Abstract
PURPOSE
Hypertension is the most common diagnosis in ambulatory care, yet little evidence exists regarding recommended screening intervals or the sensitivity and specificity of a routine office-based blood pressure measurement, the most common screening test. Screening for hypertension is usually performed by measuring blood pressure at every outpatient visit, which often results in transiently elevated findings among adults who do not have a diagnosis of hypertension. We hypothesize that a more limited annual screening strategy may increase specificity while maintaining sensitivity.
METHODS
A retrospective case-control study of 372 adults without hypertension and 68 patients with newly diagnosed hypertension was conducted to compare the usual screening practice of checking blood pressure at every visit with a second strategy that considered only annual blood pressure measurements.
RESULTS
Specificity improved from 70.4% (95% CI, 65.5%-75.0%) for the usual practice to 82.0% (95% CI, 77.7%-85.8%) for the annual screening strategy. No statistically significant difference in sensitivity existed between the 2 methods.
CONCLUSION
A limited annual screening strategy for hypertension can improve specificity without sacrificing sensitivity when compared with routine screening at every visit in previously normotensive adults.
Key words: hypertension, blood pressure, blood pressure determination, preventive health services, sensitivity and specificity, mass screening
INTRODUCTION
Hypertension is the most common diagnosis for which patients seek ambulatory care in the United States, representing more than 42 million visits in 2007.1 Yet there is little evidence to recommend a screening interval2 or to define the sensitivity and specificity of the most common screening test, a routine office-based blood pressure measurement performed by manual sphygmomanometry. There is universal agreement among major national primary care organizations, including The Joint National Committee on Prevention, Detection and Treatment of Hypertension (JNC-7), the United States Preventative Service Task Force (USPSTF), the American Academy of Family Physicians, and the American College of Physicians on the utility of screening for hypertension.2–4 JNC-7 recommends a 2-year screening interval for normotensive individuals (systolic blood pressure less than 120 mm Hg and diastolic blood pressure less than 80 mm Hg) and a 1-year interval for individuals with prehypertension (systolic blood pressure of 120-139 mm Hg or diastolic blood pressure of 80-89 mm Hg), but it does not cite any references for these recommendations.3 The USPSTF mentions the JNC-7 recommendations regarding screening intervals but states, “the optimal interval for screening adults for hypertension is not known.”2
Throughout the country, many primary care clinics routinely screen for hypertension by checking blood pressures at every clinic encounter regardless of the patient’s chief complaint, previous blood pressures, or the interval since the last blood pressure was obtained. Even so, an estimated 30% of individuals with hypertension are unaware they have the disease.3 According to JNC-7, a diagnosis of hypertension requires “the average of 2 or more properly measured, seated, blood pressure readings on each of 2 or more office visits.”3 It is well known that clinic blood pressures tend to be higher than ambulatory blood pressures, the so-called white coat effect.5–8 In addition, clinic blood pressures are often not taken according to JNC-7 specifications, leading to inaccurate and often elevated results.9,10 These factors, plus patient factors of acute pain, illness, or anxiety, make interpreting clinic blood pressure values as a screening test for hypertension difficult.
With Americans making an average 3.2 medical office visits per year and the majority of these occurring in primary care,1,12 there is ample opportunity to design a better, more limited screening strategy for hypertension that meets JNC-7’s recommendations.3 This pilot study compares the current clinical practice of screening for hypertension by checking every patient’s blood pressure at every visit vs a more limited strategy that screens for hypertension annually.
METHODS
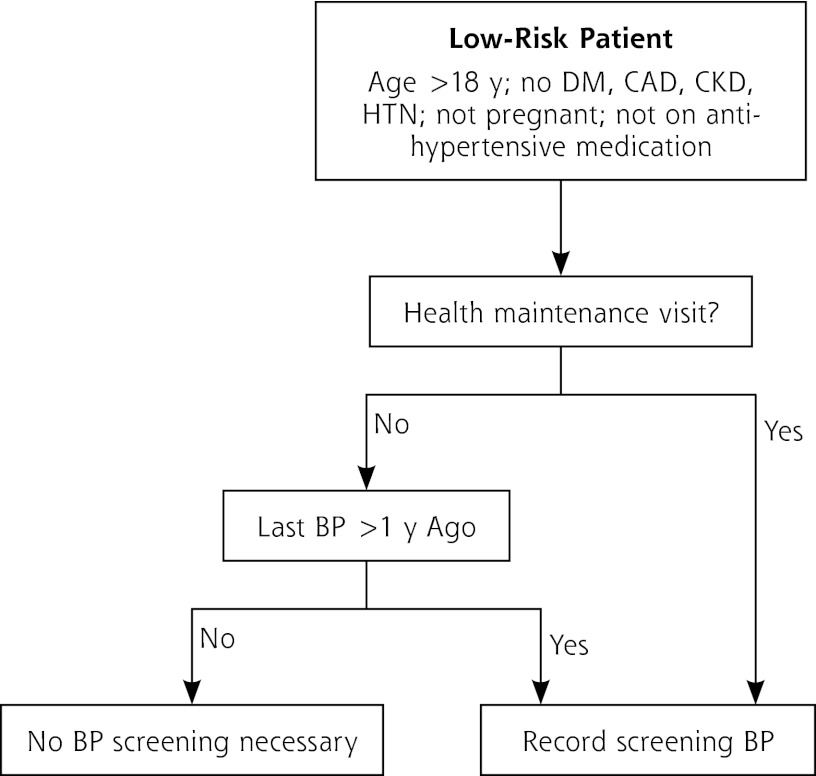
We compared 2 screening strategies for low-risk patients. The first strategy is the usual clinical practice of measuring a patient’s blood pressure at every visit. Because we hypothesized that a limited annual screening strategy would increase specificity while maintaining sensitivity, we simulated a second strategy by considering blood pressures obtained only at general medical examination visits and any other visit when it had been more than 1 year since the last blood pressure measurement was obtained (Figure 1).
Figure 1.
Proposed limited annual screening algorithm for hypertension.
BP = blood pressure; CAD = coronary artery disease; CKD = chronic kidney disease; DM = diabetes mellitus; HTN = hypertension.
To compare the screening strategies, we conducted a retrospective study for the 5 years preceding August 1, 2010. Subjects were family medicine patients at Mayo Clinic Rochester who were aged 18 to 75 years at the start of the study period, were not pregnant, remained active patients for the entire 5 years, and had at least 1 office blood pressure recorded during the study period. We excluded patients with type 1 or 2 diabetes, coronary artery disease, or stage 3 or 4 chronic kidney disease because of the differing standards for treatment of blood pressure in these individuals. Additionally, because of the effect on blood pressure, we excluded patients taking any antihypertensive medications for migraine prophylaxis, peripheral edema, or other reasons at any point during the study period before a diagnosis of hypertension. All patients had signed a research authorization allowing retrospective review of their electronic medical record. The study was reviewed and approved by our Institutional Review Board.
We used an administrative database containing International Classification of Disease (ICD-9) billing codes for the past 16 years to construct pools of patients with hypertension diagnosed during the study period and patients who did not have hypertension based on the inclusion and exclusion criteria defined previously. We looked for patients never having an ICD-9 code 401.x (hypertension) before the start of the study and who were subsequently given an ICD-9 code 401.x during the study period, as well as patients who never had an ICD-9 code 401.x.
We randomly selected 236 patients who received a diagnosis of hypertension during the study period and 500 normotensive patients using the SAS procedure survey select (SAS 9.2 , SAS Institute Inc). We screened for antihypertensive medication use with a computerized text-matching algorithm, and the investigators conducted a manual chart review of all patients.
We entered data from all study patients regarding blood pressure values at various outpatient visits, medications, and demographics into a relational database (PostgreSQL 8.3, PostSQL Global Development Group, running on Mac OS 10.7.3). The great majority of blood pressure measurements were obtained by a licensed practical nurse using a calibrated aneroid device.
Statistical analysis was carried out using R 2.15.0 statistical software (http://cran.r-project.org/src/base/R-2/R-2.15.0.tar.gz) running on Mac OS 10.7.3. Patients with diagnosed hypertension and patients in the group with no hypertension were compared using Fisher’s exact test for categorical data and t tests for numerical data. P values of less than .05 were considered significant. Sensitivity and specificity, including 95% confidence intervals, were calculated for each screening strategy using the patient as the unit of analysis. Any blood pressure of 140 mm Hg systolic or 90 mm Hg diastolic or greater was considered a positive screening test. A physician’s diagnosis of hypertension was considered the reference standard for positive disease. Assuming a sensitivity of 95% and a specificity of 75%, with desired 95% confidence intervals of 5%, it was estimated 73 patients with diagnosed hypertension and 288 patients without hypertension would be needed.
RESULTS
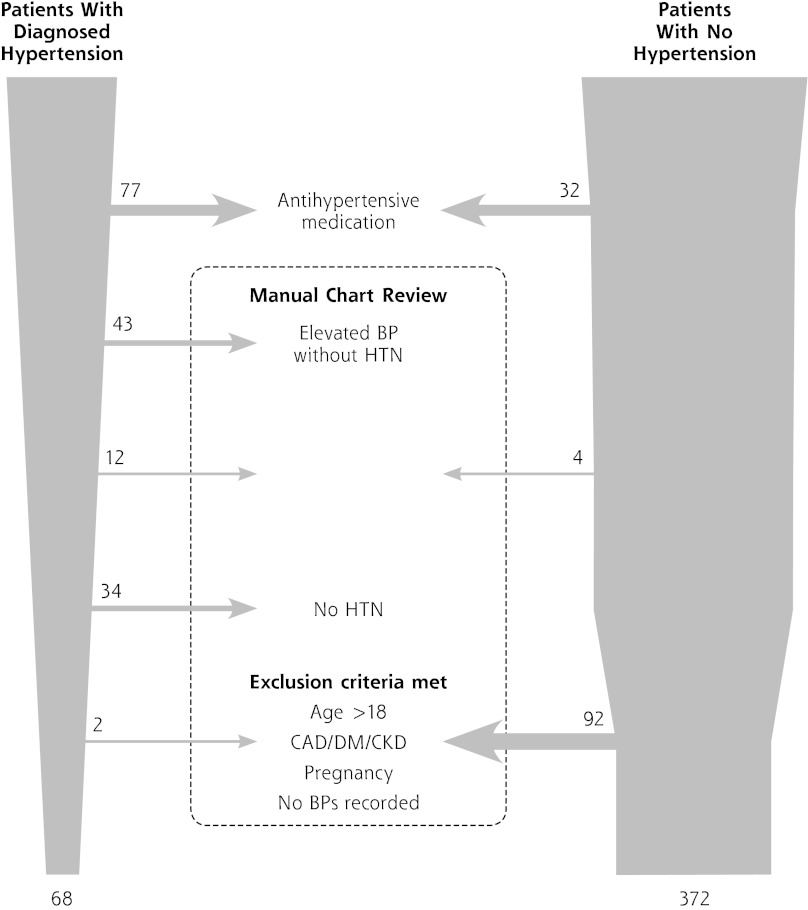
As is typical for administrative or billing databases,13,14 there were substantial differences from the actual clinical notes among the 236 potential patients with hypertension diagnosed during the study period and the 500 potential patients without hypertension. For instance, 43 patients in the hypertension group had a diagnosis of elevated blood pressure without hypertension that was mistakenly coded as ICD-9 code 401.x; 34 patients never had a diagnosis of hypertension but mistakenly were given an ICD-9 401.x billing code, often during a procedure or hospitalization; and 12 patients in the hypertension group and 4 patients in the group with no hypertension were found to have a clinical diagnosis of hypertension before the start of the study that was not recorded as a ICD-9 401.x billing code in the administrative database (Figure 2).
Figure 2.
Case and control selection.
After elimination of the miscoded patients, we analyzed data from 68 patients with hypertension diagnosed during the 5-year study period and 372 patients with no hypertension during the same period. These 440 patients had 4,287 blood pressures recorded. Sex and smoking status did not differ between those with hypertension and those with no hypertension. The number of visits per patient per year was also similar, with the patients with hypertension averaging 2.5 (SD = 2.8) visits per year and the patients with no hypertension averaging 1.9 (SD = 1.3) visits per year (P = .096). Patients with hypertension were older than patients with no hypertension (47.6 years, SD = 10.4 years vs 41.2 years, SD = 12.7 years, respectively; P <.001) and heavier (body mass index 33.6 kg/m2, SD = 6.8 vs 28.6 kg/m2, SD = 8.7 kg/m2, respectively; P <.001). As expected, average blood pressures were higher in the patients with hypertension than the patients with no hypertension. Table 1 summarizes these results.
Table 1.
Demographic Information on Patients With Diagnosed Hypertension and Patients With No Hypertension
| Characteristic | Hypertension (n = 68) |
No Hypertension (n = 372) |
P Value |
|---|---|---|---|
| Sex, No. (%) | >.999 | ||
| Male | 33 (48.5) | 179 (48.1) | |
| Female | 35 (51.5) | 193 (51.9) | |
| Age, year (SD) | 47.6 (10.4) | 41.2 (12.7) | <.001 |
| BMI, kg/m2 (SD) | 33.6 (6.8) | 28.6 (8.7) | <.001 |
| Smoking status, No. (%) | .530 | ||
| Never | 28 (66.7) | 83 (58.9) | |
| Quit | 11 (26.2) | 40 (28.3) | |
| Current | 3 (7.1) | 18 (12.8) | |
| Visits per year, No. (SD) | 2.5 (2.8) | 1.9 (1.3) | .096 |
| Average blood pressure | |||
| Systolic, mm Hg (SD) | 135.3 (11.1) | 114.7 (11.4) | <.001 |
| Diastolic, mm Hg (SD) | 82.7 (6.7) | 70.1 (7.5) | <.001 |
BMI = body mass index.
The screening strategy of checking blood pressures at every visit identified all 68 patients with hypertension diagnosed during the study period who had at least 1 positive screening blood pressure higher than 140/90 mm Hg, consistent with the criteria for diagnosis. There were, however, 110 (29.6%) patients in the group with no hypertension who were found to have at least 1 blood pressure measurement higher than 140/90 mm Hg during the study period. In fact, 266 of 3,299 (8.1%, 95% CI, 7.2%-9.0%) blood pressures obtained in this group were at or higher than 140/90 mm Hg. Usual practice, as expected, had identified 100% of patients with diagnosed hypertension (sensitivity 100%, 95% CI, 92.2%-100%), with a specificity of 70.4% (95% CI, 65.5%-75.0%).
The annual screening strategy retained 39.3% (1,686) of the 4,287 blood pressures obtained during the study period. This method found the same rate of elevated blood pressures among the retained readings from patients with no hypertension, with 106 of 1,373 (7.7%, 95% CI, 6.4%-9.3%; P = .692) with blood pressures at or higher than 140/90 mm Hg. Screening less frequently resulted in only 67 patients in the group (18.0%) with no hypertension having elevated blood pressures. The annual screening strategy failed, however, to identify 5 (7.4%) patients with hypertension on or before the date of their original diagnosis. This method yielded a sensitivity of 92.6% (95% CI, 83.7%-97.6%) and a specificity of 82.0% (95% CI, 77.7%-85.8%). Table 2 contrasts the results obtained by both methods.
Table 2.
Sensitivity and Specificity of Blood Pressure Screening Strategies
| Strategy | Hypertension
|
Sensitivity, % (95% CI) | Specificity, % (95% CI) | |
|---|---|---|---|---|
| Yes (Cases) | No (Controls) | |||
| Typical practice (all visits) | ||||
| Positive | 68 | 110 | 100 (92.2-100) | 70.4 (65.5-75.0) |
| Negative | 0 | 262 | ||
| Limited strategy (annual screening) | ||||
| Positive | 63 | 67 | 92.6 (83.7-97.6) | 82.0 (77.7-85.8) |
| Negative | 5 | 305 | ||
DISCUSSION
Hypertension screening is an important part of preventive health care delivered by primary care physicians. It is essential to understand the implications of a screening test’s characteristics to interpret results and design a screening strategy effectively. This initial pilot study proposes an annual screening strategy for hypertension using the most common screening test, the office-based manual blood pressure measurement, which improves specificity while maintaining sensitivity.
Sensitivity
An objective of any screening strategy is to classify correctly those individuals with hypertension. Sensitivity describes a test’s ability to classify correctly those with disease (Table 3). With a highly sensitive test, the false-negative or type 2 error rate is negligible. Thus, a negative result tends to rule out the possibility of disease.15
Table 3.
A 2 × 2 Table for Screening Tests for Hypertension
| Elevated Screening Blood Pressure | Yes | No |
|---|---|---|
| Yes | True positive | False positive (type I error) |
| No | False negative (type II error) | True negative |
| Sensitivity |
As expected, the baseline practice of checking blood pressure at every visit yielded 100% sensitivity. The proposed annual screening strategy failed to identify 7.4% of newly hypertensive patients as quickly as the baseline strategy. This difference was not significant, as the 95% confidence intervals overlapped. Given the slowly progressive nature of morbidity resulting from hypertension,16 whether this delay in diagnosis is clinically relevant is debatable. In this study, we could not consider visits that occurred after a diagnosis of hypertension was made, as treatment would affect these blood pressure values. Thus it was impossible to ascertain whether and when these patients would have had hypertension diagnosed using the proposed annual screening strategy. Considering that hypertensive patients had an average of 2.5 visits per year, the delay is unlikely to be more than a few months.
Specificity
Specificity describes a test’s ability to correctly classify those without disease (Table 3). With a highly specific test the false-positive or type I error rate is minimal. A positive result therefore rules in a disease.15 If large numbers of disease-free individuals are screened repeatedly, then even highly specific tests can generate unwieldy numbers of false-positive results, for which patients must undergo further testing.
This study found that the baseline practice of screening for hypertension by checking blood pressures at every office visit has a poor sensitivity of 70.4%. During the 5-year study period, 29.6% of adults who never had hypertension diagnosed had at least 1 elevated blood pressure reading. These elevated readings can lead to follow-up visits, laboratory testing, and patient anxiety, or as in “The Shepherd’s Boy and the Wolf,”11 they can lull the physician into a sense of complacency, delaying the diagnosis of actual hypertension.
One way to compensate for a screening test’s poor specificity is to target a limited population for screening; however, JNC-7 recommendations clearly indicate the need to screen all adults for hypertension.3
In slowly progressive diseases, another way to compensate for poor specificity is to reduce the frequency of screening.17 Obviously, clinical considerations come into play as the screening needs to occur frequently enough to detect the disease in its earliest stages, when it is easily treated and before morbidity develops. Mild to moderate hypertension is a slowly progressive chronic disease that causes complications and target organ damage over the course of years.16 Given a test with high sensitivity but poor specificity, such as office blood pressure screening, performing it too frequently increases false-positive results but does not improve disease detection.
Less frequent screening is the tactic applied by our proposed annual screening strategy. It reduced the number of screenings performed by 60.7%. The reduced frequency of screening produced a significant decrease in the false-positive rate from 29.6% to 18.0% of nonhypertensive adult patients over a 5-year period. Applied to the roughly 2,000 healthy adults cared for by a typical family physician, it results in 232 fewer patients needing further workup over 5 years.
Reducing the number of unnecessary blood pressures screenings in healthy adults provides benefits in addition to improving the false-positive rate. It can increase clinic efficiency, reduce clerical burdens, and focus attention on accurately obtaining screening blood pressure measurements. JNC-7 specifies that an accurate blood pressure measurement should be the mean of 2 auscultatory readings taken with an appropriately sized cuff with the patients’ feet on the floor and arm supported at heart height after being seated quietly in a chair for 5 minutes.3 In the typical busy family medicine clinic with 15-minute appointments, there is no time for this method for every patient at every visit.6,18 Instead, patients are all too often rushed down the hallway from a waiting room, and a blood pressure is immediately measured. Reducing the frequency of screening blood pressures may allow clinical staff time to measure blood pressures more accurately. For instance, oscillometric devices, such as the BpTRU (BpTRU Medical Devices), that take multiple readings over several minutes may be used.19
Limitations
Identifying patients with newly diagnosed hypertension by ICD-9 codes proved problematic. Manual chart review revealed substantial inaccuracies leading to fewer patients than originally forecast, which limited the study’s ability to detect differences in sensitivity between the 2 methods. The fewer patients did not affect the study’s primary aim of detecting differences in specificity, however.
Determining a group of patients with no hypertension was also problematic. This study used a 5-year time frame to look for the development of hypertension, and thus we do not know what happens in the future to patients who did not have hypertension diagnosed but who had elevated blood pressures. Do they go on later in life to develop hypertension? Additionally, we did not design our study to examine the effect that our proposed screening strategy might have on morbidity from hypertension. Further studies with longer time frames and other endpoints are required to answer these questions.
The proposed annual screening for hypertension (in line with selection criteria for blood pressure measurements in this analysis) would entail measuring blood pressure for each patient at all preventive care visits or if it had been at least 1 year since the last blood pressure measurement. This simplistic approach makes the algorithm easy to understand and implement, but it may overlook other important clinical factors.
Age and body mass index are well-established risk factors for hypertension,20,21 and the observed differences between patients with diagnosed hypertension and patients with no hypertension are not surprising. Such differences did not affect our sensitivity and specificity analysis.
The choice of a physician diagnosis of hypertension as the reference standard for disease may underestimate its prevalence in the study population.3 JNC-7 provides a definition for hypertension as “the average of 2 or more properly measured, seated blood pressure readings on each of 2 or more office visits.”3 Unfortunately, very few routinely obtained, office-based blood pressure measurements meet the requirements of this definition.9,10 Thus using the JNC-7 definition as the reference standard for hypertension in this study was impractical, as there was no guarantee that the retrospectively obtained blood pressures met the rigorous requirements. Although a limitation, it is not necessarily a weakness, because the purpose of this study was to investigate the screening utility of routinely obtained typical office-based blood pressure measurements, which do not always meet the strict JNC-7 requirements.
Finally, there is a distinction between obtaining a blood pressure reading for hypertension screening purposes and obtaining a blood pressure reading because it is clinically relevant. There are many clinical scenarios, such as chest pain, palpitations, lightheadedness, and severe infections, where obtaining a blood pressure measurement is necessary to guide diagnosis and treatment decisions, but the purpose is not to screen for hypertension. This study does not suggest that these blood pressures should not be obtained; only that they should be interpreted cautiously when diagnosing hypertension.
Acknowledgments
We would like to thank Melissa Gregg and Julie Maxson for their assistance with data collection. Without their expertise, this study would not have been possible.
Footnotes
To read or post commentaries in response to this article, see it online at http://www.annfammed.org/content/11/2/116.
Funding support: Funding was provided by Mayo Clinic Department of Family Medicine.
References
- 1.Hsiao CJ, Cherry DK, Beatty PC. National Ambulatory Medical Care Survey: 2007 Summary. National health statistics reports; no 27. Hyattsville, MD: National Center for Health Statistics; 2010. http://www.cdc.gov/nchs/data/nhsr/nhsr027.pdf [PubMed] [Google Scholar]
- 2.U.S. Preventive Services Task Force Screening for high blood pressure: U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2007;147(11):783–786 [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572 [DOI] [PubMed] [Google Scholar]
- 4.US Preventive Services Task Force Screening for high blood pressure: reaffirmation and recommendation statement. Am Fam Physician. 2009;79(12):1087–1088 [Google Scholar]
- 5.Zakopoulos NA, Kotsis VT, Pitiriga VCh, et al. White-coat effect in normotension and hypertension. Blood Press Monit. 2002;7(5): 271–276 [DOI] [PubMed] [Google Scholar]
- 6.Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension. 2010;55(2):195–200 [DOI] [PubMed] [Google Scholar]
- 7.Myers MG, Oh PI, Reeves RA, Joyner CD. Prevalence of white coat effect in treated hypertensive patients in the community. Am J Hypertens. 1995;8(6):591–597 [DOI] [PubMed] [Google Scholar]
- 8.Myers MG, Godwin M, Dawes M, et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. BMJ. 2011;342:d286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Villegas I, Arias IC, Botero A, Escobar A. Evaluation of the technique used by health-care workers for taking blood pressure. Hypertension. 1995;26(6 Pt 2):1204–1206 [DOI] [PubMed] [Google Scholar]
- 10.Kay LE. Accuracy of blood pressure measurement in the family practice center. JABFM. 1998. 11(4):252–258 [DOI] [PubMed] [Google Scholar]
- 11.Townsend GF, ed. Aesop’s Fables. Amazon Digital; 2008 [Google Scholar]
- 12.FastStats Ambulatory care use and physician visits. Centers for Disease Control and Prevention website. 2012. http://www.cdc.gov/nchs/fastats/docvisit.htm Accessed May 29, 2012
- 13.Li L, Chase HS, Patel CO, Friedman C, Weng C. Comparing ICD9-encoded diagnoses and N LP-processed discharge summaries for clinical trials pre-screening: a case study. AMIA Annu Symp Proc. 2008:404–408 [PMC free article] [PubMed] [Google Scholar]
- 14.Quan H, Khan N, Hemmelgarn BR, et al. Hypertension Outcome and Surveillance Team of the Canadian Hypertension Education Programs Validation of a case definition to define hypertension using administrative data. Hypertension. 2009;54(6):1423–1428 [DOI] [PubMed] [Google Scholar]
- 15.Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2nd ed Boston, MA: Little, Brown; 1991 [Google Scholar]
- 16.Zanchetti A. Target organ damage in hypertension. J Cardiovasc Risk. 1995;2(1):1–3 [PubMed] [Google Scholar]
- 17.Thompson SG, Ashton HA, Gao L, Scott RA, Multicentre Aneurysm Screening Study Group Screening men for abdominal aortic aneurysm: 10 year mortality and cost effectiveness results from the randomised Multicentre Aneurysm Screening Study. BMJ. 2009;338: b2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sala C, Santin E, Rescaldani M, Magrini F. How long shall the patient rest before clinic blood pressure measurement? Am J Hypertens. 2006;19(7):713–717 [DOI] [PubMed] [Google Scholar]
- 19.Graves JW, Nash C, Burger K, Bailey K, Sheps SG. Clinical decision-making in hypertension using an automated (BpTRU) measurement device. J Hum Hypertens. 2003;17(12):823–827 [DOI] [PubMed] [Google Scholar]
- 20.Buck CW, Donner AP./ Factors affecting the incidence of hypertension. CMAJ. 1987;136(4):357–360 [PMC free article] [PubMed] [Google Scholar]
- 21.Wang W, Lee ET, Fabsitz RR, et al. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: the Strong Heart Study. Hypertension. 2006;47(3):403–409 [DOI] [PubMed] [Google Scholar]