Abstract
Binge drinking is a public health concern due to its association with negative health outcomes as well as increased legal and social consequences. Previous studies have frequently used self-reported alcohol consumption to classify binge drinking episodes; however, these measures are often limited in both detail and accuracy. Some researchers have begun using additional measures such as blood (BAC) and breath (BrAC) alcohol concentrations to supplement self-report data. Transdermal alcohol testing, or the detection of alcohol expiration through the skin, offers advantages over BAC and BrAC measures by allowing for continuous and noninvasive monitoring of an individual's drinking behavior in real-time. Despite these advantages, this technology has not been widely used or studied outside of forensic applications. The present research compares transdermal alcohol concentration (TAC) and BrAC readings during the consumption of alcohol ranging from moderate drinking to binge drinking in 22 adult regular drinkers in order to investigate the sensitivity and specificity of the TAC monitors. We observed that BrAC and TAC measures were broadly consistent. Additionally, we were able to develop an equation that could predict BrAC results using TAC data, indicating TAC data would be an appropriate substitute in research and clinical contexts where BrAC readings are typically used. Finally, we were able to determine a cutoff point for peak TAC data that could reliably predict whether a participant had engaged in moderate or more than moderate drinking, suggesting TAC monitors could be used in settings where moderate or reduced drinking is the goal.
Keywords: TRANSDERMAL ALCOHOL MONITORING, BINGE DRINKING, ALCOHOL ABUSE
Binge alcohol drinking is a serious public health concern associated with negative health consequences and poor developmental outcomes. Alcohol binging is typically defined as a persistent pattern of drinking that produces a blood alcohol concentration of ≥ 0.08 g/dl, which would typically correspond to at least five drinks for men or four drinks for women consumed within a 2-hour period (NIAAA, 2004). This pattern of drinking exceeds normal moderate social drinking (Dawson, 2000; Dufour, 1999), and imparts an immediate risk of negative consequences including unintentional injuries, suicide, violent acts, fetal alcohol syndrome, and child abuse/neglect (Holtzman, 2003; Powell-Griner et al., 1997; Wagenaar & Wolfson, 1995; Wechsler et al., 1994). In addition, binge drinking increases the long-term risk for alcohol dependence and other substance use disorders as well as a host of other long-term health risks including diabetes, hypertension, and cardiovascular disease (Bonomo et al., 2004; Dawson, 1996; Dawson et al., 2005; Fan et al., 2008; Okosun et al., 2005; Robin et al., 1998; Schulenberg et al., 1996, 2002). Despite these risks, 20% of drinkers in the United States report binge drinking in the past month (DHHS, 2002).
Further studies are needed to better understand the etiology of binge drinking and develop effective treatment and intervention strategies for reducing this dangerous behavior. Previous studies have typically relied on self-reports of drinking behaviors; however, these measures are often limited in both detail and accuracy (e.g., Knibbe & Bloomfield, 2001; Midanik 1982; 1989; Poikolainen et al., 2002; Polich 1982). Accordingly, it has been recommended that researchers using self-report measures should also use corroborating data (e.g., blood and breath alcohol concentrations, biochemical markers, collateral informant reports) to increase confidence in the data being collected (Del Boca & Darkes, 2003). The most widely used and accepted measures for determining recent alcohol consumption are blood (BAC) and breath (BrAC) alcohol concentrations. However, these measures are limited in that they require the active participation of the drinker and only provide information about alcohol concentrations at a single point in time. Because the persistence of ethanol in the blood and breath is short-lived, BAC and/or BrAC must be measured in close proximity to peak intoxication to capture peak concentrations of alcohol and repeated measurements are necessary to determine the length of intoxication during a drinking session (e.g., Pizon et al., 2007; Swift, 2003). Other biological markers of alcohol use, including direct markers (ethanol metabolites) and indirect markers (e.g., liver enzymes) measured in the blood or urine, persist longer in the body but lack sensitivity and specificity (Conigrave et al., 2003; Neumann and Spies, 2003; Peterson, 2004; Sillanaukee, 1996; Thierauf et al., 2010).
Transdermal alcohol testing, or the detection of alcohol expiration through the skin, is a method that continuously and noninvasively gathers information about an individual's drinking behavior in real-time. Approximately 1% of ethanol consumed is excreted through sweat (Norberg et al., 2003; Pizon et al., 2007; Swift, 2003). Ethanol concentration in vapors formed above the skin was first measured in the mid 1980s using a portable electrochemical fuel sensor placed directly above the skin and a high correlation was found between ethanol concentration in these vapors and both BAC and BrAC (Giles et al., 1986; 1987). Currently, there are several transdermal alcohol monitors available from different manufacturers, including at least three ankle monitors and a wrist monitor. These devices can be worn for long periods of time (e.g., months), passively collecting transdermal alcohol concentration (TAC) data for continuous alcohol consumption monitoring. Peer reviewed publications using these devices are scarce (for examples, see Ayala et al., 2009; Davidson et al., 1997; Dumett et al., 2008; Marques & McKnight, 2009; Sakai et al., 2006; Swift et al., 1992; Swift, 2000) and focus on two devices: the Secure Continuous Remote Alcohol Monitoring (SCRAM) ankle monitor from Alcohol Monitoring Systems, Inc. (AMS, Littleton, CO) and the Wrist Transdermal Alcohol Sensor (WrisTAS) from Giner, Inc. (Newton, MA).
The transdermal alcohol monitors currently available are most commonly used in the criminal justice system to monitor offenders who have been ordered to abstain from alcohol, such as those with multiple DUI or DWI offenses. They were developed to monitor alcohol abstinence rather than provide quantitative measurements of BAC (Dumett et al., 2008; Marques & McKnight, 2009). However, investigators have compared the reliability of the WrisTAS bracelet and the SCRAM monitor with the more traditional measures BAC or BrAC and have found peak TAC and area under the TAC curve to be correlated with BrAC and BAC with no false positives and no false negatives in a laboratory setting (Davidson et al., 1997; Dumett et al., 2008; Marques & McKnight, 2009; Sakai et al., 2006; Swift et al., 1992; Swift, 2000). Sakai and colleagues (2006) concluded that the SCRAM is able to reliably detect TAC associated with two standard drinks and can discriminate between groups with low vs. high alcohol consumption. They also noted that TAC results were not equivalent to simultaneous BrAC results, consistent with findings from other research showing TAC curves are delayed by 1 to 3 hours after BrAC curves but generally follow the same form (Davidson et al., 1997; Marques & McKnight, 2009; Swift et al., 1992; Swift, 2000; 2003).
The technology used to measure TAC (i.e., TAC monitors) has improved substantially in recent years yet has not been fully embraced by researchers studying alcohol use. In the limited studies that are available, researchers have examined TAC monitor results following a high dose of alcohol (Swift et al., 1992), a low dose and a high dose (Sakai et al., 2006; Marques & NcKnight, 2009), or a range of low doses (Davidson et al., 1997). In order to advance research on drinking behaviors using TAC monitors, it is important to test the ability of these devices to detect a variety of alcohol doses that simulate typical drinking patterns, including binges, in a laboratory setting. The present research uses TAC monitors during the consumption of alcohol doses ranging from 1 to 4 (for women) or 1 to 5 (for men) standard drinks, allowing for a detailed investigation of the sensitivity and specificity of the TAC monitors. If the TAC monitor is able to discern between low, medium, and high numbers of standard drinks, TAC could be used in research and clinical settings where moderate or reduced drinking is encouraged rather than abstinence, as well as situations in which remote monitoring of drinking behaviors is necessary or desirable. In the current study, participants consumed a different number of beers on different study days (i.e., women consumed 1, 2, 3, and 4 beers across 4 study days and men consumed 1, 2, 3, 4, and 5 beers across 5 study days) and both TAC and BrAC were monitored in the laboratory. Beers were consumed at a rate that would be consistent with a binge drinking episode. We sought to determine whether peak levels of intoxication as measured through TAC paralleled peak BrAC levels and reliably detected intoxication levels following the consumption of different quantities of alcohol.
METHODS
Subjects and Criteria
Participants were recruited from the community through newspaper advertisements seeking healthy men and women aged 21 to 45 who regularly consume alcohol. Exclusion criteria included a body mass index less than 18 or greater than 30 kg/m2, a current or past Axis I psychiatric disorder, a current medical condition, a history of substance dependence, and not reporting drinking similar amounts of alcohol in the previous month at a rate that would have been expected to produce a BrAC at or above levels that were expected to be achieved in the laboratory. A total of 22 healthy adult alcohol drinkers (11 men, 11 women) enrolled in the study. Informed consent was obtained prior to study participation, and the Institutional Review Board at The University of Texas Health Science Center at San Antonio reviewed and approved the experimental protocol. Each participant was compensated $70.00 per day for their participation.
Measures of Alcohol Levels
Transdermal alcohol concentration monitoring
Secure Continuous Remote Alcohol Monitors (SCRAM-II™, Alcohol Monitoring Systems Inc., Highlands Ranch, CO) were used to continuously measure transdermal alcohol concentration (TAC). Eight SCRAM-II monitors were used in the study and each participant was assigned to only one device for the duration of their participation. Results were available both as figures and numerical values and included parameters such as peak TAC, or the highest TAC value recorded during a drinking episode, and the time to peak TAC, or the time in minutes from the last 0.000 g/dl TAC recording to the first peak TAC recording in a drinking episode.
Breath alcohol monitoring
Drager Alcotest 6810 portable breathalyzers were used during the study to measure breath alcohol concentrations (BrAC). BrAC results were displayed on the device and recorded by study personnel.
Procedure
Recruitment and study design
Interested respondents underwent an initial phone screen to determine eligibility by providing height, weight, age, and answering a series of questions about medical history and current drinking behavior. Participants who met minimum eligibility criteria were invited to the lab for an in-person interview, which included a detailed substance abuse history, a psychiatric screening using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders: Research Version, Non-Patient Edition (SCID-I/NP; First et al. 2002), and a medical history and physical examination by a physician or nurse practitioner.
Once enrolled, participation lasted 4 days for female participants and 5 days for male participants. Participants were asked to fast after midnight on the day of participation and this was confirmed via self report on the morning of each testing day. Participants provided urine (for drug and pregnancy tests) and alcohol breath samples upon arrival in the laboratory at 8:00 am on each day of participation. Each participant was also fitted with a SCRAM-II ankle monitor that was secured so that the face plate of the device was in direct contact with the skin. Participants began the alcohol administration procedure two hours after arriving at the laboratory, allowing at least 90 minutes for the TAC monitor to equilibrate. Participants then consumed their allotted alcohol dose for that testing session and their intoxication was measured using TAC and BrAC monitors. A meal was provided after a participant's BrAC level reached 0.000 g/dl or, at the latest, 4:00 pm. Participants remained in the lab until their TAC readings fell to ≤ 0.005 g/dl, which was reached approximately 2 to 3 hrs after BrAC fell to 0.000 g/dl. Monitors were removed at the end of each day and participants underwent a field sobriety test to assure that they were alert and in full control of their behavior before leaving.
Alcohol administration
A simulated alcohol binge procedure was used based on the definition, provided by NIAAA (2004) and others (e.g., Wechsler & Nelson, 2001) of an alcohol "binge" as a drinking episode that produces a blood alcohol concentration of ≥ 0.08 g/dl. By this definition, a binge drinking episode would roughly correspond to at least five drinks for men and four drinks for women consumed within a 2-hour period (NIAAA, 2004; Wechsler et al., 1994).
Twelve-ounce Corona beers, 4.6% alcohol by volume, (Grupo Modelo S.A.B. de C.V., Mexico City, Mexico) were administered to participants by research staff. To produce a range of BrAC levels for each participant, participants consumed one beer on the first study day and increased in their intake by one beer on each subsequent study day, ending with a maximum of four beers for women and five beers for men. The maximum number of beers for each sex was chosen to produce a blood alcohol concentration of ≥ 0.08 g/dl when consumed within a 2-hour period (Wechsler et al., 1994). The rate of beer consumption was monitored, and women were required to consume each beer within 30 minutes and men were required to complete each beer within 24 minutes. By definition, this rate would produce a binge episode at the 4 (women) and 5 (men) beer drinking conditions, where these beers were consumed within a 2-hour period. Accordingly, the length of alcohol consumption varied systematically with the dose of alcohol consumed that day.
Alcohol concentration monitoring
After an initial 30-minute reading, the SCRAM-II monitor recorded transdermal (TAC, Infrared [IR], and temperature) readings every five to seven minutes to gather baseline data specific to the wearer. The SCRAM-II monitor must equilibrate for about 1–1.5 hours. Once equilibration is established, the monitors begin recording data every 30 minutes. TAC, IR, and temperature recordings were stored in the memory of the device and were uploaded to the Recovery Healthcare Systems website. Beginning 15 minutes after the completion of the first beer, participants also provided exhaled breath samples every 15 minutes for the first 2 hours and then every 30 minutes until two consecutive readings of 0.000 g/dl were obtained. Participants rinsed their mouths with water twice before BrAC was measured and each exhaled air reading was acquired using a new disposable mouthpiece to avoid inaccuracies caused by the presence of residual alcohol.
Data Analysis
We first examined the degree to which individual differences in TAC levels parallel individual differences in BrAC levels. Within each drinking session, we computed correlations, across participants, between peak TAC measurements and peak BrAC measurements.
We next examined the more fundamental issue of whether changes in peak TAC levels parallel changes in peak BrAC levels for both group level and individual level (within-person correlations). Group level analyses used factorial repeated-measures ANOVAs for each sex with Number of Drinks and Device (TAC or BrAC) as two within subjects factors. Within-person correlations between peak TAC and peak BrAC were determined for each person across each drinking sessions (1 to 4 drinks for females and 1 to 5 drinks for males). Then, after computing a “within-person” correlation for each person, we averaged those correlations across all females and across all males. These averages reflect, for the average person, the degree to which increases in TAC parallel increases in BrAC.
We next developed an equation to predict or estimate an individual’s peak BrAC level during a drinking occasion. To do this, we used a multilevel modeling procedure that identifies significant predictors of peak BrAC levels. This procedure allowed us to evaluate the predictive power of stable person-level variables such as sex and BMI, as well as drinking occasion-level variables such as peak TAC level and time to peak TAC level.
Finally, we created Receiver Operating Characteristic (ROC) curves to compare the peak TAC to predict the number of drinks consumed by participants. Separate ROC curves were calculated to compare participants’ peak TAC results from the one and two drink sessions to the peak TAC values from the sessions in which more drinks were consumed. The area under the ROC curve (AUC) is considered a measure of the predictive power of peak TAC. Sensitivity in detecting alcohol consumption and specificity in classifying moderate vs. more than moderate drinking were assessed. This analysis allowed us to determine cutoff values for peak TAC that could distinguish between moderate and more than moderate drinking. We were then able to examine the accuracy of these cutoff values in correctly classifying participants’ drinking days into moderate and more than moderate drinking.
RESULTS
Twenty-two healthy adult participants (11 men, 11 women) enrolled in this study. One male participant’s data was not included in the analysis because the transdermal alcohol device assigned to him functioned intermittently, resulting in a final sample of 21 (11 women and 10 men). Characteristics of both sexes are shown in Table 1. Male and female participants did not differ on any of the demographic variables or their alcohol and cigarette use. Men and women did not differ on BMI but men were significantly taller and heavier.
Table 1.
Demographic data
| Characteristics | Men (n = 10) |
Women (n = 11) |
Combined (n = 21) |
Sex Difference |
|---|---|---|---|---|
| Mean (SD) | ||||
| Age (years) | 26.2 (6.5) | 28.5 (7.6) | 27.4 (7.0) | p = 0.48 |
| Education (years) | 14.2 (1.9) | 14.4 (2.1) | 14.3 (2.0) | p = 0.50 |
| BMI | 24.6 (3.6) | 24.5 (3.5) | 24.5 (3.4) | p = 0.97 |
| Height (inches) | 69.0 (1.9) | 63.0 (2.5) | 66.8 (3.8) | p = 0.0003 |
| Weight (lbs) | 166.2 (22.0) | 138.7 (21.9) | 151.8 (25.6) | p = 0.022 |
| Cigarettes (per day) | .3 (0.9) | 1.8 (3.8) | 1.1 (2.9) | p = 0.89 |
| Alcohol (drinks per week) | 13.8 (8.3) | 11.7 (6.9) | 12.7 (7.5) | p = 0.33 |
| Ethnicity* (AA/C/H/other) | 2/2/5/1 | 0/0/8/3 | 2/2/13/4 | p = .28 |
Ethnicity is represented as the frequency of individuals in each group identifying as African-American (AA), Caucasian (C), Hispanic (H) or other and was compared across sexes using a chi-square analysis.
Relationships between TAC and BrAC measures
First, we examined the degree to which individual differences in peak TAC levels correlated with individual differences in peak BrAC levels, for each number of drinks. As shown in Table 2 (left side), there was a range of correlations in each sex and in the sample as a whole, none of which were statistically significant.
Table 2.
Comparing BrAC with: raw TAC data and predicted BrAC (derived from TAC data using Equation 1) after different numbers of beers
| BrAC vs. Raw TAC data | BrAC vs. Predicted BrAC | |||||
|---|---|---|---|---|---|---|
| Men | Women | All | Men | Women | All | |
| 1 beer | 0.36 | −0.49 | −0.24 | 0.42 | −0.26 | −0.05 |
| 2 beers | −0.06 | 0.43 | 0.2 | 0.48 | 0.79** | 0.73*** |
| 3 beers | −0.14 | 0.36 | 0.24 | 0.55† | 0.84** | 0.81*** |
| 4 beers | −0.46 | 0.32 | −0.02 | 0.66* | 0.92*** | 0.90*** |
| 5 beers1 | 0.01 | ----- | ----- | 0.89*** | ----- | ----- |
p < .10,
p< .05,
p < .01,
p < .001,
5 beers condition only includes male participants.
Next, we examined the ability of TAC and BrAC to detect changes in peak alcohol levels. Results show robust associations between changes in peak TAC levels and changes in peak BrAC levels at both the group level and individual level. The relationship between observed TAC levels and BrAC levels across different numbers of drinks appears in Figure 1.
Figure 1.
a. Mean peak TAC in g/dl (± SE) and mean peak BrAC in g/dl (± SE) for each drinking condition among male participants.
b. Mean peak TAC in g/dl (± SE) and mean peak BrAC in g/dl (± SE) for each drinking condition among female participants.
As expected, ANOVAs revealed robust effects of number of drinks on peak measurements for both Devices (breathalyzer and SCRAM-II ankle monitor). Among Females, the main effect of Number of Drinks was significant (F(3, 30) = 79.94, p < .0001, partial η2 = .89). The main effect of Device was significant as well (F(1,10) = 20.74, p = .0011, partial η2 = .67), indicating that the mean BrAC level was greater than the mean TAC levels. The interaction was non-significant (F(3,30) = .43, p = .7347, partial η2 = .04), suggesting that the Devices did not differ in their sensitivity under any specific number of drinks. Among Males, the main effect of Number of Drinks was again significant, as expected (F(4, 36) = 72.40, p < .0001, partial η2 = .89). Neither the main effect of Device (F(1, 9) = 1.97, p = .1943, partial η2 = .18) nor the interaction were significant (F(4, 36) = 1.27, p = .2978, partial η2 = .12). For both genders, post hoc analyses of the main effect of Number of Drinks revealed significant increases in alcohol levels with each increase in the Number of Drinks. Overall, these results demonstrate that increases in the number of drinks consumed produces increases in peak measurements for both Devices, and that the increases are essentially parallel across the two Devices.
Moving from the group level to an individual level perspective on correlated change, we computed Pearson correlation coefficients between peak BrAC levels and peak TAC levels for each participant individually. The correlations are robust, ranging from 0.700 to 0.997, with the mean correlation for each gender significantly greater than zero (Female Mean r = .91, SD = .09, t(10) = 33.32, p < .0001; Male Mean r = .86, SD = .10, t(9) = 27.47, p < .0001). The difference between the Female and Male means was not significant (t(19) = 1.10, p = .2834). The magnitudes and significance of these correlations demonstrate that, for the average person, changes in TAC levels strongly parallel changes in BrAC levels as the number of drinks increase.
Development of a TAC-based model for predicting BrAC
A multilevel modeling procedure was used to develop an equation to predict an individual’s peak BrAC level from their TAC data. Initial phases of multilevel modeling focused on potential predictors at level 1, or occasion-level predictors (Nezlek, 2007). Accordingly, peak TAC level and time to peak TAC were entered in level 1. It should be noted that TAC levels did not change from 0.000 g/dl in the one beer condition for two female participants and one male participant; their data for that session were excluded from analysis. Results indicated that both predictors were positively associated with peak BrAC, the slopes for both were statistically significant, the slope for peak TAC level should be treated as a randomly-varying, and that the intercept and the slope for time to peak TAC should be treated as fixed. This model is presented in Equation 1 of Table 3, and its coefficients can be interpreted as unstandardized regression coefficients.
Table 3.
Equations for predicting BrAC
| Equation | Formulation | Pearson rho |
Spearman rho |
|---|---|---|---|
| 1 | 0.01863 + 0.4939*PkTAC + 0.000155*ZeroToPkTAC | 0.932 | 0.925 |
| 2 | 0.01727 + 0.3497*PkTAC + 0.000164*ZeroToPkTAC + 0.002195*Gender + 0.2207*PkTAC*Gender + 0.000001652*ZeroToPkTAC*Gender |
0.929 | 0.921 |
| 3 | 0.0223 + 0.5674*PkTAC + 0.000293*ZeroToPkTAC + 0.000672 *Gender + (−0.00002) *Weight + 0.1609*PkTAC*Gender + (−0.00000711)*ZeroToPkTAC*Gender + (−0.00128)*PkTAC*Weight + (−0.000000862)*ZeroToPkTAC*Weight |
0.930 | 0.921 |
| 4 | 0.0142 + 0.6878*PkTAC + 0.00027*ZeroToPkTAC + 0.001321*Gender + 0.000174*BMI + 0.2056*PkTAC*Gender + 0.000011*ZeroToPkTAC*Gender + (−0.01362)*PkTAC*BMI + (−0.0000048)*ZeroToPkTAC*BMI |
0.929 | 0.922 |
In the next phases of multilevel modeling, the model was expanded to include predictors at level 2, or the person-level predictors. We entered sex (coded 0 = male and 1 = female), weight, and BMI as level 2 predictors because these factors are commonly used in the calculation of relationships between blood alcohol levels and number of drinks consumed (e.g., Widmark, 1981). Across several models, sex, weight, and BMI were not significant predictors of BrAC and did not improve the model beyond TAC data alone. The model that best predicted peak BrAC contained peak TAC and time to peak TAC only. The equations produced by the different models are presented in Table 3 (Equations 2–4).
Predictive accuracy of the TAC-based model
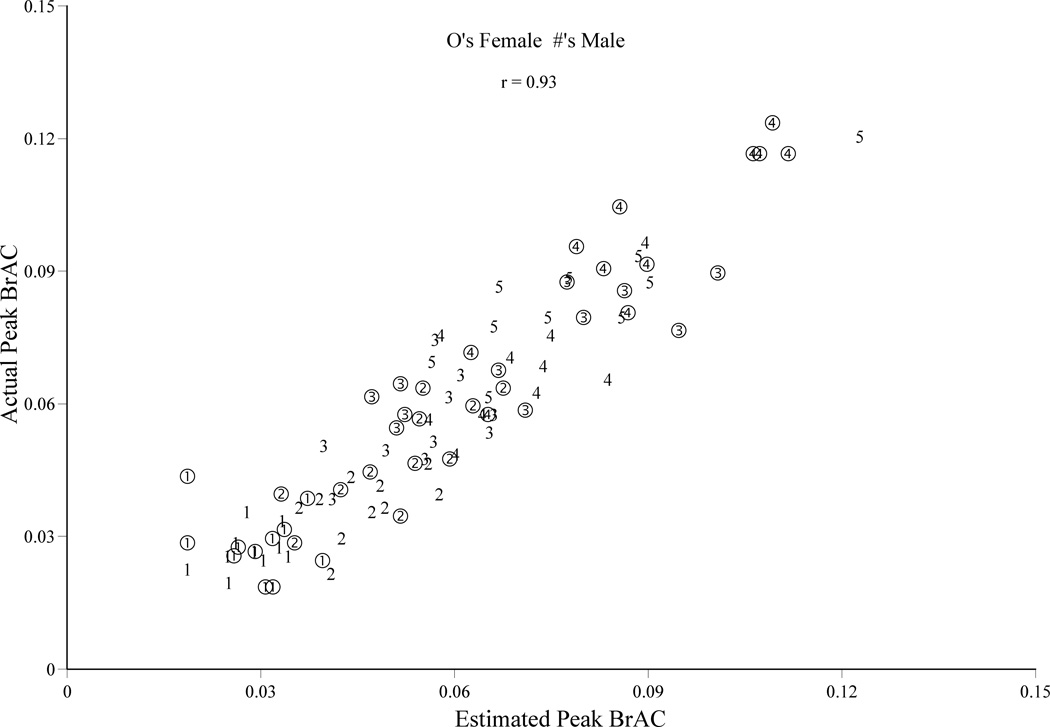
A final set of analyses was performed to determine to what extent the most accurate equation derived from multilevel modeling (Equation 1) could predict peak BrAC using values (n = 91) for each participant in each drinking condition. These data appear in Figure 2. To evaluate the model’s general predictive accuracy, we computed Pearson correlation coefficients for the comparison between these predicted values and participants’ actual peak BrAC values. The correlation was large (r = 0.93), indicating a very high level of predictive accuracy1.
Figure 2.
Scatterplot of association between predicted and actual peak BrAC (g/dl), across all participants in all drinking conditions. Circles with numbers inside represent a data point from a female and the number of beers. Numbers represent a data point from a male and numbers of beers.
Next, in order to measure how well the model could predict BrAC values within drinking conditions (1–5 drinks), the predicted BrAC values were correlated with the actual BrAC values within each drinking occasion; these data are presented in Table 2 (right side). In the one drink condition, the predictive accuracy was poor and non-significant; however, the predictive accuracy was robust and statistically significant in every other condition. This indicates that although raw TAC readings do not correspond closely with BrAC readings, other data collected by the TAC monitor can be used in an equation that predicts BrAC readings with greatly improved accuracy. Interestingly, the correlations between predicted and actual BrAC increased as the number of drinks increased from r = −0.05 in the one drink condition to r = 0.89 in the five drink condition.
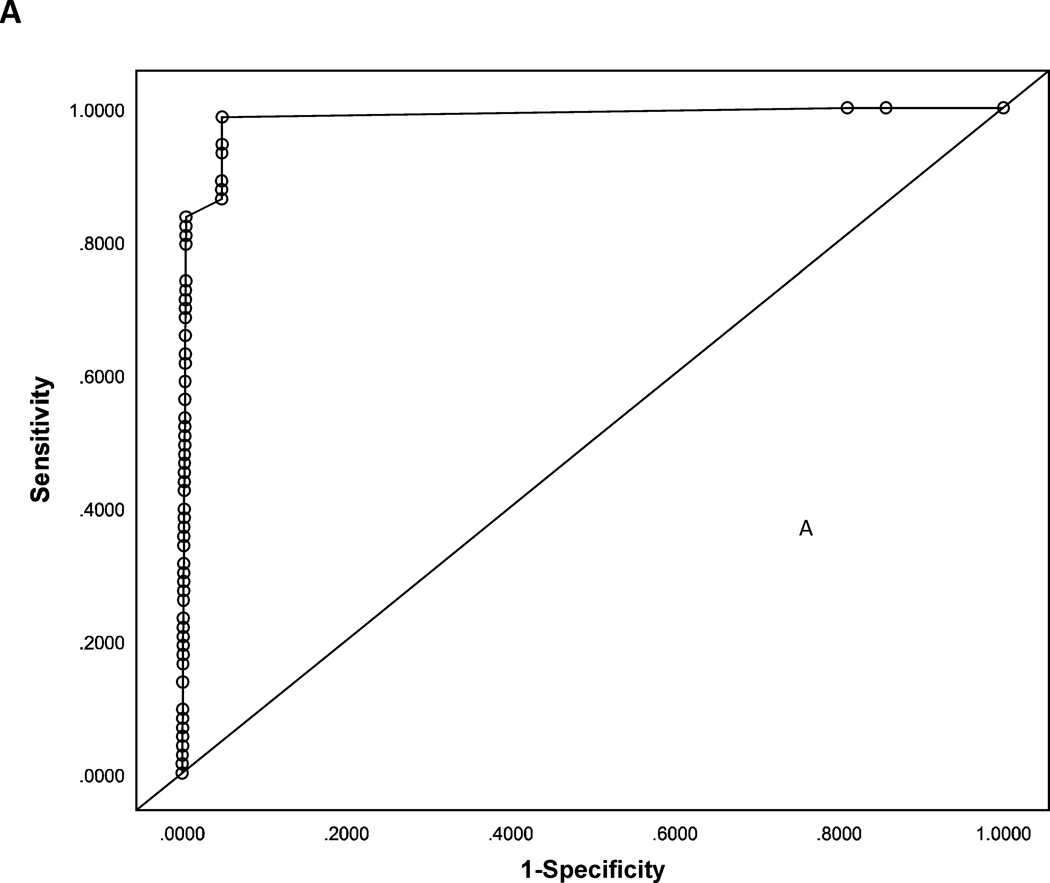
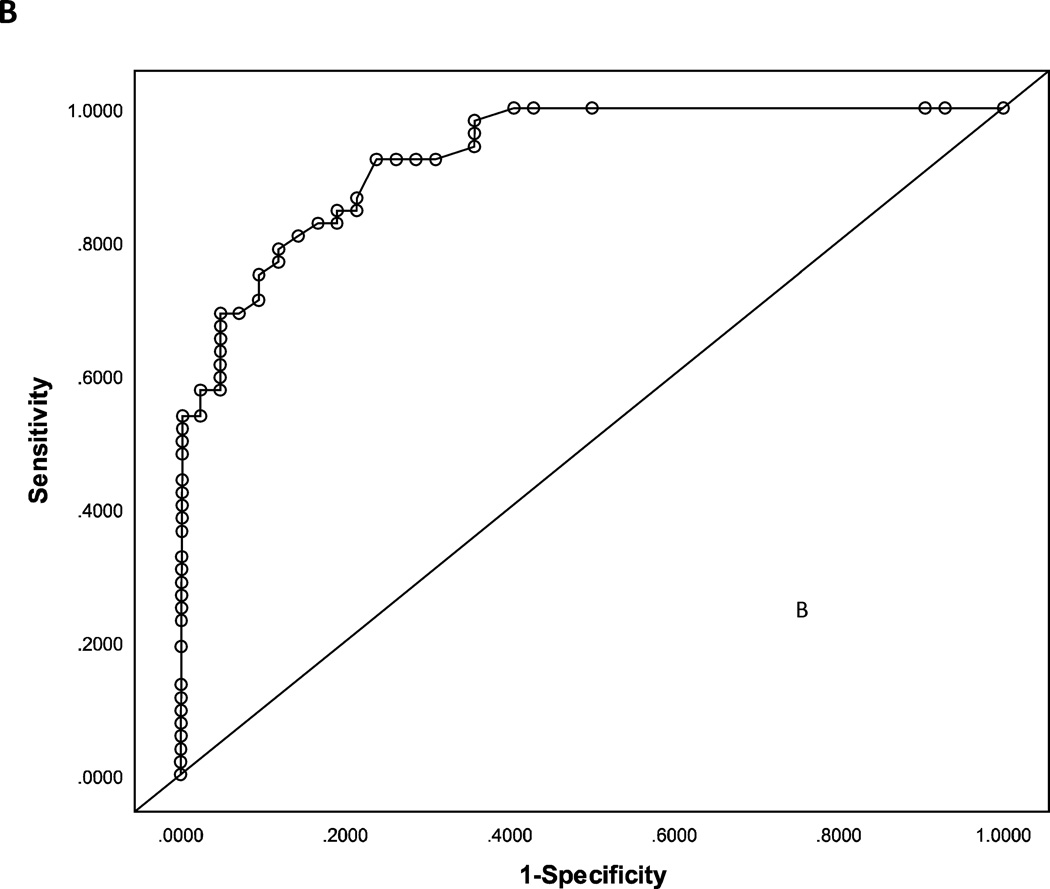
Detection of drinking
Receiver operating characteristic (ROC) curves were plotted using peak TAC to predict the number of drinks consumed by participants. Separate ROC curves were calculated to compare participants’ peak TAC results from the one and two drink sessions to the peak TAC values from the sessions in which more drinks were consumed. The ROC curve comparing TAC data for the one beer session to all other sessions is presented in Figure 3a. A cutoff of ≥ 0.011 g/dl peak TAC value classified participants as having drank one beer or greater than one beer with 97.9% accuracy, area under the curve (AUC) = 0.99, sensitivity = 98.6%, and specificity = 95.0%. The ROC curve comparing peak TAC values for the one and two beer sessions to the peak TAC values for the sessions in which greater than two beers were consumed is presented in Figure 3b. A cutoff of ≥ 0.024 g/dl peak TAC value classified participants as having drank 1–2 beers or greater than 2 beers with 85.1% accuracy, AUC = 0.93, sensitivity = 92.3%, and specificity = 76.2%. Overall, ability of these cutoff points in peak TAC scores to predict the number of drinks consumed is excellent.
Figure 3.
a-b. ROC curves indicating the sensitivity and specificity associated with cutoffs on peakTAC (g/dl) as they predict whether a participant has consumed more than one drink (3a) and more than two drinks (3b).
DISCUSSION
This project was designed to test relationships of transdermal alcohol concentration (TAC) measures to breath alcohol concentration (BrAC) measures across a range of alcohol doses consumed in a binge-like pattern. Twenty-one participants (11 women and 10 men), with a broad range of weight and BMI, consumed varying amounts of alcohol on different study days while having their BrAC and TAC measured by researchers. We observed that BrAC and TAC measures were broadly consistent across a range of alcohol consumption levels. Using a multilevel modeling procedure to develop an equation to predict an individual’s peak BrAC level from their TAC data, the model that best predicted peak BrAC contained peak TAC and time to peak TAC only. That is, across several models, sex, BMI, and weight were not significant predictors of BrAC and did not improve the model beyond TAC data alone. Taken together, our data indicates that TAC may be a suitable measure for indexing alcohol consumption in real-world settings to study binge drinking and other patterns of problem alcohol consumption.
Relationships between TAC, BrAC, and number of drinks consumed
We observed that TAC readings increased linearly as a function of the number of drinks consumed, consistent with previous research on TAC results in laboratory alcohol dose experiments (Sakai et al., 2006; Davidson et al., 1997). Increases in TAC readings across drink conditions also paralleled BrAC readings, indicating these measures can be used similarly. However, correlations between TAC readings and BrAC readings differed in their magnitude and there were no significant correlations across participants between raw TAC reading and BrAC reading for any of the levels of drinks in either sex. Although one study found the SCRAM device more readily detects TAC in male subjects than female subjects (Marques & McKnight, 2009), correlations between TAC results from our newer model of the SCRAM and BrAC results did not differ significantly by sex at each level of drinks consumed in this study. Taken together, the findings suggest these TAC data could be used in place of BrAC data in clinical and research settings with equivalent confidence as more traditional alcohol detection measures for measuring alcohol consumption in men and women. However, because TAC data is not highly correlated with BrAC data across individuals, calculations are necessary to convert TAC readings into meaningful assessments of the number of drinks consumed by an individual.
A TAC-based model for predicting BrAC
The results of multilevel modeling indicated that Equation 1 in Table 3, which includes only peak TAC and time to peak TAC to predict BrAC, was most effective at estimating BrAC readings. Although researchers frequently consider both participant sex and body weight when estimating the effect of consumed alcohol on alcohol concentrations in the body (e.g., Guillot et al., 2010), adding sex, weight, or BMI to the model containing TAC results did not increase the discriminative ability of the multilevel model. Given that TAC data is specific to each participant, it is likely that individual differences in the rate of alcohol metabolism are accounted for by including time to peak TAC reading in the equation. The relationship between the predicted and observed BrAC values were high overall but varied depending on the number of drinks consumed. Specifically, correlation was near zero in the one drink condition but significantly increased at higher drink levels. These results suggest Equation 1 can be used to reliably predict BrAC when an individual has consumed at least 2 standard drinks, indicating TAC data would be an appropriate substitute in research and clinical contexts where BrAC readings are undesirable or difficult to obtain or where continuous monitoring may be helpful.
Detection of drinking
A cutoff of 0.02 g/dl is commonly used by forensic alcohol detection devices, such as TAC and ignition interlock devices, to establish alcohol consumption. A report sponsored by the National Highway Traffic Safety Administration (NHTSA, 2007) created ROC curves to determine the minimum TAC readings on SCRAM and WrisTAS devices that reliably predicted alcohol consumption. They determined that a TAC reading of 0.02 g/dl provided optimal discrimination, though it should be noted this cutoff produced a 12.34% false positive rate with SCRAM devices. We determined that participants who had only one drink could reliably be discriminated from participants who drank more when we used a cutoff slightly lower than the results from the earlier report (i.e., 0.011 g/dl). The finding that this cutoff correctly classified nearly all participants in the current study suggests that lower TAC readings could be used to detect more than moderate alcohol use with a lower likelihood of false negatives. Using a slightly higher cutoff of 0.024 g/dl, we determined that participants who drank 1–2 drinks, an amount that could be described as moderate drinking, could be discriminated from those who consumed a larger number of drinks. This suggests that the use of this slightly higher cutoff could be used in situations where a lower level of alcohol use (e.g., less than 3 drinks) is the target of the research or clinical intervention, such as research on binge drinking and other problematic alcohol use patterns.
Summary and future directions
The present findings suggest TAC data is reliably related to alcohol consumption and has convergent validity with BrAC, a more commonly used measure of alcohol intake. Additionally, TAC monitoring has unique advantages over other methods of monitoring drinking behavior that can improve the quality of data obtained and decrease the interference of monitoring procedures with wearers’ normal behavior. Therefore, TAC monitors could be used in both clinical and research contexts where determining a range of blood alcohol levels may be necessary. Likely clinical and research applications for TAC monitors include patterns of problematic alcohol use and alcohol use disorder treatment. Research and clinical interventions focused on binge drinking typically describe moderate drinking as the preferred outcome, rather than complete abstinence (for review, see Carey et al., 2007). Because TAC monitors can discriminate between moderate alcohol use and binge drinking, they may be useful in situations where moderate drinking is encouraged. TAC monitor wearers can be provided with objective evidence that their drinking patterns are well outside the range of normal, healthy alcohol use, and they can learn to adjust their drinking to a more moderate level. The use of TAC monitors and tailored feedback might be a more palatable intervention than the more general information provided in interventions such as required alcohol education classes for individuals who engage in problematic drinking patterns, such as binge drinking, but are not necessarily seeking treatment.
For individuals who are seeking treatment for an alcohol use disorder, treatment is generally conducted in a graduated manner, with treatment being more intensive earlier in the episode and becoming less rigorous over time. There is a heightened risk of relapse at each decrease in treatment intensity, and monitoring a patient’s alcohol use via TAC would allow treatment providers to objectively detect alcohol use between visits and conduct timely interventions when necessary to stop initial lapses from developing into full-blown relapses. Additional research is needed to determine the utility of applying TAC monitoring to clinical settings, however this technology has the potential to revolutionize the treatment of alcohol use disorders by more effectively monitoring consumption outside of inpatient settings.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/pha
Because this correlation is computed across participants and drinking occasions, it reflects variability at both levels. Given the multilevel, non-independent nature of these data, the appropriate degrees of freedom for this correlation are not clear. Thus, we conducted no significance test of this correlation, but we believe that its magnitude speaks clearly without such a test.
References
- Ayala J, Simons K, Kerrigan S. Quantitative determination of caffeine and alcohol in energy drinks and the potential to produce positive transdermal alcohol concentrations in human subjects. Journal of Analytical Toxicology. 2009;33:27–33. doi: 10.1093/jat/33.1.27. [DOI] [PubMed] [Google Scholar]
- Bonomo YA, Bowes G, Coffey C, Carlin JB, Patton GC. Teenage drinking and the onset of alcohol dependence: A cohort study over seven years. Addiction. 2004;99:1520–1528. doi: 10.1111/j.1360-0443.2004.00846.x. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conigrave KM, Davies P, Haber P, Whitfield JB. Traditional markers of excessive alcohol use. Addiction. 2003;98(Suppl. 2):31–43. doi: 10.1046/j.1359-6357.2003.00581.x. [DOI] [PubMed] [Google Scholar]
- Davidson D, Camara P, Swift R. Behavioral Effects and Pharmacokinetics of Low-Dose Intravenous Alcohol in Humans. Alcoholism: Clinical and Experimental Research. 1997;21:1294–1299. [PubMed] [Google Scholar]
- Dawson D. Gender differences in the risk of alcohol dependence: United States, 1992. Addiction. 1996;91:1831–1842. [PubMed] [Google Scholar]
- Dawson DA. Drinking patterns among individuals with and without DSM-IV alcohol use disorders. Journal of Studies on Alcohol. 2000;61:111–120. doi: 10.15288/jsa.2000.61.111. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Li TK. Quantifying the risks associated with exceeding recommended drinking limits. Alcoholism: Clinical and Experimental Research. 2005;29:902–908. doi: 10.1097/01.alc.0000164544.45746.a7. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: State of the science and challenges for research. Addiction. 2003;98:1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- DHHS, Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Washington, D.C.: U.S. Government Printing Office; 2002. [Retrieved September 23, 2011]. Results from the 2001 National Household Survey on Drug Abuse: Volume I. Summary of National Findings. (Office of Applied Studies, NHSDA Series H-17 ed.) (BKD461, SMA 02-3758), from http://www.oas.samhsa.gov/nhsda/2k1nhsda/vol1/Chapter3.htm. [Google Scholar]
- Dufour MC. What is moderate drinking? Defining “drinks” and drinking levels. Alcohol Research and Health. 1999;23:5–14. [PMC free article] [PubMed] [Google Scholar]
- Dumett MA, Rosen IG, Sabat J, Shaman A, Tempelman L, et al. Deconvolving an estimate of breath measured blood alcohol concentration from biosensor collected transdermal ethanol data. Applied Mathematics and Computation. 2008;196:724–743. doi: 10.1016/j.amc.2007.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan AZ, Russel M, Naimi T, Li Y, Liao Y, et al. Patterns of alcohol consumption and metabolic syndrome. Journal of Clinical Endrocrinology and Metabolism. 2008;93:3833–3838. doi: 10.1210/jc.2007-2788. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Giles HG, Renaud GE, Meggiorini S, Israel Y. New instrument using gas sensors for the quantitative analysis of ethanol in biological liquids. Alcoholism: Clinical and Experimental Research. 1986;10:521–525. doi: 10.1111/j.1530-0277.1986.tb05135.x. [DOI] [PubMed] [Google Scholar]
- Giles HG, Meggiorini S, Renaud GE, Thiessen JJ, Vidins EI, et al. Ethanol vapor above skin: determination by a gas sensor instrument and relationship with plasma concentration. Alcoholism: Clinical and Experimental Research. 1987;11:249–253. doi: 10.1111/j.1530-0277.1987.tb01300.x. [DOI] [PubMed] [Google Scholar]
- Guillot C, Bullock J, Fanning J, McCloskey M, Berman M. Effects of alcohol on tests of executive functioning in men and women: A dose response examination. Experimental and Clinical Psychopharmacology. 2010;18:409–417. doi: 10.1037/a0021053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzman D. The Behavioral Risk Factor Surveillance System. In: Blumenthal D, DiClemente R, editors. Community-based health research: Issues and methods. New York: Springer Publishers; 2003. pp. 115–131. [Google Scholar]
- Knibbe RA, Bloomfield K. Alcohol consumption estimates in surveys in Europe: Comparability and sensitivity for gender differences. Substance Abuse. 2001;22:23–38. doi: 10.1080/08897070109511443. [DOI] [PubMed] [Google Scholar]
- Marques PR, McKnight AS. Field and laboratory alcohol detection with 2 types of transdermal devices. Alcoholism: Clinical and Experimental Research. 2009;33:703–711. doi: 10.1111/j.1530-0277.2008.00887.x. [DOI] [PubMed] [Google Scholar]
- Midanik L. Over-reports of recent alcohol consumption in a clinical population: A validity study. Drug and Alcohol Dependence. 1982;9:101–110. doi: 10.1016/0376-8716(82)90055-2. [DOI] [PubMed] [Google Scholar]
- Midanik LT. Perspectives on the validity of self-reported alcohol use. British Journal Of Addiction. 1989;84:1419–1423. doi: 10.1111/j.1360-0443.1989.tb03920.x. [DOI] [PubMed] [Google Scholar]
- Neumann T, Spies C. Use of biomarkers for alcohol use disorders in clinical practice. Addiction. 2003;98(suppl 2):81–91. doi: 10.1046/j.1359-6357.2003.00587.x. [DOI] [PubMed] [Google Scholar]
- Nezlek JB. Multilevel modeling in research on personality. In: Robins R, Fraley RC, Krueger R, editors. Handbook of research methods in personality psychology. New York, NY: Guilford; 2007. pp. 502–523. [Google Scholar]
- NIAAA. NIAAA Council Approves Definition of Binge Drinking. NIAAA Newsletter. 2004 Winter;No. 3:3. [Google Scholar]
- NHTSA. Evaluating Transdermal Alcohol Measuring Devices. [Accessed on November 22, 2011];2007 from http://www.nhtsa.gov/DOT/NHTSA/Traffic%20Injury%20Control/Articles/Associated%20Files/810875.pdf.
- Norberg A, Jones AW, Hahn RG, Gabrielsson JL. Role of variability in explaining ethanol pharmacokinetics: research and forensic applications. Clinical Pharmacokinetics. 2003;42:1–31. doi: 10.2165/00003088-200342010-00001. [DOI] [PubMed] [Google Scholar]
- Okosun IS, Seale JP, Daniel JB, Eriksen MP. Poor health is associated with episodic heavy alcohol use: Evidence from a national survey. Public Health. 2005;119:509–517. doi: 10.1016/j.puhe.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Peterson K. Biomarkers for alcohol use and abuse: A summary. Alcohol Research & Health. 2004;28:30–37. [PMC free article] [PubMed] [Google Scholar]
- Pizon AF, Becker CE, Bikin D. The clinical significance of variations in ethanol toxicokinetics. Journal of Medical Toxicology. 2007;3:63–72. doi: 10.1007/BF03160911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poikolainen K, Podkletnova I, Alho H. Accuracy of quantity-frequency and graduated frequency questionnaires in measuring alcohol intake: Comparison with daily diary and commonly used laboratory markers. Alcohol and Alcoholism. 2002;37:573–576. doi: 10.1093/alcalc/37.6.573. [DOI] [PubMed] [Google Scholar]
- Polich J. The validity of self-reports in alcoholism research. Addictive Behaviors. 1982;7:123–132. doi: 10.1016/0306-4603(82)90037-5. [DOI] [PubMed] [Google Scholar]
- Powell-Griner E, Anderson JE, Murphy W. State- and sex-specific prevalence of selected characteristics- Behavioral Risk Factor Surveillance System, 1994 and 1995. MMWR CDC Surveillance Summary. 1997;46:1–31. [PubMed] [Google Scholar]
- Robin RW, Long JC, Rasmussen JK, Albaugh B, Goldman D. Relationship of binge drinking to alcohol dependence, other psychiatric disorders, and behavioral problems in an American Indian tribe. Alcoholism: Clinical and Experimental Research. 1998;22:518–523. [PubMed] [Google Scholar]
- Sakai JT, Mikulich-Gilbertson SK, Long RJ, Crowley TJ. Validity of transdermal alcohol monitoring: Fixed and self-regulated dosing. Alcoholism: Clinical and Experimental Research. 2006;30:26–33. doi: 10.1111/j.1530-0277.2006.00004.x. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, Maggs J. Developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. Journal of Studies on Alcohol. 2002;14S:54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, O'Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: Trajectories of frequent binge drinking during the transition to young adulthood. Journal of Studies on Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Sillanaukee P. Laboratory markers of alcohol abuse. Alcohol and Alcoholism. 1996;31:613–616. doi: 10.1093/oxfordjournals.alcalc.a008199. [DOI] [PubMed] [Google Scholar]
- Swift RM. Transdermal alcohol measurement for estimation of blood alcohol concentration. Alcoholism: Clinical and Experimental Research. 2000;24:422–423. [PubMed] [Google Scholar]
- Swift RM. Direct measurement of alcohol and its metabolites. Addiction. 2003;98(Suppl2):73–80. doi: 10.1046/j.1359-6357.2003.00605.x. [DOI] [PubMed] [Google Scholar]
- Swift RM, Martin C, Swette L, LaConti A, Kackley N. Studies on a wearable, electronic, transdermal alcohol sensor. Alcoholism: Clinical and Experimental Research. 1992;16:721–725. doi: 10.1111/j.1530-0277.1992.tb00668.x. [DOI] [PubMed] [Google Scholar]
- Thierauf A, Halter CC, Rana S, Auwaerter V, Wohlfarth A, et al. Urine tested positive for ethyl glucuronide after trace amounts of ethanol. Addiction. 2009;104:2007–2012. doi: 10.1111/j.1360-0443.2009.02722.x. [DOI] [PubMed] [Google Scholar]
- Wagenaar AC, Wolfson M. Deterring sales and provision of alcohol to minors: A study of enforcement in 295 counties in four states. Public Health Reports. 1995;110:419–427. [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, Castillo S. Health and behavioural consequences of binge drinking in college: A national survey of students at 140 campuses. Journal of the American Medical Association. 1994;272:1672–1677. [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. Binge drinking and the American college student: What's five drinks? Psychology of Addictive Behaviors. 2001;15:287–291. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]
- Widmark EMP. Principles and Applications of Medicolegal Alcohol Determination. Davis, CA: Biomedical Publications; 1981. [Google Scholar]