Abstract
Untreated obstructive sleep apnea (OSA) can lead to important neurobehavioral consequences including cognitive deficits, hyperactivity/inattention, daytime sleepiness, and mood disturbances. Interestingly, the potential role of OSA in the pathogenesis of impulse-control disorders such as nail biting (onychophagia) is currently unknown. We present a case of a man with severe onychophagia and biting-induced finger mutilation that was completely resolved after diagnosis and treatment of severe OSA. Accordingly, this report represents an important clinical observation that suggests a connection between sleep physiology and the neurobiological circuits implicated in the regulation of impulse-control behaviors. Further research in this area may improve our current understanding of the neurobehavioral consequences of untreated OSA.
Citation:
Nino G; Singareddy R. Severe onychophagia and finger mutilation associated with obstructive sleep apnea. J Clin Sleep Med 2013;9(4):379-381.
Keywords: OSA, nail biting, onychophagia, finger mutilation
Severe nail biting (onychophagia) and finger self-mutilation are often associated with psychiatric disorders such as schizophrenia, obsessive-compulsive personality traits, anxiety, autism, and mental retardation.1 Although obstructive sleep apnea (OSA) has been linked to cognitive deficits, hyperactivity/inattention, daytime sleepiness and mood disturbances,2 its potential role in the pathogenesis of impulse-control behavior disorders like onychophagia is currently unknown.
REPORT OF CASE
We present the case of a 47-year-old man with history of quadriplegia due to complete spinal injury at C5 level following a motor vehicle accident occurring 20 years before, who was referred for evaluation of severe snoring, multiple awakenings, and nocturnal breathing difficulties suggestive of OSA. His spinal injury did not abolish diaphragmatic function, so he did not require mechanical ventilatory support during wakefulness or sleep. There were no symptoms of restless legs syndrome or nightmares, and average sleep duration of 6-8 h was reported. He was tired and had excessive daytime sleepiness, scoring 15/24 on the Epworth Sleepiness Scale (ESS). There were no hallucinations, cataplexy, or other features of narcolepsy. There was no history of neuropathic pain. He also had a history of several years of diurnal and nocturnal onychophagia associated with biting-induced nail avulsion and finger mutilation (Figure 1A). He had required medical attention multiple times due to soft tissue infection and bleeding after finger injuries. He was on sertraline (150 mg) and imipramine (25 mg) for major depression and had continued to have mild depressive symptoms as indicated by a Beck Depression Inventory-II score of 15. Physical examination revealed a body mass index of 28 kg/ m 2, crowded pharyngeal appearance (Mallampati score 3), and atrophic nail beds on both hands with mutilation of the fourth and fifth fingertips of the left hand (Fig 1A.). He had neurological sequelae of quadriplegia, consistent on motor and sensory deficits below C5 level without elbow extension and no finger or wrist movement. Contractures and muscle wasting were present, but he had good head, neck, and shoulder mobility with adequate elbow flexion, which together allowed him sufficient range of motion to produce the self-injurious behavior.
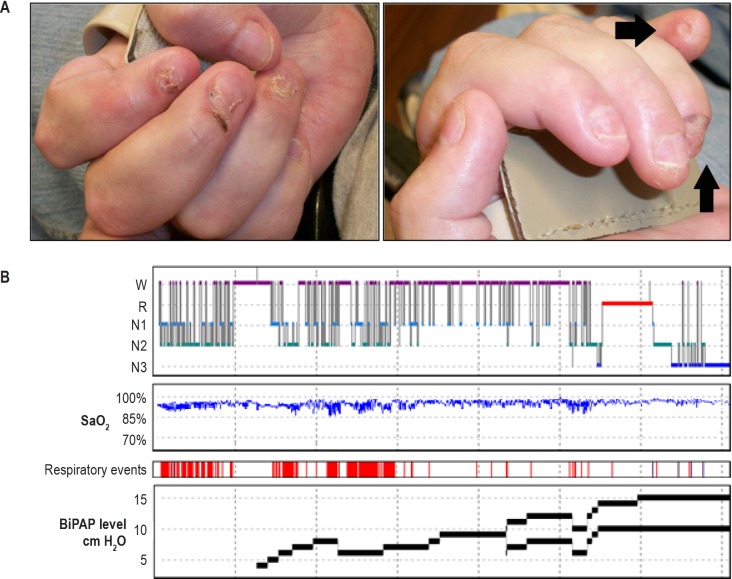
Figure 1.
(A) Right and left hand with nail avulsions and fingertip mutilation. Note mutilation of fourth and fifth fingertips in the left hand (black arrows) and generalized nail atrophy.(B) Polysomnography (Room air). Severe OSA (AHI 65/h) associated with sleep fragmentation and intermittent hypoxemia. BiPAP levels of 14/10 cm H2O (last portion of the night) completely improved sleep breathing abnormalities.
Given his clinical history, overnight polysomnogram (PSG) was conducted to assess for OSA. His PSG demonstrated severe OSA with an apnea-hypopnea-index (AHI) of 65/h; therefore, positive airway pressure (PAP) titration was performed (Figure 1B). PAP titration was started at 4 cm H2O of continuous PAP (CPAP) and increased to 14/10 cm H2O of bilevel PAP (BiPAP) which completely resolved his sleep disordered breathing (Figure 1B). His follow-up evaluation 8 weeks after BiPAP initiation revealed excellent objective compliance. His BiPAP smart card download showed that the device was used 95% of the nights with an average of 7 h per night. Clinically, he had substantial improvement in nocturnal awakenings and daytime sleepiness (ESS = 5/24) and complete resolution of snoring. Of particular interest was the clinical improvement in onychophagia, which essentially disappeared after OSA therapy with BiPAP. One year following initial OSA diagnosis and treatment, he has had no further episodes of nail biting or finger injury.
DISCUSSION
Untreated OSA has been linked to daytime sleepiness, hyper-activity/inattention, cognitive deficits and mood disturbances.2 Although severe onychophagia is known to be associated with sleep disturbances,1 to our knowledge, this is the first description of OSA being associated with this type of impulse control disorder. Our patient had been biting and mutilating his fingers for several years. This behavior was not associated with any major psychopathology or traits of personality disorder and it was not responsive to antidepressant medications, which are reported to have beneficial effects in some cases of severe onycophagia.1 Interestingly, after starting therapy for severe OSA, there was a complete resolution of his onychophagia. There were also reported improvements in his mood despite no changes in the dosage of antidepressant medications. While the dramatic neurobehavioral improvement of this quadriplegic patient cannot be generalized to the general population, this case report represents an important clinical observation that suggests that the psychopathological consequences of untreated OSA may be more broad and complex than currently known.
There are several possible mechanisms that may explain such a dramatic neurobehavioral improvement following OSA therapy. For instance, in this case OSA was associated with severe sleep fragmentation (Figure 1B) resulting in chronic sleep deprivation, which is known to increase impulsive behavior.3 In this regard, it is noteworthy that recent evidence suggests that the biological activity of dopamine in the brain, which is implicated in the regulation of impulse control,4 is greatly affected by sleep deprivation via down-regulation of central dopamine D2 receptor signaling, as determined by positron emission tomography (PET) measurements in human brains and cerebral microdialysis in rodents.5 Moreover, we have previously reported that individuals with pathological excoriation or skin picking have poorer subjective sleep,6 which suggests a broader connection between impulse control disorders and disturbances of sleep in general, not just OSA. Accordingly, obtaining a careful sleep history may be of critical importance in the evaluation of patients with intractable self-injurious behaviors. In our particular case, nail biting and finger self-mutilation could also have been influenced by cognitive deficits that are known to occur in OSA patients.2 Not surprisingly, deficits in an executive function dimension (risk-related decision making) that is implicated in impulse control were recently identified in individuals at risk for OSA.7 In conclusion, although the precise underlying mechanisms remain unclear, the present report highlights the relationship between sleep and the neurobiological circuits that regulate impulse control behaviors. Further research in this area may elucidate novel mechanisms underlying the neurobehavioral consequences of untreated OSA.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Michopoulos I, Gournellis R, Papadopoulou M, et al. A case of autophagia: a man who was mutilating his fingers by biting them. J Nerv Ment Dis. 2012;200:183–5. doi: 10.1097/NMD.0b013e318243989b. [DOI] [PubMed] [Google Scholar]
- 2.Owens JA. Neurocognitive and behavioral impact of sleep disordered breathing in children. Pediatr Pulmonol. 2009;44:417–22. doi: 10.1002/ppul.20981. [DOI] [PubMed] [Google Scholar]
- 3.Acheson A, Richards JB, de Wit H. Effects of sleep deprivation on impulsive behaviors in men and women. Physiol Behav. 2007;91:579–87. doi: 10.1016/j.physbeh.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 4.Winstanley CA, Theobald DE, Dalley JW, Robbins TW. Interactions between serotonin and dopamine in the control of impulsive choice in rats: therapeutic implications for impulse control disorders. Neuropsychopharmacology. 2005;30:669–82. doi: 10.1038/sj.npp.1300610. [DOI] [PubMed] [Google Scholar]
- 5.Volkow ND, Tomasi D, Wang GJ, et al. Evidence that sleep deprivation down-regulates dopamine D2R in ventral striatum in the human brain. J Neurosci. 2012;32:6711–7. doi: 10.1523/JNEUROSCI.0045-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singareddy R, Moin A, Spurlock L, Merritt-Davis O, Uhde TW. Skin picking and sleep disturbances: relationship to anxiety and need for research. Depress Anxiety. 2003;18:228–32. doi: 10.1002/da.10153. [DOI] [PubMed] [Google Scholar]
- 7.McNally KA, Shear PK, Tlustos S, Amin RS, Beebe DW. Iowa Gambling Task performance in overweight children and adolescents at risk for obstructive sleep apnea. J Int Neuropsychol Soc. 2012;18:481–9. doi: 10.1017/S1355617711001937. [DOI] [PMC free article] [PubMed] [Google Scholar]