Abstract
Previous research indicates that people with hoarding sometimes under- or over-report the severity of their symptoms. This article examines the results of two separate studies that evaluate severity ratings made by participants with hoarding disorder (HD) in comparison to ratings by family members or independent evaluators. In Study 1, HD participants’ ratings of the severity of the clutter in their home and their hoarding behaviors were less severe than those made by their friends or family members. This result may be accounted for by family members’ rejecting attitudes towards the participant. In Study 2, HD participants appeared to under-report specific hoarding symptoms while over-reporting their overall global impression of hoarding severity. A three-pronged assessment approach is recommended in which ratings of hoarding severity are made by the HD participant, their family member, and an independent observer or clinician. Such an approach would better inform future research, and also clinical treatment.
Keywords: Hoarding disorder, Collecting, Clutter, Insight, Patient rejection
1. Introduction
According to proposed DSM-5 criteria, hoarding disorder (HD) includes the following major elements: 1) persistent difficulty discarding or parting with possessions due to a perceived need to save them and distress associated with discarding; 2) symptoms result in the accumulation of a large number of possessions which clutter living areas and compromise their use; and 3) symptoms cause clinically significant distress or impairment in important areas of functioning (American Psychiatric Association, 2010). HD is a debilitating and costly public health problem that can lead to medical complications, fire hazards, pest infestations, and eviction (Tolin, Frost, Steketee, Gray, & Fitch, 2008).
Previous research suggests that the pervasive negative impact of HD symptoms is often compounded by poor insight among sufferers, and that this poor insight poses a significant obstacle to treatment (Frost, Tolin, & Maltby, 2010; Tolin, Fitch, Frost, & Steketee, 2010). Poor insight may explain why individuals with HD often express little motivation to seek treatment (Damecour & Charron, 1998) and are more likely to drop out of treatment than are patients with non-hoarding obsessive-compulsive disorder (Mataix-Cols, Marks, Greist, Kobak, & Baer, 2002). Limited insight may also lead individuals with HD to minimize the severity of their symptoms or the resulting functional impairment, posing a problem for accurate assessment.
However, other research suggests that HD might not be characterized by a systematic under-reporting of symptom severity. Frost et al. (2008) compared the self-rated Clutter Image Rating (CIR) scores of HD participants to CIR ratings made by independent evaluators who visited their homes. There was no significant difference between the two, and the two scores were highly correlated. However, when the authors compared the two groups’ ratings on another measure of clutter, the Clutter Scale, HD participants actually over-reported their clutter severity in comparison to observer ratings. These findings are difficult to reconcile with reports of family members who generally describe their loved ones with HD as exhibiting poor insight into their problem (Tolin, Fitch, Frost, & Steketee, 2010). One possible explanation is that family members, particularly those who are distressed about the hoarding, over-report the severity of the problem. Another possibility is that HD participants who elect to enroll in research studies tend to over-report the severity of their symptoms in order to qualify for the research.
The aim of the first study was to compare hoarding severity and functional impact reported by HD participants versus their loved ones (friends, family members). To accomplish this aim, we analyzed data collected from paired samples of individuals with HD and their loved ones who completed the same questionnaires regarding the HD participant’s symptoms and level of impairment. Based on findings of limited insight among people who hoard, it was predicted that HD participants’ would under-report their symptoms in comparison to their friends or family members (FFMs) due to limited insight. In the second study, we compared HD participants’ ratings to those of trained independent evaluators (IEs). It was again predicted that, compared to the other evaluators, HD participants would systematically under-report the severity of their hoarding behaviors and associated functional impairment.
2. Study 1
2.1. Methods
2.1.1. Participants
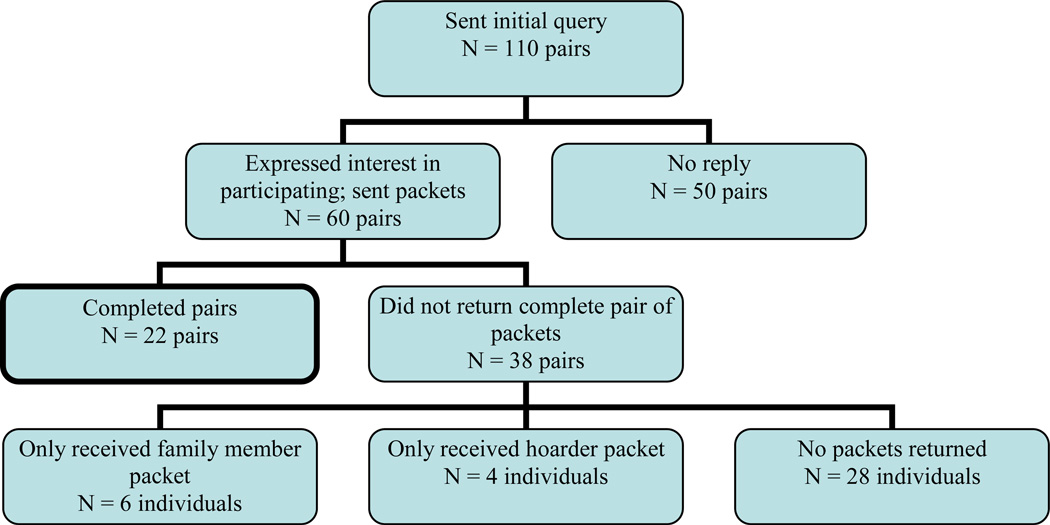
Pairs of individuals with HD and friends or family members (FFM) were recruited via an advertisement in a free newsletter and via email sent to a database of over 8,000 individuals who had contacted the researchers between January 2004 and January 2007 for information about HD. The advertisement/email indicated that the researchers were seeking pairs of individuals, one of whom had HD and the other of whom was a friend or family member who knows the HD individual well, to complete the study. Interested respondents were asked to send an email to the researchers. As shown in Figure A.1, 110 individuals replied and were sent a follow-up email. Those who responded to the second email were mailed two packets of questionnaires, one for the person with HD and one for the FFMFM.
Figure A.1.
Flow chart of enrollment.
Completed questionnaire packets were received from 22 pairs. Both the individuals with HD and their FFMs were predominantly female (77.3% HD, 66.7% FFM) and white (100% HD, 95.2% FFM). The individuals with HD were, on average, 7.4 years older than the other pair member (58.6 vs. 51.2). Ten (45.5%) FFMs were spouses or partners of an HD participant, 7 (31.8%) were adult children of an HD participant, 2 (9.1%) were siblings, 2 (9.1%) were friends, and 1 (4.5%) was a parent. Eleven (50%) of the FFMs were living with the individuals with HD about whom they completed the measures; of these, 8 (72.7%) were the HD individual’s significant other, and the remaining 3 were the HD individual’s parent (27.3%).
Participants were included only if they met standard Hoarding Rating Scale criteria: a score of “moderate” or above on subscale items assessing difficulty discarding, clutter, and impairment or distress (Tolin, Frost, Steketee, Gray, & Fitch, 2008; Tolin, Frost, & Steketee, 2010). This inclusion criterion was utilized to ensure the validity of a clinical hoarding sample.
2.1.2. Materials
All packets contained an informed consent document, as well as a letter instructing participants not to discuss their responses with the other member of the pair until all measures were completed. All measures of symptom severity were completed in relation to the HD participant’s home or behaviors unless otherwise noted. The HD and FFM packets contained the following measures:
A Demographics Questionnaire was used to collect information about the age, sex, race/ethnicity, relationship status, employment status, and educational status of all participants. FFMs were also asked to indicate the age and gender of the HD, their relationship to the HD, and whether they were currently living with the HD.
The Clutter Image Rating (CIR; Frost, Steketee, Tolin, & Renaud, 2008) includes a series of 9 photographs each of a kitchen, living room, and bedroom with varying degrees of clutter. Participants are requested to select the photograph that most closely resembles each of the three rooms in the HD’s home. Internal consistency, test-retest reliability, and inter-rater reliability for the CIR are high, as are correlations with validated hoarding measures (Frost, Steketee, Tolin, & Renaud, 2008).
The Saving Inventory-Revised (SI-R; Frost, Steketee, & Grisham, 2004) is a 23-item questionnaire of compulsive hoarding severity. The SI-R is composed of 3 subscales, mirroring the core symptoms of compulsive hoarding: Clutter (9 items), Difficulty Discarding (7 items), and Acquisition (7 items). Internal consistency was excellent for the total score (α= 0.92) and for the 3 subscales (α= .87–.91) (Frost, Steketee, & Grisham, 2004). Principal component analysis demonstrated that the aforementioned factors account for 70.82% of the total variance, and the results of a multivariate regression analysis indicated favorable convergent validity (Mohammadzadeh, 2009).
The Activities of Daily Living in Hoarding scale (ADL-H; Frost, Hristova, Steketee, & Tolin, 2012) contains 15 questions about daily activities that may be affected by hoarding (i.e., eating, sleeping, use of furniture). The ADL-H was modeled after similar measures used in health service settings to assess impairment of behavioral activities due to illness. Preliminary findings indicated good internal consistency and discriminant validity in relation to measures of hoarding severity and other psychopathology. As in the original publication, the ADL-H scores in the present research are means rather than total scores.
The Sheehan Disability Scale (SDS; Leon, Shear, Portera, & Klerman, 1992) is a brief self-report measure of work, social, and family disability on 10-point scales. The SDS has demonstrated acceptable reliability and satisfactory construct and criterion-related validity in a study of panic patients (Leon et al., 1992) and has proven sensitive to treatment effects in obsessive-compulsive disorder (OCD) patients (Diefenbach, Abramowitz, Norberg, & Tolin, 2007).
The Clinical Global Impression Severity Scale (CGI; Guy, 1976) is a widely used single-item instrument assessing global severity on a 7-point scale from 1 (“Not at all ill”) to 7 (“Extremely ill”). The CGI has demonstrated good inter-rater reliability and is frequently used in clinical and research settings to establish baseline severity of illness, as well as assess changes during and after treatment. We used a participant-rated version of the CGI (Hannan & Tolin, 2007) to assess both participants’ overall impressions of illness severity.
The Home Environment Index (HEI; Rasmussen, Steketee, Tolin, Frost, & Brown, submitted for publication) is a 20-item self-report measure containing items that assess squalor in hoarding, particularly in terms of domestic conditions and personal care. Internal reliability for the scales was good (α = .89). Convergent validity was evident in stronger correlations of the HEI with measures of hoarding than measures of OCD, depression, anxiety, and stress.
The Hoarding Rating Scale-Self-Report (HRS-SR; Tolin, Frost, Steketee, Gray, & Fitch, 2008) is a self-report adaptation of the interview version of the HRS (HRS-I; Tolin, Frost, & Steketee, 2010). This measure was used to determine the severity of illness of the HDs. Like the interview, the HRS-SR consists of 5 Likert-type ratings from 0 (“None”) to 8 (“Extreme”) of clutter, difficulty discarding, excessive acquisition, distress, and impairment. The HRS-I showed excellent internal consistency and test-retest reliability (Tolin, Frost, & Steketee, 2010); the HRS-SR correlated strongly with the HRS-I (Tolin, Frost, Steketee, Gray, & Fitch, 2008) and demonstrated 73% agreement of diagnostic status between clinician- and self-report (Tolin et al., 2008).
The Depression Anxiety Stress Scale (DASS; Lovibond & Lovibond, 1995) is a 42-item self-report measures that assesses symptoms of depression, anxiety, and stress experience over the past week. Items are rated on a 4-point scale from 0 (“Did not apply to me at all”) to 3 (“Applied to me very much, or most of the time”). Previous studies have shown that the three scales demonstrated good internal consistency, and factor analyses supported the convergent and discriminant validity of the scales. In addition, the DASS demonstrated adequate test-retest reliability, and adequately distinguished between clinician-rated mood and anxiety disorders (Brown, Chorpita, Korotitsch, & Barlow, 1997). In Study 1, both HD individuals and FFMs completed the DASS in terms of their own personal ratings.
The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS; Goodman et al., 1989) item 11 was used to assess insight. Originally designed for clinician interviewers, the Y-BOCS has shown good psychometric properties as a self-report instrument (Steketee, Frost, & Bogart, 1996). Individuals with HD were asked to rate the extent to which they believe they have a hoarding problem; FFMs completed a parallel measure, used in previous research (Tolin, Fitch, Frost, & Steketee, 2010), in which they rated the HD individual’s level of insight as 0 = Excellent insight/fully rational, 1 = Good insight, 2 = Fair insight, 3 = Poor insight, or 4 = Lacks insight/delusional. See Tolin et al. (2010) for the complete scale. Previous analyses in a related study indicated that FFMs’ insight ratings correlate significantly with discrepancy of perceived opinion about various aspects of hoarding between individuals with HD and FFMs (Tolin, Fitch, Frost, & Steketee, 2010).
The HD packets, but not the FFM packets, contained the following measure:
The Magical Ideation Scale (MIS; Eckblad & Chapman, 1983) is a 30-item true/false scale measuring belief in forms of causation that by conventional standards are invalid (i.e. “I think I could learn to read others’ minds if I wanted to”). Internal consistency coefficients for the MIS ranged from .82 to .85, and it was modestly correlated with the Perceptual Aberration Scale (PAS). Those with high MIS scores were disproportionately more likely than those with low scores to meet diagnostic criteria for mood, personality, and psychotic disorders (Eckblad & Chapman, 1983).
The FFM packets, but not the HD packets, contained the following measure:
The Patient Rejection Scale (PRS; Kreisman, Simmens, & Joy, 1979) was used to assess friend and family member frustration. This 11-item measure assesses rejecting or hostile attitudes toward the target individual (i.e., “I don't expect much from him/her anymore;” “I wish he/she had never been born”), in this case the HD participant. Items are rated from 1 (“Never”) to 3 (“Often”), with 5 reverse-scored items. Scores on the PRS can range from 11–33. The PRS showed high internal consistency and test-retest reliability (Kreisman et al., 1979), and has been demonstrated to be elevated in family members of patients with OCD (Amir, Freshman, & Foa, 2000) and HD (Tolin, Frost, Steketee, & Fitch, 2008).
2.1.3. Procedure
Study 1 was approved by the Institutional Review Board at Hartford Hospital. Pairs of participants were assigned a code number, and each half of the pair was assigned a letter to distinguish him/her as the individual with HD or the FFM.
2.2. Results
Difference scores between the HD participant and the FFM’s ratings were calculated for each measure and examined in relation to demographic data, symptom severity, and impairment severity. We then conducted the same analyses, controlling for the FFM’s Patient Rejection Scale scores. Repeated-measures analyses of variance (ANOVAs), uncontrolled and controlling for FFM PRS score, were calculated for each measure (Table A.1). As demonstrated in Table A.1., HD participants’ MIS scores were minimal, indicating that their self-assessments were not affected by the presence of psychosis. Descriptive statistics demonstrated a consistent tendency by the individual with HD to report lower severity of their hoarding symptoms and other variables in comparison to their FFM; the most notable differences were evident in HD participants’ lower estimates of clutter (CIR), acquiring behavior (SI-R), domestic squalor (HEI), and global illness severity (CGI-Severity); however, only SI-R acquiring remained so after controlling for patient rejection (PRS) scores. Thus, results demonstrated differences between groups on a variety of measures when considered independently. However, when the PRS was added as a covariate, these differences were no longer significant.
Table A.1.
Study 1 comparisons of ratings made by hoarding disorder (HD) participants versus those made by friends/family members (FFMs), uncontrolled and controlling for FFM Patient Rejection Scale (PRS) scores.
| HD Participant (M, SD) |
FFM (M, SD) |
F without PRS covariate |
F with PRS covariate |
Cronbach’s α (HD) |
|
|---|---|---|---|---|---|
| ADL-H | 1.76 (0.73) | 1.99 (0.97) | 2.47 | 0.11 | 0.94 |
| CGI-Severity | 3.10 (1.41) | 4.00 (1.56) | 4.41a | 0.00 | -- |
| CIR | 3.52 (1.55) | 4.29 (2.02) | 6.27a | 1.17 | 0.85 |
| DASS Anxiety | 5.71 (7.22) | 5.05 (5.57) | 0.10 | 0.05 | 0.84 |
| DASS Depress. | 12.76 (10.13) | 12.10 (13.59) | 0.03 | 1.49 | 0.96 |
| DASS Stress | 13.05 (8.85) | 13.71 (11.60) | 0.04 | 1.03 | 0.91 |
| HEI Total | 26.21 (8.14) | 29.94 (10.38) | 5.08a | 2.84 | 0.80 |
| MIS Total | 6.00 (5.22) | -- | -- | -- | -- |
| SDS Total | 12.67 (9.17) | 13.02 (7.74) | 0.04 | 1.62 | 0.88 |
| SI-R Acquiring | 13.82 (5.73) | 16.64 (4.07) | 5.32a | 3.82a | 0.75 |
| SI-R Clutter | 22.27 (8.08) | 24.41 (7.34) | 2.65 | 2.62 | 0.93 |
| SI-R D.D. | 16.77 (6.50) | 17.41 (2.72) | 0.17 | 1.19 | 0.80 |
| SI-R Total | 52.86 (18.05) | 58.46 (2.66) | 2.33 | 2.88 | 0.94 |
| Y-BOCS #11 | 0.86 (1.17) | 1.55 (1.18) | 3.07a | 4.22a | -- |
| PRS | -- | 21.55 (2.05) | -- | -- | -- |
p < .05
Note. ADL-H = Activities of Daily Living in Hoarding; CGI = Clinical Global Impression; CIR = Clutter Image Rating; DASS = Depression Anxiety Stress Scale; HEI = Home Environment Index; MIS = Magical Ideation Scale; SDS = Sheehan Disability Scale; SI-R = Saving Inventory—Revised; Y-BOCS = Yale-Brown Obsessive-Compulsive Scale.
Also significant was the discrepancy in assessments of insight: HD participants’ significantly lower scores on Y-BOCS item 11 indicate that they believed they mostly recognized their hoarding problems, whereas their relatives believed they were reluctant to admit the problem. This difference remained significant after controlling for PRS scores.
A CGI discrepancy score was calculated by subtracting the HD individual’s CGI score from the FFM’s CGI score. Accordingly, a score of “2” indicates that the family member’s rating of hoarding severity was 2 points higher than that of the individual with HD. The mean (standard deviation) CGI discrepancy score was 0.90 (1.92); the range was -3 to 4. Correlations between CGI discrepancy scores and various measures can be seen in Table A.2. Older participants demonstrated greater discrepancy scores with their FFMs than did their younger counterparts. CGI discrepancy scores did not correlate significantly with the FFMs’ patient rejection attitudes (PRS).As reported in Table A.2, when hoarding severity (HRS score) was controlled for, the correlations between CGI discrepancy scores and other measures did not change significantly.
Table A.2.
Correlations between Clinical Global Impression (CGI) discrepancy scores and various measures in Study 1, with and without Hoarding Rating Scale scores as a covariate.
| HD Participant (without covariate) |
FFM (without covariate) |
HD Participant (with HRS covariate) |
FFM (with HRS covariate) |
|
|---|---|---|---|---|
| ADL-H | −0.09 | 0.27 | −0.09 | 0.30 |
| Age | 0.51a | −0.11 | 0.50a | −0.06 |
| DASS Anxiety | −.015 | −0.07 | −0.36 | −1.0 |
| DASS Depress. | −0.03 | 0.12 | −0.39 | 0.14 |
| DASS Stress | −0.24 | 0.28 | −0.36 | 0.29 |
| HEI Total | −0.20 | 0.18 | −0.60b | −0.17 |
| SDS Total | −0.13 | 0.47a | −0.46 | 0.28 |
| SI-R Acquiring | −0.46a | 0.44 | −0.74b | 0.20 |
| SI-R Clutter | −0.10 | 0.43 | −0.47b | 0.19 |
| SI-R D.D. | −0.62b | 0.63b | −0.68b | 0.53a |
| SI-R Total | −0.28 | 0.53a | −0.68b | 0.42 |
| YBOCS #11 | 0.38 | 0.58a | 0.37 | 0.54a |
p < .05;
p < .01
Note. Magnitude of correlations did not change when selecting only those pairs that live together (N = 11).
Note. ADL-H = Activities of Daily Living in Hoarding; DASS = Depression Anxiety Stress Scale; HEI = Home Environment Index; PRS = Patient Rejection Scale; SDS = Sheehan Disability Scale; SI-R = Saving Inventory— Revised; Y-BOCS = Yale-Brown Obsessive-Compulsive Scale.
A stepwise linear regression was used to predict family members’ ratings on Y-BOCS item 11 (insight). Predictors included discrepancy scores on the ADL-H, CGI, HEI, SDS, and SI-R, as well as the separate family members’ ratings of their relative on the ADL-H, CGI, HEI, SDS, and SI-R and family members’ distress on the DASS. The only significant predictor of family members’ Y-BOCS item 11 scores was the CGI discrepancy score, which accounted for 38.4% of the variance (F1,18 = 9.15, p = .007, β = 0.58). No other variables added significantly to the model.
2.3. Discussion
Results from this study suggest significant differences between individuals with HDs’ and their friends/family members’ perceptions of hoarding behaviors and their associated functional impact. As noted above, individuals with HD reported lower severity of clutter, acquiring behavior, impact on activities of daily living and safety, and domestic squalor than did their friends and family members. They also described themselves as possessing better insight than did their friends/family members. However, only acquiring and insight remained significantly different when rejecting attitudes of family members were taken into account, suggesting that these attitudes might impair the judgment of family members.
From the Study 1 results, it cannot be determined whether these differences are due to the individual with HD under-reporting, the friend or family member over-reporting, or a combination of the two. Previous research has supported both interpretations (Frost & Steketee, 1999; Tolin, Frost, Steketee, & Fitch, 2008). In Study 1, when the hostility and rejection felt by FFMs is taken into account, significant differences between the two raters disappeared (Table A.2), which may suggest that the FFMs over-reported due to strong negative emotions. However, rejection attitudes did not correlate significantly with the discrepancy of overall illness severity, suggesting that rejection was unlikely to account for the differences.
Because the current research is cross-sectional rather than experimental, an alternate causal pathway to the one proposed above may also be possible. For example, an HD individual with low insight and significant discrepancies between his/her own and family members’ perceived severity of hoarding may produce more tension and rejecting attitudes among family members. An objective indication of severity (such as scores from an external rater) may have helped clarify the nature of this relationship.
The small sample size of Study 1 also limits the conclusions that can be drawn. Though 110 pairs of participants were recruited, only 22 pairs completed both assessments. Also, Study 1 did not include ratings from an objective, trained rater without emotional investment in the situation. Thus, in Study 2, we sought to compare ratings of individuals with HD to those of trained raters. As in Study 1, we predicted that HD participants’ low insight would result in the under-reporting of their symptoms in comparison to ratings made by IEs.
3. Study 2
3.1. Method
3.1.1. Participants
Participants were recruited from health and mental health clinics, newspapers and informational websites, and media appearances made by the investigators. The sample included 183 participants (75% women; 88% white) with an average age of 53.2 years (SD=9.6). All participants were interviewed by independent evaluators, and found to meet criteria for clinical hoarding based on moderate or greater clutter, difficulty discarding, and either distress or impairment from hoarding on the HRS-I.
3.1.2. Materials
As in Study 1, participants and independent evaluators (IEs) completed the CIR, CGI, and ADL-H; participants also completed a demographics questionnaire. Additionally, participants and IEs completed the Clutter Scale (CS; Hartl, Allen, Frost, & Steketee, 2002), which contains seven questions about the condition of three target rooms (living room, kitchen, bedroom), including space occupied by clutter, neatness, organization, ease of finding items, difficulty walking, cluttered furniture tops, and floor spaces. Each question was scored on a 7-point scale with possible scores ranging from 7 to 49, with higher scores indicating more clutter. Internal consistencies for CS ratings range from 0.87 to 0.94 (Frost et al., 2008). Individuals with HD completed all self-report measures at the baseline appointment, and again during a home visit; the evaluator completed all clinician-administered measures at the home visit.
3.1.3. Procedure
This study was approved by the Institutional Review Boards at Smith College, Boston University, and Hartford Hospital. All participants signed an informed consent form before beginning participation at either the Boston University or The Institute of Living/Hartford Hospital site. Clinical interviews were conducted in participants’ homes by master’s level clinical psychologists, postdoctoral fellows, or senior research assistants supervised by licensed psychologists. Participants who met diagnostic criteria completed the self-report forms. Complete procedures for Study 2 can be found in Frost et al. (2008).
3.2. Results
As reported in Table A.3, significant differences were found between HD participant and IE ratings for CGI-Severity and Clutter Scale scores for Kitchen and Bedroom. HD participants assigned themselves significantly more severe scores on CGI-Severity, but the pattern was reversed for CS scores, for which they reported less kitchen and living room clutter.
Table A.3.
Study 2 comparisons of ratings made by individuals with HD versus those made by independent evaluators at the home visit.
| HD Participant (M, SD) |
Independent Evaluator (M, SD) |
t | Cronbach’s α (HD) |
|
|---|---|---|---|---|
| ADL-H | 1.89 (0.76) | 1.97 (0.82) | 1.47 | 0.94 |
| CGI | 5.21 (1.01) | 4.71 (0.94) | 5.24a | -- |
| CIR | 3.72 (1.60) | 3.70 (1.59) | 0.25 | 0.77 |
| CS Bedroom | 33.75 (10.40) | 35.85 (8.86) | −3.48a | − 0.01 |
| CS Kitchen | 29.02 (11.18) | 31.02 (9.21) | −3.00a | −0.09 |
| CS Living Room | 30.55 (11.87) | 31.84 (10.63) | −.92 | −0.10 |
| SI-R Acquiring | 15.7 (5.7)b | -- | -- | 0.69 |
| SI-R Clutter | 25.8 (6.4)b | -- | -- | 0.89 |
| SI-R D.D. | 17.7 (6.7)c | -- | -- | 0.71 |
| SI-R Total | 60.5 (13.4)b | -- | -- | 0.87 |
p < .05;
missing data for 62 participants;
missing data for 53 participants.
Note. ADL-H = Activities of Daily Living in Hoarding; CGI = Clinical Global Impression; CIR = Clutter Image Rating; CS = Clutter Scale; SI-R = Savings Inventory—Revised.
In order to determine whether rater discrepancies might be explained by a tendency to under- or over-report hoarding severity by HD participants or evaluators, a discrepancy score was calculated for the difference in rater scores on the CGI. HD participant’s CGI scores were subtracted from IE scores yielding a mean of −0.50 (SD=1.06), with a range of −6.00 to 3.00; scores farther from 0 reflected greater discrepancy, with negative scores indicating higher ratings by the HD participant and positive scores reflecting higher ratings by the IE.
Table A.4 presents correlations between CGI discrepancy scores and various hoarding measures, as well as partial correlations controlling for HRS ratings by IEs. All correlations between the CGI discrepancy scores and the IEs’ ratings were significant and positive, indicating that more discrepancy between self- and clinician-rated CGI scores was associated with more severe IE ratings of hoarding severity on all measures. In contrast to the IE ratings, three of the four self-report scales (SIR-Acquiring, Difficulty Discarding, and Total score) were significantly negatively correlated with CGI Discrepancy scores. That is, more discrepant self and assessor ratings were associated with lower self-rated hoarding. However, these correlations were no longer significant when hoarding severity (HRS) was controlled.
Table A.4.
Study 2 correlations between Clinical Global Impression (CGI) discrepancy scores and various measures at the home visit, with and without Hoarding Rating Scale scores as a covariate.
| HD Participant (without covariate) |
IE (without covariate) |
HD Participant (with HRS covariate) |
IE (with HRS covariate) |
|
|---|---|---|---|---|
| ADL-H | −0.05 | 0.19 | 0.08 | 0.30b |
| CIR | 0.11 | 0.25a | 0.18 | 0.34b |
| CS Bedroom | 0.05 | 0.25a | 0.07 | 0.27b |
| CS Kitchen | 0.06 | 0.27a | 0.10 | 0.38b |
| CS Living Room | 0.03 | 0.23a | 0.11 | 0.33b |
| SI-R Acquiring | −0.27b | -- | −0.06 | -- |
| SI-R Clutter | −0.16 | -- | −0.09 | -- |
| SI-R Difficulty | −0.22a | -- | −0.09 | -- |
| Discarding | ||||
| SI-R Total | −0.27a | -- | −0.12 | -- |
p < .05;
p < .01
Note. ADL-H = Activities of Daily Living in Hoarding; CIR = Clutter Image Rating; CS = Clutter Scale; SI-R = Saving Inventory—Revised.
3.3. Discussion
Analyses identified three significant differences between HD and IE ratings of hoarding severity, one of which was associated with higher scores made by the HD participant (CGI-Severity), and two of which were associated with higher scores made by the IE (Clutter Scale—Kitchen and Clutter Scale—Bedroom). Thus, while HD participants may under-report certain aspects of their hoarding, their overall global impressions do not demonstrate a lack of insight as reflected in the discrepancy scores. If anything, the results suggested that HD participants may have over-reported their CGI score compared to independent observers. As in Study 1, partial correlations controlling for hoarding severity in most cases supported the validity and utility of the CGI discrepancy scores.
Overall, the relatively few significant differences between HD participants’ and IEs’ measures of hoarding severity suggest that HD participants may be reasonably accurate when reporting on the severity of their hoarding. In fact, milder cases—as identified by lower CGI-S scores—demonstrated a somewhat greater discrepancy between their ratings and those made by their independent evaluators across various measures. However, even with these cases, the correlations were small.
4. General Discussion
4.1. Synthesis
While in Study 1 the majority of the discrepancies in scores could be attributed to HD participants’ under-reporting in comparison to their friends/family members, findings also demonstrated that family members’ evaluations seem to be moderated by their degree of their rejection of the individual with HD. The results from Study 2 were more complicated. Specifically, few significant differences were evident between mean ratings by HD and IE participants; and in one of the cases where there was a discrepancy, HD participants rated themselves more severely. This finding suggests a more aligned relationship between the global evaluations made by individuals with HD and their IEs than between those made by individuals with HD and their FFMs.
Our results also indicate that friends and family members’ rejections of the individuals with HD were related to their over-reporting of the severity of the hoarding and the discrepancies between the two groups’ ratings. Specifically, differences in ratings were present for various measures when those measures were considered independently; however, those differences disappeared when PRS was included as a covariate. This suggests that rejection significantly impacts friends and family members’ evaluations of their loved ones’ hoarding symptoms. Additional research must be done to identify what other factors may contribute to these differences.
The considerable impact of rejecting attitudes on family members’ evaluations may be due to the fact that their lives are negatively affected by the hoarding behaviors. Previous research has demonstrated the burden of compulsive hoarding on family members, and its tendency to engender family conflict (Tolin, Frost, Steketee, Gray, & Fitch, 2008). Because of this, and because they may lack objectivity, family members may over-report the severity of hoarding behaviors and their consequences especially when they are frustrated and angry at the relative who hoards. Despite this, family member response is important to understanding hoarding and its treatment, and familial support may improve therapy outcomes.
Thus, some evidence demonstrated that greater difference scores between the HD participant and the independent evaluators’ were positively associated with IE’s ratings of hoarding severity and negatively associated with HD participants’ self-ratings. Taken together, then, the results of these two studies demonstrate a complicated interaction in the evaluations of hoarding severity by varying individuals, each with their own perspective on the situation and its effects. Significantly, the results of these studies cannot definitively identify or determine which perspective is the most objectively accurate or reliable.
Future research should assess how well HD clients judge the severity of their symptoms compared to other clinical groups, such as non-hoarding OCD and depressed patients. Because scientific literature and clinical impressions tend to characterize HD clients as being particularly limited in terms of insight, and insight is included as a specifier for HD diagnosis in the DSM-5 (Mataix-Cols et al., 2012), it is important to evaluate the validity of this assumption by comparing HD to other clinical samples on this symptom.
4.2. Limitations
The present research is limited by its cross-sectional design and self-report assessment from participants in both studies. Future studies that include reports from patients, family/friends and independent assessors on the same HD participant, as well as behavioral/experimental tests of insight are needed. In addition, Study 1 was limited by its small sample size.
A second significant limitation was the potential selection bias inherent in recruiting individuals who volunteer or are invited by a friend or family member to participate in a study about their insight into hoarding severity. It is unlikely that HD individuals with low insight into their hoarding symptoms will engage in such research. Thus, the samples in both Study 1 and Study 2 may comprise a subset of the HD population that excludes the least insightful individuals and for whom under-reporting is comparatively less problematic.
4.3. Conclusion
Ultimately, our findings demonstrate that the evaluations of friends and family members are moderated by the degree of their rejection of the individual with HD. Furthermore, though HD participants may under-report or lack insight regarding the specifics of their hoarding (i.e. the severity of clutter in a given room) in comparison to independent evaluators, the majority of their scores either demonstrated no significant difference from those made by IEs—or, in the case of a global impression score, actually demonstrated over-reporting.
A clearer picture of the accuracy of reports about hoarding may be obtained using matched evaluations from HD participants, their friends and family, and their treatment providers or a home observer. If all of these individuals with hoarding disorder, their friends or family members, and their treatment providers were to all completed the same questionnaires about the severity and functional impact of the compulsive hoarding behaviors, a fuller picture of this complex and often puzzling disorder would be better achieved—and this, in turn, would help to better inform not only future research, but also future treatment.
Highlights.
►The results of two studies evaluating insight in Hoarding Disorder were considered. ► Study 1 suggests that family members may over-report the severity of symptoms. ► Study 2 suggests that patients may underreport the severity of specific symptoms. ► Study 2 also suggests that patients may over-report their global symptom severity. ► The ratings of patients, family members and therapists should be evaluated jointly.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amir N, Freshman M, Foa EB. Family distress and involvement in relatives of obsessive-compulsive disorder patients. Journal of Anxiety Disorders. 2000;14:209–217. doi: 10.1016/s0887-6185(99)00032-8. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- Damecour CL, Charron M. Hoarding: a symptom, not a syndrome. Journal of Clinical Psychiatry. 1998;59:267–272. [PubMed] [Google Scholar]
- Diefenbach GJ, Abramowitz JS, Norberg MM, Tolin DF. Changes in quality of life following cognitive-behavioral therapy for obsessive-compulsive disorder. Behaviour Research and Therapy. 2007;45:3060–3068. doi: 10.1016/j.brat.2007.04.014. [DOI] [PubMed] [Google Scholar]
- Eckblad M, Chapman LJ. Magical ideation as an indicator of schizotypy. Journal of Consulting and Clinical Psychology. 1983;51:215–225. doi: 10.1037//0022-006x.51.2.215. [DOI] [PubMed] [Google Scholar]
- Frost RO, Hristova V, Steketee G, Tolin DF. Activities of Daily Living Scale in hoarding disorder. 2012 doi: 10.1016/j.jocrd.2012.12.004. Submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, Steketee G. Issues in the treatment of compulsive hoarding. Cognitive and Behavioral Practice. 1999;6:397–407. [Google Scholar]
- Frost RO, Steketee G, Grisham J. Measurement of compulsive hoarding: Saving Inventory-Revised. Behaviour Research and Therapy. 2004;42:1163–1182. doi: 10.1016/j.brat.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Tolin DF, Renaud S. Development and validation of the Clutter Image Rating. Journal of Psychopathology and Behavioral Assessment. 2008;32:401–417. [Google Scholar]
- Frost RO, Tolin DF, Maltby N. Insight-related challenges in the treatment of hoarding. Cognitive and Behavioral Practice. 2010;17:404–413. [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Guy W. Assessment manual for psychopharmacology. Washington, DC: U.S. Government Printing Office; 1976. [Google Scholar]
- Hannan SE, Tolin DF. Examination of the validity of therapist rated and patient rated Clinical Global Impression scores. Paper presented at the Annual Meeting of the Association of Behavioral and Cognitive Therapies, Philadelphia; 2007. Nov, [Google Scholar]
- Hartl TL, Allen GJ, Frost RO, Steketee G. Validation of a new measure of clutter to asses room and photographs. 2002. Unpublished manuscript. [Google Scholar]
- Kreisman DE, Simmens SJ, Joy VD. Rejecting the patient: preliminary validation of a self-report scale. Schizophr Bull. 1979;5:220–222. doi: 10.1093/schbul/5.2.220. [DOI] [PubMed] [Google Scholar]
- Leon AC, Shear MK, Portera L, Klerman GL. Assessing impairment in patients with panic disorder: The Sheehan Disability Scale. Social Psychiatry and Psychiatric Epidemiology. 1992;27:78–82. doi: 10.1007/BF00788510. [DOI] [PubMed] [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney: The Psychology Foundation of Australia; 1995. [Google Scholar]
- Mataix-Cols D, Billotti D, Fernández de la Cruz L, Nordsletten AE. The London field trial for hoarding disorder. Psychological Medicine. 2012 doi: 10.1017/S0033291712001560. Available on CJO 2012 doi: 10.1017/S0033291712001560. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Marks IM, Greist JH, Kobak KA, Baer L. Obsessivecompulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychotherapy and Psychosomatics. 2002;71:255–262. doi: 10.1159/000064812. [DOI] [PubMed] [Google Scholar]
- Mohammadzadeh A. Validation of Saving Inventory-Revised (SI-R): Compulsive Hoarding Measure. Iranian Journal of Psychiatry and Clinical Psychology. 2009;15:33–41. [Google Scholar]
- Rasmussen JL, Steketee G, Tolin DF, Frost RO, Brown TA. Assessing squalor in hoarding: The home environment index. doi: 10.1007/s10597-013-9665-8. (submitted for publication) [DOI] [PubMed] [Google Scholar]
- Steketee G, Frost RO, Bogart K. The Yale-Brown Obsessive Compulsive Scale: interview versus self-report. Behaviour Research and Therapy. 1996;34:675–684. doi: 10.1016/0005-7967(96)00036-8. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Fitch KE, Frost RO, Steketee G. Family informants' perceptions of insight in compulsive hoarding. Cognitive Therapy and Research. 2010;34:69–81. [Google Scholar]
- Tolin DF, Frost RO, Steketee G. A brief interview for assessing compulsive hoarding: the Hoarding Rating Scale-Interview. Psychiatry Research. 2010;178:147–152. doi: 10.1016/j.psychres.2009.05.001. doi: S0165-1781(09)00178-4 [pii] 10.1016/j.psychres.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, Fitch KE. Family burden of compulsive hoarding: results of an internet survey. Behaviour Research and Therapy. 2008;46:334–344. doi: 10.1016/j.brat.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, Gray KD, Fitch KE. The economic and social burden of compulsive hoarding. Psychiat Res. 2008;160:200–211. doi: 10.1016/j.psychres.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]