Abstract
Coronary computed tomographic angiography (CCTA) is emerging as a key non-invasive method for assessing cardiovascular risk by measurement of coronary stenosis and coronary artery calcium (CAC). New advancements in CCTA technology have led to the ability to directly identify and quantify the so-called “vulnerable” plaques that have features of positive remodeling and low density components. In addition, CCTA presents a new opportunity for noninvasive measurement of total coronary plaque burden that has not previously been available. The use of CCTA needs also to be balanced by its risks and, in particular, the associated radiation exposure. We review current uses of CCTA, CCTA’s ability to measure plaque quantity and characteristics, and new developments in risk stratification and CCTA technology. CCTA represents a quickly developing field that will play a growing role in the non-invasive management of cardiovascular disease.
Keywords: Coronary Computed Tomographic Angiography, CT, Atherosclerosis, Plaque, Non-Calcified, Acute Coronary Syndrome, Vulnerable Plaque, Spotty Calcification, Coronary Artery Calcium, Reconstruction
Introduction
Coronary artery disease (CAD) remains the leading cause of morbidity and mortality worldwide despite major pharmacologic and risk stratification advancements over the last two decades.(1) In 30–50 % of patients, the first sign of CAD is presentation with acute myocardial infarction.(2) Multiple studies have linked non-calcified atheroma to adverse outcomes.(3, 4) Interestingly, patients who experience acute MI are generally found to have previous sub-acute plaque ruptures prior to their major event.(5, 6) Therefore, the detection of these vulnerable plaques may allow for ideal risk stratification prior to a severe CAD outcome. Recent technological innovations in coronary computed tomography angiography (CCTA) have improved imaging resolution such that CCTA can now provide both visualization of the coronary lumen, and identification of at-risk non-calcified plaque.(7–10) The reference standard diagnostic tool for coronary stenosis is quantitative coronary angiography (QCA), while intravascular ultrasound (IVUS) is the standard for investigation of in-vivo intracoronary plaque characteristics. However, both modalities are unsuitable for screening purposes, as they are invasive and expensive. Although CCTA currently does not carry the spatial resolution of IVUS, it is non-invasive and technological increases have improved speed and resolution while decreasing radiation exposure.(11–14) These properties make CCTA an ideal screening modality for genetically susceptible and intermediate-risk patients, as well as a plausible method to quantitatively track the utility of atherosclerosis treatment.(15, 16)
Accurate analysis of plaque characteristics by CCTA would allow for improved risk stratification, measurement of response to therapy, and understanding of genetic markers of disease. This review will focus on CCTA in the context of non-calcified plaque, specifically: 1) characteristics and epidemiology of vulnerable plaques, 2) the ability of CCTA to identify, quantify, and assess plaque characteristics, and 3) recent technological improvements and future directions in CCTA.
Current Methods of Risk Stratification by Coronary Computed Tomographic Angiography
Technological advancements in CCTA have resulted in increasing diagnostic capability as well as an accelerating trend in utilization. CCTA is well validated for analysis of coronary artery calcium while more sophisticated techniques for plaque burden and composition remain under development.
Coronary Artery Calcium Score
Currently, CT is used to assess coronary artery calcium (CAC) score, which has been successfully used as an independent predictor of negative CAD events such as myocardial infarction (MI), revascularization, and mortality.(17–19) Detrano et al.’s study from the multiethnic study of atherosclerosis (MESA) has expanded CAC’s applicability to multiple ethnic groups including white, black, Hispanic, and Chinese. Doubling the CAC score increased the risk of a cardiac event by 18–39%. No major differences were seen between ethnic groups in the predictive ability of CAC score.(20) Additionally, CAC has been shown to add incremental value to a number of the standard measurements of cardiac risk such as JUPITER and Framingham risk scores. Blaha et al. found that in a cohort of MESA patients with CAC score >0, and meeting JUPITER inclusion criteria, the five-year number-needed-to-treat (NNT) to prevent cardiovascular disease (stroke and MI and complications) was only 30.(21) In the Heinz Nixdorf Recall Study, CAC was used to correctly reclassify patients with intermediate cardiac risk by Framingham Risk Score, resulting in a net reclassification index (NRI) of 21.7% to a low risk category (determined by CAC<100) and 30.6% to a higher risk category (determined by CAC≥400).(22) A study of the MESA population by Polonsky et al. found a similar NRI for CAC score on top of traditional risk factors (age, gender, tobacco, blood pressure, cholesterol, and ethnicity), at an overall rate of 25%.(23) However, while CAC appears to be an excellent surrogate marker for presence of disease, calcification of atherosclerotic plaque is thought to represent the endpoint of plaque maturation and lesion stabilization. Heavily calcified plaque is not the typical culprit lesion implicated in acute coronary syndrome.
Low CAC scores appear to be insufficient to fully assess risk. Multiple studies of patients with a CAC score of 0 have confirmed the presence of NCP and significant coronary artery stenosis, with prevalence of 11–13% and 0.9–3.7% respectively and severe stenosis (>70% luminal narrowing) seen in 0.4–1.5%.(24–27) CAC score of 0 has only a 45% sensitivity to predict the absence of ≥50% stenosis.(28) Additionally, within approximately 20% of asymptomatic patients with cardiac risk factors and no detectable CAC, significant stenosis is present. Within almost one third of these patients, these stenoses result in ischemia.(29) These studies show that there is a significant at-risk population that is unable to be diagnosed by CAC and traditional risk factors alone.
Measurement of Coronary Artery Plaque Stenosis by CCTA
In 2008, three major prospective multi-center trials marked the establishment of CCTA as a technology that could equal or eventually surpass invasive angiography for determining the degree of coronary artery stenosis. These three trials (CORE-64, ACCURACY, and Meijboom et al.) compared CCTA to QCA with sensitivities/specificities of 85%/90%,(30) 95%/83%,(31) and 99%/64%,(32), respectively. These multi-center trials that offered comparison to invasive angiography establish the diagnostic capability of CCTA. In general, these trials support the concept of the use of CCTA for the evaluation of patients at intermediate risk of coronary artery disease. For patients at high risk, CCTA may be unnecessary since invasive angiography serves to diagnose and treat in the same setting.
In addition to angiography, the degree of coronary stenosis by CCTA has been compared to IVUS. In a recent meta-analysis, Voros et al. identified 33 studies comparing CCTA to IVUS. They showed that CCTA was excellent for detection of coronary plaques (sensitivity 90%, specificity 92%), with increased accuracy with improving scanner technology. CCTA slightly overestimated lumen area (0.46 mm2 p=0.005) compared to IVUS, but there were no significant differences between plaque area, volume, weighted mean difference of volume, and percent area stenosis.(33) Thus, CCTA’s ability to identify plaque in the coronary arteries even beyond that which causes stenosis is well established.
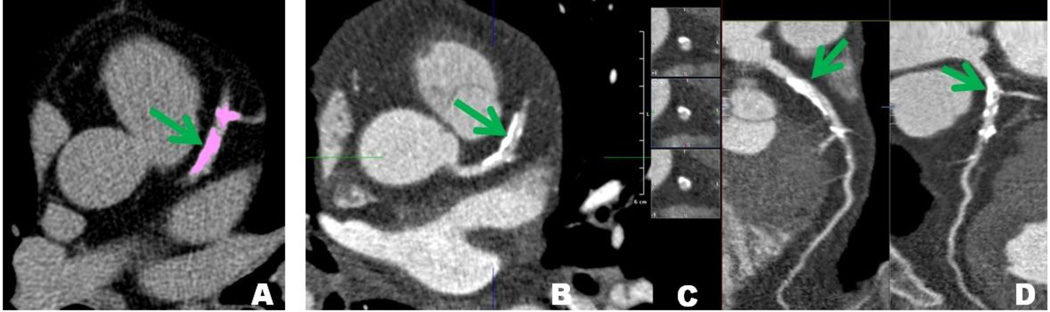
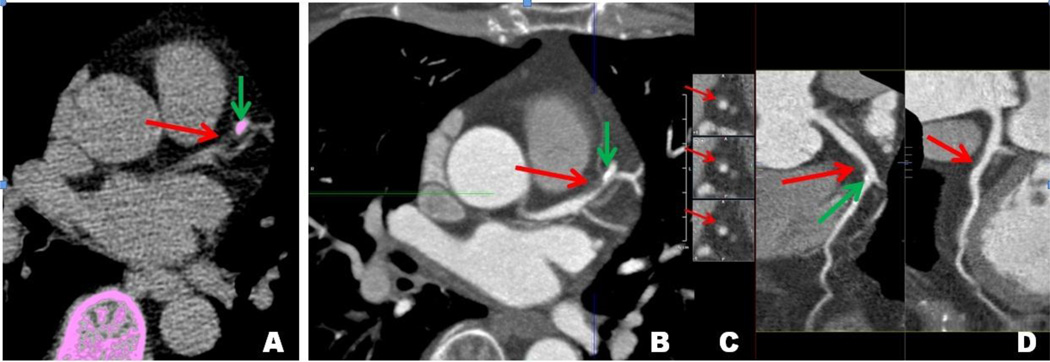
Beyond detection of plaque, CCTA has shown promise in characterizing the type of plaque that is present. In our laboratory using Vital Images software (Vitrea fX 6.1), the total amount of plaque can be determined by a semi-automated method (Sureplaque) that detects the inner and outer vessel walls over a length of the coronary artery. Area between inner and outer vessel walls is counted as plaque. Plaque burden is calculated by normalizing the volume of plaque within the vessel by the length of the vessel. In this system, an artery that appears normal, without visually identifiable plaque, had a total plaque burden (TPB) of approximately 6.5–7.5 mm2. Patients with increased amounts of plaque (eg figures 1a and 1b) have larger scores. The total plaque is further divided by the software into several components by HU density (soft plaque: −100–29; fibrous plaque: 30–149; calcified plaque: 150–1300). The subdivided plaque burdens in normal-appearing vessels are soft plaque burden (SPB) of <2 mm2, fibrous plaque burden (FPB) of <4 mm2, and calcified plaque burden (CPB) of <2 mm2. Figure 1a shows visualization of calcification within coronary arteries using different CCTA views, with the patient’s corresponding plaque burdens. The use of CCTA for characterizing plaque is discussed in greater detail below.
Figure 1.
a. Calcified coronary arteries. A) Agatston calcium score axial view. B) Filtered Back-projection axial view. C) Arterial cross section view. D) Orthogonal curved multiplanar reconstruction view. Green arrows: Calcified plaque in left anterior descending (LAD) artery visualized in multiple modalities. This patient’s CAC score was 1982. Total plaque burden (TPB) is 11.0; soft plaque burden (SPB) is 1.9; fibrous plaque burden (FPB) is 4.4; calcified plaque burden (CPB) is 4.7.
b. Coronary arteries exhibiting non-calcified plaque. A) Agatston calcium score axial view. B) Filtered Back-projection axial view. C) Arterial cross section view. D) Orthogonal curved multiplanar reconstruction view. Green arrows: Mixed LAD plaque.. Red arrows: Significant non-calcified plaque in LAD proximal to calcified segment. The patient’s CAC score is 54. Total plaque burden (TPB) is 10.1; Soft plaque burden (SPB) is 1.7; Fibrous plaque burden (FPB) is 5.3; Calcified plaque burden (CPB) is 3.1.
Plaque characterization with CCTA
Overview: Vulnerable Plaques and Acute Coronary Syndromes
Culprit lesions responsible for rupture, thrombosis, and acute MI are typically larger soft plaques with incomplete or no calcification representing a different segment of disease from CAC.(34–36) These plaques were found to be 1) lipid laden and non-calcified plaques (NCP), 2) thin-capped, and 3) positively remodeled(37–39) implying that vulnerable, pre-rupture plaques would share the same characteristics.
The clarity of the term “non-calcified plaque” has suffered greatly from its dual use as a descriptive and definitive phrase. Early studies focusing on CCTA alone have often defined NCP as any discernable object within the vessel wall with enhancement greater than the wall structures but less than the lumen,(26, 40, 41) effectively defining NCP as any plaque that is not completely calcified. Recent SCCT guidelines have recommended subdividing plaque type into calcified, non-calcified, or mixed.(42) IVUS comparison studies further subdivide plaque categories with definitions of NCP excluding plaques with minor calcified elements within.(4, 43) Histological comparison studies subdivide plaques by the Stary classification system, with NCP synonymous with corresponding Stary stages.(44) For the purposes of this review, we will refer to NCP as plaques that are not completely calcified, encompassing both SCCT categories of “non-calcified plaque” and “mixed plaque,” and corresponding with the characteristics of the culprit lesions discussed above.
While many studies have attempted to correlate plaque sub-types with risk factors, results have been highly inconsistent. States generally found to be associated with NCP include typical cardiac risk factors such as: hypertension,(45, 46) smoking,(45–47) obesity,(46, 48) gender,(47) diabetes,(47) CAC score,(49) high-sensitivity CRP,(50) and apolipoprotein A1;(50) as well as non-typical factors such as: pericardial fat volume,(51) epicardial fat volume,(52) and inflammatory monocyte subsets.(53) It is important to note that not all studies found statistical strength of association for these factors.(48) The variability in correlating NCP with known cardiovascular risk factors suggests a significant need for prospectively designed studies.
Recent evidence suggests that CAC is not a perfect indicator of atherosclerotic burden. In patients with zero CAC score, the rate of obstructive NCP in asymptomatic populations is estimated to be <1%. However, in symptomatic patients this percentage is much higher, suggesting that there are at-risk population subsets that would benefit from NCP screening.(26) In fact, elevated NCP burden is present in almost all patients who present with ACS.(38, 39, 54) A study by Motoyama et al. found that culprit lesions were comprised of NCP in 79% of ruptured lesions causing ACS, whereas stable lesions causing typical angina were comprised of NCP in only 9%.(55) The prospective multicenter ACCURACY trial showed that plaque composition by CCTA is related to stenosis severity by QCA; mixed plaques showed a higher rate of stenoses ≥70% (68%) compared with completely non-calcified and calcified plaque (28% and 3.6%).(56) Other studies demonstrated higher proportions of mixed plaques in patients with ACS vs. stable CAD, as well as higher proportions of NCP.(4) These studies suggest that NCP represents a clinically-significant type of measurable pathology, associated with both ACS and stenosis, and not adequately addressed by CAC score.
Coronary Computed Tomography and the Ability to Characterize Plaque Types
Ever since early multi-detector coronary CTA, researchers have been interested in the ability to non-invasively differentiate plaque types. Comparison of 4-detector row CT with histology by Becker et al. noted that CCTA could assess significant attenuation differences between lipid-rich and fibrous-rich non-calcified plaque (47±9 and 104±28 HU, respectively; p<0.01),(57). Further developments in CT technology enabled more precise differentiation between plaque types with 16-slice MDCT, although microcalcification within plaques remained difficult to classify.(58–60)
As imaging technology has improved, ex-vivo histological comparisons have become less prevalent. Despite concerns about accuracy,(61, 62) IVUS has become the gold standard for intravascular plaque analysis.(63, 64) Early comparisons of CCTA with IVUS showed promise for characterization and quantification of plaques, but results suffered from poor scan resolution and reproducibility, (65–68) especially outside of the proximal coronary tree segments.(69) Improvements in CT technology in more recent studies resulted in improving ability to quantify and distinguish plaque types,(4, 43, 70–72) especially if the measured areas were limited to regions with high scan quality, without blurring or heavy calcification.(73) Figure 1b shows CCTA visualization of calcified and non-calcified plaque within coronary arteries.
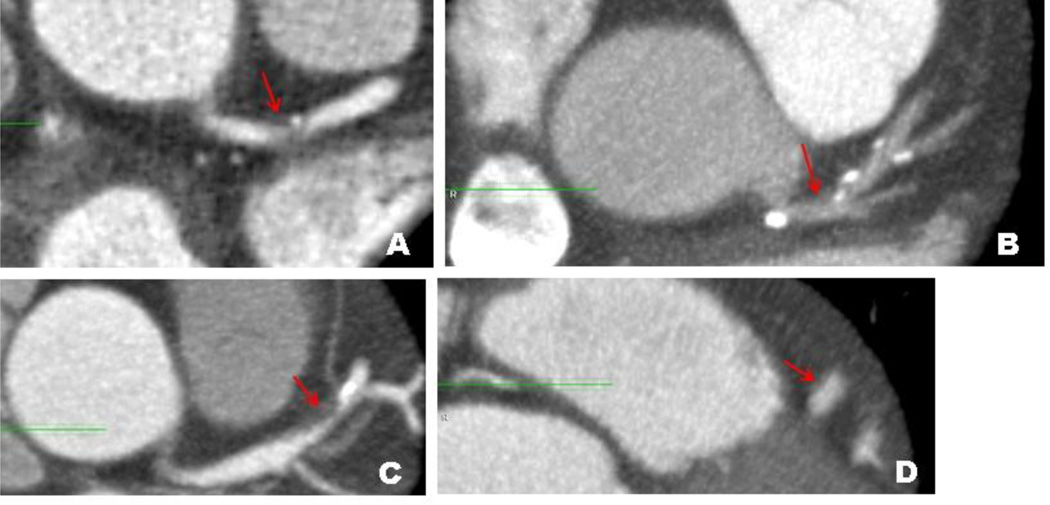
Multiple studies have attempted to determine distinct HU ranges corresponding to different histological plaque types. Mean HU densities for lipid-rich soft plaques range from 14–75 HU,(66, 74) fibrous plaques range from 67–149 HU,(75, 76) and calcified plaques range from 135–1089 HU.(77, 78) Table 1 summarizes recent studies correlating attenuation with plaque characteristics. Figure 2 shows lipid-rich and fibrous soft plaques visualized on CCTA.
Table 1.
Studies correlating attenuation level with plaque characteristics.
| First Author |
Year | Citation | CT | Comparison | N (lesions) | Soft/Lipid- Rich/hypoechoic (HU) |
Intermediate/Fibrous /hyperechoic (HU) |
Calcified (HU) |
|---|---|---|---|---|---|---|---|---|
| Kopp | 2001 | (65) | 4-MDCT | IVUS | 6 | 6 ± 28 and −5 ± 25 | 83 ± 17 and 51 ± 19 | 489 ± 372 and 423 ± 111 |
| Schroeder | 2004 | (44) | 4-MDCT | Histology | 17 | 42 ± 22 (Stary III/IV) | 70 ± 21 (Stary V) | 715 ± 328 (Stary VII) |
| Sakakura | 2006 | (119) | 16-MDCT | IVUS | 23 | 50.6 ± 14.8 | 131 ± 21.0 | 721 ± 231 |
| Becker | 2003 | (57) | 4-MDCT | Histology | 33 | 47 ± 9 (Stary IV and Va) | 104 ± 28 | ----------------- |
| Schroeder | 2001 | (66) | 4-MDCT | IVUS | 34 | 14 ± 26 | 91 ± 21 | 419 ± 194 |
| Xiao | 2007 | (120) | 16-MDCT | Histology | 38 | 53 ± 12 | 106 ± 17 | 429 ± 94 |
| 64-MDCT | Histology | 38 | 51 ± 13 | 110 ± 19 | 435 ± 87 | |||
| Hur | 2009 | (72) | 64-MDCT | IVUS | 61 | 54 ± 13 | 82 ± 17 | 392 ± 155 |
| Chopard | 2010 | (62) | 64-MDCT | Histology | 83 | 70 ± 41 | 83 ± 35 | 966 ± 473 |
| IVUS | 83 | 67 ± 31 | 84 ± 40 | 724 ± 564 | ||||
| Iriart | 2007 | (121) | 16-MDCT | IVUS | 84 | 38 ± 33 | 94 ± 44 | 561 ± 216 |
| Carrascosa | 2003 | (76) | 4-MDCT | IVUS | 156 | 75.73 ± 44.30 | 148.61 ± 36.54 | 449.07 ± 221.4 |
| Ferencik | 2006 | (77) | 16-MDCT | OCT | 164 | 29 ± 43 | 101 ± 21 | 135 ± 199 |
| Viles-Gonzalez | 2004 | (122) | 16-MDCT | Histology (Non-human) | 182 | 51 ± 25 | 116 ± 27 | ----------------------- |
| Kitagawa | 2007 | (75) | 64-MDCT | IVUS | 202 | 18 ± 17 | 67 ± 21 | ----------------------- |
| Pohle | 2007 | (123) | 16-MDCT | IVUS | 252 | 58 ± 43 | 121 ± 34 | ----------------------- |
| Carrascosa | 2006 | (74) | 4-MDCT | IVUS | 276 | 71.5 ± 32.1 | 116.3 ± 35.7 | 383.3 ± 186.1 |
| Leber | 2004 | (67) | 16-MDCT | IVUS | 450 | 49 ± 22 | 91 ± 22 | 391 ± 156 |
| Choi | 2008 | (82) | 64-MDCT | IVUS | 80 | 41.3 ± 26.4 (≥10% necrotic core volume) | 93.1 ± 37.5 (<10% necrotic core volume) | |
| 44 (26–63) (Stary V); | ||||||||
| Galonska | 2008 | (78) | 16-MDCT | Histology | 195 | 50 (33–59) (Stary IV) | 40 (36–67) (Stary VI); 67 (37–124) (Stary VIII) | 1089 (333–1944) (Stary VII) |
| 34 ± 19 (Stary V); 104 | ||||||||
| Leschka | 2010 | (59) | DSCT | Histology | 245 | 55 ± 12 (Stary IV) | ± 84 (Stary VI); 91 ± 16 (Stary VIII) | 501 ± 402 (Stary VII) |
| 51 ± 25 | 92 ± 59 | 968 ± 494 |
Figure 2.
Filtered back-projection reconstructions of coronary arteries exhibiting non-calcified plaque indicated by red arrows, with occasional calcification (not marked). A) Patient with plaque in left main coronary artery. HU of plaque is 5, consistent with lipid-rich plaque. Total plaque burden (TPB) is 7.9; soft plaque burden (SPB) is 1.5; fibrous plaque burden (FPB) is 3.6; calcified plaque burden (CPB) is 2.8. B) Patient with plaque in left main coronary artery. HU of plaque is 29, consistent with lipid-rich plaque. TPB is 6.5; SPB is 2.6; FPB is 3.5; CPB is 0.4. C) Patient with plaque in left anterior descending artery. HU of plaque is 85, consistent with fibrous non-calcified plaque. TPB is 10.1; SPB is 1.7; FPB is 5.3; CPB is 3.1. D) Patient with plaque in left anterior descending artery. HU of plaque is 85, consistent with fibrous non-calcified plaque. TPB is 8.7; SPB is 1.7; FPB is 4.9; CPB is 2.1.
Comparison is difficult between these studies, due to different modes of classification for CCTA-determined plaque types (non-calcified/mixed/calcified, fatty/fibrous/calcified, hyperechoic/hypoechoic/calcified, or stratification by Hounsfield units), which do not precisely correspond to the different modes of IVUS classification (soft/intermediate/calcified, calcified/mixed/fibrous/soft, fatty/fibrous/calcified, fibrotic/fibro-fatty/necrotic-core/calcified) or histological classification. Despite the need for future improvement of CCTA, there is a clear trend that improving technology continues to close the gap to provide a non-invasive, cost-saving alternative to expensive and invasive gold standard measurements.
CCTA and the Ability to Identify Vulnerable Plaques
As our understanding of plaque histology has improved,(79) interest has risen in the ability of CCTA to identify particularly-at-risk plaque structures. At risk plaques tend to have low x-ray attenuation (Hounsfield unit) values. Alternatively, soft plaque may had specific anatomic characteristics such as the “napkin-ring sign” that indicate a specific morphology.
CCTA quantification of plaque types subdivided by SCCT recommendation (non-calcified, calcified, partially calcified) shows excellent inter and intra-rater agreement.(80) While the categories lack the descriptive strength of pathology-based histological subtypes by Stary classification, CCTA and IVUS-based histology correspond well in some important respects. Highly vulnerable plaques such as thin-capped fibroatheromas (TCFA) are found in 32% of plaques classified as partially calcified by CCTA, versus 13% for “non-calcified,” and 8% for calcified.(43) Additionally, TCFA may be associated with the “napkin-ring sign” on CCTA, a ring-like enhancing lesion that has been implicated in rupture and ACS in multiple studies.(7–9) In these cases, the ring may be due to differential density of necrotic lipid core surrounded by thin fibrous material, as the lesion itself is typically associated with large plaques with necrotic lipid cores.(10)
More recent studies show a weak correlation between high density NCP and fibrous plaque tissue (R=0.47) as well as between low-density NCP and fibrofatty/necrotic core plaques (R=0.25), as noted in the ATLANTA I study using quantitative CCTA to IVUS.(81) Choi et al. demonstrated that plaques with greater than 10% necrotic core volume had significantly lower HU densities (41.3±26.4 vs 93.1±37.5) and significant correlations were found between HU density and percent necrotic core (r=−0.53) and fibrotic component (r=0.57), but not with fibrofatty component or calcium determined by IVUS. (82)
CCTA and the Ability to Identify Positive Remodeling
Positive remodeling, as described by Glagov et al.,(83), is the tendency of coronary arteries to undergo compensatory enlargement from early atherosclerosis. Positive remodeling is measured by dividing the cross sectional vessel wall area by a corresponding proximal and distal segment reference area or lesion area. While definition of the proximal and distal reference segments is somewhat subjective, the CCTA approach has been validated against IVUS (75, 84, 85) and has shown excellent reproducibility.(80) Positive remodeling has been associated with a high risk of ACS. (37, 38) Kitagawa et al. which showed that within NCP lesions, remodeling index was the only factor that correlated with culprit lesions causing ACS and non-culprit lesions within patients who had ACS due to plaque rupture at a different site.(86) Positive remodeling is presumed to be associated with inflammation and increased propensity for rupture. Negative, or constrictive remodeling, is associated with lesion stabilization and has been observed in plaques following statin treatment.(87)
More recent studies have examined the use of positive remodeling, which is easily measured by CCTA, as a surrogate marker for regions of vulnerable plaque. IVUS studies have demonstrated that positive remodeling is associated with increased intra-plaque lipid volume and decreased calcium and fibrous tissue, a composition typical for vulnerable plaque.(88, 89) This association is supported within the CCTA literature, as Schmid et al. demonstrated correlation between degree of remodeling and CT attenuation of plaque in a sample of 72 lesions. Positively-remodeled plaque attenuation had a significantly lower value than lesions displaying no or negative remodeling (59±22 HU versus 91±20HU, p<0.001).(90) Additionally, a study by Kroner et al demonstrated that thin capped fibroatheromas by IVUS were associated with 43% of positively-remodeled plaques by 64MDCT as compared to 4.8% of negatively remodeled lesions.(91) The authors concluded that CCTA positive remodeling was correlated with actual histological markers of plaque instability.
Future Directions in Coronary Computed Tomographic Angiography
Plaque characterization by CCTA has potential application for 1) assessing overall risk for primary prevention, 2) evaluation of ACS, and 3) following progression of disease and response to therapy. These topics are reviewed below.
Plaque assessment for primary prevention
There have been several studies looking at the prognostic value of plaque characteristics both individually and in addition to current modes of risk stratification. In 810 patients, Matsumoto et al. demonstrated that low attenuation plaque (HU <68) was associated with higher rates of major cardiac events over 2.9 years (OR:2.9 95%CI:1.2–6.7 p<0.05).(92) In a study of 517 patients referred for cardiac evaluation undergoing 16-slice MDCT and myocardial perfusion imaging, van Werkhoven et al showed that having two or more segments with completely non-calcified plaque was predictive of events (HR:5.0 95%CI:2.2–11.7 p<0.01) and that having three or more segments with mixed plaque was also predictive of events (HR:3.5 95%CI:1.5–8.1 p<0.005).(93) This same group was also followed for composite all-cause mortality, non-fatal MI, and unstable angina over a median follow-up of 22 months in 432 patients undergoing CAC and 6-slice CCTA. There was a significant incremental predictive value of CCTA in patients with a calcium score greater than 1000, particularly with regards to number of NCP’s (HR:1.3 95%CI:1.1–1.4 p=0.001) and mixed plaque-containing segments (HR:1.2 95%CI:1.0–1.4 p=0.039). The number of calcified segments was not predictive.(94)
More impressively, Ahmadi et al. recently showed that CCTA plaque type had significant predictive value in 1,102 symptomatic patients with non-obstructive (stenosis <50%) CAD followed over 78±12 months.(95) In this cohort, the rate of death increased in association with calcified plaque (1.4%) to mixed plaque (3.3%) to completely non-calcified plaque (9.6%). The risk-adjusted hazard ratio in patients with mixed plaque was 3.2 (95%CI1.3–8.0 p<0.001) and for completely non-calcified plaque the risk was twice as high at 7.4 (95%CI:2.7–20.1, p<0.001). These studies demonstrate that the presence of soft plaque and mixed plaque provided incremental value in predicting all-cause mortality over traditional measurements of risk.
Plaque assessment and acute coronary syndrome
Distinguishing between ACS and stable angina on presentation would allow for faster and more accurate treatment. Retrospective analysis of CCTA from patients presenting with ACS have shown differences between their plaque characteristics compared to those with stable angina. Volumetric plaque burden was assessed by 64-slice CCTA in 57 patients with NSTEMI compared to 19 with stable angina pectoris, finding that the mean HU density was lower in patients with NSTEMI (74 vs. 99HU p=0.02), and that the volume of calcified plaque and number of lesions with calcified plaque was decreased in NSTEMI. Stable angina patients had fewer segments with NCP, and positive remodeling was found in 19% of patients with NSTEMI as compared none in patients with stable angina.(96)
Two studies have looked at developing standardized scoring methods for detecting culprit lesions, which include plaque characteristics such as low attenuation, remodeling index, spotty calcification, and plaque volume. In one of these studies, Kim et al. combined plaque attenuation of ≤ 60 HU, remodeling index ≥1.05, and presence of NCP or spotty calcification to predict ACS patients with a sensitivity of 97.1% and specificity of 67.6%, ROC analysis showed an (AUC:0.908 p<0.001).(97) Ferencik et al. used presence of positive remodeling, spotty calcium, and stenosis length >4.5mm, finding that this was associated with OR 4.6, 95% CI 1.6 to 13.7 (AUC 0.824) for prediction of ACS over stable angina.(98)
Although prognosis before the onset of MI is ideal, using CCTA to stratify risk after diagnosis of ACS may also be of value. Stone et al. revealed that recurrence of a major cardiac event after treatment with percutaneous coronary intervention was attributed to a different, untreated vessel region almost half of the time. These untreated regions were associated with the typical characteristics of vulnerable plaque by IVUS,(3) therefore, if CCTA is able to identify co-existing vulnerable plaques, treatment decisions can be tailored to the patient’s individual risk. In a study of 312 patients, CCTA measurement of NCP volume in patients presenting with NSTEMI was a better predictor of future cardiac events over 16 months than clinical variables and left-ventricular ejection fraction (LVEF).(99) Watabe et al. showed that CCTA-defined culprit lesions prior to percutaneous coronary intervention may be predictive of myocardial necrosis and significantly greater post-procedural risk.(100)
Plaque assessment to monitor treatment progression
There is little biological evidence that statins are able to reduce the burden of calcified plaque, but earlier studies magnetic resonance imaging studies of the aorta and carotid arteries have shown reduced plaque burden in response to intensive statin treatment. (101–108) With CCTA, a number of studies have showed decreased NCP with treatment.(16, 109–111) Burgstahler et al. demonstrated that initiation of atorvastatin therapy reduces NCP volumes (24±13% p<0.05) but does not impact calcium scoring (Agatston score: 261±301 vs. 282±360 p>0.05) or total plaque burden (0.15±0.11ml vs. 0.13± 0.075ml p>0.05).(112) Inoue et al. used serial CCTA to track decreases in plaque volume in response to fluvastatin treatment, and found decreases in both low attenuating plaque volume (4.9 ± 7.8 vs. 1.3 ± 2.3 mm3, p = 0.01) and total plaque volume (92.3 ± 37.7 vs. 76.4 ± 26.5 mm3, p < 0.01).(16) While specific therapy to prevent NCP rupture has yet to be discovered, there is evidence that statins may cause constrictive remodeling and increased plaque stability, suggesting that the decrease in plaque volume in the studies above may be protective against ACS events.(87)
Technical issues for plaque characterization with CCTA
Radiation Reduction in Coronary CTA
Accurate assessment of coronary plaque by CCTA requires high spatial resolution and excellent contrast resolution. Unfortunately both “requirements” are associated with high radiation dose. In addition, the concept of CCTA monitoring of plaque healing implies multiple CCTA examinations with further radiation exposure. Already, CT use for non-cardiac applications represents the greatest contributor to medical radiation in the US which has now reached equivalence to natural background radiation.(113, 114) Radiation exposure associated with CCTA is especially concerning because of the widespread nature of coronary artery disease and high radiation doses that were used with early CT scanning devices. The sections below indicate recent developments that have allowed cardiac CT radiation exposure to transition from one of the highest dose to one of the lowest dose CT scanning applications.
CCTA presents a unique set of hurdles due to the necessity for high resolution images in an anatomical area predisposed towards significant motion artifacts. Widespread evaluation of CCTA began in 2004, with radiation dose estimates ranging from 9–21.4 mSv per scan(14) due to continual scanning throughout the cardiac cycle at maximum tube current and voltage with retrospective electrocardiogram (ECG) gating. ECG-based tube current modulation was subsequently introduced, where tube voltage was decreased by 75–96% when outside of diastole, resulting in a decrease to approximately 8–10 mSv per scan.(13) Low tube voltage protocols were the next development in patients with BMI<25, with reduction of tube voltage from 120 kV to 100 kV, resulting in a radiation dose of approximately 6.5 mSv.(13) Prospective ECG triggered gating, or “Step-and-shoot” technology, where the x-ray tube is only activated during pre-determined moments in diastole effectively took the ECG-based tube current modulation technology to its limit. While this procedure generally was only useful in patients with lower heart rates, radiation dose was decreased to 1.5–4 mSv depending on the tube voltage protocol that was used.(13) Most recently, development and improvement of multidetector CT (MDCT) with large scale detector systems has allowed single-beat acquisition of CCTA for patients with heart rate <63 bpm and decreases in exposure to the 1 mSv range.(11, 13, 14)
Image Reconstruction in Coronary CTA
More recent innovations have focused in improvement of post-processing techniques through computationally intense algorithms that improve the clarity and quality of scans to compensate for decreased scan radiation.(115, 116) Classically, image reconstruction in CT has used a Filtered Back Projection (FBP) algorithm. This mode of reconstruction creates images by combining the multiple axial 2D back-projections generated by each gantry revolution and applying filters to increase contrast and compensate for the increased signal intensity at the center of the image. FBP relies on a few simplifying assumptions, idealizing the characteristics and interactions of the x-ray beam with the patient and the detector, although leading to some inaccuracies and artifacts. FBP has the benefit of being fast with low computational load, but suffers in scanning large patients, imaging at high resolution or in areas of high bone density (e.g. the pelvis) or using when low-dose technique.(117)
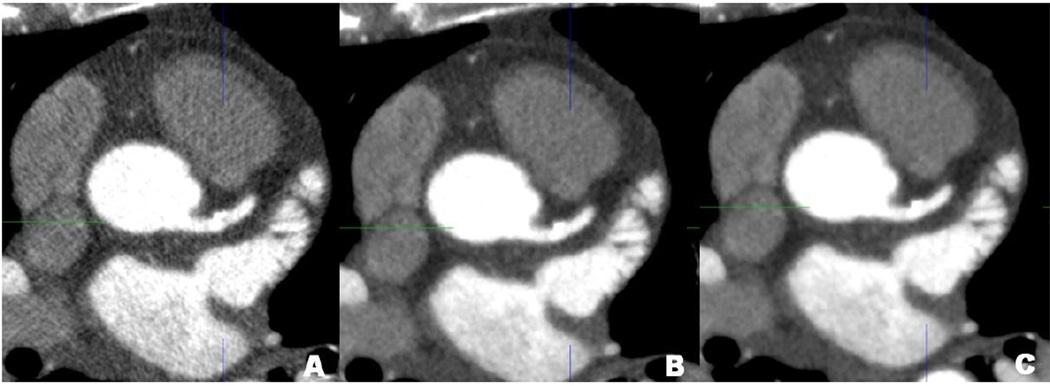
Iterative reconstruction refers to a repeated process of image reconstruction that draws the reconstructed image closer to an idealized model, creating a reconstruction with less noise and higher clarity. Figure 3 shows a comparison of FBP versus iterative reconstruction, showing decreased noise in the iterative reconstruction views. This approach can compensate for lower radiation dose, making sub-millisievert CCTA possible.(118) While based on similar reconstruction theory, these techniques are not exactly the same and the literature reveals subtle differences between all of these methods. The variety and range of new techniques for radiation dose reduction are defined in Table 2.
Figure 3.
Comparison of axial and arterial cross-sectional views using different reconstruction techniques from same data set. A) Filtered back-projection. B) Adaptive Iterative Dose Reduction, mild level. C) Adaptive Iterative Dose Reduction, standard level. Notable for increased incremental image quality, decreased noise and increased smoothness in higher levels of iterative dose reduction (right) versus traditional reconstruction by filtered back-projection (left).
Table 2.
Iterative reconstruction techniques for radiation dose reduction
| Abbreviation | Name | Company | # CCTA Studies | Conclusion | Citations |
|---|---|---|---|---|---|
| ASiR | Adaptive Statistical Iterative Reconstruction | GE Healthcare | 5 | 27% dose reduction versus FBP possible with equal image quality | (124–128) |
| iDose | iDose Iterative Reconstruction Technique | Philips Healthcare | 3 | Hypothetical 76% dose reduction, improved image quality over FBP in normal and low-dose protocols | (129–131) |
| IRIS | Iterative Reconstruction in Image Space | Siemens Medical Solutions | 2 | 68% dose reduction versus FBP with equivalent noise levels | (132, 133) |
| SAFIRE | Sonogram-Affirmed Iterative Reconstruction | Siemens Medical Solutions | 2 | 50% dose reduction versus FBP with improved image quality | (134, 135) |
| ADIR | Adaptive Iterative Dose Reduction | Toshiba Medical Systems Corporation | 1 | Dose reduction unknown, 42% noise reduction, 70% CNR improvement | (136) |
| MBIR | Model Based Iterative Reconstruction | GE Healthcare | 2 | Dose reduction unknown, ex vivo study shows increased image quality, 51–69% CNR increase over ASiR and FBP | (137, 138) |
Conclusion
New technological developments have expanded the ability of CCTA to elucidate aspects of cardiovascular disease previously only measurable through invasive modalities; however, concerns still remain about utilization and radiation exposure. New methods of reconstruction may allow CCTA to be performed with lower radiation dose and better image quality. Besides assessment of coronary stenosis, plaque composition and characteristics have begun to assume increasing importance. CCTA can thus combine features of stenosis detection by invasive angiography and plaque characterization by invasive ultrasound. Assessment of plaque by CCTA may be used to assess prognosis as well as to identify at risk plaques. Finally, the concept of medical therapy and monitoring of plaque healing and regression by CCTA has recently become possible using low radiation dose techniques.
Acknowledgments
Funded by the National Institutes of Health (NIH) Intramural program
This research was made possible through the National Institutes of Health (NIH) Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and generous contributions to the Foundation for the NIH from Pfizer Inc, The Leona M. and Harry B. Helmsley Charitable Trust, and the Howard Hughes Medical Institute, as well as other private donors. For a complete list, please visit the Foundation website at http://www.fnih.org/work/programs-development/medical-research-scholars-program).
Footnotes
Disclosure
No potential conflicts of interest relevant to this article were reported.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. Epub 2009/12/19. 10.1161/CIRCULATIONAHA.109.192667. PubMed PMID: 20019324. [DOI] [PubMed] [Google Scholar]
- 2.Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986;111(2):383–390. doi: 10.1016/0002-8703(86)90155-9. Epub 1986/02/01. PubMed PMID: 3946178. [DOI] [PubMed] [Google Scholar]
- 3.Stone GW, Maehara A, Lansky AJ, Bruyne Bd, Cristea E, Mintz GS, et al. A Prospective Natural-History Study of Coronary Atherosclerosis. The New England Journal of Medicine. 2011;364(3):226–235. doi: 10.1056/NEJMoa1002358. Epub January 20, 2011. PubMed Central PMCID: PMC21247313. [DOI] [PubMed] [Google Scholar]
- 4.Pundziute G, Schuijf JD, Jukema JW, Decramer I, Sarno G, Vanhoenacker PK, et al. Evaluation of plaque characteristics in acute coronary syndromes: non-invasive assessment with multi-slice computed tomography and invasive evaluation with intravascular ultrasound radiofrequency data analysis. Eur Heart J. 2008;29(19):2373–2381. doi: 10.1093/eurheartj/ehn356. Epub 2008/08/07. 10.1093/eurheartj/ehn356. PubMed PMID: 18682447. [DOI] [PubMed] [Google Scholar]
- 5.Rioufol G, Finet G, Andre-Fouet X, Rossi R, Vialle E, Desjoyaux E, et al. Multiple ruptures of atherosclerotic plaques in acute coronary syndrome. Endocoronary ultrasonography study of three arteries. Arch Mal Coeur Vaiss. 2002;95(3):157–165. Epub 2002/05/10. PubMed PMID: 11998329. [PubMed] [Google Scholar]
- 6.Rioufol G, Finet G, Ginon I, Andre-Fouet X, Rossi R, Vialle E, et al. Multiple atherosclerotic plaque rupture in acute coronary syndrome: a three-vessel intravascular ultrasound study. Circulation. 2002;106(7):804–808. doi: 10.1161/01.cir.0000025609.13806.31. Epub 2002/08/15. PubMed PMID: 12176951. [DOI] [PubMed] [Google Scholar]
- 7.Tanaka A, Shimada K, Yoshida K, Jissyo S, Tanaka H, Sakamoto M, et al. Non-invasive assessment of plaque rupture by 64-slice multidetector computed tomography--comparison with intravascular ultrasound. Circulation journal: official journal of the Japanese Circulation Society. 2008;72(8):1276. doi: 10.1253/circj.72.1276. [DOI] [PubMed] [Google Scholar]
- 8.Kashiwagi M, Tanaka A, Kitabata H, Tsujioka H, Kataiwa H, Komukai K, et al. Feasibility of noninvasive assessment of thin-cap fibroatheroma by multidetector computed tomography. JACC: Cardiovascular Imaging. 2009;2(12):1412–1419. doi: 10.1016/j.jcmg.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Maurovich-Horvat P, Hoffmann U, Vorpahl M, Nakano M, Virmani R, Alkadhi H. The napkin-ring sign: CT signature of high-risk coronary plaques? JACC Cardiovascular Imaging. 2010;3(4):440. doi: 10.1016/j.jcmg.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Seifarth H, Schlett CL, Nakano M, Otsuka F, Karolyi M, Liew G, et al. Histopathological correlates of the napkin-ring sign plaque in coronary CT angiography. Atherosclerosis. 2012 doi: 10.1016/j.atherosclerosis.2012.06.021. Epub 2012/07/10. 10.1016/j.atherosclerosis.2012.06.021. PubMed PMID: 22771191. [DOI] [PubMed] [Google Scholar]
- 11.Rybicki FJ. Lower radiation dose coronary CT angiography with new imaging technologies. The International Journal of Cardiovascular Imaging (formerly Cardiac Imaging) 2009;25:149–151. [Google Scholar]
- 12.McCollough CH, Bruesewitz MR, Kofler JM., Jr CT Dose Reduction and Dose Management Tools: Overview of Available Options1. Radiographics. 2006;26(2):503–512. doi: 10.1148/rg.262055138. [DOI] [PubMed] [Google Scholar]
- 13.Alkadhi H, Leschka S. Radiation dose of cardiac computed tomography–what has been achieved and what needs to be done. European Radiology. 2011;21(3):505–509. doi: 10.1007/s00330-010-1984-3. [DOI] [PubMed] [Google Scholar]
- 14.Raff GL. Radiation dose from coronary CT angiography: five years of progress. Journal of Cardiovascular Computed Tomography. 2010;4(6):365–374. doi: 10.1016/j.jcct.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Schmid M, Achenbach S, Ropers D, Komatsu S, Ropers U, Daniel WG, et al. Assessment of changes in non-calcified atherosclerotic plaque volume in the left main and left anterior descending coronary arteries over time by 64-slice computed tomography. Am J Cardiol. 2008;101(5):579–584. doi: 10.1016/j.amjcard.2007.10.016. Epub 2008/03/01. 10.1016/j.amjcard.2007.10.016. PubMed PMID: 18308002. [DOI] [PubMed] [Google Scholar]
- 16. Inoue K, Motoyama S, Sarai M, Sato T, Harigaya H, Hara T, et al. Serial Coronary CT Angiography–Verified Changes in Plaque Characteristics as an End PointEvaluation of Effect of Statin Intervention. JACC: Cardiovascular Imaging. 2010;3(7):691–698. doi: 10.1016/j.jcmg.2010.04.011. *CCTA is able to measure changes in plaque stability in response to statin treatment.
- 17.Pletcher MJ, Tice JA, Pignone M, Browner WS. Using the coronary artery calcium score to predict coronary heart disease events: a systematic review and meta-analysis. Arch Intern Med. 2004;164(12):1285. doi: 10.1001/archinte.164.12.1285. [DOI] [PubMed] [Google Scholar]
- 18.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. Journal of the American College of Cardiology. 1990;15(4):827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 19.Raggi P, Callister TQ, Cooil B, He ZX, Lippolis NJ, Russo DJ, et al. Identification of patients at increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation. 2000;101(8):850–855. doi: 10.1161/01.cir.101.8.850. [DOI] [PubMed] [Google Scholar]
- 20.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary Calcium as a Predictor of Coronary Events in Four Racial or Ethnic Groups. N Engl J Med. 2008;358(13):1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 21. Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. The Lancet. 2011;378(9792):684–692. doi: 10.1016/S0140-6736(11)60784-8. **Strong evidence for including CAC score in risk assessment.
- 22. Erbel R, Möhlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. Journal of the American College of Cardiology. 2010;56(17):1397–1406. doi: 10.1016/j.jacc.2010.06.030. **Strong evidence for including CAC score in risk assessment.
- 23.Achenbach S, Ropers D, Mohlenkamp S, Schmermund A, Muschiol G, Groth J, et al. Variability of repeated coronary artery calcium measurements by electron beam tomography. Am J Cardiol. 2001;87(2):210–213. A8. doi: 10.1016/s0002-9149(00)01319-9. Epub 2001/01/12. PubMed PMID: 11152842. [DOI] [PubMed] [Google Scholar]
- 24.Morita H, Fujimoto S, Kondo T, Arai T, Sekine T, Matsutani H, et al. Prevalence of computed tomographic angiography-verified high-risk plaques and significant luminal stenosis in patients with zero coronary calcium score. International Journal of Cardiology. 2012;158(2):272–278. doi: 10.1016/j.ijcard.2011.02.052. [DOI] [PubMed] [Google Scholar]
- 25.Kelly JL, Thickman D, Abramson SD, Chen PR, Smazal SF, Fleishman MJ, et al. Coronary CT angiography findings in patients without coronary calcification. American Journal of Roentgenology. 2008;191(1):50–55. doi: 10.2214/AJR.07.2954. [DOI] [PubMed] [Google Scholar]
- 26.Iwasaki K, Matsumoto T, Aono H, Furukawa H, Samukawa M. Prevalence of non-calcified coronary plaque on 64-slice computed tomography in asymptomatic patients with zero and low coronary artery calcium. Can J Cardiol. 2010;26(7):377–380. doi: 10.1016/s0828-282x(10)70419-0. Epub 2010/09/18. PubMed PMID: 20847965; PubMed Central PMCID: PMC2950712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uretsky S, Rozanski A, Singh P, Supariwala A, Atluri P, Bangalore S, et al. The presence, characterization and prognosis of coronary plaques among patients with zero coronary calcium scores. Int J Cardiovasc Imaging. 2011;27(6):805–812. doi: 10.1007/s10554-010-9730-0. Epub 2010/10/23. PubMed PMID: 20967569. [DOI] [PubMed] [Google Scholar]
- 28. Gottlieb I, Miller JM, Arbab-Zadeh A, Dewey M, Clouse ME, Sara L, et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55(7):627–634. doi: 10.1016/j.jacc.2009.07.072. Epub 2010/02/23. 10.1016/j.jacc.2009.07.072. PubMed PMID: 20170786. **Evidence for further need of risk stratification modes separate from CAC score
- 29.Iwasaki K, Matsumoto T, Aono H, Furukawa H, Samukawa M. Prevalence of subclinical atherosclerosis in asymptomatic patients with low-to-intermediate risk by 64-slice computed tomography. Coronary Artery Disease. 2011;22(1):18–25. doi: 10.1097/MCA.0b013e32833b20a5. [DOI] [PubMed] [Google Scholar]
- 30.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359(22):2324–2336. doi: 10.1056/NEJMoa0806576. Epub 2008/11/29. 10.1056/NEJMoa0806576. PubMed PMID: 19038879. [DOI] [PubMed] [Google Scholar]
- 31.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic Performance of 64-Multidetector Row Coronary Computed Tomographic Angiography for Evaluation of Coronary Artery Stenosis in Individuals Without Known Coronary Artery Disease: Results From the Prospective Multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) Trial. Journal of the American College of Cardiology. 2008;52(21):1724–1732. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 32.Meijboom WB, Meijs MFL, Schuijf JD, Cramer MJ, Mollet NR, van Mieghem CAG, et al. Diagnostic Accuracy of 64-Slice Computed Tomography Coronary Angiography: A Prospective, Multicenter, Multivendor Study. Journal of the American College of Cardiology. 52(25):2135–2144. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 33.Voros S, Rinehart S, Qian Z, Joshi P, Vazquez G, Fischer C, et al. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging. 2011;4(5):537–548. doi: 10.1016/j.jcmg.2011.03.006. Epub 2011/05/14. 10.1016/j.jcmg.2011.03.006. PubMed PMID: 21565743. [DOI] [PubMed] [Google Scholar]
- 34.Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. Journal of the American College of Cardiology. 2006;47(8):C13–C18. doi: 10.1016/j.jacc.2005.10.065. [DOI] [PubMed] [Google Scholar]
- 35.Davies MJ. The pathophysiology of acute coronary syndromes. Heart. 2000;83(3):361–366. doi: 10.1136/heart.83.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Falk E, Shah PK, Fuster V. Coronary plaque disruption. Circulation. 1995;92(3):657–671. doi: 10.1161/01.cir.92.3.657. [DOI] [PubMed] [Google Scholar]
- 37.Yamagishi M, Terashima M, Awano K, Kijima M, Nakatani S, Daikoku S, et al. Morphology of vulnerable coronary plaque: insights from follow-up of patients examined by intravascular ultrasound before an acute coronary syndrome. J Am Coll Cardiol. 2000;35(1):106–111. doi: 10.1016/s0735-1097(99)00533-1. Epub 2000/01/15. PubMed PMID: 10636267. [DOI] [PubMed] [Google Scholar]
- 38.Pflederer T, Marwan M, Schepis T, Ropers D, Seltmann M, Muschiol G, et al. Characterization of culprit lesions in acute coronary syndromes using coronary dual-source CT angiography. Atherosclerosis. 2010;211(2):437–444. doi: 10.1016/j.atherosclerosis.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 39.Motoyama S, Sarai M, Harigaya H, Anno H, Inoue K, Hara T, et al. Computed Tomographic Angiography Characteristics of Atherosclerotic Plaques Subsequently Resulting in Acute Coronary Syndrome. Journal of the American College of Cardiology. 2009;54(1):49–57. doi: 10.1016/j.jacc.2009.02.068. [DOI] [PubMed] [Google Scholar]
- 40.Hausleiter J, Meyer T, Hadamitzky M, Kastrati A, Martinoff S, Schömig A. Prevalence of Noncalcified Coronary Plaques by 64-Slice Computed Tomography in Patients With an Intermediate Risk for Significant Coronary Artery Disease. Journal of the American College of Cardiology. 2006;48(2):312–318. doi: 10.1016/j.jacc.2006.02.064. [DOI] [PubMed] [Google Scholar]
- 41.Fitch KV, Lo J, Abbara S, Ghoshhajra B, Shturman L, Soni A, et al. Increased coronary artery calcium score and noncalcified plaque among HIV-infected men: relationship to metabolic syndrome and cardiac risk parameters. Journal of acquired immune deficiency syndromes. 1999;55(4):495. doi: 10.1097/QAI.0b013e3181edab0b. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ, et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. Journal of Cardiovascular Computed Tomography. 2009;3(2):122–136. doi: 10.1016/j.jcct.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 43.Pundziute G, Schuijf JD, Jukema JW, Decramer I, Sarno G, Vanhoenacker PK, et al. Head-to-Head Comparison of Coronary Plaque Evaluation Between Multislice Computed Tomography and Intravascular Ultrasound Radiofrequency Data Analysis. JACC: Cardiovascular Interventions. 2008;1(2):176–182. doi: 10.1016/j.jcin.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 44.Schroeder S, Kuettner A, Leitritz M, Janzen J, Kopp AF, Herdeg C, et al. Reliability of differentiating human coronary plaque morphology using contrast-enhanced multislice spiral computed tomography: a comparison with histology. J Comput Assist Tomogr. 2004;28(4):449–454. doi: 10.1097/00004728-200407000-00003. Epub 2004/07/03. PubMed PMID: 15232374. [DOI] [PubMed] [Google Scholar]
- 45.Funabashi N, Asano M, Komuro I. Predictors of non-calcified plaques in the coronary arteries of 242 subjects using multislice computed tomography and logistic regression models. Int J Cardiol. 2007;117(2):191–197. doi: 10.1016/j.ijcard.2006.06.009. Epub 2006/07/25. 10.1016/j.ijcard.2006.06.009. PubMed PMID: 16859769. [DOI] [PubMed] [Google Scholar]
- 46.Aggarwal NR, Knickelbine T, Tande A, Stoltzfus L, Lesser JR, Schwartz RS. Non calcified plaque: Relationship between results of multi slice computed tomography, risk factors and late clinical outcome. Catheter Cardiovasc Interv. 2011 doi: 10.1002/ccd.23138. Epub 2011/05/05. PubMed PMID: 21542104. [DOI] [PubMed] [Google Scholar]
- 47.Rivera JJ, Nasir K, Cox PR, Choi EK, Yoon Y, Cho I, et al. Association of traditional cardiovascular risk factors with coronary plaque sub-types assessed by 64-slice computed tomography angiography in a large cohort of asymptomatic subjects. Atherosclerosis. 2009;206(2):451–457. doi: 10.1016/j.atherosclerosis.2009.05.027. Epub 2009/06/16. 10.1016/j.atherosclerosis.2009.05.027. PubMed PMID: 19524922. [DOI] [PubMed] [Google Scholar]
- 48.Isma'eel H, Tellalian D, Hamirani YS, Kadakia J, Nasir K, Budoff MJ. Effect of obesity on coronary artery plaque using 64 slice multidetector cardiac computed tomography angiography. Int J Cardiol. 2010;140(3):358–360. doi: 10.1016/j.ijcard.2008.11.049. Epub 2009/01/02. 10.1016/j.ijcard.2008.11.049. PubMed PMID: 19117625. [DOI] [PubMed] [Google Scholar]
- 49.Cheng VY, Lepor NE, Madyoon H, Eshaghian S, Naraghi AL, Shah PK. Presence and Severity of Noncalcified Coronary Plaque on 64-Slice Computed Tomographic Coronary Angiography in Patients With Zero and Low Coronary Artery Calcium. The American Journal of Cardiology. 2007;99(9):1183–1186. doi: 10.1016/j.amjcard.2006.12.026. [DOI] [PubMed] [Google Scholar]
- 50.Bamberg F, Truong QA, Koenig W, Schlett CL, Nasir K, Butler J, et al. Differential associations between blood biomarkers of inflammation, oxidation, and lipid metabolism with varying forms of coronary atherosclerotic plaque as quantified by coronary CT angiography. The International Journal of Cardiovascular Imaging. 2011 doi: 10.1007/s10554-010-9773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Konishi M, Sugiyama S, Sugamura K, Nozaki T, Ohba K, Matsubara J, et al. Association of pericardial fat accumulation rather than abdominal obesity with coronary atherosclerotic plaque formation in patients with suspected coronary artery disease. Atherosclerosis. 2010;209(2):573–578. doi: 10.1016/j.atherosclerosis.2009.10.008. Epub 2009/11/07. 10.1016/j.atherosclerosis.2009.10.008. PubMed PMID: 19892354. [DOI] [PubMed] [Google Scholar]
- 52.Oka T, Yamamoto H, Ohashi N, Kitagawa T, Kunita E, Utsunomiya H, et al. Association between epicardial adipose tissue volume and characteristics of non-calcified plaques assessed by coronary computed tomographic angiography. International Journal of Cardiology. 2011 doi: 10.1016/j.ijcard.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 53.Kashiwagi M, Imanishi T, Tsujioka H, Ikejima H, Kuroi A, Ozaki Y, et al. Association of monocyte subsets with vulnerability characteristics of coronary plaques as assessed by 64-slice multidetector computed tomography in patients with stable angina pectoris. Atherosclerosis. 2010;212(1):171–176. doi: 10.1016/j.atherosclerosis.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 54.Feuchtner G, Postel T, Weidinger F, Frick M, Alber H, Dichtl W, et al. Is There a Relation between Non-Calcifying Coronary Plaques and Acute Coronary Syndromes? A Retrospective Study Using Multislice Computed Tomography. Cardiology. 2008;110(4):241–248. doi: 10.1159/000112407. [DOI] [PubMed] [Google Scholar]
- 55.Motoyama S, Kondo T, Sarai M, Sugiura A, Harigaya H, Sato T, et al. Multislice Computed Tomographic Characteristics of Coronary Lesions in Acute Coronary Syndromes. Journal of the American College of Cardiology. 2007;50(4):319–326. doi: 10.1016/j.jacc.2007.03.044. [DOI] [PubMed] [Google Scholar]
- 56.Min JK, Edwardes M, Lin FY, Labounty T, Weinsaft JW, Choi J-H, et al. Relationship of coronary artery plaque composition to coronary artery stenosis severity: Results from the prospective multicenter ACCURACY trial. Atherosclerosis. 2011 doi: 10.1016/j.atherosclerosis.2011.05.032. [DOI] [PubMed] [Google Scholar]
- 57.Becker CR, Nikolaou K, Muders M, Babaryka G, Crispin A, Schoepf UJ, et al. Ex vivo coronary atherosclerotic plaque characterization with multi-detector-row CT. European Radiology. 2003;13(9):2094–2098. doi: 10.1007/s00330-003-1889-5. [DOI] [PubMed] [Google Scholar]
- 58.Schroeder S. Non-invasive evaluation of atherosclerosis with contrast enhanced 16 slice spiral computed tomography: results of ex vivo investigations. Heart. 2004;90(12):1471–1475. doi: 10.1136/hrt.2004.037861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leschka S, Seitun S, Dettmer M, Baumuller S, Stolzmann P, Goetti R, et al. Ex vivo evaluation of coronary atherosclerotic plaques: characterization with dual-source CT in comparison with histopathology. J Cardiovasc Comput Tomogr. 2010;4(5):301–308. doi: 10.1016/j.jcct.2010.05.016. Epub 2010/10/16. 10.1016/j.jcct.2010.05.016. PubMed PMID: 20947041. [DOI] [PubMed] [Google Scholar]
- 60.Kimura S, Yonetsu T, Suzuki K, Isobe M, Iesaka Y, Kakuta T. Characterisation of non-calcified coronary plaque by 16-slice multidetector computed tomography: comparison with histopathological specimens obtained by directional coronary atherectomy. The International Journal of Cardiovascular Imaging (formerly Cardiac Imaging) 2011:1–14. doi: 10.1007/s10554-011-9992-1. [DOI] [PubMed] [Google Scholar]
- 61.Granada JF, Wallace-Bradley D, Win HK, Alviar CL, Builes A, Lev EI, et al. In vivo plaque characterization using intravascular ultrasound–virtual histology in a porcine model of complex coronary lesions. Arterioscler Thromb Vac Biol. 2007;27(2):387–393. doi: 10.1161/01.ATV.0000253907.51681.0e. [DOI] [PubMed] [Google Scholar]
- 62.Chopard R, Boussel L, Motreff P, Rioufol G, Tabib A, Douek P, et al. How reliable are 40 MHz IVUS and 64-slice MDCT in characterizing coronary plaque composition? An ex vivo study with histopathological comparison. The International Journal of Cardiovascular Imaging. 2010;26(4):373–383. doi: 10.1007/s10554-009-9562-y. [DOI] [PubMed] [Google Scholar]
- 63.Carlier SG, Tanaka K. Studying coronary plaque regression with IVUS: a critical review of recent studies. JIntervent Cardiol. 2006;19(1):11–15. doi: 10.1111/j.1540-8183.2006.00098.x. [DOI] [PubMed] [Google Scholar]
- 64.Voros S. Can Computed Tomography Angiography of the Coronary Arteries Characterize Atherosclerotic Plaque Composition?: Is the CAT (Scan) Out of the Bag? JACC: Cardiovascular Interventions. 2008;1(2):183–185. doi: 10.1016/j.jcin.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 65.Kopp AF, Schroeder S, Baumbach A, Kuettner A, Georg C, Ohnesorge B, et al. Non-invasive characterisation of coronary lesion morphology and composition by multislice CT: first results in comparison with intracoronary ultrasound. Eur Radiol. 2001;11(9):1607–1611. doi: 10.1007/s003300100850. Epub 2001/08/21. PubMed PMID: 11511879. [DOI] [PubMed] [Google Scholar]
- 66.Schroeder S, Kopp AF, Baumbach A, Meisner C, Kuettner A, Georg C, et al. Noninvasive detection and evaluation of atherosclerotic coronary plaques with multislice computed tomography. J Am Coll Cardiol. 2001;37(5):1430–1435. doi: 10.1016/s0735-1097(01)01115-9. Epub 2001/04/13. PubMed PMID: 11300457. [DOI] [PubMed] [Google Scholar]
- 67.Leber AW, Knez A, Becker A, Becker C, von Ziegler F, Nikolaou K, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol. 2004;43(7):1241–1247. doi: 10.1016/j.jacc.2003.10.059. Epub 2004/04/06. S0735109704001081 [pii]. PubMed PMID: 15063437. [DOI] [PubMed] [Google Scholar]
- 68.Leber AW, Knez A, von Ziegler F, Becker A, Nikolaou K, Paul S, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005;46(1):147–154. doi: 10.1016/j.jacc.2005.03.071. Epub 2005/07/05. 10.1016/j.jacc.2005.03.071. PubMed PMID: 15992649. [DOI] [PubMed] [Google Scholar]
- 69.Achenbach S, Moselewski F, Ropers D, Ferencik M, Hoffmann U, MacNeill B, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation. 2004;109(1):14–17. doi: 10.1161/01.CIR.0000111517.69230.0F. Epub 2003/12/24. 01.CIR.0000111517.69230.0F [pii]. PubMed PMID: 14691045. [DOI] [PubMed] [Google Scholar]
- 70.Brodoefel H, Burgstahler C, Heuschmid M, Reimann A, Khosa F, Kopp A, et al. Accuracy of dual-source CT in the characterisation of non-calcified plaque: use of a colour-coded analysis compared with virtual histology intravascular ultrasound. Br J Radiol. 2009;82(982):805–812. doi: 10.1259/bjr/35768497. Epub 2009/04/01. 10.1259/bjr/35768497. PubMed PMID: 19332517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brodoefel H, Burgstahler C, Sabir A, Yam CS, Khosa F, Claussen CD, et al. Coronary plaque quantification by voxel analysis: dual-source MDCT angiography versus intravascular sonography. AJR Am J Roentgenol. 2009;192(3):W84–W89. doi: 10.2214/AJR.08.1381. Epub 2009/02/24. 10.2214/AJR.08.1381. PubMed PMID: 19234244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hur J, Kim YJ, Lee HJ, Nam JE, Choe KO, Seo JS, et al. Quantification and characterization of obstructive coronary plaques using 64-slice computed tomography: a comparison with intravascular ultrasound. J Comput Assist Tomogr. 2009;33(2):186–92. doi: 10.1097/RCT.0b013e31817c420f. Epub 2009/04/07. 00004728-200903000-00005 [pii]. PubMed PMID: 19346843. [DOI] [PubMed] [Google Scholar]
- 73.Otsuka M, Bruining N, Van Pelt NC, Mollet NR, Ligthart JM, Vourvouri E, et al. Quantification of coronary plaque by 64-slice computed tomography: a comparison with quantitative intracoronary ultrasound. Invest Radiol. 2008;43(5):314–321. doi: 10.1097/RLI.0b013e31816a88a9. Epub 2008/04/22. 00004424-200805000-00006 [pii]. PubMed PMID: 18424952. [DOI] [PubMed] [Google Scholar]
- 74.Carrascosa PM, Capunay CM, Garcia-Merletti P, Carrascosa J, Garcia MF. Characterization of coronary atherosclerotic plaques by multidetector computed tomography. Am J Cardiol. 2006;97(5):598–602. doi: 10.1016/j.amjcard.2005.09.096. Epub 2006/02/24. 10.1016/j.amjcard.2005.09.096. PubMed PMID: 16490420. [DOI] [PubMed] [Google Scholar]
- 75.Kitagawa T, Yamamoto H, Ohhashi N, Okimoto T, Horiguchi J, Hirai N, et al. Comprehensive evaluation of noncalcified coronary plaque characteristics detected using 64-slice computed tomography in patients with proven or suspected coronary artery disease. Am Heart J. 2007;154(6):1191–1198. doi: 10.1016/j.ahj.2007.07.020. Epub 2007/11/24. PubMed PMID: 18035094. [DOI] [PubMed] [Google Scholar]
- 76.Carrascosa PM, Capunay CM, Parodi JC, Padilla LT, Johnson P, Carrascosa JM, et al. General utilities of multislice tomography in the cardiac field. Herz. 2003;28(1):44–51. doi: 10.1007/s00059-003-2443-6. Epub 2003/03/05. PubMed PMID: 12616320. [DOI] [PubMed] [Google Scholar]
- 77.Ferencik M, Chan RC, Achenbach S, Lisauskas JB, Houser SL, Hoffmann U, et al. Arterial Wall Imaging: Evaluation with 16-Section Multidetector CT in Blood Vessel Phantoms and ex Vivo Coronary Arteries1. Radiology. 2006;240(3):708–716. doi: 10.1148/radiol.2403051204. [DOI] [PubMed] [Google Scholar]
- 78.Galonska M, Ducke F, Kertesz-Zborilova T, Meyer R, Guski H, Knollmann FD. Characterization of Atherosclerotic Plaques in Human Coronary Arteries With 16-Slice Multidetector Row Computed Tomography by Analysis of Attenuation Profiles. Acad Radiol. 2008;15(2):222–230. doi: 10.1016/j.acra.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 79.Saraste A, Knuuti J. Novel CT-based imaging markers for high-risk coronary plaques. European Heart Journal–Cardiovascular Imaging. 2012;13(8):633–634. doi: 10.1093/ehjci/jes129. [DOI] [PubMed] [Google Scholar]
- 80.Rinehart S, Vazquez G, Qian Z, Murrieta L, Christian K, Voros S. Quantitative measurements of coronary arterial stenosis, plaque geometry, and composition are highly reproducible with a standardized coronary arterial computed tomographic approach in high-quality CT datasets. Journal of Cardiovascular Computed Tomography. 2011;5(1):35–43. doi: 10.1016/j.jcct.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 81.Voros S, Rinehart S, Qian Z, Vazquez G, Anderson H, Murrieta L, et al. Prospective Validation of Standardized, 3-Dimensional, Quantitative Coronary Computed Tomographic Plaque Measurements Using Radiofrequency Backscatter Intravascular Ultrasound as Reference Standard in Intermediate Coronary Arterial Lesions. JACC: Cardiovascular Interventions. 2011;4(2):198–208. doi: 10.1016/j.jcin.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 82.Choi BJ, Kang DK, Tahk SJ, Choi SY, Yoon MH, Lim HS, et al. Comparison of 64-slice multidetector computed tomography with spectral analysis of intravascular ultrasound backscatter signals for characterizations of noncalcified coronary arterial plaques. Am J Cardiol. 2008;102(8):988–993. doi: 10.1016/j.amjcard.2008.05.060. Epub 2008/10/22. 10.1016/j.amjcard.2008.05.060. PubMed PMID: 18929698. [DOI] [PubMed] [Google Scholar]
- 83.Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ. Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med. 1987;316(22):1371–1375. doi: 10.1056/NEJM198705283162204. [DOI] [PubMed] [Google Scholar]
- 84.Achenbach S, Ropers D, Hoffmann U, MacNeill B, Baum U, Pohle K, et al. assessment of coronary remodeling in stenotic and nonstenotic coronary atherosclerotic lesions by multidetector spiral computed tomography. Journal of the American College of Cardiology. 2004;43(5):842–847. doi: 10.1016/j.jacc.2003.09.053. [DOI] [PubMed] [Google Scholar]
- 85.Schoenhagen P, Murat Tuzcu E, Stillman AE, Moliterno DJ, Halliburton SS, Kuzmiak SA, et al. Non-invasive assessment of plaque morphology and remodeling in mildly stenotic coronary segments: comparison of 16-slice computed tomography and intravascular ultrasound. Coronary Artery Disease. 2003;14(6):459. doi: 10.1097/00019501-200309000-00007. [DOI] [PubMed] [Google Scholar]
- 86.Kitagawa T, Yamamoto H, Horiguchi J, Ohhashi N, Tadehara F, Shokawa T, et al. Characterization of noncalcified coronary plaques and identification of culprit lesions in patients with acute coronary syndrome by 64-slice computed tomography. JACC Cardiovasc Imaging. 2009;2(2):153–160. doi: 10.1016/j.jcmg.2008.09.015. Epub 2009/04/10. PubMed PMID: 19356549. [DOI] [PubMed] [Google Scholar]
- 87.Schoenhagen P, Tuzcu EM, Apperson-Hansen C, Wang C, Wolski K, Lin S, et al. Determinants of arterial wall remodeling during lipid-lowering therapy: serial intravascular ultrasound observations from the Reversal of Atherosclerosis with Aggressive Lipid Lowering Therapy (REVERSAL) trial. Circulation. 2006;113(24):2826–2834. doi: 10.1161/CIRCULATIONAHA.105.585703. Epub 2006/06/14. 10.1161/CIRCULATIONAHA.105.585703. PubMed PMID: 16769916. [DOI] [PubMed] [Google Scholar]
- 88.Sabate M, Kay IP, de Feyter PJ, van Domburg RT, Deshpande NV, Ligthart JM, et al. Remodeling of atherosclerotic coronary arteries varies in relation to location and composition of plaque. Am J Cardiol. 1999;84(2):135–140. doi: 10.1016/s0002-9149(99)00222-2. Epub 1999/07/30. PubMed PMID: 10426328. [DOI] [PubMed] [Google Scholar]
- 89.Takeuchi H, Morino Y, Matsukage T, Masuda N, Kawamura Y, Kasai S, et al. Impact of vascular remodeling on the coronary plaque compositions: an investigation with in vivo tissue characterization using integrated backscatter-intravascular ultrasound. Atherosclerosis. 2009;202(2):476–482. doi: 10.1016/j.atherosclerosis.2008.05.052. Epub 2008/07/09. 10.1016/j.atherosclerosis.2008.05.052. PubMed PMID: 18606416. [DOI] [PubMed] [Google Scholar]
- 90.Schmid M, Pflederer T, Jang I-K, Ropers D, Sei K, Daniel WG, et al. Relationship between degree of remodeling and CT attenuation of plaque in coronary atherosclerotic lesions: An in-vivo analysis by multi-detector computed tomography. Atherosclerosis. 2008;197(1):457–464. doi: 10.1016/j.atherosclerosis.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 91.Kroner ES, van Velzen JE, Boogers MJ, Siebelink HM, Schalij MJ, Kroft LJ, et al. Positive remodeling on coronary computed tomography as a marker for plaque vulnerability on virtual histology intravascular ultrasound. Am J Cardiol. 2011;107(12):1725–179. doi: 10.1016/j.amjcard.2011.02.337. Epub 2011/04/13. PubMed PMID: 21481832. [DOI] [PubMed] [Google Scholar]
- 92.Matsumoto N, Sato Y, Yoda S, Nakano Y, Kunimasa T, Matsuo S, et al. Prognostic value of non-obstructive CT low-dense coronary artery plaques detected by multislice computed tomography. Circ J. 2007;71(12):1898–1903. doi: 10.1253/circj.71.1898. Epub 2007/11/27. PubMed PMID: 18037743. [DOI] [PubMed] [Google Scholar]
- 93.van Werkhoven JM, Schuijf JD, Gaemperli O, Jukema JW, Boersma E, Wijns W, et al. Prognostic value of multislice computed tomography and gated single-photon emission computed tomography in patients with suspected coronary artery disease. J Am Coll Cardiol. 2009;53(7):623–632. doi: 10.1016/j.jacc.2008.10.043. Epub 2009/02/14. 10.1016/j.jacc.2008.10.043. PubMed PMID: 19215839. [DOI] [PubMed] [Google Scholar]
- 94.van Werkhoven JM, Schuijf JD, Gaemperli O, Jukema JW, Kroft LJ, Boersma E, et al. Incremental prognostic value of multi-slice computed tomography coronary angiography over coronary artery calcium scoring in patients with suspected coronary artery disease. Eur Heart J. 2009;30(21):2622–2639. doi: 10.1093/eurheartj/ehp272. Epub 2009/07/02. 10.1093/eurheartj/ehp272. PubMed PMID: 19567382. [DOI] [PubMed] [Google Scholar]
- 95.Ahmadi N, Nabavi V, Hajsadeghi F, Flores F, French WJ, Mao SS, et al. Mortality incidence of patients with non-obstructive coronary artery disease diagnosed by computed tomography angiography. Am J Cardiol. 2011;107(1):10–16. doi: 10.1016/j.amjcard.2010.08.034. Epub 2010/12/15. 10.1016/j.amjcard.2010.08.034. PubMed PMID: 21146679. [DOI] [PubMed] [Google Scholar]
- 96.Hammer-Hansen S, Kofoed KF, Kelbaek H, Kristensen T, Kuhl JT, Thune JJ, et al. Volumetric evaluation of coronary plaque in patients presenting with acute myocardial infarction or stable angina pectoris-a multislice computerized tomography study. Am Heart J. 2009;157(3):481–487. doi: 10.1016/j.ahj.2008.10.011. Epub 2009/03/03. 10.1016/j.ahj.2008.10.011. PubMed PMID: 19249418. [DOI] [PubMed] [Google Scholar]
- 97.Kim SY, Kim KS, Seung MJ, Chung JW, Kim JH, Mun SH, et al. The culprit lesion score on multi-detector computed tomography can detect vulnerable coronary artery plaque. Int J Cardiovasc Imaging. 2010;26(Suppl 2):245–252. doi: 10.1007/s10554-010-9712-2. Epub 2010/10/07. PubMed PMID: 20924792. [DOI] [PubMed] [Google Scholar]
- 98.Ferencik M, Schlett CL, Ghoshhajra BB, Kriegel MF, Joshi SB, Maurovich-Horvat P, et al. A Computed Tomography-Based Coronary Lesion Score to Predict Acute Coronary Syndrome Among Patients With Acute Chest Pain and Significant Coronary Stenosis on Coronary Computed Tomographic Angiogram. The American Journal of Cardiology. 2012;110(2):183–189. doi: 10.1016/j.amjcard.2012.02.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kristensen TS, Kofoed KF, Kühl JT, Nielsen WB, Nielsen MB, Kelbæk H. Prognostic Implications of Nonobstructive Coronary Plaques in Patients With Non–ST-Segment Elevation Myocardial Infarction. Journal of the American College of Cardiology. 2011;58(5):502–509. doi: 10.1016/j.jacc.2011.01.058. [DOI] [PubMed] [Google Scholar]
- 100.Watabe H, Sato A, Akiyama D, Kakefuda Y, Adachi T, Ojima E, et al. Impact of Coronary Plaque Composition on Cardiac Troponin Elevation After Percutaneous Coronary Intervention in Stable Angina Pectoris: A Computed Tomography Analysis. Journal of the American College of Cardiology. 2012;59(21):1881–1888. doi: 10.1016/j.jacc.2012.01.051. [DOI] [PubMed] [Google Scholar]
- 101.Gottlieb I, Agarwal S, Gautam S, Desai M, Steen H, Warren WP, et al. Aortic plaque regression as determined by magnetic resonance imaging with high-dose and low-dose statin therapy. J Cardiovasc Med (Hagerstown) 2008;9(7):700–706. doi: 10.2459/JCM.0b013e3282f447c3. Epub 2008/06/12. PubMed PMID: 18545070. [DOI] [PubMed] [Google Scholar]
- 102.Lima JA, Desai MY, Steen H, Warren WP, Gautam S, Lai S. Statin-induced cholesterol lowering and plaque regression after 6 months of magnetic resonance imaging-monitored therapy. Circulation. 2004;110(16):2336–2341. doi: 10.1161/01.CIR.0000145170.22652.51. Epub 2004/10/13. PubMed PMID: 15477398. [DOI] [PubMed] [Google Scholar]
- 103.Fayad ZA, Mani V, Woodward M, Kallend D, Abt M, Burgess T, et al. Safety and efficacy of dalcetrapib on atherosclerotic disease using novel non-invasive multimodality imaging (dal-PLAQUE): a randomised clinical trial. Lancet. 2011;378(9802):1547–1559. doi: 10.1016/S0140-6736(11)61383-4. Epub 2011/09/13. PubMed PMID: 21908036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yonemura A, Momiyama Y, Fayad ZA, Ayaori M, Ohmori R, Kihara T, et al. Effect of lipid-lowering therapy with atorvastatin on atherosclerotic aortic plaques: a 2-year follow-up by noninvasive MRI. Eur J Cardiovasc Prev Rehabil. 2009;16(2):222–228. doi: 10.1097/HJR.0b013e32832948a0. Epub 2009/02/27. PubMed PMID: 19242355. [DOI] [PubMed] [Google Scholar]
- 105.Corti R, Fuster V, Fayad ZA, Worthley SG, Helft G, Chaplin WF, et al. Effects of aggressive versus conventional lipid-lowering therapy by simvastatin on human atherosclerotic lesions: a prospective, randomized, double-blind trial with high-resolution magnetic resonance imaging. J Am Coll Cardiol. 2005;46(1):106–112. doi: 10.1016/j.jacc.2005.03.054. Epub 2005/07/05. PubMed PMID: 15992643. [DOI] [PubMed] [Google Scholar]
- 106.Yonemura A, Momiyama Y, Fayad ZA, Ayaori M, Ohmori R, Higashi K, et al. Effect of lipid-lowering therapy with atorvastatin on atherosclerotic aortic plaques detected by noninvasive magnetic resonance imaging. J Am Coll Cardiol. 2005;45(5):733–742. doi: 10.1016/j.jacc.2004.11.039. Epub 2005/03/01. PubMed PMID: 15734619. [DOI] [PubMed] [Google Scholar]
- 107.Corti R, Fuster V, Fayad ZA, Worthley SG, Helft G, Smith D, et al. Lipid lowering by simvastatin induces regression of human atherosclerotic lesions: two years' follow-up by high-resolution noninvasive magnetic resonance imaging. Circulation. 2002;106(23):2884–2887. doi: 10.1161/01.cir.0000041255.88750.f0. Epub 2002/12/04. PubMed PMID: 12460866. [DOI] [PubMed] [Google Scholar]
- 108.Helft G, Worthley SG, Fuster V, Fayad ZA, Zaman AG, Corti R, et al. Progression and regression of atherosclerotic lesions: monitoring with serial noninvasive magnetic resonance imaging. Circulation. 2002;105(8):993–998. doi: 10.1161/hc0802.104325. Epub 2002/02/28. PubMed PMID: 11864931. [DOI] [PubMed] [Google Scholar]
- 109.Hoffmann H, Frieler K, Schlattmann P, Hamm B, Dewey M. Influence of statin treatment on coronary atherosclerosis visualised using multidetector computed tomography. Eur Radiol. 2010;20(12):2824–2833. doi: 10.1007/s00330-010-1880-x. Epub 2010/07/20. PubMed PMID: 20640900. [DOI] [PubMed] [Google Scholar]
- 110.Kitagawa T, Yamamoto H, Horiguchi J, Ohashi N, Kunita E, Utsunomiya H, et al. Effects of statin therapy on non-calcified coronary plaque assessed by 64-slice computed tomography. International Journal of Cardiology. 2011;150(2):146–150. doi: 10.1016/j.ijcard.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 111.Otagiri K, Tsutsui H, Kumazaki S, Miyashita Y, Aizawa K, Koshikawa M, et al. Early intervention with rosuvastatin decreases the lipid components of the plaque in acute coronary syndrome: analysis using integrated backscatter IVUS (ELAN study) Circ J. 2011;75(3):633–641. doi: 10.1253/circj.cj-10-0600. Epub 2011/01/27. PubMed PMID: 21266787. [DOI] [PubMed] [Google Scholar]
- 112.Burgstahler C, Reimann A, Beck T, Kuettner A, Baumann D, Heuschmid M, et al. Influence of a lipid-lowering therapy on calcified and noncalcified coronary plaques monitored by multislice detector computed tomography: results of the New Age II Pilot Study. Invest Radiol. 2007;42(3):189–195. doi: 10.1097/01.rli.0000254408.96355.85. Epub 2007/02/09. 00004424-200703000-00006 [pii]. PubMed PMID: 17287649. [DOI] [PubMed] [Google Scholar]
- 113.Mettler FA, Jr, Thomadsen BR, Bhargavan M, Gilley DB, Gray JE, Lipoti JA, et al. Medical radiation exposure in the U.S. in 2006: preliminary results. Health Phys. 2008;95(5):502–507. doi: 10.1097/01.HP.0000326333.42287.a2. Epub 2008/10/14. 00004032-200811000-00006 [pii]. PubMed PMID: 18849682. [DOI] [PubMed] [Google Scholar]
- 114.Schauer DA, Linton OW. National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Radiology. 2009;253(2):293–296. doi: 10.1148/radiol.2532090494. Epub 2009/10/30. 10.1148/radiol.2532090494. PubMed PMID: 19864524. [DOI] [PubMed] [Google Scholar]
- 115.Silva AC, Lawder HJ, Hara A, Kujak J, Pavlicek W. Innovations in CT dose reduction strategy: application of the adaptive statistical iterative reconstruction algorithm. AJR Am J Roentgenol. 2010;194(1):191–199. doi: 10.2214/AJR.09.2953. Epub 2009/12/24. PubMed PMID: 20028923. [DOI] [PubMed] [Google Scholar]
- 116.Gosling O, Loader R, Venables P, Roobottom C, Rowles N, Bellenger N, et al. A comparison of radiation doses between state-of-the-art multislice CT coronary angiography with iterative reconstruction, multislice CT coronary angiography with standard filtered back-projection and invasive diagnostic coronary angiography. Heart. 2010;96(12):922–926. doi: 10.1136/hrt.2010.195909. [DOI] [PubMed] [Google Scholar]
- 117.Nelson RC, Feuerlein S, Boll DT. New iterative reconstruction techniques for cardiovascular computed tomography: how do they work, and what are the advantages and disadvantages? J Cardiovasc Comput Tomogr. 2011;5(5):286–292. doi: 10.1016/j.jcct.2011.07.001. Epub 2011/08/31. 10.1016/j.jcct.2011.07.001. PubMed PMID: 21875826. [DOI] [PubMed] [Google Scholar]
- 118.Heilbron B, Leipsic J. Submillisievert coronary computed tomography angiography using adaptive statistical iterative reconstruction–a new reality. The Canadian journal of cardiology. 2010;26(1):35. doi: 10.1016/s0828-282x(10)70333-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sakakura K, Yasu T, Kobayashi Y, Katayama T, Sugawara Y, Funayama H, et al. Noninvasive tissue characterization of coronary arterial plaque by 16-slice computed tomography in acute coronary syndrome. Angiology. 2006;57(2):155–160. doi: 10.1177/000331970605700204. Epub 2006/03/07. PubMed PMID: 16518522. [DOI] [PubMed] [Google Scholar]
- 120.Xiao XG, Xie DX, Shen BZ, Han X, Li AY, Ma ZW, et al. Value of multi-slice computed tomography in diagnosis of coronary plaque characterization. Zhonghua yi xue za zhi. 2007;87(46):3247–3250. Epub 2008/04/10. PubMed PMID: 18396617. [PubMed] [Google Scholar]
- 121.Iriart X, Brunot S, Coste P, Montaudon M, Dos-Santos P, Leroux L, et al. Early characterization of atherosclerotic coronary plaques with multidetector computed tomography in patients with acute coronary syndrome: a comparative study with intravascular ultrasound. Eur Radiol. 2007;17(10):2581–2588. doi: 10.1007/s00330-007-0665-3. Epub 2007/06/06. PubMed PMID: 17549491. [DOI] [PubMed] [Google Scholar]
- 122.Viles-Gonzalez JF, Poon M, Sanz J, Rius T, Nikolaou K, Fayad ZA, et al. In Vivo 16-Slice, Multidetector-Row Computed Tomography for the Assessment of Experimental Atherosclerosis. Circulation. 2004;110(11):1467–1472. doi: 10.1161/01.CIR.0000141732.28175.2A. [DOI] [PubMed] [Google Scholar]
- 123.Pohle K, Achenbach S, MacNeill B, Ropers D, Ferencik M, Moselewski F, et al. Characterization of non-calcified coronary atherosclerotic plaque by multi-detector row CT: Comparison to IVUS. Atherosclerosis. 2007;190(1):174–180. doi: 10.1016/j.atherosclerosis.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 124. Leipsic J, LaBounty TM, Heilbron B, Min JK, Mancini G, Lin FY, et al. Adaptive statistical iterative reconstruction: assessment of image noise and image quality in coronary CT angiography. American Journal of Roentgenology. 2010;195(3):649–654. doi: 10.2214/AJR.10.4285. **Prospective study showing benefit of iterative reconstruction.
- 125.Miéville FA, Gudinchet F, Rizzo E, Ou P, Brunelle F, Bochud FO, et al. Paediatric cardiac CT examinations: impact of the iterative reconstruction method ASIR on image quality–preliminary findings. Pediatr Radiol. 2011:1–11. doi: 10.1007/s00247-011-2146-8. [DOI] [PubMed] [Google Scholar]
- 126.Jang H, Cho J, Lee H, Hong I, Cho M, Park C, et al. Dose assessment according to changes in algorithm in cardiac CT. 2011 [Google Scholar]
- 127.Kazakauskaite E, Husmann L, Stehli J, Fuchs T, Fiechter M, Klaeser B, et al. Image quality in low-dose coronary computed tomography angiography with a new high-definition CT scanner. The International Journal of Cardiovascular Imaging (formerly Cardiac Imaging) 2012:1–7. doi: 10.1007/s10554-012-0100-y. [DOI] [PubMed] [Google Scholar]
- 128.Leipsic J, LaBounty TM, Heilbron B, Min JK, Mancini GBJ, Lin FY, et al. Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. American Journal of Roentgenology. 2010;195(3):655–660. doi: 10.2214/AJR.10.4288. [DOI] [PubMed] [Google Scholar]
- 129.Funama Y, Taguchi K, Utsunomiya D, Oda S, Yanaga Y, Yamashita Y, et al. Combination of a low-tube-voltage technique with hybrid iterative reconstruction (iDose) algorithm at coronary computed tomographic angiography. J Comput Assist Tomogr. 2011;35(4):480. doi: 10.1097/RCT.0b013e31821fee94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Oda S, Utsunomiya D, Funama Y, Yonenaga K, Namimoto T, Nakaura T, et al. A Hybrid Iterative Reconstruction Algorithm That Improves the Image Quality of Low-Tube-Voltage Coronary CT Angiography. American Journal of Roentgenology. 2012;198(5):1126–1131. doi: 10.2214/AJR.11.7117. [DOI] [PubMed] [Google Scholar]
- 131.Utsunomiya D, Weigold WG, Weissman G, Taylor AJ. Effect of hybrid iterative reconstruction technique on quantitative and qualitative image analysis at 256-slice prospective gating cardiac CT. European Radiology. 2011:1–8. doi: 10.1007/s00330-011-2361-6. [DOI] [PubMed] [Google Scholar]
- 132.Engel LC, Kröpil P, Sidhu MS, Techasith T, Maurovich-Horvat P, Abbara S, et al. Effects of Iterative Reconstruction Technique on Image Quality in Cardiac CT Angiography: Initial Experience. Journal of Biomedical Graphics and Computing. 2012;2(1):80. [Google Scholar]
- 133.Renker M, Ramachandra A, Schoepf UJ, Raupach R, Apfaltrer P, Rowe GW, et al. Iterative image reconstruction techniques: Applications for cardiac CT. J Cardiovasc Comput Tomogr. 2011;5(4):225–230. doi: 10.1016/j.jcct.2011.05.002. Epub 2011/07/05. PubMed PMID: 21723513. [DOI] [PubMed] [Google Scholar]
- 134.Moscariello A, Takx RAP, Schoepf UJ, Renker M, Zwerner PL, O’Brien TX, et al. Coronary CT angiography: image quality, diagnostic accuracy, and potential for radiation dose reduction using a novel iterative image reconstruction technique—comparison with traditional filtered back projection. European Radiology. 2011:1–9. doi: 10.1007/s00330-011-2164-9. [DOI] [PubMed] [Google Scholar]
- 135.Wang R, Schoepf UJ, Wu R, Reddy RP, Zhang C, Yu W, et al. Image quality and radiation dose of low dose coronary CT angiography in obese patients: Sinogram affirmed iterative reconstruction versus filtered back projection. European Journal of Radiology. 2012 doi: 10.1016/j.ejrad.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 136.Tatsugami F, Matsuki M, Nakai G, Inada Y, Kanazawa S, Takeda Y, et al. The effect of adaptive iterative dose reduction on image quality in 320-detector row ct coronary angiography. British Journal of Radiology. 2012 doi: 10.1259/bjr/10084599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Scheffel H, Stolzmann P, Schlett CL, Engel LC, Major GP, Károlyi M, et al. Coronary artery plaques: Cardiac CT with model-based and adaptive-statistical iterative reconstruction technique. European Journal of Radiology. 2011 doi: 10.1016/j.ejrad.2011.11.051. [DOI] [PubMed] [Google Scholar]
- 138.Stolzmann P, Schlett CL, Maurovich-Horvat P, Maehara A, Ma S, Scheffel H, et al. Variability and accuracy of coronary CT angiography including use of iterative reconstruction algorithms for plaque burden assessment as compared with intravascular ultrasound—an ex vivo study. European Radiology. 2012:1–9. doi: 10.1007/s00330-012-2464-8. [DOI] [PubMed] [Google Scholar]