Abstract
Study Objectives:
Patients undergoing surgery have severe sleep and sleep-wake rhythm disturbances resulting in increased morbidity. Actigraphy is a tool that can be used to quantify these disturbances. The aim of this manuscript was to present the literature where actigraphy has been used to measure sleep and sleep-wake rhythms in relation to surgery.
Methods:
A systematic review was performed in 3 databases (Medline, Embase, and Psycinfo), including all literature until July 2012.
Results:
Thirty-two studies were included in the review. Actigraphy could demonstrate that total sleep time and sleep efficiency was reduced after surgery and number of awakenings was increased in patients undergoing major surgery. Disturbances were less severe in patients undergoing minor surgery. Actigraphy could be used to differentiate between delirious and non-delirious patients after major surgery. Actigraphy measurements could determine a differential effect of surgery based on the patient's age. The effect of pharmacological interventions (chronobiotics and hypnotics) in surgical patients could also be demonstrated by actigraphy.
Conclusion:
Actigraphy can be used to measure sleep and sleep-wake rhythms in patients undergoing surgery.
Citation:
Madsen MT; Rosenberg J; Gögenur I. Actigraphy for measurement of sleep and sleep-wake rhythms in relation to surgery. J Clin Sleep Med 2013;9(4):387-394.
Keywords: Actigraphy, surgery, sleep disturbances, sleep-wake rhythm, and activity
Disturbed sleep and sleep-wake rhythms represent a major problem for patients after surgery1 and may result in prolonged postoperative convalescence,2 cardiovascular morbidity,3–5 cognitive dysfunction,6,7 and impaired immune function.8–11 Furthermore, improved morbidity and mortality has been correlated with a more marked rest-activity rhythm.12,13
The golden standard for measuring sleep is polysomnography (PSG). Although ambulatory devices have been developed the method includes multiple electrodes, resulting in reduced mobility and discomfort.14 The analysis of a PSG recording is also resource demanding,15 and there exists no automatic analysis scoring system with sufficient reliability.16 An actigraph, which is a small wrist-worn device, can be used to measure sleep, circadian rhythm, activity rhythm, and activity in general.17 The advantages of actigraphy are high level of mobility,14 the possibility of measuring over longer periods of time (days to months),18 low cost,18 and minimal data editing required for data analysis.15,19 Actigraphy has been validated against polysomnography with high levels of sensitivity and specificity in various nonsurgical patient populations.17,18,20,21 In this systematic review, we present an overview of studies where actigraphy has been used to describe sleep and sleep-wake rhythms in relation to surgery, including patients undergoing cardiac surgery, general surgery, and ambulatory surgery. The strengths and weaknesses of actigraphy will be reviewed and discussed.
METHOD
The systematic search was performed in 3 databases: MEDLINE, Embase, and PsycINFO. All 3 systematic searches were performed in July 2012. The following terms where used for inclusion of studies: “surgery OR outpatient surgery OR fast track surgery OR general surgery” AND “actigraphy [Mesh-term] OR actigraphy* OR actigraphy OR actigraphic recording OR wrist actigraphy OR actometer OR actimeter OR actical OR actiwatch OR sleep-watch”. There were no limitations on study design. The impact of the surgical intervention on sleep and sleep-wake rhythms was the primary outcome of interest. Neurosurgical procedures were excluded due to the possibility of direct central nervous system influence on regulation of sleep and sleep-wake rhythms. Ear, nose, and throat surgery were excluded because ear, nose, and throat diseases have chronic sleep disturbances as one of their manifestations. The endocrine metabolic stress response is also minimal in ear, nose, and throat surgery. Only studies in which actigraphy was used to assess sleep or sleep-wake rhythm were included. The perioperative period was defined as one week preoperatively to six months postoperatively. This was done because the effect of the surgical trauma on sleep, circadian rhythm, and activity was the area of interest. Non-English language studies were excluded, and no conference abstracts or dissertations were included in the review. Information was extracted from each study on study design, surgery type, and number of patients included.
RESULTS
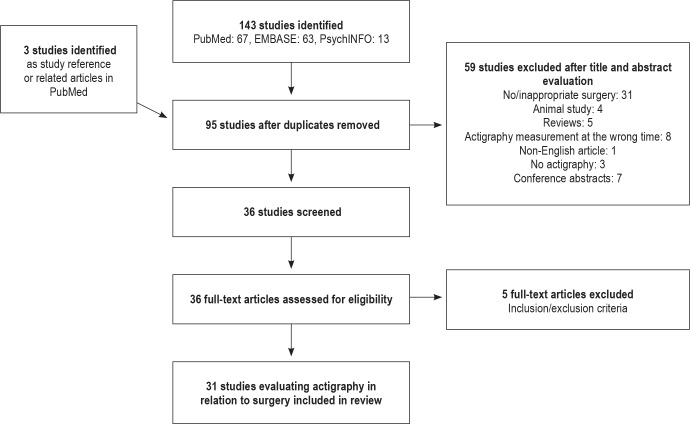
Based on the search strategy, a total of 143 studies were identified from the 3 search engines (Figure 1). After duplicates were removed, 95 studies were left and these were evaluated on title and abstract. Thirty-six studies were selected for full article examination, and 59 were excluded due to the exclusion criteria. The primary reason for exclusion were no surgical procedure or surgical procedures within the exclusion criteria (31/59), animal studies (4/59), reviews (5/59), wrong time placement of actigraph (not in relation to the perioperative phase; 8/59), non-English article (1/59), no actigraphy measurement (3/59), and conference abstracts (7/59). After full article reading, another 5 studies were excluded, 4 due to procedures within the exclusion criteria and one because the measurement was not in the perioperative period. Therefore, 31 articles were included in the final review. Sleep and sleep-wake rhythm were the focus in 24 and 15 studies, respectively. Eight of the studies measured both sleep and sleep-wake rhythm.2,22–27
Figure 1. Flowchart for studies included in systematic review.
Sleep
Of the 24 studies in which actigraphy was used to assess sleep, 9 studies were in patients undergoing cardiac surgery,25–27,31–36 6 general surgery,2,22–24,37,38 5 outpatient surgery,39–43 2 breast surgery,44,45 and the last 2 studies involved gynecological/obstetric surgery.46,47 Three studies were randomized clinical trials.24,42,43 The 24 studies were conducted between 1996 and 2011. The smallest study included 11 patients, and the largest included 169 patients. In 12 studies there was a control group22,24–27,32,40–43,46,47; 5 of these studies included healthy controls.22,26,27,40,41
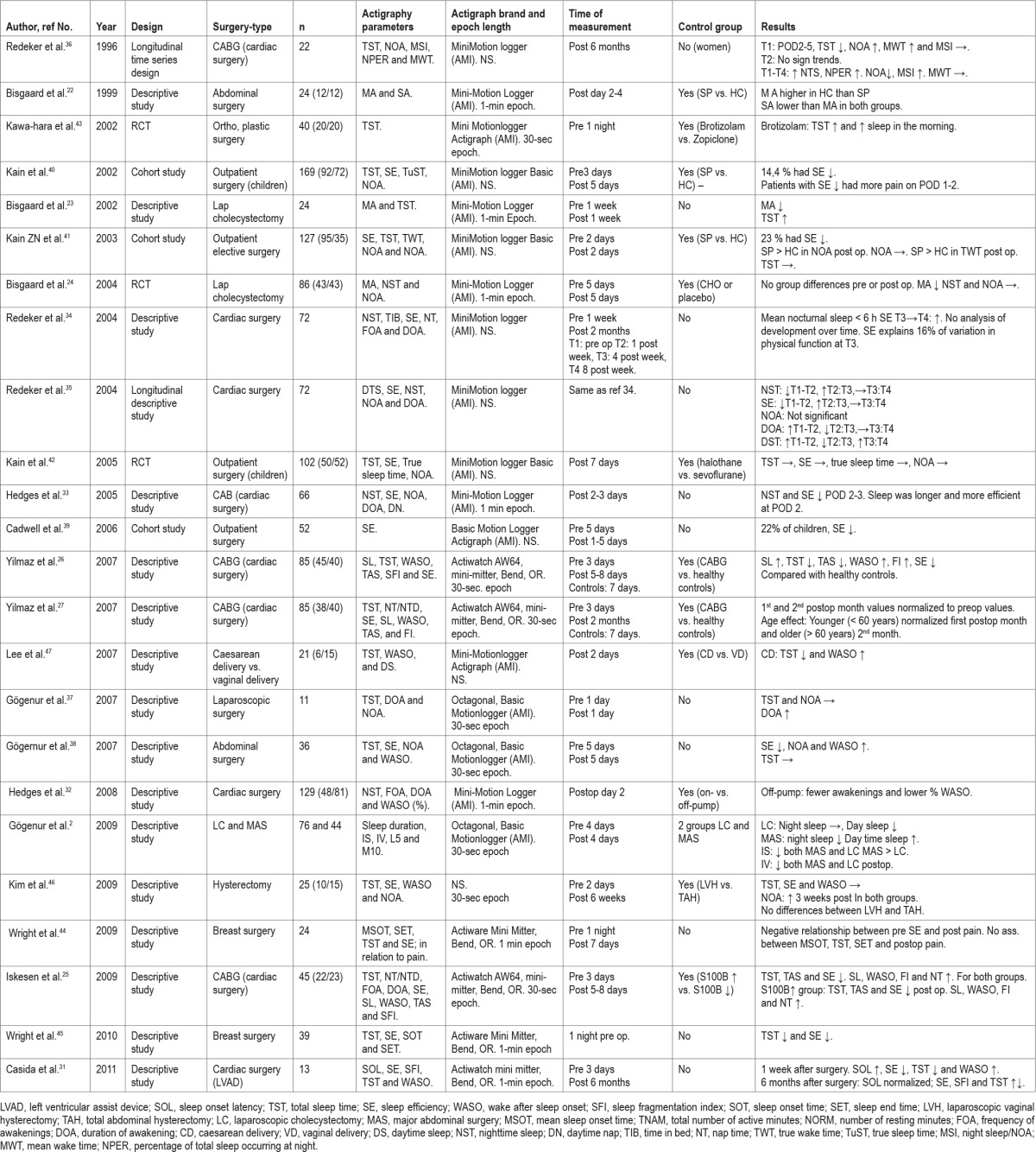
In 23 of the 24 studies, total sleep time/nighttime sleep was assessed by actigraphy (Table 1). In 16 studies, sleep efficiency was reported. In 16 studies, the frequency, number, and duration of awakenings was reported; in 8 studies, wake after sleep onset was reported.
Table 1.
Sleep studies
Cardiac Surgery
In the 9 studies including patients undergoing cardiac surgery,25–27,31–36 the population size was 13-129. Most of the procedures were coronary artery bypass surgery25–27,32–36; one was placement of a left ventricular assist device through an open procedure.31 Six of the 9 studies included both preoperative and postoperative values,25–27,31,34,35 with only postoperative values in the remaining 3 studies.32,33,36
When using actigraphy to assess sleep after cardiac surgery, it was shown that total sleep time was reduced in the first week after surgery. The sleep time tended to normalize after one month but could be affected as long as 6 months postoperatively. Sleep efficiency was measured in 7 of the 9 studies25–27,31,32,35,36 and showed the same tendency as total sleep time, with a reduction in the first postoperative week and normalization one month postoperatively. An age effect was shown, where people < 60 years returned to preoperative values after one month, but people > 60 years needed 2 months to return to preoperative values.27 Number of awakenings, measured in 5 studies,32–36 did not change after cardiac surgery. The duration of awakenings, however, increased in the postoperative week, and returned to normal after one month. Wake after sleep onset was measured in 5 of the 9 studies25–27,31,32 and increased in the first postoperative week. In a case-control study where 48 patients undergoing on-pump cardiac surgery were compared with 81 patients undergoing off-pump surgery, it was shown that patients undergoing off-pump cardiac surgery had fewer awakenings and a lower percentage of wake after sleep onset.32 In 3 studies,25–27 sleep latency was shown to be increased in the postoperative week and normalized after one month. Another study25 also showed that the total sleep time, sleep efficiency, number and duration of awakenings, wake after sleep onset, and sleep latency all were disturbed after cardiac surgery. In the same study it was shown that patients with increased S100B (plasma marker of CNS injury) measured 12 h postoperatively had a more disturbed sleep than patients without increased S100B.
General Surgery
Sleep was measured with actigraphy in relation to general surgery in 6 studies.2,22–24,37,38 Population size was between 11 and 120 patients; there was one randomized controlled trial.24 The surgical procedures were either laparoscopic,23,24,37 major abdominal surgery,22,38 or both.2 All 6 studies included measurements before and after the surgical procedure. Total sleep time was not changed after laparoscopic procedures,24,37 and this was also the case with number of awakenings.24,37 The only exception was in the study by Bisgaard et al.,23 who showed an increase in total sleep time in the first 2 days after uncomplicated laparoscopic cholecystectomy. In patients undergoing major abdominal surgery, daytime sleep increased after surgery compared to preoperatively.2 Sleep efficiency was also reduced after major abdominal surgery,38 and number of awakenings and wake after sleep onset were increased.38
Ambulatory Surgery
There were 5 studies in the ambulatory setting,39–43 where patients underwent orthopedic, plastic, ophthalmic, or minor general surgical procedures. Three of these studies39–41 defined sleep impairment as a reduction of one standard deviation in sleep efficiency measured by actigraphy. All 3 studies included both preoperative and postoperative measurements. Two of these studies only included children undergoing outpatient surgery.39,40 In these children, 14% to 22% suffered from sleep impairment39,40; in the adult population, 23% had sleep impairment after surgery.41 A healthy control group was present in 2 of the studies40,41; the studies included 92-95 patients and 35-72 controls. In the adult study, surgical patients also had an increased number of awakenings longer than 5 minutes compared with the healthy controls.41
In a double-blinded randomized clinical trial,42 halothane anesthesia was compared with sevoflurane anesthesia. The study showed no difference between the groups for any of the sleep parameters after ambulatory surgery (total sleep time, sleep efficiency, or number of awakenings). In another randomized clinical trial,43 brotizolam was compared with zopiclone as a preoperative hypnotic with actigraphic measurements of sleep on the night before surgery. Here it was shown that patients treated with brotizolam had better sleep with significantly higher total sleep time than patients treated with zopiclone.
Other Surgical Procedures
Two studies described sleep in relation to breast surgery.44,45 One study45 showed that intrusive thoughts and anxiety about the operation were associated with total sleep time and sleep efficiency on the preoperative night. An increasing degree of intrusive thoughts resulted in a reduced total sleep time and sleep efficiency. In a study by the same author,44 it was shown that preoperative reduced sleep efficiency measured by actigraphy was an indicator of the severity of postoperative pain. The duration of preoperative sleep had no effect on postoperative pain, but the disruption (low sleep efficiency) of preoperative sleep was an indicator of postoperative pain.
Two studies involved gynecological or obstetric procedures.46,47 One study compared caesarian versus vaginal delivery.47 The study showed that women undergoing caesarian section had a shorter total sleep time and a higher wake after sleep onset than women having vaginal delivery. The women undergoing caesarian section also had increased daytime sleep. In the other gynecological study,46 patients undergoing laparoscopic vaginal hysterectomy were compared with patients undergoing total abdominal hysterectomy. In the patient group as a whole, there was an increase in number of awakening 3 weeks after surgery but no change in total sleep time or sleep efficiency. Between the 2 groups, however, there were no significant differences in any of the parameters.46
Sleep-Wake Rhythm
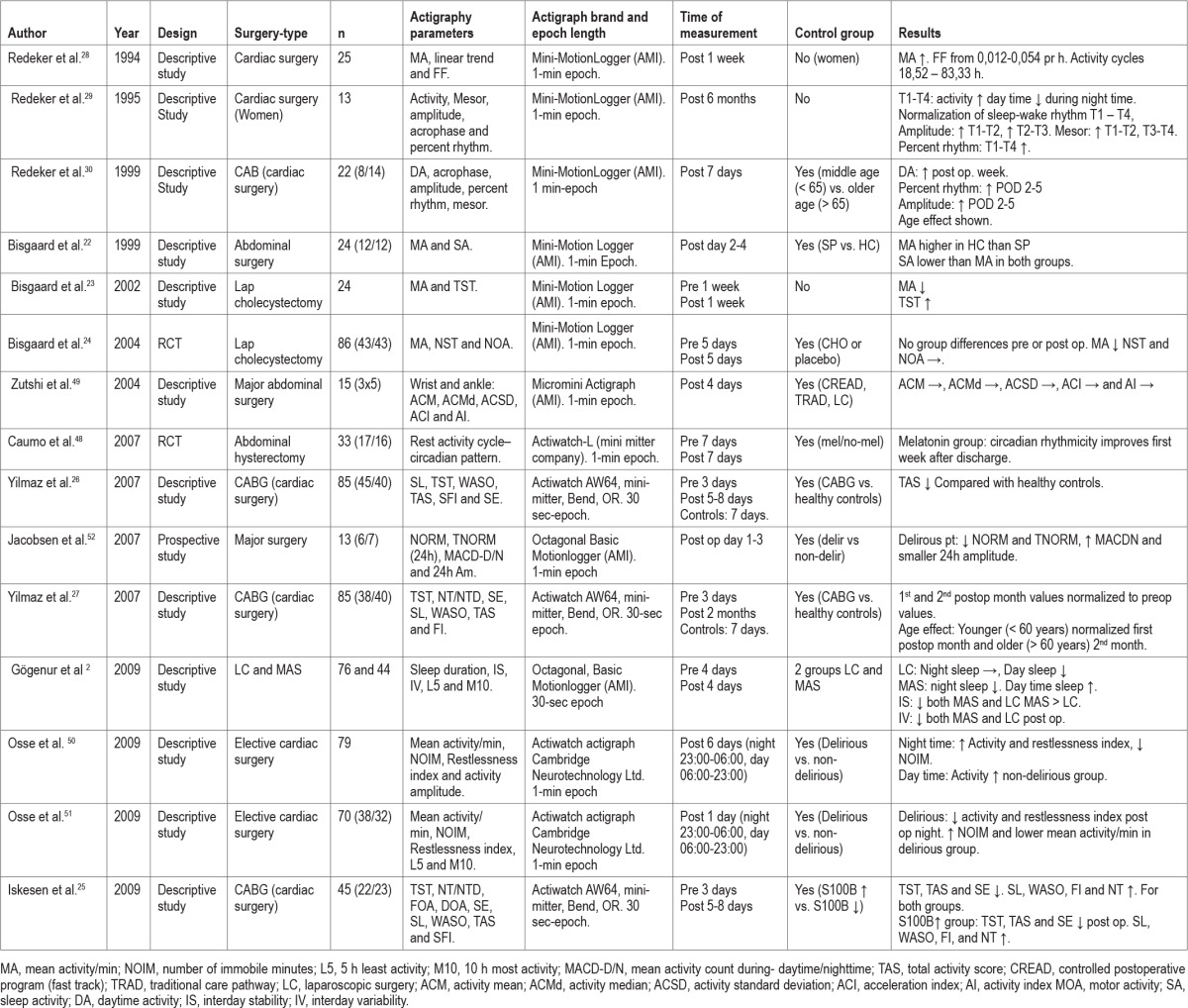
Of the 31 studies included in this review, 15 described sleep-wake rhythm or rest-activity rhythm in relation to surgery (Table 2). The sleep-wake rhythm was quantified as activity levels (mean activity count/minute) but also as mesor, acro-phase, amplitudes, and percentage rhythm. Eight of the studies included patients undergoing thoracic surgery,25–30,50,51 and 6 studies included patients undergoing general surgery.2,22–24,49,52 The last of the 15 studies involved abdominal hysterectomy and was a randomized double-blinded placebo-controlled study.48 In the 15 studies, the study population size was between 13 and 120 patients.
Table 2.
Sleep-wake rhythms
Cardiac Surgery
In studies regarding cardiac surgery, the 8 studies included patients undergoing coronary artery bypass.25–30,50,51 Only 3 of the cardiac surgery studies25–27 included measurements of pre-operative activity making pre- and post-surgery comparison possible. All 3 showed a reduction in total activity in the first postoperative week, but the values returned to normal one month postoperatively.
The rest of the studies,28–30,50,51 measured only in the postoperative period and can therefore only describe postoperative changes. In 3 of these studies,28–30 outcome measures were activity, mesor, acrophase, amplitudes, and percentage rhythm. The studies showed a tendency of increase in the mean activity in the postoperative period until the first month postoperatively. Furthermore an age effect was shown on postoperative day 4, where activity in people < 65 years increased more than in people > 65 years. The amplitude, being a measure of difference between the highest and lowest level of activity during the day, increased from the first week after surgery until 6 weeks postoperatively. The percentage rhythm, a measure of the strength of the daily rest-activity rhythm, was also improved gradually, with an increase from 32% during the first week after surgery to 49% six months postoperatively. Younger people (< 65 years) had a faster increase in amplitude and percent rhythm in the postoperative period.30 The adjusted mean of the rhythm and the mesor were increased after discharge compared with the first postoperative week in hospital.29 After a period of stagnation between the first weeks after discharge to 6 weeks postoperatively, the mesor increased again until 6 months postoperatively. Acrophase time, which represents the time of peak activity, was placed between 13:00 and 14:00, showing a small variability. Six months postoperatively, the acrophase was between 11:00 and 17:00, showing a greater variability. From the first postoperative week to one week after discharge a phase delay developed; and between 6 weeks and 6 months postoperatively a phase advance was present. In another study,28 it was shown that 14 of 25 patients who had undergone open cardiac surgery had an activity cycle of approximately 24 h; 5 had a shorter activity cycle; and 6 had a longer activity cycle.
Two studies50,51 compared patients with and without delirium, and it was shown that delirious patients had a lower level of mean activity 24 h postoperatively, with a higher number of immobile moments during the day period. In the 6-day postoperative period, both groups had increased nighttime activity and reduced number of immobile moments during the day. Patients without delirium showed a higher degree of activity during the whole 5-day postoperative period.51 Restlessness (% of time spend moving / % of immobility phases of 1 min) showed an increase in the 5-day postoperative period, with non-delirious patients having a higher increase. The number of immobile moments decreased over the 5-day postoperative period, and the non-delirious patients had a lower number than delirious patients.51
General Surgery
Six studies2,22–24,49,52 measured sleep-wake rhythm in relation to general surgery; the population size of these studies was between 13 and 120 patients. Three studies2,23,24 measured both preoperatively and postoperatively, including both minor and major abdominal surgery. Two of these studies23,24 included patients undergoing laparoscopic cholecystectomy, and they both showed a reduction in mean activity following surgery. Mean activity was reduced on postoperative day 0-1 and had normalized by postoperative day 2.
Gögenur et al.2 compared the activity rhythm in patients undergoing laparoscopic cholecystectomy with patients undergoing major abdominal surgery. Interday stability, the degree of resemblance between activity patterns of individual days, dropped after major abdominal surgery and laparoscopic surgery. However, there was a greater decrease in interday stability in the major surgery group compared with the laparoscopic group. Interday variability, a measure of the fragmentation of periods between activities at rest in a 24-h period, showed an increase in the fragmentation of the rhythm and a drop in the amplitude both after major abdominal surgery and laparoscopic surgery.
The other 3 studies22,49,52 measured only the postoperative period after major abdominal surgery. In one study,22 mean activity during the day and night was compared between patients undergoing major abdominal surgery and healthy controls. The study showed that mean activity during the day was higher in healthy controls than in the surgical patients. Another descriptive study49 of patients undergoing major abdominal surgery found no difference in activity level or trend over time between fast-track surgery, laparoscopic, and open surgical procedures. In 13 patients undergoing major abdominal surgery,52 it was shown that delirious patients had a lower number of rest minutes, higher mean activity, and smaller 24-h amplitude than non-delirious patients.
Other Surgical Procedures
In a double-blinded randomized trial of melatonin versus placebo, Caumo et al.48 measured rest-activity rhythm of patients undergoing abdominal hysterectomy. The first week after discharge, the melatonin group had a better recovery on the 24-h actigraphically determined percentile rhythm.
DISCUSSION
This review set out to give an overview of studies in surgical patients where actigraphy had been used to describe sleep and sleep-wake rhythms. Actigraphy was used in 31 studies in relation to surgery. Actigraphy was primarily used for sleep parameters and in patients undergoing cardiac or general surgery. Use of actigraphy could in the cardiac and general surgery setting demonstrate that total sleep time and sleep efficiency were reduced after surgery. No increase was shown in the number of awakenings after cardiac surgery, but the duration of the awakenings increased. After major abdominal surgery, there was an increase in both number of awakenings and wake after sleep onset, with the sleep time also being reduced at night and increased during the day.2 The impaired sleep was normalized one month after surgery, but this was not measured in the general surgical setting. In the outpatient surgery setting, use of actigraphy could demonstrate impairment of sleep, both in children39,40 and adults.41 Use of actigraphy could also be used to show that patients undergoing laparoscopic surgery had less impaired sleep than after major abdominal surgery.2 Activity measured by actigraphy could also be used to differentiate between delirious and non-delirious patients after major surgery. The effect of pharmacological interventions, such as hypnotics, different anesthetics, etc., in patients undergoing surgery could be demonstrated by measuring sleep-wake rhythms with actigraphy.
A relevant question in relation to the use of actigraphy is whether the technique has been validated against a gold standard. Actigraphy has been validated against PSG with high levels of correlation.17,21,53 For total sleep time, agreement between actigraphy and PSG has been shown to be above 90%.17,21,53 High correlation for sleep duration has also been shown in nursing home populations,17 infants,21 and people with sleep related breathing disorders.21 With regard to whole night sleep and sleep efficiency, high correlations have also been shown.20 Other sleep variables, however, have reduced validity in actigraphy measurement, e.g., sleep onset latency and wake after sleep onset.17 Generally, it is in the transition from wake-sleep or sleep-wake where the actigraphy is not precise. However, epoch-by-epoch validation has not been performed in surgical patients. Of the 31 studies included in the review, only one study22 set out to validate actigraphy. Here, activity measured by actigraphy was validated with a sleep and activity questionnaire in 12 patients undergoing major abdominal surgery and in 12 healthy controls. The study concluded that actigraphy was reliable for sleep assessment after major abdominal surgery. Further studies are needed, though, to establish epoch-by-epoch validation between actigraphy and PSG in various surgical patient groups.
The studies included in this review were heterogeneous. Several types of surgery were included, different study-designs were, used and a varying number of patients were included. It is impossible to make a randomized study of surgery vs. no surgery when investigating the effects of the surgery on sleep and sleep-wake rhythm. The next best thing is a comparison with healthy controls matched for age and sex, and this was done in five of the 31 studies.22,26,27,40,41 Also five studies2,32,46,47,49 compared different surgical procedures, three42,43,48 compared different pharmacological/anesthetic interventions, and three50,51,52 compared patients with and without postoperative delirium. In total 18/31 studies had some kind of comparison group. Thus, actigraphy was used to compare the effect of drugs, type of surgical procedure, and anesthesia in different groups of patients.
It is important to have preoperative measurements when investigating the effect of surgery. Here 19 of 31 studies measured both preoperative and postoperative values. Duration of measurement also seems important; it has been recommended to record continuous data for at least 72 hours.54 This will provide sufficient data for simple sleep variables and parametric analysis of circadian variables.15 However when nonparametric measures of activity rhythm are needed (e.g., the intradaily variability and interdaily stability), at least 7 days of continuous measurement is recommended.55 Of the studies included in this review, 24 of 31 studies used continuous measurement for at least 3 days.
The surgical trauma itself is not the only factor that can influence sleep. In a classification system used by Liao et al.,56 factors associated with sleep disturbances after heart surgery were divided into four categories: individual, physiological, psychological, and environmental factors. Individual factors are, e.g., age and gender. With regard to age, it was shown that with increasing age, sleep was severely affected and recuperation took longer compared with younger individuals.27,56 With the use of actigraphy to assess sleep, it could be shown that it took patients older than 60 years twice as long to regain a normal sleep pattern as patients younger than 60.27 Females perceived their sleep to be worse34 and had longer duration of daytime napping35 than their male comparisons. Psychological factors like depression and anxiety also may play a major role on sleep after CABG surgery and also greatly affects quality of life.56 In patients with breast cancer, intrusive thoughts and anxiety about surgery resulted in a reduced sleep efficiency and total sleep time preoperatively measured by actigraphy.44 Liao et al.56 suggested that management of pain and reduction in the influence of environmental factors (noise, light, or disruption from caretakers) were important to improve sleep quality. It was proposed that a solution could be to synchronize a given care schedule with the patient's sleep-wake rhythm and that actigraphy could be used for this purpose.
Actigraphy could be used in the perioperative period as a diagnostic tool to identify patients in need of special attention. In patients with breast cancer,45 it was shown that the low pre-operative sleep efficiency was indicative of a higher degree of postoperative pain. So sleep efficiency estimated by actigraphy preoperatively can function as a predictor of increased postoperative pain. Poor sleep the night before a stressful condition may result in a reduced immunologic response to the stressful condition.57 Identification of poor sleepers by using actigraphy could be used to identify patients with increased risk of developing sleep problems. Likewise, actigraphy could be used to identify patients with increased risk of developing severe delirium after surgery.50–52 Furthermore it was shown that patients undergoing cardiac surgery with increased S100B (measured 12 h postoperatively) had more disturbed sleep measured by actigraphy.25 Thus, coupling actigraphy measurements with, e.g., S100B measurements could enhance the possibility of finding patients in need of extra attention.
In four studies,24,42,43,48 actigraphy was used in a randomized study design, in three to evaluate sleep,24,42,43 and in one to evaluate sleep-wake pattern.48 Actigraphy was also used to evaluate a medical/pharmaceutical intervention.43 In one of the studies, two different inhalation anaesthetic agents (sevoflurane vs. halothane) were compared in children, and the study showed no difference on the measured sleep parameters.42 Bisgaard et al.24 investigated preoperative carbohydrate loading effect on postoperative recovery, and the study showed no difference between the carbohydrate loading group and the placebo group. In another study,43 brotizolam and zopiclone were compared as a preoperative hypnotics, and the actigraphy measurements showed that brotizolam was the better hypnotic with a longer total sleep time. Caumo et al.48 showed that preoperatively administered melatonin in patients undergoing hysterectomy resulted in a faster return of circadian rhythm. Thus, actigraphy is a valid tool that can be chosen to test the effect of drugs on patient's sleep or activity rhythm in relation to surgery.
In conclusion, surgery affects sleep and sleep-wake rhythm in a negative manner. With increasing surgical stress, sleep disturbances and circadian disturbances become more pronounced. The disturbances affect people of all ages, although younger age seems to facilitate a faster recovery. Studies using actigraphy in relation to surgery are heterogeneous, and the use of standardized procedures for the use of actigraphy would help with future study comparisons. Further work should strive to follow the guidelines from the American Academy of Sleep Medicine.58 In spite of this, actigraphy is a relevant tool and can be used to identify patient populations with increased risk of sleep problems in the perioperative period and can be used to measure the effect of the different surgical procedures or drugs.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work has received financial support from the Danish Medical Society of Copenhagen.
ABBREVIATIONS
- PSG
polysomnography
- S100B
plasma marker of CNS injury
DEFINITIONS
Total sleep time (TST)
Duration of the sleep episode, based on the actual time of sleep start and sleep end.
Sleep latency (SL)
Difference between time in bed and the actual time the monitored subject starts sleeping.
Mean activity (MA)
Number of movements in 1 min.
Number of awakenings (NOA)
Number of awakenings during the sleep period.
Wake after sleep onset (WASO)
Wake time in minutes after sleep onset.
Sleep efficiency (SE %)
Is the percentage of effective sleep while being in bed at night.
Intradaily variability (IV)
Quantifies the degree of resemblance between the activity patterns on individual days, ranges from 0-1.
Interdaily stability (IS)
Quantifies the fragmentation of periods of rest and activity; ranges from 0-2, with higher values indicating a more fragmented rhythm.
Mesor
Estimates the arithmetic mean of the values throughout the 24-hour period.
Amplitude
Distance from rhythmic mean to peak or trough of a mathematical model.
Percent rhythm
Percent of variance in activity accounted for by the cosinor model.
Acrophase
Time interval during which the highest values of activity are expected.
REFERENCES
- 1.Gögenur I. Postoperative circadian disturbances. Dan Med Bull. 2010;57:B4205. [PubMed] [Google Scholar]
- 2.Gögenur I, Bisgaard T, Burgdorf S, van SE, Rosenberg J. Disturbances in the circadian pattern of activity and sleep after laparoscopic versus open abdominal surgery. Surg Endosc. 2009;23:1026–31. doi: 10.1007/s00464-008-0112-9. [DOI] [PubMed] [Google Scholar]
- 3.Willich SN, Levy D, Rocco MB, Tofler GH, Stone PH, Muller JE. Circadian variation in the incidence of sudden cardiac death in the Framingham Heart Study population. Am J Cardiol. 1987;60:801–6. doi: 10.1016/0002-9149(87)91027-7. [DOI] [PubMed] [Google Scholar]
- 4.Tofler GH, Brezinski D, Schafer AI, et al. Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med. 1987;316:1514–8. doi: 10.1056/NEJM198706113162405. [DOI] [PubMed] [Google Scholar]
- 5.Belcaro G, Nicolaides AN, Geroulakos G, et al. Circadian pattern of post-surgical fatal pulmonary embolism. Vasa. 1997;26:287–90. [PubMed] [Google Scholar]
- 6.Lewis MC, Nevo I, Paniagua MA, et al. Uncomplicated general anesthesia in the elderly results in cognitive decline: does cognitive decline predict morbidity and mortality? Med Hypotheses. 2007;68:484–92. doi: 10.1016/j.mehy.2006.08.030. [DOI] [PubMed] [Google Scholar]
- 7.Ramlawi B, Rudolph JL, Mieno S, et al. Serologic markers of brain injury and cognitive function after cardiopulmonary bypass. Ann Surg. 2006;244:593–601. doi: 10.1097/01.sla.0000239087.00826.b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blask DE. Melatonin, sleep disturbance and cancer risk. Sleep Med Rev. 2009;13:257–64. doi: 10.1016/j.smrv.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Redwine L, Dang J, Hall M, Irwin M. Disordered sleep, nocturnal cytokines, and immunity in alcoholics. Psychosom Med. 2003;65:75–85. doi: 10.1097/01.psy.0000038943.33335.d2. [DOI] [PubMed] [Google Scholar]
- 10.Irwin M, Mascovich A, Gillin JC, Willoughby R, Pike J, Smith TL. Partial sleep deprivation reduces natural killer cell activity in humans. Psychosom Med. 1994;56:493–8. doi: 10.1097/00006842-199411000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Irwin M, McClintick J, Costlow C, Fortner M, White J, Gillin JC. Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. FASEB J. 1996;10:643–53. doi: 10.1096/fasebj.10.5.8621064. [DOI] [PubMed] [Google Scholar]
- 12.Mormont MC, Waterhouse J, Bleuzen P, et al. Marked 24-h rest/activity rhythms are associated with better quality of life, better response, and longer survival in patients with metastatic colorectal cancer and good performance status. Clin Cancer Res. 2000;6:3038–45. [PubMed] [Google Scholar]
- 13.Rich T, Innominato PF, Boerner J, et al. Elevated serum cytokines correlated with altered behavior, serum cortisol rhythm, and dampened 24-hour rest-activity patterns in patients with metastatic colorectal cancer. Clin Cancer Res. 2005;11:1757–64. doi: 10.1158/1078-0432.CCR-04-2000. [DOI] [PubMed] [Google Scholar]
- 14.Kanady JC, Drummond SP, Mednick SC. Actigraphic assessment of a polysomnographic-recorded nap: a validation study. J Sleep Res. 2011;20:214–22. doi: 10.1111/j.1365-2869.2010.00858.x. [DOI] [PubMed] [Google Scholar]
- 15.Calogiuri G, Weydahl A, Carandente F. Methodological issues for studying the rest-activity cycle and sleep disturbances: a chronobiological approach using actigraphy data. Biol Res Nurs. 2011 Aug; doi: 10.1177/1099800411416224. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Özturk O, Mutlu LC, Sagcan G, Deniz Y, Cuhadaroglu C. The concordance of manuel (visual) scoring and automatic analysis in sleep staging. Tuberk Toraks. 2009;57:306–13. [PubMed] [Google Scholar]
- 17.Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–92. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- 18.Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2:389–96. doi: 10.1016/s1389-9457(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 19.Berger AM, Wielgus KK, Young-McCaughan S, Fischer P, Farr L, Lee KA. Methodological challenges when using actigraphy in research. J Pain Symptom Manage. 2008;36:191–9. doi: 10.1016/j.jpainsymman.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Acebo C. Actigraphy. In: Lee-Chiong T, editor. Sleep: A Comprehensive Handbook. Hoboken, NJ: John Wiley & Sons; 2005. pp. 1035–8. [Google Scholar]
- 21.Morgenthaler T, Alessi C, Friedman L, et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30:519–29. doi: 10.1093/sleep/30.4.519. [DOI] [PubMed] [Google Scholar]
- 22.Bisgaard T, Kjaersgaard M, Bernhard A, Kehlet H, Rosenberg J. Computerized monitoring of physical activity and sleep in postoperative abdominal surgery patients. J Clin Monit Comput. 1999;15:1–8. doi: 10.1023/a:1009930026753. [DOI] [PubMed] [Google Scholar]
- 23.Bisgaard T, Klarskov B, Kehlet H, Rosenberg J. Recovery after uncomplicated laparoscopic cholecystectomy. Surgery. 2002;132:817–25. doi: 10.1067/msy.2002.127682. [DOI] [PubMed] [Google Scholar]
- 24.Bisgaard T, Kristiansen VB, Hjortso NC, Jacobsen LS, Rosenberg J, Kehlet H. Randomized clinical trial comparing an oral carbohydrate beverage with placebo before laparoscopic cholecystectomy. Br J Surg. 2004;91:151–8. doi: 10.1002/bjs.4412. [DOI] [PubMed] [Google Scholar]
- 25.Iskesen I, Kurdal AT, Yilmaz H, Cerrahoglu M, Sirin BH. Sleep disturbances after cardiac surgery with or without elevated S100B levels. Acta Cardiol. 2009;64:741–6. doi: 10.2143/AC.64.6.2044737. [DOI] [PubMed] [Google Scholar]
- 26.Yilmaz H, Iskesen I. Objective and subjective characteristics of sleep after coronary artery bypass graft surgery in the early period: a prospective study with healthy subjects. Heart Surg Forum. 2007;10:16–20. doi: 10.1532/HSF98.20061128. [DOI] [PubMed] [Google Scholar]
- 27.Yilmaz H, Iskesen I. Follow-up with objective and subjective tests of the sleep characteristics of patients after cardiac surgery. Circ J. 2007;71:1506–10. doi: 10.1253/circj.71.1506. [DOI] [PubMed] [Google Scholar]
- 28.Redeker NS, Mason DJ, Wykpisz E, Glica B, Miner C. First postoperative week activity patterns and recovery in women after coronary artery bypass surgery. Nurs Res. 1994;43:168–73. [PubMed] [Google Scholar]
- 29.Redeker NS, Mason DJ, Wykpisz E, Glica B. Women's patterns of activity over 6 months after coronary artery bypass surgery. Heart Lung. 1995;24:502–11. doi: 10.1016/s0147-9563(95)80028-x. [DOI] [PubMed] [Google Scholar]
- 30.Redeker NS, Wykpisz E. Effects of age on activity patterns after coronary artery bypass surgery. Heart Lung. 1999;28:5–14. doi: 10.1016/s0147-9563(99)70038-5. [DOI] [PubMed] [Google Scholar]
- 31.Casida JM, Davis JE, Brewer RJ, Smith C, Yarandi H. Sleep and daytime sleepiness of patients with left ventricular assist devices: a longitudinal pilot study. Prog Transplant. 2011;21:131–6. doi: 10.1177/152692481102100208. [DOI] [PubMed] [Google Scholar]
- 32.Hedges C, Redeker NS. Comparison of sleep and mood in patients after on-pump and off-pump coronary artery bypass surgery. Am J Crit Care. 2008;17:133–40. [PubMed] [Google Scholar]
- 33.Hedges C. Sleep, memory, and learning in off-pump coronary artery bypass patients. Res Nurs Health. 2005;28:462–73. doi: 10.1002/nur.20101. [DOI] [PubMed] [Google Scholar]
- 34.Redeker NS, Ruggiero J, Hedges C. Patterns and predictors of sleep pattern disturbance after cardiac surgery. Res Nurs Health. 2004;27:217–24. doi: 10.1002/nur.20023. [DOI] [PubMed] [Google Scholar]
- 35.Redeker NS, Ruggiero JS, Hedges C. Sleep is related to physical function and emotional well-being after cardiac surgery. Nurs Res. 2004;53:154–62. doi: 10.1097/00006199-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Redeker NS, Mason DJ, Wykpisz E, Glica B. Sleep patterns in women after coronary artery bypass surgery. Appl Nurs Res. 1996;9:115–22. doi: 10.1016/s0897-1897(96)80206-0. [DOI] [PubMed] [Google Scholar]
- 37.Gögenur I, Middleton B, Kristiansen VB, Skene DJ, Rosenberg J. Disturbances in melatonin and core body temperature circadian rhythms after minimal invasive surgery. Acta Anaesthesiol Scand. 2007;51:1099–106. doi: 10.1111/j.1399-6576.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- 38.Gögenur I, Middleton B, Burgdorf S, Rasmussen LS, Skene DJ, Rosenberg J. Impact of sleep and circadian disturbances in urinary 6-sulphatoxymelatonin levels, on cognitive function after major surgery. J Pineal Res. 2007;43:179–84. doi: 10.1111/j.1600-079X.2007.00460.x. [DOI] [PubMed] [Google Scholar]
- 39.Caldwell-Andrews AA, Kain ZN. Psychological predictors of postoperative sleep in children undergoing outpatient surgery. Paediatr Anaesth. 2006;16:144–51. doi: 10.1111/j.1460-9592.2005.01706.x. [DOI] [PubMed] [Google Scholar]
- 40.Kain ZN, Mayes LC, Caldwell-Andrews AA, et al. Sleeping characteristics of children undergoing outpatient elective surgery. Anesthesiology. 2002;97:1093–101. doi: 10.1097/00000542-200211000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Kain ZN, Caldwell-Andrews AA. Sleeping characteristics of adults undergoing outpatient elective surgery: a cohort study. J Clin Anesth. 2003;15:505–9. doi: 10.1016/j.jclinane.2003.02.002. [DOI] [PubMed] [Google Scholar]
- 42.Kain ZN, Caldwell-Andrews AA, Weinberg ME, et al. Sevoflurane versus halothane: postoperative maladaptive behavioral changes: a randomized, controlled trial. Anesthesiology. 2005;102:720–6. doi: 10.1097/00000542-200504000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Kawahara R, Nishimura S, Inagaki Y, Taenaka N, Kawahara H. Actigraphic assessment of the preoperative hypnotic effects of brotizolam and zopiclone. Acta Anaesthesiol Belg. 2002;53:27–31. [PubMed] [Google Scholar]
- 44.Wright CE, Bovbjerg DH, Montgomery GH, et al. Disrupted sleep the night before breast surgery is associated with increased postoperative pain. J Pain Symptom Manage. 2009;37:352–62. doi: 10.1016/j.jpainsymman.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wright CE, Schnur JB, Montgomery GH, Bovbjerg DH. Psychological factors associated with poor sleep prior to breast surgery: an exploratory study. Behav Med. 2010;36:85–91. doi: 10.1080/08964280903521305. [DOI] [PubMed] [Google Scholar]
- 46.Kim KH, Lee KA. Sleep and fatigue symptoms in women before and 6 weeks after hysterectomy. J Obstet Gynecol Neonatal Nurs. 2009;38:344–52. doi: 10.1111/j.1552-6909.2009.01029.x. [DOI] [PubMed] [Google Scholar]
- 47.Lee SY, Lee KA. Early postpartum sleep and fatigue for mothers after cesarean delivery compared with vaginal delivery: an exploratory study. J Perinat Neonatal Nurs. 2007;21:109–13. doi: 10.1097/01.JPN.0000270627.73993.b0. [DOI] [PubMed] [Google Scholar]
- 48.Caumo W, Torres F, Moreira NL, Jr., et al. The clinical impact of preoperative melatonin on postoperative outcomes in patients undergoing abdominal hysterectomy. Anesth Analg. 2007;105:1263–71. doi: 10.1213/01.ane.0000282834.78456.90. [DOI] [PubMed] [Google Scholar]
- 49.Zutshi M, Delaney CP, Senagore AJ, Fazio VW. Shorter hospital stay associated with fastrack postoperative care pathways and laparoscopic intestinal resection are not associated with increased physical activity. Colorectal Dis. 2004;6:477–80. doi: 10.1111/j.1463-1318.2004.00692.x. [DOI] [PubMed] [Google Scholar]
- 50.Osse RJ, Tulen JH, Hengeveld MW, Bogers AJ. Screening methods for delirium: early diagnosis by means of objective quantification of motor activity patterns using wrist-actigraphy. Interact Cardiovasc Thorac Surg. 2009;8:344–8. doi: 10.1510/icvts.2008.192278. [DOI] [PubMed] [Google Scholar]
- 51.Osse RJ, Tulen JH, Bogers AJ, Hengeveld MW. Disturbed circadian motor activity patterns in postcardiotomy delirium. Psychiatry Clin Neurosci. 2009;63:56–64. doi: 10.1111/j.1440-1819.2008.01888.x. [DOI] [PubMed] [Google Scholar]
- 52.Jacobson SA, Dwyer PC, Machan JT, Carskadon MA. Quantitative analysis of rest-activity patterns in elderly postoperative patients with delirium: support for a theory of pathologic wakefulness. J Clin Sleep Med. 2008;4:137–42. [PMC free article] [PubMed] [Google Scholar]
- 53.Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Med Rev. 2002;6:113–24. doi: 10.1053/smrv.2001.0182. [DOI] [PubMed] [Google Scholar]
- 54.Littner M, Kushida CA, Anderson WM, et al. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep. 2003;26:337–41. doi: 10.1093/sleep/26.3.337. [DOI] [PubMed] [Google Scholar]
- 55.Van Someren EJ, Lijzenga C, Mirmiran M, Swaab DF. Long-term fitness training improves the circadian rest-activity rhythm in healthy elderly males. J Biol Rhythms. 1997;12:146–56. doi: 10.1177/074873049701200206. [DOI] [PubMed] [Google Scholar]
- 56.Liao WC, Huang CY, Huang TY, Hwang SL. A systematic review of sleep patterns and factors that disturb sleep after heart surgery. J Nurs Res. 2011;19:275–88. doi: 10.1097/JNR.0b013e318236cf68. [DOI] [PubMed] [Google Scholar]
- 57.Wright CE, Erblich J, Valdimarsdottir HB, Bovbjerg DH. Poor sleep the night before an experimental stressor predicts reduced NK cell mobilization and slowed recovery in healthy women. Brain Behav Immun. 2007;21:358–63. doi: 10.1016/j.bbi.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 58.Morgenthaler T, Alessi C, Friedman L, et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30:519–29. doi: 10.1093/sleep/30.4.519. [DOI] [PubMed] [Google Scholar]
- 59.Natalem V, Plazzi G, Martoni M. Actigraphy in the assessment of insomnia: a quantitative approach. Sleep. 2009;32:767–71. doi: 10.1093/sleep/32.6.767. [DOI] [PMC free article] [PubMed] [Google Scholar]