004. [DOI] [PubMed] [Google Scholar]
- 19.Hersovici S, Peker A, Papyan S, Lavie P. Detecting REM sleep from the finger; an autonomic REM sleep algorithm based on peripheral arterial tone and actigraphy. Physiol Meas. 2007;28:129–40. doi: 10.1088/0967-3334/28/2/002. [DOI] [PubMed] [Google Scholar]
- 20.Ceylan T, Firat H, Kuran G, Ardic S, Bilgin E, Celenk F. Quick diagnosis in obstructive sleep apnea syndrome: WatchPAT-200. Iran Red Crescent Med J. 2012;14:475–8. [PMC free article] [PubMed] [Google Scholar]
- 21.O'Brien LM, Bullough AS, Shelgikar AV, Chames MC, Armitage R, Chervin RD. Validation of Watch-PAT 200 against polysomnography during pregnancy. J Clin Sleep Med. 2012;8:287–94. doi: 10.5664/jcsm.1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paciorek M, Korczynski P, Bielicki P, Byskiniewicz K, Zielinski J, Chazan R. Obstructive sleep apnea in shift workers. Sleep Med. 2011;12:274–7. doi: 10.1016/j.sleep.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Laudencka A, Klawe JJ, Tafil-Klawe M, Ztomanczuk P. Does night-shift work induce apnea events in obstructive sleep apnea patients? J Physiol Pharmacol. 2007;58(Suppl)(Pt 1):345–7. [PubMed] [Google Scholar]


