Abstract
Background
Post-traumatic sepsis is a significant cause of in-hospital death. However, socio-demographic and clinical characteristics that may predict sepsis in injured patients are not well known. The objective of this study was to identify risk factors that may be associated with post-traumatic sepsis.
Methods
Retrospective analysis of patients in the National Trauma Data Bank for 2007–2008. Patients older than 16 years of age with an Injury Severity Score (ISS) ≥9 points were included. Multivariable logistic regression was used to determine association of sepsis with patient (age, gender, ethnicity, and insurance status), injury (mechanism, ISS, injury type, hypotension), and clinical (major surgical procedure, intensive care unit admission) characteristics.
Results
Of a total of 1.3 million patients, 373,370 met the study criteria, and 1.4% developed sepsis, with an associated mortality rate of approximately 20%. Age, male gender, African-American race, hypotension on emergency department presentation, and motor vehicle crash as the injury mechanism were independently associated with post-traumatic sepsis.
Conclusions
Socio-demographic and injury factors, such as age, race, hypotension on admission, and severity and mechanism of injury predict post-traumatic sepsis significantly. Further exploration to explain why these patient groups are at increased risk is warranted in order to understand better and potentially prevent this life-threatening complication.
With an estimated 750,000 cases annually, severe sepsis is the tenth leading cause of death overall in the United States [1–3]. Sepsis is the principal cause of in-hospital death outside of coronary intensive care units (ICUs), and surgical patients account for one-third of all diagnosed cases [4]. Physiology of sepsis in surgical patients is believed to be distinct because of immune modulation associated with surgery and trauma [5]. Current literature suggests a mortality rate of 17%–23% in patients who develop post-traumatic sepsis during their hospital stays [6–8]. Knowledge of patient- and injury-specific characteristics associated with its development may help in early identification of this complication and timely intervention to improve clinical outcomes. However, our understanding of the relation between patient and injury characteristics and predisposition to post-traumatic sepsis is limited [6,7].
The primary objective of this study was to identify the role of socio-demographic and injury characteristics in predisposition to post-traumatic sepsis in moderately to severely injured patients. This study also explored associations between these characteristics and death in patients who developed sepsis.
Patients and Methods
Data source
This study retrospectively analyzed adult patients entered in the National Trauma Data Bank (NTDB) between 2007 and 2008. The NTDB is maintained by the American College of Surgeons and contains data contributed by more than 900 trauma centers in the United States and its territories. Data reporting to the NTDB is voluntary, and some institutions do not submit complication and demographics information. Patients from facilities that did not submit data on complications and insurance status were therefore excluded. We calculated the percentage of missing information for the complications field for each facility and included only patients from facilities that reported at least one patient with sepsis. A similar strategy has been successful in work published previously to address the potential for differential reporting of complications across centers [27]. We further excluded patients who died in the emergency department. Patients 16 years of age or older who had a penetrating or blunt injury and an Injury Severity Score (ISS) of ≥9 points were included.
Outcomes
The primary outcome of this study was development of sepsis during the hospital stay. The secondary outcome was death in patients with sepsis. By consensus, sepsis has been defined as the combination of a pathologic infection and physiologic changes that constitute the systemic inflammatory response syndrome (SIRS) [9]. Patients were deemed to have sepsis if they were identified to have “systemic sepsis” in the hospital complications field of the NTDB or any of the following International Statistical Classification of Disease (ICD)-9 discharge diagnosis codes associated with sepsis: 038 (septicemia), 020.0 (septicemic), 790.7 (bacteremia), 117.9 (disseminated fungal infection), 112.5 (disseminated Candida infection), and 112.81 (disseminated fungal endocarditis). These codes were chosen as they were used in a large study of sepsis among surgical patients [10]. The field “systemic sepsis” is defined in the NTDB as definitive evidence of infection, plus evidence of a systemic response to infection. This systemic response is manifested by the presence of infection and two or more of the following conditions: (1) Temperature >38°C or <36°C; (2) sepsis with hypotension despite adequate fluid resuscitation combined with perfusion abnormalities that may include, but are not limited to, lactic acidosis, oliguria, or an acute alteration in mental status. Patients who are on inotropic or vasopressor agents may not be hypotensive at the time perfusion abnormalities are measured; (3) heart rate >90 beats/min; (4) ventilator rate >20 breaths/min or PaCO2 <32 mm Hg (<4.3 kPa); and (5) white blood cell (WBC) count >12,000 cell/mm3, <4,000 cells/mm3, or >10% immature (band) forms. This study used data from 2007 onward because of the implementation of the National Trauma Data Standards (NTDS) in 2007 [11]. The goal of the NTDS is to “improve the quality of data in the NTDB by standardizing the inclusion criteria, data coding and methods of data collection” [11]. Thus, data on complications have been reported more consistently in recent years. The NTDS requires that hospitals report complication data recorded on the hospital discharge sheet, history and physical record, and billing sheet, in order of hierarchy.
Patient demographics included age, gender, and race/ethnicity [14]. Injury characteristics were ISS, presence of shock at admission (systolic blood pressure <90 mm Hg) [12], motor component of the Glasgow Coma Scale (GCS) score, type of injury (blunt vs. penetrating), and mechanism of injury. For model parsimony, the mechanisms of injury were categorized into fall, motor vehicle crash, and other (pedestrians struck, bicyclists, and motorcyclists) [13]. Clinical characteristics retrieved were major surgical intervention, length of stay, ICU-free length of stay, admission in and duration of ICU stay, requirement for and number of ventilator days, and death. The ICD-9 codes were used to categorize major surgical procedures into the following groups: Nervous system (01.00–05.99); respiratory, cardiovascular, digestive, and urinary system (30.00–59.99); and musculoskeletal system (77.00–78.99, 81.00–81.99, 83.00–84.99) Finally, insurance status was added to the model to control for differences in outcomes based on reported insurance status (insured vs. uninsured) [15]. Uninsured patients were defined only as those who were listed as “self-pay,” whereas patients with all other types of funding, including Medicaid and Medicare, were classified as insured [16].
Statistical analysis
The Student t-test was used to compare continuous variables. If the assumptions of this test were not met, the Mann-Whitney U test was used instead. Chi-square analysis was used to compare categorical variables. Multivariable logistic regression was used to determine the independent predictors of sepsis and their effect sizes after adjustment for potential confounders. The final model included the following variables: Age, sex, race, motor component of the GCS score, ISS, presence of shock on admission, type and mechanism of injury, insurance status, major surgical intervention, and ICU admission. Only adjusting for anatomic measures of injury severity raises the question of residual confounding. Therefore, we also included physiologic measures of injury severity (motor component of the GCS score and presence of shock on admission) in the final model. We have previously demonstrated that the combination of these two physiological parameters, motor component of the GCS score, shock are excellent predictors of death [12]. Ventilator requirement was not included in the final model because of its co-linearity with the motor component of the GCS score. No significant interaction was found between ISS and hypotension or ISS and GCS score. To control for the potential differences in treatments and procedures at various facilities, clustering by facility identifier was included during the multivariable analysis [17]. In a separate analysis, death was considered the primary outcome in patients with sepsis, and all the co-variates mentioned above were controlled for in the model. To ensure that missing data did not bias the results, a sensitivity analysis using multiple imputation was performed [18]. Multiple imputation was performed five times for each variable to generate five imputed datasets. The average values of these five datasets were used to obtain the odds ratios (ORs) in the final multiple logistic regression model. All analyses were done using Stata/MP version 11 (Stata, College Station, TX), and statistical significance was defined as a p value <0.05.
Results
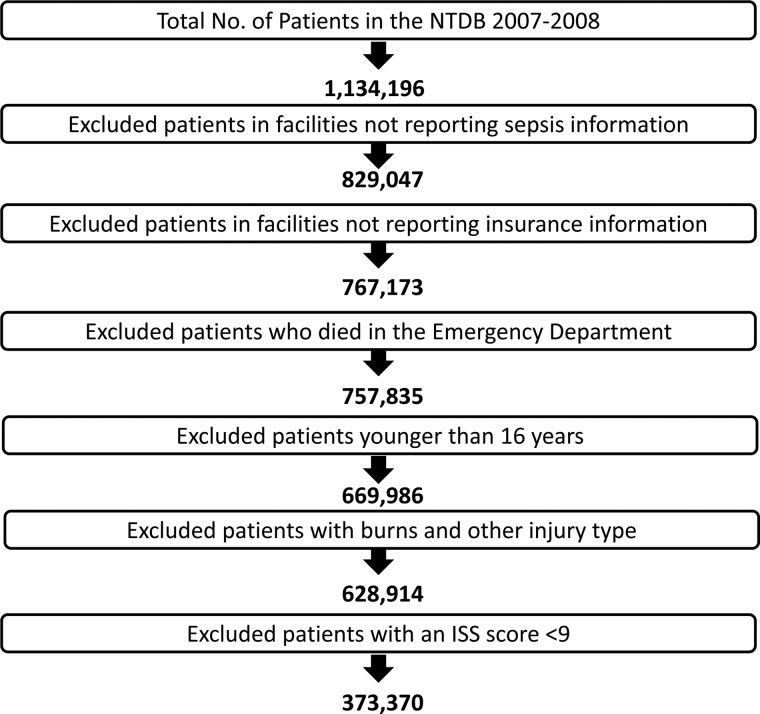
The NTDB included approximately 1.13 million patients. Of these, 767,173 were from facilities that reported sepsis and insurance information routinely. The study exclusion/inclusion criteria selected 373,370 patients. Complete data on all variables were available for 260,888 patients, and these were included in the final regression model. Figure 1 outlines our patient selection.
FIG. 1.
Patient selection outline.
Table 1 demonstrates the distribution of the socio-demographic and clinical characteristics of the study population. The median age was 47 years (interquartile range [IQR] 28–68 years). The majority of the patients were male and Caucasian. The median ISS score was 13 (IQR 9–19), the median duration of total hospital stay and ICU-free stay was 5 d (IQR 3–9 d) and 4 d (IQR 2–7 d), respectively.
Table 1.
Socio-Demographic and Clinical Characteristics of Patients (N=373,370)
| Number of patients (% of total) | |
|---|---|
| Age | |
| 16–25 | 77,861 (20.9) |
| 26–35 | 51,969 (13.9) |
| 36–45 | 50,349 (13.5) |
| 46–55 | 53,232 (14.3) |
| 56–65 | 39,635 (10.6) |
| 66–75 | 30,934 ( 8.3) |
| 76–85 | 41,793 (11.2) |
| >85 | 27,035 ( 7.2) |
| Missing | 562 ( 0.15) |
| Female/male | 127,612 (34.2)/237,639 (63.7) |
| Missing | 8,119 ( 2.2) |
| Race | |
| Caucasian | 242,593 (64.9) |
| African American | 47,499 (12.7) |
| Hispanic | 39,174 (10.5) |
| Other | 18,935 ( 5.1) |
| Missing | 25,169 ( 6.7) |
| Hypotensive on arrival in emergency department | |
| No | 344,428 (92.3) |
| Yes | 13,560 ( 3.6) |
| Missing | 15,382 ( 4.1) |
| Glasgow Coma Scale motor score | |
| 1–2 | 32,271 (8.7) |
| 3–4 | 7,360 (2.0) |
| 5–6 | 298,954 (80.1) |
| Missing | 34,785 (9.3) |
| Injury Severity Score | |
| 9–15 | 207,296 (55.5) |
| 16–24 | 86,511 (23.2) |
| 25–75 | 60,049 (16.1) |
| Missing | 19,514 ( 5.2) |
| Mechanism | |
| Fall | 136,422 (36.5) |
| Motor vehicle traffic | 97,927 (26.2) |
| Pedestrians struck | 14,573 ( 3.9) |
| Bicycle | 3,113 ( 0.8) |
| Motorcycle | 27,447 ( 7.4) |
| Other | 91,597 (24.5) |
| Missing | 2,291 ( 0.6) |
| Penetrating injury | |
| No | 335,345 (89.8) |
| Yes | 35,734 ( 9.6) |
| Missing | 2,291 ( 0.6) |
| Major surgical intervention | |
| No | 302,330 (81.0) |
| Yes | 71,040 (19.0) |
| Nervous system | 9,141 ( 6.4) |
| Intensive care unit admission | |
| No | 222,306 (59.5) |
| Yes | 149,718 (40.1) |
| Missing | 1,346 ( 0.4) |
| Need for ventilator | |
| No | 311,742 (83.5) |
| Yes | 59,968 (16.1) |
| Missing | 1,660 ( 0.4) |
| Insured | |
| No | 57,087 (15.3) |
| Yes | 260,786 (69.9) |
| Missing | 55,497 (14.9) |
| Trauma level | |
| I | 258,623 (69.3) |
| II | 92,143 (24.7) |
| III | 9,732 ( 2.6) |
| IV | 541 ( 0.1) |
| Missing | 12,331 ( 3.3) |
Missing=data not available.
Of the total of 373,370 patients, 5,276 (1.41%) developed sepsis. Among patients who developed sepsis, the mortality rate was 18.9%. A number of risk factors for the development of sepsis were identified by univariable analysis (Table 2). All measures for length of stay were significantly higher in patients with sepsis than in patients without sepsis. Similarly, a number of these risk factors were associated with death in patients with sepsis (Table 3).
Table 2.
Univariable Analysis: Associations of Sepsis in Moderately to Severely Injured Patients (N=373, 370)
| Patients without sepsis n=368,094 (98.6%) n (%) | Patients with sepsis n=5,276 (1.4%) n (%) | Total n=373,370 | p value | |
|---|---|---|---|---|
| Age | ||||
| 16–25a | 76,862 (98.72) | 999 (1.28) | 77,861 | |
| 26–35 | 51,168 (98.46) | 801 (1.54) | 51,969 | <0.001 |
| 36–45 | 49,588 (98.49) | 761 (1.51) | 50,349 | 0.001 |
| 46–55 | 52,355 (98.35) | 877 (1.65) | 53,232 | <0.001 |
| 56–65 | 38,935 (98.23) | 700 (1.77) | 39,635 | <0.001 |
| 66–75 | 30,431 (98.37) | 503 (1.63) | 30,934 | <0.001 |
| 76–85 | 41,351 (98.94) | 442 (1.06) | 41,793 | 0.001 |
| >85 | 26,847 (99.30) | 188 (0.70) | 27,035 | <0.001 |
| Male sex | ||||
| No | 126,340 (99.00) | 1,272 (1.00) | 127,612 | |
| Yes | 233,643 (98.32) | 3,996 (1.68) | 237,639 | <0.001 |
| Race | ||||
| Caucasiana | 239,395 (98.68) | 3,198 (1.32) | 242,593 | |
| African-American | 46,461 (97.81) | 1,038 (2.19) | 47,499 | <0.001 |
| Hispanic | 38,606 (98.55) | 568 (1.45) | 39,174 | 0.04 |
| Other | 18,674 (98.62) | 261 (1.38) | 18,935 | 0.49 |
| Hypotensive on arrival to ED | ||||
| No | 339,992 (98.71) | 4,436 (1.29) | 344,428 | |
| Yes | 12,871 (94.92) | 689 (5.08) | 13,560 | <0.001 |
| Glasgow Coma Scale motor score | ||||
| 1–2a | 30,753 (95.30) | 1,518 (4.70) | 32,271 | |
| 3–4 | 7,062 (95.95) | 298 (4.05) | 7,360 | 0.02 |
| 5–6 | 295,846 (98.96) | 3,108 (1.04) | 298,954 | <0.001 |
| Injury Severity Score | ||||
| 9–15 | 206,252 (99.50) | 1,044 (0.50) | 207,296 | |
| 16–24 | 85,159 (98.44) | 1,352 (1.56) | 86,511 | <0.001 |
| 25–75 | 57,352 (95.51) | 2,697 (4.90) | 60,049 | <0.001 |
| Mechanism of injury | ||||
| Falla | 135,347 (99.21) | 1,075 (0.79) | 136,422 | |
| Motor vehicle traffic | 95,957 (97.99) | 1,970 (2.01) | 97,927 | <0.001 |
| Pedestrian Struck | 14,218 (97.56) | 355 (2.44) | 14,573 | <0.001 |
| Bicycle | 3,072 (98.68) | 41 (1.32) | 3,113 | 0.001 |
| Motorcycle | 26,941 (98.16) | 506 (1.84) | 27,447 | <0.001 |
| Other | 90,288 (98.57) | 1,309 (1.43) | 91,597 | <0.001 |
| Penetrating injury | ||||
| No | 330,782 (98.64) | 4,436 (1.29) | 335,345 | |
| Yes | 12,871 (94.92) | 689 (5.08) | 35,734 | <0.001 |
| Major surgical intervention | ||||
| No | 299,047 (98.91) | 3,283 (1.09) | 302,330 | |
| Yes | 69,047 (97.19) | 1,993 (2.81) | 71,040 | <0.001 |
| Intensive care unit admission | ||||
| No | 221,859 (99.80) | 447 (0.20) | 222,306 | |
| Yes | 144,923 (96.80) | 4,795 (3.20) | 149,718 | <0.001 |
| Need for ventilator | ||||
| No | 310,495 (99.60) | 1,247 (0.40) | 311,742 | <0.001 |
| Yes | 55,985 (93.36) | 3,983 (6.64) | 59,968 | |
| Insured | ||||
| No | 56,186 (98.42) | 901 (1.58) | 57,087 | <0.001 |
| Yes | 257,169 (98.61) | 3,617 (1.39) | 260,786 | |
Reference group.
Table 3.
Univariable Analysis: Factors Associated with Death in Patients with Sepsis
| Alive n=4,183 (81.1%) n (%) | Died n=972 (18.9%) n (%) | Total n=5,155 | P value | |
|---|---|---|---|---|
| Age | ||||
| 16–25a | 877 (89.40) | 104 (10.60) | 981 | |
| 26–35 | 691 (89.16) | 84 (10.84) | 775 | 0.87 |
| 36–45 | 659 (88.34) | 87 (11.66) | 746 | 0.49 |
| 46–55 | 721 (83.55) | 142 (16.45) | 863 | <0.001 |
| 56–65 | 535 (77.65) | 154 (22.35) | 689 | <0.001 |
| 66–75 | 334 (68.40) | 155 (31.70) | 489 | <0.001 |
| 76–85 | 258 (60.14) | 171 (39.86) | 429 | <0.001 |
| >85 | 104 (58.43) | 74 (41.57) | 178 | <0.001 |
| Male sex | ||||
| No | 989 (80.21) | 244 (19.79) | 1,223 | |
| Yes | 3,189 (81.41) | 728 (18.59) | 3,917 | 0.35 |
| Race | ||||
| Caucasiana | 2,498 (80.17) | 618 (19.83) | 3,116 | |
| African American | 851 (83.84) | 164 (16.16) | 1,015 | 0.01 |
| Hispanic | 463 (82.53) | 98 (17.47) | 561 | 0.19 |
| Other | 208 (81.25) | 48 (18.75) | 256 | 0.68 |
| Hypotensive on arrival in emergency department | ||||
| No | 3,540 (81.72) | 792 (18.28) | 4,332 | |
| Yes | 533 (78.61) | 145 (21.39) | 678 | 0.05 |
| Glasgow Coma Scale motor score | ||||
| 1–2a | 1,212 (81.78) | 270 (18.22) | 1,482 | |
| 3–4 | 247 (85.17) | 43 (14.83) | 290 | 0.17 |
| 5–6 | 2,464 (81.11) | 574 (18.89) | 3,038 | 0.58 |
| Injury severity score | ||||
| 9–15a | 804 (80.24) | 198 (19.76) | 1,002 (100) | |
| 16–24 | 1,095 (82.93) | 228 (17.07) | 1,323 (100) | 0.12 |
| 25–75 | 2,140 (80.83) | 515 (19.17) | 2,655 (100) | 0.81 |
| Mechanism | ||||
| Falla | 728 (70.50) | 309 (29.50) | 1,037 | |
| Motor vehicle traffic | 1,592 (82.23) | 344 (17.77) | 1,936 | <0.001 |
| Pedestrian struck | 287 (70.37) | 57 (29.63) | 344 | <0.001 |
| Bicycle | 35 (85.37) | 6 (14.63) | 41 | 0.04 |
| Motorcycle | 446 (89.20) | 54 (10.80) | 500 | <0.001 |
| Other | 1,082 (84.66) | 196 (15.34) | 1,278 | <0.001 |
| Penetrating injury | ||||
| No | 3,578 (80.30) | 878 (19.70) | 4,456 | |
| Yes | 592 (87.06) | 88 (12.94) | 680 | <0.001 |
| Major surgical intervention | ||||
| No | 2,605 (81.13) | 606 (18.87) | 3,211 | |
| Yes | 1,578 (81.17) | 366 (18.83) | 1,944 | 0.97 |
| Intensive care unit admission | ||||
| No | 343 (82.65) | 72 (17.35) | 415 | |
| Yes | 3,821 (81.09) | 891 (18.91) | 4,712 | 0.44 |
| Need for ventilator | ||||
| No | 979 (81.92) | 216 (18.08) | 1,195 | |
| Yes | 3,178 (81.11) | 740 (18.89) | 3,918 | 0.53 |
| Insured | ||||
| No | 741 (84.11) | 140 (15.89) | 881 | |
| Yes | 2,821 (79.62) | 722 (20.38) | 3,543 | 0.003 |
Reference group.
After adjusting for patient, injury, and demographic factors, we found that older age, male sex, African American race, deranged physiology at admission, motor vehicle crash as the mechanism of injury, major surgical intervention, and ICU admission were independent predictors of post-traumatic sepsis (Table 4). In patients with sepsis, older age, higher ISS, lower GCS score, and fall as the mechanism of injury emerged as independent predictors of death.
Table 4.
Adjusted Odds Ratios (ORs)* with Confidence Intervals (CIs) for Predictors of Sepsis in Moderately to Severely Injured Patients Determined by Logistic Regression
| No. with sepsis n=260,888 | Deaths in patients with sepsis n=3,800 | |
|---|---|---|
| Age | ||
| 16–25 | 1 | 1 |
| 26–35 | 1.29 (1.15, 1.43) | 1.08 (0.78, 1.50) |
| 36–45 | 1.44 (1.28, 1.63) | 1.19 (0.85, 1.66) |
| 46–55 | 1.68 (1.54, 1.82) | 1.64 (1.24, 2.17) |
| 56–65 | 2.06 (1.82, 2.34) | 2.75 (2.08, 3.64) |
| 66–75 | 2.14 (1.83, 2.50) | 5.26 (3.87, 7.15) |
| 76–85 | 1.88 (1.58, 2.24) | 8.09 (5.67, 11.56) |
| >85 | 1.60 (1.23, 2.06) | 9.97 (6.09, 16.35) |
| Male sex | 1.36 (1.24, 1.49) | 1.10 (0.87, 1.40) |
| Race | ||
| Caucasian | 1 | 1 |
| African American | 1.60 (1.30, 1.96) | 1.18 (0.95, 1.48) |
| Hispanic | 0.95 (0.69, 1.29) | 1.41 (0.99, 2.00) |
| Other | 0.87 (0.68, 1.12) | 1.29 (0.85, 1.95) |
| Hypotensive on arrival in emergency department | 1.66 (1.50, 1.84) | 1.26 (0.98, 1.61) |
| Glasgow Coma Scale motor score | ||
| 1–2 | 1 | 1 |
| 3–4 | 1.01 (0.81, 1.24) | 0.68 (0.43, 1.07) |
| 5–6 | 0.67 (0.60, 0.76) | 0.74 (0.59, 0.93) |
| Injury Severity Score | ||
| 9–15 | 1 | 1 |
| 16–24 | 1.44 (1.26, 1.65) | 1.22 (0.84, 1.50) |
| 25–75 | 2.67 (2.24, 3.15) | 1.50 (1.14, 1.98) |
| Mechanism | ||
| Fall | 1 | 1 |
| Motor vehicle traffic | 1.88 (1.56, 2.27) | 0.72 (0.57, 0.91) |
| Other | 1.40 (1.24, 1.58) | 0.68 (0.56, 0.84) |
| Major surgical procedure | 1.71 (1.46, 2.00) | 0.98 (0.82, 1.16) |
| Penetrating injury | 1.09 (0.94, 1.26) | 0.98 (0.73, 1.31) |
| Intensive care unit admission | 10.75 (8.19, 14.11) | 1.74 (0.71, 4.30) |
| Uninsured | 1.08 (0.69, 1.70) | 1.24 (0.95, 1.64) |
Model was adjusted for year of presentation.
Data in boldface are statistically significant.
Sensitivity analysis using multiple imputations to account for the covariate data that was missing yielded results that were qualitatively similar to the non-imputed results. Only minor differences in ORs were noticed during multivariable analyses on both the imputed and non-imputed results.
Discussion
The incidence of sepsis among adult patients with moderate-to-severe injury who had complete data in the 2007–2008 National Trauma Data Bank is 1.4%. In this group of patients, sepsis appeared to be highly associated with death, as approximately 20% of patients with post-traumatic sepsis died during their index hospitalization. In the literature, the mortality rate in surgical patients with severe sepsis/septic shock is 35%–40% [5]. Older age, male gender, African-American race, physiologic derangement on admission, motor vehicle crash as the mechanism of injury, major surgical intervention, and ICU admission are significantly associated with post-traumatic sepsis. Similarly, older age, higher ISS score, and lower GCS score are significantly associated with death in patients with sepsis.
The incidence of sepsis in post-traumatic patients reported in literature is between 2% and 10% [6,7]. Moore et al. evaluated sepsis in general surgical patients and reported a rate of approximately 5% with an associated mortality rate of 18% [5]. Osborn et al. included approximately 30,000 trauma patients and estimated that 2% of the patients develop sepsis, with an associated mortality rate of 23% [6]. The findings of the present study are similar to these rates described previously of sepsis and associated mortality rate in general surgical and post-traumatic populations.
Older age is known to be associated with sepsis in non-trauma patients [2,3]. This study found the same to be true, and increasing age was noted to be a significant predictor of post-traumatic sepsis. A possible explanation for this finding may be differences in the distribution of co-morbidities across patient age groups. Also, increasing age decreases physiologic reserve, thus altering the ability of the injured patient to mount an inflammatory response [19]. However, as co-morbidities are not well recorded in the NTDB, they could not be adjusted for as a possible confounder. A significant sex disparity also was observed in this study, with men at higher risk of sepsis than women. This finding is in line with multiple previous studies confirming that men have worse outcomes and increased complications after traumatic injury [20–23].
African-American patients were more likely to develop post-traumatic sepsis in this analysis. To the best of our knowledge, racial/ethnic disparities have not been explored extensively in this context. A recent study investigating various characteristics associated with sepsis in general surgery patients did not report any association between sepsis and ethnicity [5], although there was a much smaller number of patients in that study (n=231). The reasons for the association of ethnicity with post-traumatic sepsis cannot be elucidated from this analysis, but future research, including the potential impact of race-related genetics, in this area is warranted.
Injury Severity Score is used as a proxy measure of the magnitude of the initial trauma load and is a known predictor of infection and sepsis [24,25]. The ISS was higher in patients who developed post-traumatic sepsis in the German Trauma Registry (mean ISS 33 vs. 25 points in non-septic patients) [7]. We observed similar findings. In addition, we found that patients who were hypotensive and had lower GCS scores at presentation were more likely to develop sepsis. These findings support the role of physiologic derangements at presentation in predisposition to post-traumatic sepsis.
Patients with motor vehicle crash as a mechanism of injury were more likely to develop post-traumatic sepsis in this study. In a study of trauma patients involved in a motor vehicle crashes, Previdi et al. found that 4.1% developed sepsis, whereas this study including patients with multiple mechanisms of injury found that only 1.4% developed sepsis [26]. Significant early predictors of sepsis after a motor vehicle crash were receiving a blood transfusion, suffering seven or more injuries, having a Glasgow Coma Scale score<10 and hypertension, co-morbidities, and certain kinds of injury, such as head trauma or internal injury of the chest or abdomen [26].
Early recognition of sepsis is sometimes challenging due to its non-specific signs and symptoms that also are also present in injured patients. Knowledge of patient and injury-specific characteristics that may help in identifying patients at risk for sepsis therefore may be valuable. We identified six risk factors associated with the development of sepsis in post-traumatic patients: Age older than 55 years, male gender, African-American race, physiologic derangements at presentation, ISS >15, and motor vehicle crash as the mechanism of injury. In addition, older age and higher ISS increase the likelihood of death in patients with sepsis.
The development of in-hospital sepsis is considered a measure of quality of care, and pressures to prevent this complication are increasing. The findings of this study suggest the need for greater vigilance in patients with risk factors described above and a suspicion of sepsis. These risk factors might also be incorporated into clinical risk prediction models for sepsis that could, in turn, be used for screening or treatment decisions.
This study has several limitations. The NTDB is a retrospective dataset, and underreporting of complications is known to be common. We reduced the potential impact of this limitation by limiting our analysis to the 2007 and 2008 datasets that were collected using the National Trauma Data Standard (NTDS), which has significantly improved the reliability and fidelity of the data, and by including patients from facilities that reported at least one patient with sepsis. A similar strategy has been successful in previously published work to address the potential for differential reporting of complications across centers [27]. Further, the NTDB does not collect data on when, in the course of the hospitalization, a patient developed sepsis. Finally, even after adjusting for multiple patient and injury covariates, information regarding co-morbidities was unavailable and so could not be considered. Despite these limitations, with a sample size of more than 350,000 patients, this is a robust dataset to evaluate predictors of sepsis in trauma patients.
In summary, we have identified several important patient- and injury-specific factors associated with post-traumatic sepsis. These factors can help identify trauma patients at risk of sepsis and target preventive interventions. In addition, differential predisposition to sepsis across these groups suggests further work is needed in understanding the connection between these variables and the pathophysiology of sepsis.
Acknowledgments
Financial support for this work was provided by the National Institutes of Health/National Institute of General Medical Sciences K23GM093112-01 and an American College of Surgeons C. James Carrico Fellowship for the study of Trauma and Critical Care (to AHH and MK). The authors have no financial conflicts of interest in relation to this manuscript.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Anderson RN. Smith BL. Deaths: Leading causes for 2001. Natl Vital Stat Rep. 2003;52:1–85. [PubMed] [Google Scholar]
- 2.Sands KE. Bates DW. Lanken PN, et al. Epidemiology of sepsis syndrome in 8 academic medical centers. JAMA. 1997;278:234–240. [PubMed] [Google Scholar]
- 3.Angus DC. Linde-Zwirble WT. Lidicker J, et al. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Vogel TR. Dombrovskiy VY. Carson JL, et al. Postoperative sepsis in the United States. Ann Surg. 2010;252:1065–1071. doi: 10.1097/SLA.0b013e3181dcf36e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore LJ. McKinley BA. Turner KL, et al. The epidemiology of sepsis in general surgery patients. J Trauma. 2011;70:672–680. doi: 10.1097/TA.0b013e31820e7803. [DOI] [PubMed] [Google Scholar]
- 6.Osborn TM. Tracy JK. Dunne JR, et al. Epidemiology of sepsis in patients with traumatic injury. Crit Care Med. 2004;32:2234–2340. doi: 10.1097/01.ccm.0000145586.23276.0f. [DOI] [PubMed] [Google Scholar]
- 7.Wafaisade A. Lefering R. Bouillon B, et al. Epidemiology and risk factors of sepsis after multiple trauma: An analysis of 29,829 patients from the Trauma Registry of the German Trauma Society. Crit Care Med. 2011;39:621–628. doi: 10.1097/CCM.0b013e318206d3df. [DOI] [PubMed] [Google Scholar]
- 8.Ingraham AM. Xiong W. Hemmila MR, et al. The attributable mortality and length of stay of trauma-related complications: A matched cohort study. Ann Surg. 2010;252:358–362. doi: 10.1097/SLA.0b013e3181e623bf. [DOI] [PubMed] [Google Scholar]
- 9.Bone RC. Balk RA. Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine, 1992. Chest. 2009;136(5 Suppl):e28. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 10.Martin GS. Mannino DM. Eaton S, et al. The epidermiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 11.National Trauma Data Standard Dictionary 2011 Admissions. http://www.ntdsdictionary.org/data Elements/documents/NTDS2011_Final3.pdf http://www.ntdsdictionary.org/data Elements/documents/NTDS2011_Final3.pdf
- 12.Oyetunji T. Crompton JG. Efron DT, et al. Simplifying physiologic injury severity measurement for predicting trauma outcomes. J Surg Res. 2011;159:627–632. doi: 10.1016/j.jss.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 13.Haider AH. Chang DC. Haut ER, et al. Mechanism of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009;153:138–142. doi: 10.1016/j.jss.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 14.Haider AH. Efron DT. Haut ER, et al. Black children experience worse clinical and functional outcomes after traumatic brain injury: An analysis of the National Pediatric Trauma Registry. J Trauma. 2007;62:1259–1262. doi: 10.1097/TA.0b013e31803c760e. [DOI] [PubMed] [Google Scholar]
- 15.Haider AH. Chang DC. Efron DT, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 16.Crandall M. Sharp D. Brasel K, et al. Lower extremity vascular injuries: Increased mortality for minorities and the uninsured? Surgery. 2011;150:656–664. doi: 10.1016/j.surg.2011.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roudsari B. Field C. Caetano R. Clustered and missing data in the US National Trauma Data Bank: Implications for analysis. Inj Prev. 2008;14:96–100. doi: 10.1136/ip.2007.017129. [DOI] [PubMed] [Google Scholar]
- 18.Oyetunji TA. Crompton JG. Ehanire ID, et al. Multiple imputation in trauma disparity research. J Surg Res. 2011;165:e37–e41. doi: 10.1016/j.jss.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 19.Valente SA. Fallon WF., Jr Alexander TS, et al. Immunologic function in the elderly after injury: The neutrophil and innate immunity. J Trauma. 2009;67:968–974. doi: 10.1097/TA.0b013e3181b84279. [DOI] [PubMed] [Google Scholar]
- 20.Haider AH. Crompton JG. Chang DC, et al. Evidence of hormonal basis for improved survival among females with trauma-associated shock: An analysis of the National Trauma Data Bank. J Trauma. 2010;69:537–540. doi: 10.1097/TA.0b013e3181efc67b. [DOI] [PubMed] [Google Scholar]
- 21.Hubacek JA. Stuber F. Frohlich D, et al. Gene variants of the bactericidal/permeability increasing protein and lipopolysaccharide binding protein in sepsis patients: Gender-specific genetic predisposition to sepsis. Crit Care Med. 2001;29:557–561. doi: 10.1097/00003246-200103000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Knoferl MW. Angele MK. Diodato MD, et al. Female sex hormones regulate macrophage function after trauma-hemorrhage and prevent increased death rate from subsequent sepsis. Ann Surg. 2002;235:105–112. doi: 10.1097/00000658-200201000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kisat M. Zafar SN. Latif A, et al. Predictors of positive head CT scan and neurosurgical procedures after minor head trauma. J Surg Res. 2012;173:31–37. doi: 10.1016/j.jss.2011.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Croce MA. Fabian TC. Waddle-Smith L. Maxwell RA. Identification of early predictors for post-traumatic pneumonia. Am Surg. 2001;67:105–110. [PubMed] [Google Scholar]
- 25.Papia G. McLellan BA. El-Helou P, et al. Infection in hospitalized trauma patients: Incidence, risk factors, and complications. J Trauma. 1999;47:923–927. doi: 10.1097/00005373-199911000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Previdi JK. Cayten CG. Byrne DW. Early predictors of sepsis in the motor-vehicle crash trauma victim. Prehosp Disaster Med. 1996;11:27–36. doi: 10.1017/s1049023x0004231x. [DOI] [PubMed] [Google Scholar]
- 27.Huseynova K. Xiong W. Ray JG, et al. Venous thromboembolism as a marker of quality of care in trauma. J Am Coll Surg. 2009;208:547–552. doi: 10.1016/j.jamcollsurg.2009.01.002. [DOI] [PubMed] [Google Scholar]