Abstract
Aim
To evaluate the effects of inferior oblique muscle recession (IOR) in cases of laterally incomitant hypertropia <10 prism dioptres (PD) in central gaze thact 2t are clinically consistent with superior oblique palsy (SOP).
Methods
We retrospectively reviewed patients with SOP and hypertropias <10 PD in central gaze who underwent graded IOR. Primary outcomes were reduction of lateral incomitance and number of overcorrections in central gaze.
Results
Twenty-five patients were included. Mean follow-up was 13.8 months (range 1.4–66). Mean central gaze hypertropia decreased from 5.6±2.1 to 0.2±1.6 PD (p<0.001). Contralateral gaze hypertropia decreased from 15.9±7.6 to 2.3±3.3 PD (p<0.001). Lateral incomitance (central vs contralateral gaze) was 10.3±6.9 PD preoperatively and 2.0±3.0 PD postoperatively (p<0.001). There were two patients overcorrected in central gaze, and one patient overcorrected in downgaze. One patient necessitated further surgery for overcorrection.
Conclusions
Although small hypertropias can be treated with prisms or small, adjustable inferior rectus recessions, IOR collapses incomitance without causing much overcorrection. IOR is a reasonable treatment for small, laterally incomitant hypertropia due to SOP.
INTRODUCTION
Multiple surgical options exist for the treatment of hypertropia resulting from presumed superior oblique palsy (SOP). The surgical plan depends on the deviation in central gaze, the amount of over elevation in adduction, the degree of under depression in adduction and pattern of comitance.1–3 Many studies have evaluated the effects of inferior oblique surgery on hypertropias.4–6 Inferior oblique recession (IOR) is a well accepted surgery for patients with SOP who exhibit over elevation in adduction.4,7–14 Recession of the inferior oblique muscle (IO) was argued by Parks to be the most effective and long lasting of the IO weakening procedures.7 Anatomical studies in the 1970s introduced new tables for graded recessions.15 It has been claimed that 8–10 mm IOR corrects 9–15 prism dioptres (PD) central gaze hypertropia.8–10 Recently, Metten et al14 published dose-response for IOR of 0.5°/mm recession in central gaze, and up to 1.4°/mm in adduction. Depending on vertical deviation in central and lateral gazes, it may be necessary to combine IOR with another procedure such as contralateral inferior rectus recession (IRR), ipsilateral superior rectus recession or ipsilateral SO tuck.8,9,16 Although overcorrection is uncommon with IOR,13,17 there is concern about overcorrection when central gaze hypertropia is small due to the non-adjustable nature of the procedure. For this reason, surgeons may opt to treat patients who have small hypertropia with prisms or with a contralateral IRR, which can be performed as an adjustable procedure. This alternative surgery however, may in itself cause overcorrections as well as instability with recurring hypertropia.18–20 IRR is not expected to effectively address the horizontal incomitance found in SOP. In addition, IRR alone may not sufficiently address coexisting excyclotropia.21
In this study, we evaluated effects of IOR in laterally incomitant hypertropia <10 PD in central gaze and clinically consistent with SOP. Our goal was to determine the incidence of postoperative overcorrections and the effect of surgery on lateral incomitance.
METHODS
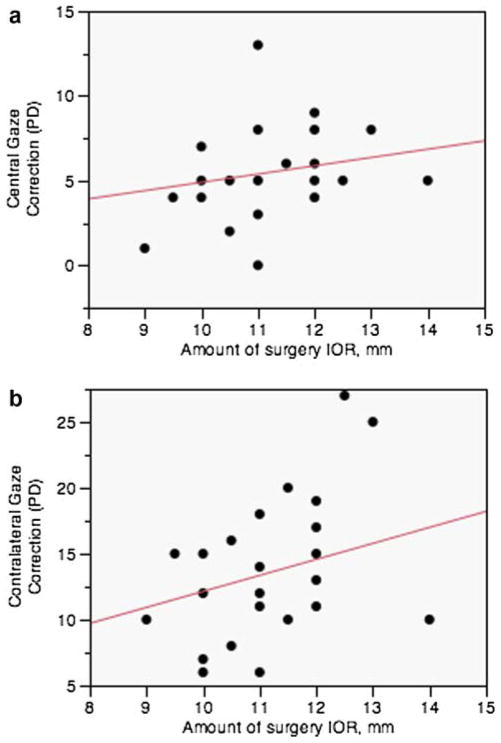
This study was approved by the University of California Los Angeles Institutional Review Board and conformed to the requirements of the US Health Insurance Portability and Accountability Act. This was a retrospective review of patients with 3-step testing compatible with SOP who presented with central gaze hypertropia <10 PD who underwent graded IOR between the years 1992–2011. A minimum follow-up time of 6 weeks was required for inclusion in the study. The study excluded patients who had surgery on another vertical muscle at the same time as IOR, and patients who had previous strabismus surgery. All of the IORs were performed using fixed sutures. IOR was graded such that a 14 mm recession was when the IO was sutured to the sclera 5 mm posterior to the insertion of the inferior rectus (IR). For each mm of recession less than 14 mm, the IO was sutured to the sclera an additional 1 mm lateral to the IR (figure 1).
Figure 1.
Graded inferior oblique recession. Grading of inferior oblique recession by 1 mm increments from a 14 mm recession which is at the temporal inferior rectus (IR) border 5 mm posterior to the IR insertion. This figure is only reproduced in colour in the online version.
The following characteristics were recorded from the patients’ records: age at surgery, amount of surgery, aetiology, visual acuity, motor alignment in primary and secondary gaze positions at distance and near, versions, stereoacuity and torsion. Stereoacuity was tested with the Titmus fly test, and torsion was tested with double Maddox rods. A patch was placed over one eye for 30 min and alignment was then re-examined due to the small deviation in primary gaze. All measures were recorded at the preoperative visit, 1 day postoperative visit and final visit. The final visit was either the last documented visit in the patient’s chart, or the last visit before a reoperation. Primary outcomes were reduction of lateral incomitance after surgery and the number of postoperative overcorrections, defined as any deviation opposite the original deviation. Undercorrection was defined as any residual hypertropia.
Statistical analyses were performed using Microsoft Excel (Microsoft Corporation, Redmond, Washington, USA), and analysis of variance. Student’s t-test was used to compare differences of means, with 0.05 considered statistically significant. Linear regression analysis was performed for dose response forced through zero assuming that no surgery would yield zero effect.
RESULTS
Twenty-five patients with SOP who underwent graded IOR were included in this study. Mean follow-up was 13.8 months (range, 1.4–66). Characteristics of these patients are shown in table 1. The preoperative hypertropia in primary and secondary positions and at near, and postoperative correction are shown in table 2. Mean central gaze hypertropia decreased from (mean ± SD) 5.6±2.1 to 0.2±1.6 PD (p<0.001). Mean contralateral gaze hypertropia decreased from 15.9±7.6 to 2.3±3.3 PD (p<0.001). For both groups, the differences between preoperative and final visit measurements in all gazes were statistically significant (p<0.05). Torsion significantly decreased by 4.6±3.1° (p<0.001). There was an overall mean postoperative correction (preoperative to final) of 5.4±2.7 PD in central gaze, and 13.6±5.7 PD in contralateral gaze. Lateral incomitance (central vs contralateral gaze) decreased from 10.3±6.9 PD pre-operatively to 2.0±3.0 PD postoperatively (p<0.001). There was no statistically significant change in the mean deviation in any gaze position from the first postoperative visit to the final visit.
Table 1.
Characteristics of patients
| Number of patients | 25 |
|---|---|
| Age at surgery, mean (years ± SD, range) | 34.6 ± 25.3 (1.7–82) |
| Amount of surgery, mm (range) | 11.2 ± 1.2 (9–14) |
| Follow-up (months ± SD, range) | 13.8 ± 17.2 (1.4–66) |
| Laterality OD/OS (# of patients) | 9/16 |
| Concurrent horizontal surgery (n) | 2 |
OD, right eye; OS, left eye.
Table 2.
Preoperative vertical deviation and postoperative correction
| Hypertropia PD mean ± SD (range) | IOR preop | IOR correction | p Value (preop/final visit) |
|---|---|---|---|
| Central | 5.6 ± 2.1 (0–8) | 5.4 ± 2.7 (0–13) | <0.001 |
| Contralateral | 15.9 ± 7.6 (6–35) | 13.6 ± 5.7 (6–27) | <0.001 |
| Ipsilateral | 1.5 ± 1.9 (0–6) | 1.6 ± 2.6 (−1–10) | 0.02 |
| Upgaze | 7.1 ± 3.6 (0–16) | 7.4 ± 4.5 (0–15) | 0.004 |
| Downgaze | 3.3 ± 3.2 (0–12) | 2.4 ± 3.4 (−2–12) | <0.001 |
| Near | 3.7 ± 3.4 (0–12) | 3.1 ± 2.8 (0–8) | 0.001 |
| Excyclotropia (°) | 7.7 ± 2.5 (4–12) | 4.6 ± 3.1 (−1–8) | 0.001 |
IOR, inferior oblique recession; PD, prism dioptre; Correction, amount of change in deviation from the preoperative visit exam to the final visit exam.
Nineteen of 25 patients (76%) were orthotropic in central gaze at final exam, two patients (8%) were overcorrected, and four patients (16%) were undercorrected all by <4 PD. In a subanalysis of patients who had a preoperative central gaze deviation of ≤5 PD (n=13), there were no overcorrections in central gaze.
The number of overcorrections in primary and secondary gaze positions is shown in table 3. There were 8% central gaze overcorrections. The two patients overcorrected in central gaze on the final visit had deviations of 5 and 1 PD. The largest amounts of correction in central gaze were 9 and 13 PD, for 12 and 11 mm recessions, respectively. These were seen in the over-corrected patients whose preoperative central gaze hypertropia was 8 PD, with larger contralateral gaze deviations. The patient with the larger overcorrection showed a clinical pattern of an unmasked SOP of the opposite eye. This patient also had over-correction in downgaze.
Table 3.
Overcorrections
| Gaze direction of overcorrections | n (%) |
|---|---|
| Central | 2 (8) |
| Contralateral | 1 (4) |
| Ipsilateral | 2 (8) |
| Upgaze | 3 (12) |
| Downgaze | 1 (4) |
| Near | 2 (8) |
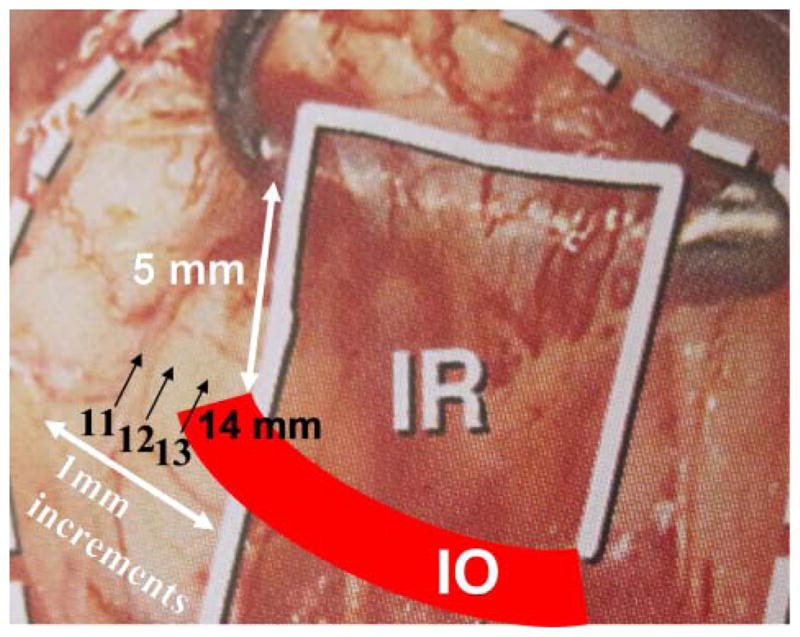
A scatterplot depicting the dose-response behaviour after surgery is presented in figure 2. There were varied responses to each dose of surgery. The slope of the fitted line (ie, dose response) for the central gaze calculation is 0.5 PD/mm (r2=0.04) and for the contralateral gaze calculation is 1.2 PD/mm (r2=0.28).
Figure 2.
Dose-response relationship for inferior oblique recession (IOR) in (A) central and (B) contralateral gaze. Correlation of amount of IOR (mm) with correction of deviation (prism diopters (PD)) in (A) central gaze and (B) contralateral gaze. Regression lines were forced through zero. Every circle represents an operated eye. Correction of 0.5 PD per mm recession in central gaze (r2=0.04), and 1.2 PD per mm in contralateral gaze (r2=0.28). This figure is only reproduced in colour in the online version.
Two of the patients underwent a repeat operation, one for overcorrection and the other for undercorrection. Both of these patients necessitated the use of prism glasses until their repeat operation was performed.
DISCUSSION
This study is the first to evaluate the effect of IOR on patients at risk for overcorrection from IOR due to small angle central gaze hypertropia resulting from SOP. This group had 5.6±2.1 PD mean preoperative central gaze hypertropia at distance, with no hypertropia exceeding 8 PD, and only 3.7±3.4 PD hypertropia at near. Graded IOR, with an average of 11 mm, produced 5.4±2.7 PD mean central gaze correction and 13.6±5.7 PD contralateral gaze correction, with two patients overcorrected. Of the two patients overcorrected, only one was symptomatic. These results show that the larger contralateral gaze hypertropias can be treated by IOR without appreciable central gaze overcorrection.
In the study by Morad et al8 the mean preoperative central gaze hypertropia was 12.5±6.2 PD for patients who underwent a 10 mm IOR, showing an average correction of 9.1 PD for central gaze and 15.4 PD for contralateral gaze. The authors point out that in most patients the operation appeared to be ‘self-surgical dosage adjusting’ in that the amount of improvement in primary position was highly correlated with the pre-operative deviation. This same finding of greater effect of surgery in the cases with greater preoperative deviation was shown in earlier studies on IO myectomies, IORs and IO anterior transpositions in patients with SOP.4,22 In the study by Hatz et al,9 the group undergoing IOR had 7±5 PD mean pre-operative hypertropia (distance) and 9±8 PD (near) that decreased to 2±2 PD at distance and 2±3 PD at near. Hatz et al9 also suggested that IO weakening is a self-titrating procedure, as evidenced by the absence of overcorrections even in patients who had minimal central gaze hyperdeviation. In our study, central gaze hypertropia was even less than in these previous studies. Given evidence from Morad et al8 that a 10 mm IOR provides 9 PD correction of hypertropia, one might have expected our patients to have frequent overcorrection using IOR. However, overcorrection was observed in only two patients (8%), of maximally 5 PD. The paucity of overcorrections may be because graded recessions were performed. In our calculated dose-response, a 10 mm recession produced a mean correction of 5 PD. Also, the 10 mm recession performed by Morad et al has some effect of anteriorisation and may be a stronger procedure than a 12–14 mm recession,17 thus leading to a larger correction than our procedures. The present findings support the view that there may be a non-specific beneficial effect of IOR, since patients who underwent large or very small 9 mm recessions had similar correction in central gaze and in contralateral gaze, in each instance corresponding to the original incomitance of the hypertropia. This ‘self adjusting’ theory remains to be further elucidated, but might be attributable to non-dose dependent effects of IOR.
Metten et al14 recently calculated a dose response relationship for IOR, showing correction of 0.6°/mm in central gaze, and up to 1.4°/mm in adduction. This is twice the correction found in the current study, but may be because the preoperative hypertropias studied by Metten et al were also twice the central and contralateral values included in the current study. In the Metten study, as in the present study, there was a large range of results for each dose of IOR, although there was an increase in the mean correction with increasing IOR. It is impossible to determine whether this is a true dose-response relationship versus a self-adjusting response. Our results argue for some degree of self-adjusting since there were so few overcorrections in patients with very small primary position deviations, even when there was full correction of the larger contralateral gaze deviation.
The most likely surgical alternative to IOR in patients such as in this study would be contralateral IRR. This surgery could be performed using an adjustable suture technique. However, IRR is prone to overcorrection due to non-adherence, alters the lid fissure depending on the amount of recession performed, and does not address the lateral incomitance. There was up to 41% overcorrection after adjustable IRR in the study by Sprunger and Helveston, and 38% undercorrection in the study by Scotcher et al18,23 It has been well documented that IRR, particularly when performed on adjustable suture, has a tendency toward both overcorrection or undercorrection postoperatively even in patients without thyroid eye disease.18–20,23 Wright has shown overcorrection 4–6 weeks postoperatively in patients who underwent both fixed and adjustable sutures.20 Interestingly, Kushner reported eight patients diagnosed with SOP (Knapp class II) with central gaze hypertropia <10 PD who underwent contralateral IRR, none of whom had postoperative overcorrections during a follow-up period of a mean of 3.7 years.21 This perhaps may be explained by the use of semiadjustable sutures24 for some patients, or because of the small amount of patients in that study.21 Kushner describes an alternative procedure for patients with SOP with small deviation hypertropia combining contralateral IRR and ipsilateral IR nasal transposition.25 This permits extra correction of excyclotropia. IRR alone may have less effect on excyclotropia than IOR in patients with SOP.
This study must be understood within the context of its limitations. Because it is a retrospective study, it is subject to measurement and interpretation errors that can accompany retrospective studies. In addition, because there is no alternative surgery for this specific group of patients that could be comparable to IOR in addressing lateral incomitance, we did not include a control group in this study.
In conclusion, we have shown that IOR can correct lateral incomitance even when treating small central gaze hypertropia, without causing significant overcorrection in central gaze. IOR is a predictable and stable procedure and a safe and effective treatment for SOP with small angle deviations in central position.
Acknowledgments
Funding This work was supported by: NIH/NEI grant K23EY021762, Knights Templar Eye Foundation, and US Public Health Service, NEI grant EY08313.
Footnotes
Dr Rosenbaum died on 22 June 2010
Contributors Conception and design: KH, SLP, FGV; acquisition of data: KH; analysis of results: KH, SLP; interpretation of data: KH, SLP, JLD, FGV; contribution of patients for this study: ALR, FGV, GV, JLD; preparation of manuscript: KH; critical revision of this manuscript: KH, SLP, JLD, GV, FGV.
Competing interests None
Ethics approval University of California Los Angeles Institutional Review Board.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement Data available on request from the corresponding author: FGV; velez@jsei.ucla.edu.
References
- 1.Knapp P. Classification and treatment of superior oblique palsy. Am Oprthoptic J. 1974;24:18–22. [PubMed] [Google Scholar]
- 2.Helveston EM, Mora JS, Lipsky SN, et al. Surgical treatment of superior oblique palsy. Trans Am Ophthalmol Soc. 1996;94:315–35. [PMC free article] [PubMed] [Google Scholar]
- 3.Scott WE, Kraft SP. Pediatric ophthalmology and strabismus: trans new Orleans Acad Ophthalmol. Raven Press; New York: 1986. Classification and treatment of superior oblique palsy: I. Unilateral superior oblique palsy; pp. 15–38. [PubMed] [Google Scholar]
- 4.Shipman T, Burke J. Unilateral inferior oblique muscle myectomy and recession in the treatment of inferior oblique muscle overaction: a longitudinal study. Eye. 2003;17:1013–18. doi: 10.1038/sj.eye.6700488. [DOI] [PubMed] [Google Scholar]
- 5.Maruo T, Iwashige H, Kubota N, et al. Long-term results of surgery for superior oblique palsy. Jpn J Ophthalmol. 1996;40:235–8. [PubMed] [Google Scholar]
- 6.Simons BD, Saunders TG, Siatkowsky RM, et al. Outcome of surgical management of superior oblique palsy. A study of 123 cases. Binocul Vis Strabismus Q. 1998;13:273–82. [PubMed] [Google Scholar]
- 7.Parks MM. The weakening surgical procedure for eliminating overaction of the inferior oblique muscle. Am J Ophthalmol. 1972;73:107–22. doi: 10.1016/0002-9394(72)90313-3. [DOI] [PubMed] [Google Scholar]
- 8.Morad Y, Weinstock VM, Kraft SP. Outcome of inferior oblique recession with or without vertical rectus recession for unilateral superior oblique paresis. Binocul Vis Strabismus Q. 2001;16:23–8. [PubMed] [Google Scholar]
- 9.Hatz KB, Brodsky MC, Killer HE. When is isolated inferior oblique muscle surgery an appropriate treatment for superior oblique palsy? Eur J Ophthalmol. 2006;16:10–16. doi: 10.1177/112067210601600103. [DOI] [PubMed] [Google Scholar]
- 10.Mittelman D, Folk ER. The evaluation and treatment of superior oblique muscle palsy. Trans Am Acad Ophthalmol Otolaryngol. 1976;81:893–7. [PubMed] [Google Scholar]
- 11.Singh V, Agrawal S, Agrawal S. Outcome of unilateral inferior oblique recession. J Pediatr Ophthalmol Strabismus. 2009;46:350–7. doi: 10.3928/01913913-20090818-09. [DOI] [PubMed] [Google Scholar]
- 12.Ehrt O, Bekl Y, Boergen KP. Effect of inferior oblique recession in strabismus sursoadductorius. Strabismus. 2002;10:63–8. doi: 10.1076/stra.10.2.63.8138. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt S, Gräf M, Kaufmann H, et al. Surgery for strabismus sursoadductorius (congenital superior oblique palsy) in childhood. Klin Monbl Augenheilkd. 2011;228:874–9. doi: 10.1055/s-0031-1281759. [DOI] [PubMed] [Google Scholar]
- 14.Metten M, Link H, Staubach F, et al. Dose-response relationship in inferior oblique muscle recession. Graefes Arch Clin Exp Ophthalmol. 2008;246:593–8. doi: 10.1007/s00417-007-0763-6. [DOI] [PubMed] [Google Scholar]
- 15.Apt L, Call NB. Inferior oblique muscle recession. Am J Ophthalmol. 1978;85:95–100. doi: 10.1016/s0002-9394(14)76672-3. [DOI] [PubMed] [Google Scholar]
- 16.Gräf M, Lorenz B, Eckstein A, et al. Superior oblique tucking with versus without additional inferior oblique recession for acquired trochlear nerve palsy. Graefes Arch Clin Exp Ophthalmol. 2010;248:223–9. doi: 10.1007/s00417-009-1188-1. [DOI] [PubMed] [Google Scholar]
- 17.Isenberg SJ, Apt L. Inferior oblique weakening procedures: Technique and indications. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management. Philadelphia: WB Saunders; 1999. pp. 449–58. [Google Scholar]
- 18.Scotcher SM, O’Flynn EA, Morris RJ. Inferior rectus recession—an effective procedure? Br J Ophthalmol. 1997;81:1031–6. doi: 10.1136/bjo.81.12.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vazquez CW, Muñoz M. Overcorrection after adjustable suture suspension-recession of the inferior rectus muscle in non-thyroid eye disease. Binocul Vis Strabismus Q. 1999;14:103–6. [PubMed] [Google Scholar]
- 20.Wright KW. Late overcorrection after inferior rectus recession. Ophthalmol. 1996;103:1503–7. doi: 10.1016/s0161-6420(96)30476-4. [DOI] [PubMed] [Google Scholar]
- 21.Kushner BJ. Vertical rectus surgery for Knapp class II superior oblique muscle paresis. Arch Ophthalmol. 2010;128:585–8. doi: 10.1001/archophthalmol.2010.64. [DOI] [PubMed] [Google Scholar]
- 22.May MA, Beauchamp GR, Price RL. Recession and anterior transposition of the inferior oblique for treatment of superior oblique muscle palsy. Graefes Arch Clin Exp Ophthalmol. 1988;226:407–9. doi: 10.1007/BF02169997. [DOI] [PubMed] [Google Scholar]
- 23.Sprunger DT, Helveston EM. Progressive overcorrection after inferior rectus recession. J Pediatr Ophthalmol Strabismus. 1993;30:145–8. doi: 10.3928/0191-3913-19930501-04. [DOI] [PubMed] [Google Scholar]
- 24.Kushner BJ. An evaluation of the semiadjustable suture strabismus surgical procedure. J AAPOS. 2004;8:481–7. doi: 10.1016/j.jaapos.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Santiago AP, Isenberg AJ, Apt L, et al. The effect of anterior transposition of the inferior oblique muscle on ocular torsion. J AAPOS. 1997;1:191–6. doi: 10.1016/s1091-8531(97)90036-7. [DOI] [PubMed] [Google Scholar]