Abstract
In the present historical review, we highlight several articles outlining contributions of the Framingham Heart Study over the span of nearly seven decades to our understanding of the epidemiology of blood pressure (BP), atrial fibrillation and genetic factors as they relate to cerebrovascular disease. In 1970, Framingham investigators led by William Kannel, explored the epidemiological relations of BP and its various components to risk of ischemic stroke as well as hemorrhage, and noted the greater impact of hypertension to risk of stroke compared to other cardiovascular outcomes. Framingham investigators changed the prevalent concepts in terms of the contribution of BP components to stroke risk; i.e. they showed systolic pressure to be no less important a component for stroke risk than the diastolic or mean arterial pressures. In addition, they challenged the notion that hypertension was a normal consequence of increasing age, as connoted by the term “essential” hypertension. They also refuted the idea that blood pressure elevation in the elderly is innocuous by demonstrating that increased stroke risk persisted in advanced age in hypertensive persons. Thirty years later, the Framingham Study attained long term follow up of an entire generation of participants with excellent retention to follow-up, thus providing an opportunity to study hypertension and risk of stroke in a general population sample. Framingham investigators examined the impact of various BP components over a 50-year follow-up in normotensive and untreated hypertensive individuals as regards stroke risk, and showed the long term importance of antecedent (midlife) hypertension in future stroke risk . Similarly by calling attention to the importance of chronic non-valvular atrial fibrillation as a contributor to stroke, particularly in the elderly, FHS investigators confirmed the clinical observations of the founder of stroke neurology, C. Miller Fisher, M.D., who had made the clinical and pathological association of AF to stroke. Lastly, in the dawn of the era of individualized preventive medicine, FHS is participating in the effort to further our understanding of the role of genetic factors to stroke incidence.
The contributions of the Framingham Heart Study have been many and have shaped our understanding of the relation of BP, AF and other risk factors to stroke risk, thereby setting the stage for clinical trials which demonstrated how control of these risk contributors could prevent stroke and enable stroke prevention. FHS investigators are collaborating with other geneticists and epidemiologists internationally to elucidate the role of genetic factors and stroke susceptibility, which is likely continue to shape the practice of preventive cardiovascular medicine.
Introduction
The role of elevated blood pressure (BP) in causing cerebrovascular disease was first recognized in the 1920s. Keith and colleagues recognized symptoms arising from organic lesions of the central nervous system in 29 of 81 patients in their description of the syndrome of malignant hypertension.1 Nonetheless, the relation of hypertension and cerebrovascular disease, particularly ischemic stroke, remained unclear for nearly 50 years. The label “benign hypertension” was used to describe hypertensive individuals and in the elderly even marked BP elevations were not considered pathological.2 Subsequently, it was not until the availability of antihypertensive medications in the mid to late 1960’s, was treatment of extreme levels of diastolic hypertension undertaken by Fries who demonstrated their effectiveness in reducing cardiovascular disease particularly stroke.3 Thus began the series of clinical trials of patients with lower and lower diastolic BP levels uniformly demonstrating the efficacy of blood pressure reduction in stroke prevention. Based on epidemiological data provided by the FHS, the National High Blood Pressure Education Program was started in 1972 with the goal of educating health care professionals and the public on the adverse impact of hypertension.4 The contribution of individual components of blood pressure was first elucidated by Dr Kannel and colleagues in 1970 in their “Landmark JAMA publication” which was recognized in the first Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure in 1977, which used BP risk stratification cut points defined by the FHS.5 Contributions of the FHS undoubtedly influenced the understanding of the role of individual components of BP as they relate to stroke. The scientific community eventually embraced these concepts leading to evaluation and identification of effective therapies for individuals with much lower BP values, less focus on the DBP than the SBP, and in hypertensive elderly (above age 80 years) than previously even considered.
The Framingham Study provided an exemplary model for the conduct of epidemiological studies, achieving the challenging task of close and comprehensive serial follow-up of three generations of participants, with remarkable participant retention at follow up. The study began in 1948 with the enrollment of the Original Cohort, following participants prospectively over more than 5 decades. This has allowed for a more accurate understanding of the natural history of participants with and without hypertension, in terms of their risk of cerebrovascular disease, clinically evident in the form of overt stroke, and in subclinical stages. Since antihypertensive medication was not utilized in clinical practice until the early 1970s, FHS investigators were able to observe the impact of untreated blood pressure levels, including elevated levels, on a number of outcomes including aspects of cognitive impairment.6
An additional important contribution by investigators of the Framingham study as it relates to stroke prevention is the identification of non-valvular atrial fibrillation as a strong predictor of risk of stroke. Follow up for an extended period allowed for the evaluation of risk in persons at a wide age range, showing the strong and relative contributions of AF to stroke risk, particularly in the elderly.
More recently, the FHS has contributed significantly to elucidation of the role of genetic factors in stroke risk. The careful ascertainment of stroke occurrence in the Original and Offspring cohorts of the FHS permitted clarification of the contribution of parental history of stroke, to stroke risk in the offspring, and provided evidence that genetic factors contribute substantially to stroke susceptibility. Advances in genetic methods have been incorporated in the FHS, allowing for the performance of genome wide association studies (GWAS) where single nucleotide polymorphisms (SNPs) distributed across the entire human genome can be assessed, without assuming a priori hypothesis. FHS investigators directed a collaborative effort to identify previously unknown genes variations in common forms of stroke, leading to the identification of novel genes implied in stroke risk.
In the present historical review, we highlight several selected FHS publications over the course of nearly seven decades, to our understanding of the role of BP in general, its individual components in particular (systolic, diastolic and pulse pressures), and AF as regards cerebrovascular disease (More comprehensive treatment of this subject can be found elsewhere).7,8 We also describe a unique contribution provided by the FHS, emphasizing the importance of antecedent blood pressure measurements to stroke risk prediction compared with use of current BP measurements, and FHS contributions to the understanding of the role of genetic factors in stroke risk.
Blood Pressure and its Relation to Cerebrovascular Disease
In 1970, Drs Kannel, Wolf and colleagues,9 reiterated hypertension as “the most common and potent precursor of atherothrombotic brain infarction (ABI)”, and further suggested that “the key to the prevention of CVAs would therefore, appear to be early detection and control of hypertension”. Forty two years later these statements remain true. In this report, Kannel et al. describe the relationship of BP and its components to stroke in 5,209 Original cohort participants followed biennially over 14years for the occurrence of stroke in general and ischemic stroke attributable to atherosclerotic brain infarction (ABI), i.e., brain infarction in the absence of an obvious cardiac source of emboli, in particular. A casual blood pressure, representing the mean of 2 measurements recorded by a physician was taken as the BP at the examination rather than the basal or resting pressure, which was the measure recommended at the time. Hypertension was arbitrarily defined as BP greater or equal to 160/95 mmHg, normotension as BP less than 140/90 mm Hg and borderline BP for measures within this range and stroke was defined according to conventional clinical criteria. The method of surveillance for occurrence of stroke included a brief neurological exam during the biennial examination, confirmation of cases by a neurologist in consultation, examination of study participants admitted with a presumptive or confirmed diagnosis of stroke to the only local hospital in Framingham (since 1965); surviving participants were followed regularly after the stroke and in cases of death, all pertinent information concerning circumstances of death was reviewed to determine if stroke was the cause of death. Further information was gathered by interview of participants regarding the occurrence of stroke in their spouse. The investigators tested the accuracy of their stroke detection methods in a random subset of 263 participants who underwent detailed neurological evaluation at the time of their biennial examination, and found that no additional cases of stroke were uncovered.
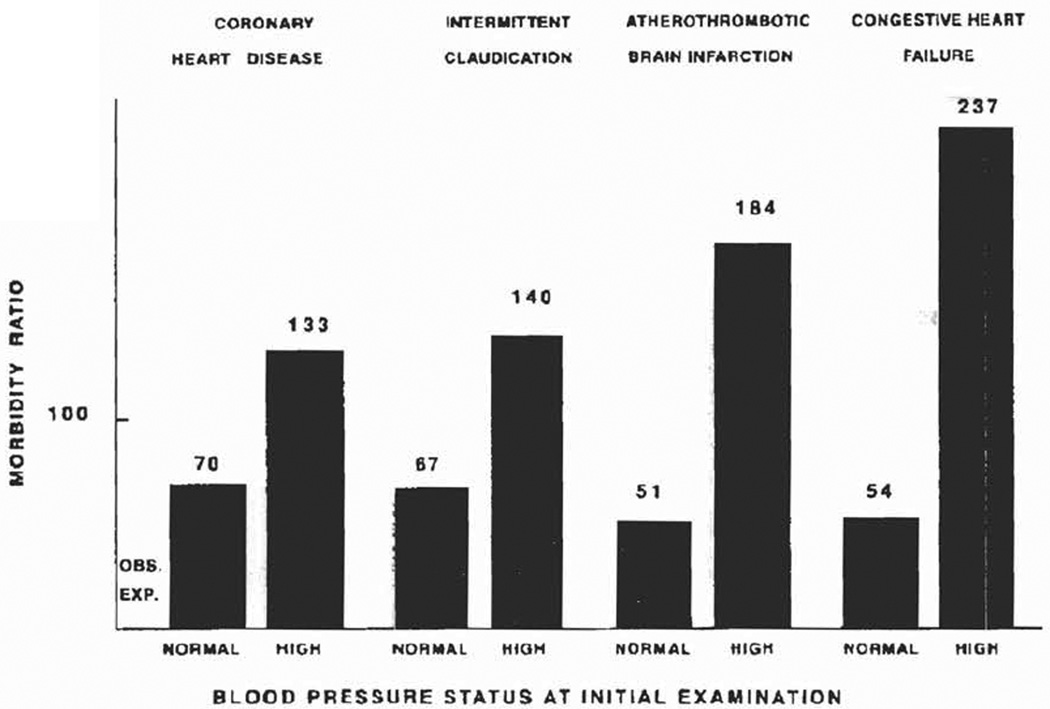
Retention of participants at follow up was impressive with less than 2% lost to follow up in 14years. During this period, 135 participants developed strokes (65 men, 70 women), with 86 considered ABI (39 men, 47 women). ABI incidence increased with age in both men and women, with women reflecting increased incidence in the older age groups and male predominance at younger ages (figure 1). Another important observation in this study is the finding that the incidence of stroke in hypertensive individuals (with the BP cut points defined above), compared to normotensive participants was much higher compared to coronary heart disease (Figure 2). FHS investigators also noted sex differences in stroke rates compared to coronary artery disease and peripheral arterial disease, where there is a male predominance and a closing gap between sexes with advancing age. Women had similar rates of CAD and ABI, whereas men had greater incidence of CAD than ABI. Risk of stroke was distinctly related to BP status at initial examination. Contrary to prevailing notion, the relative risk of intracranial hemorrhage (intra -cerebral or subarachnoid hemorrhage) and ABI was not different in relation to blood pressure level.
Figure 1.
(Source Kannel WB, Wolf PA, Verter J, McNamara PM. Epidemiologic assessment of the role of blood pressure in stroke. The Framingham study. JAMA : the journal of the American Medical Association. Oct 12 1970;214(2):301–310, figure 1, page 1271).
Prevalence of hypertension and incidence of atherotrombotic brain infarction by age and sex. Men and women aged 30 to 62 years at entry.
Figure 2.
(Source Kannel WB, Wolf PA, Verter J, McNamara PM. Epidemiologic assessment of the role of blood pressure in stroke. The Framingham study. JAMA : the journal of the American Medical Association. Oct 12 1970;214(2):301–310, figure 2, page 1271).
Risk of cardiovascular disease (14 years) according to blood pressure status. Men aged 30 to 62 years at entry.
Role of systolic, diastolic and mean arterial pressure in occurrence of ABI
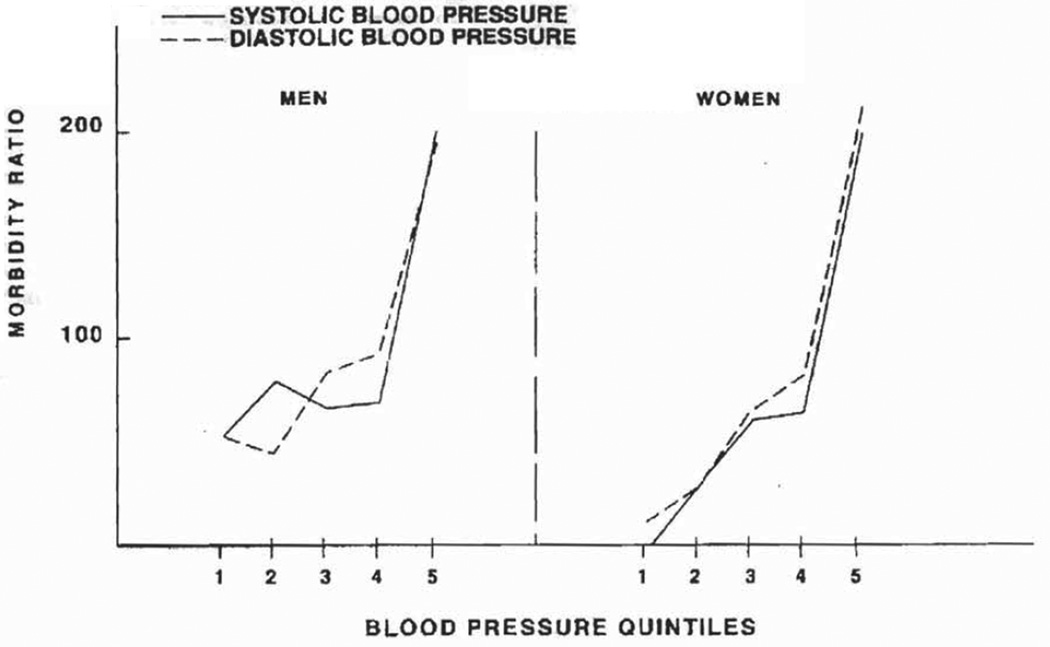
The authors examined the relation of each BP component to ABI, observing that the gradient of ABI risk was similar according to SBP first and then DBP. Age-adjusted analysis in the entire population sample disclosed several crucial observations: 1) No critical level of BP is evident, the risk “being simply proportional to the level from the lowest to the highest recorded”, and 2) “gradients for SBP and DBP are quite similar with nothing to suggest a closer relation to DBP” (figure 3). In addition, blood pressure, SBP or DBP, was a more powerful discriminator of risk of stroke than any of the other major cardiovascular consequences except for congestive heart failure. In fact, the risk estimates were nearly twice as high for stroke compared to coronary heart disease, especially for men (Table 1). In this report, FHS investigators also studied the role of mean arterial pressure (MAP), showing that MAP discriminated cases no better than SBP alone, but it was better than DBP. In women, MAP seemed to discriminate as well as SBP. Kannel and colleagues reached an important conclusion that again challenged prevalent notions at the time, “this gives no indication that SBP plays a minor role in ABI”. They reasoned that MAP predicts no better than SBP alone, likely deriving from the fact that both are highly correlated and SBP is more accurately measured than DBP. A third observation opposing prevalent notions at the time was that “there was no tendency of the impact of SBP to decrease with age in either sex”, thus, disproving the notion that elevated BP in the elderly is innocuous.
Figure 3.
(Source Kannel WB, Wolf PA, Verter J, McNamara PM. Epidemiologic assessment of the role of blood pressure in stroke. The Framingham study. JAMA : the journal of the American Medical Association. Oct 12 1970;214(2):301–310, figure 4, page 1273).
Risk of ABI (14 years) according to systolic and diastolic blood pressure. Men and women aged 30 to 62 years at entry.
Table 1.
(Source Kannel WB, Wolf PA, Verter J, McNamara PM. Epidemiologic assessment of the role of blood pressure in stroke. The Framingham study. JAMA : the journal of the American Medical Association. Oct 12 1970;214(2):301–310, Table 3, page 1272).
Average of Standardized Mean Deviations of Systolic Blood pressure in Men and Women 38 to 69 years of age developing disease vs. those remaining free of disease.
| Coronary Heart Disease Mean Deviation |
Intermittent Claudication Mean Deviation |
Cardiovascular Accident Mean Deviation |
Congestive Heart Failure Mean Deviation |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Systolic | Diastolic | No. | Systolic | Diastolic | No. | Systolic | Diastolic | No. | Systolic | Diastolic | |
| Men | (252) | 0.41 | 0.28 | (58) | 0.60 | 0.15 | (53) | 0.83 | 0.61 | (44) | 0.92 | 0.62 |
| Women | (135) | 0.68 | 0.39 | (30) | 0.23 | 0.03 | (53) | 0.81 | 0.70 | (30) | 0.93 | 0.65 |
.
This table summarizes the age specific mean deviations. The differences between disease categories is not accounted for by differences in age distribution. Mean deviations were not found to vary appreciably with age.
When comparing SBP and DBP as stroke risk predictors combined versus either component alone, the discriminatory analysis showed that when used together, both achieved little more than SBP alone, DBP discriminated no better than SBP, and there was no decrement with age. Furthermore, the authors discussed the role of confounding factors on the relation of interest, thus pioneering underlying concepts in multivariable analysis. The report studied the role of obesity, diabetes and gout in the observations noted previously. Excluding individuals with these conditions, the investigators observed that there was a distinct residual gradient of risk proportional to the BP level. Similarly, in subjects without left ventricular hypertrophy or congestive heart failure, risk of ABI was distinctly related to BP alone. Lipid levels were also studied, finding that little was added to the risk of ABI by lipid level (cholesterol and triglycerides), though they acknowledged that subgroup analysis was limited by small numbers.
The conclusions of this study changed existent conceptions of the relation of BP and cerebrovascular disease at the time, and provided the foundations for preventive interventions in clinical practice: “though treatment thresholds are arbitrary, this was first step to guide clinicians in decisions to treat patients in order to reduce risk of stroke”. Although not directly evaluated in this report, on the basis of the strength of the relation of BP and stroke, the authors correctly estimated that even labile BP (as opposed to fixed) is likely to play a role. They provided convincing evidence contrasting the existing notion that DBP the cerebrovascular consequences of BP derive from the DBP component. This analysis showed that both components were not better predictors than SBP alone. The notion that SBP represented aortic rigidity and a natural, innocuous consequence of aging was dispelled. The authors provided further insight into the hypothesis concerning the mechanism by which hypertension affects the occurrence of stroke, including mechanical damage of vessels and impairment of cardiac function, suggested by the stronger relation of hypertension to stroke than other cardiovascular outcomes. Lastly, acknowledging the results of one of the first clinical trials showing benefits of blood pressure lowering on stroke risk reduction,3 Dr Kannel and colleagues made a statement that would only be truly understood decades later: “asymptomatic mild hypertension is far from innocuous even in the elderly and treatment should begin early”.
Interim Recognition of the FHS contribution
In 1996 a perspective article in JAMA called attention to the relevance of the 1970 FHS publication.10 The editorial highlighted several important observations made in the study, which emphasizes a crucial function of the FHS over time, providing clinicians in the medical community with a practical contribution for the care of patients on a daily basis. This article highlights some of such contributions: 1) Classification of individuals on the basis of BP recordings made during a routine clinical examination making possible for clinicians to extrapolate this practice to medical care; 2) Provision of one of the earliest classification systems for stroke etiology using available knowledge and techniques; and 3) Elucidation of the contribution of individual components of BP to stroke risk. Again noting the fact that while at the time it was believed that DBP played a more important role in causing hypertensive organ damage, the authors demonstrated rather clearly that this was not the case for stroke, where SBP was more strongly related than DBP.
The author noted a number of the predictions of FHS investigators which had stood the test of time, with multiple subsequent studies showing the same results, for instance by the Seven Countries Study. Dr. Kannel and colleagues correctly implied that the treatment of hypertension would reduce stroke incidence, which has been proved through multiple randomized clinical trials, and is now a most essential component of all practice guidelines for stroke prevention. No threshold effects were discerned, as stroke risk increases steeply with BP over the whole range of BP. Current practice guidelines by the American Heart Association for secondary prevention of stroke implicitly integrate this concept when recommending that “an absolute target BP level and reduction are uncertain and should be individualized, but benefit has been associated with an average reduction of approximately 10/5 mm Hg, and normal BP levels have been defined as <120/80 mm Hg by JNC 7”.11
Antecedent (midlife) hypertension and risk of stroke
The prospective, long term and meticulous follow up of FHS participants over decades has provided FHS investigators with the opportunity to relate of past BP measurements in the prediction of future stroke, after accounting for the influence of current BP measures, and in currently normotensive individuals.12 Follow up for an extended period of time with such high retention of participants and comprehensive assessments attests to the reliability of the results of this report. In this article, the study spanned a period of 50 years, including 5197 Original cohort participants free of prevalent stroke at the index examination. The role of each component of blood pressure, systolic, diastolic and pulse pressure was assessed to evaluate for differential contribution of past BP measures to future risk of ischemic stroke. The authors considered three aspects of BP: 1) current BP at time of prediction, which occurred at a baseline age of 60, 70 or 80years; 2) recent past BP in the decade preceding risk prediction; and, 3) remote past BP, 10 to 20 years before risk prediction. Ascertainment of ischemic stroke now included brain imaging with MRI of CT performed in 85% of all strokes, and used autopsy data when available. Stroke was classified as ABI in the absence of a cardiac source of emboli, and included three etiological groups: large artery infarct, lacunar infarcts and infarcts of unknown origin. The analysis evaluated the effect of 1 SD change in current BP (SBP, DBP or PP) on the 10yr stroke risk in 60, 70 and 80 year old participants without adjusting for past BP measurements. Subsequent analysis was additionally adjusted for current BP, and the incremental prognostic utility of remote BP was assessed similarly. In order to minimize effects of regression dilution bias, given that the authors used multiple measurements of antecedent BP (2–5 BP readings depending on the number of available examinations during the decade of interest), they randomly repeated the analysis using BP recorded at single random examinations within the decade of interest to represent antecedent BP. Additional secondary analysis included stratified analysis according to current BP status (hypertensive versus non-hypertensive), by treatment status (yes versus no) and by year when baseline age was reached (pre or post-1975).
The study included 3,761 subjects reaching the age of 60 years free of stroke with information available for analysis, 3049 subjects reaching age of 70 years and 1203 reaching age 80 years. The mean SBP and PP increased with age and mean DBP decreased with age, which is a finding reflecting one of the contributions of the FHS to the understanding of the changes in BP with age, and the underlying pathophysiology of hypertension. The proportion of subjects taking antihypertensive medications increased with age, and was over 40% in participants aged 80 years at baseline exam, also indirectly reflecting the influence of the FHS on medical practice. In prior decades persons in this age group would not have been considered for antihypertensive therapy. There were 830 completed strokes during the 50year period in 5197 participants. 740 of the strokes occurred between age 60 and 89 years, 521 occurred in subjects who attended within 1 year of biennial exam and could give reliable information for current BP at baseline. Regarding current BP measurements, participants with higher levels of BP at the time of risk prediction showed an increased 10yr risk of stroke for all BP components, SBP, DBP, and PP. The effect was strongest at age of 60 years and weakest at the age of 80years. In the 80 year old group, the risk was greater for SBP and PP than for DBP.
In analysis adjusted for current BP, antecedent BP demonstrated a further increase in the 10yr risk of stroke (Table 2). The effect was significant and ranged between 68 to 92% increase at age 60, 14 to 72% increase risk at age 70years and up to 32% at age 80years. Similar effects were noted as regards remote antecedent BP. The authors noted that the relationships observed varied with age and sex. The effect of current and antecedent BP was most powerful at age 60years, with risk estimates being lower at age 70 and 80years. In 70yo men SBP and PP were more informative than DBP. Recent or current DBP was not significant in men aged 70years, but remote DBP remained significantly predictive. In the specified secondary analyses, the relations of antecedent BP and risk of stroke persisted even when a single random BP measure was used, though the effect size decreased. There was no significant effect modification in stratified analysis by sex or antihypertensive medication use, although the subgroup analysis had lower statistical power due to small numbers in the subgroups. The effect of recent antecedent BP remained significant in stratified analysis by time period pre or post-1975.
Table 2.
(Source Seshadri S, Wolf PA, Beiser A, et al. Elevated midlife blood pressure increases stroke risk in elderly persons: the Framingham Study. Archives of internal medicine. Oct 22 2001;161(19):2343–2350, Table 2, page 2347).
Regression of ischemic stroke incidence on current and antecedent blood pressure measurements, by blood pressure component.
| Women |
Men |
|||||
|---|---|---|---|---|---|---|
| Blood Pressure Measurement | Systolic Blood Pressure |
Diastolic Blood Pressure |
Pulse Pressure |
Systolic Blood Pressure |
Diastolic Blood Pressure |
Pulse Pressure |
| Baseline Age of 60 y | ||||||
| 71 Ischemic strokes in 2197 subjects | 71 Ischemic strokes in 1564 subjects | |||||
| Current: age, 60 y | 2.03 (1.69–2.44) | 1.85 (1.56–2.21) | 1.78 (1.48–2.15) | 1.39 (1.12–1.72) | 1.42 (1.15–1.74) | 1.23 (0.98–1.53) |
| Recent past: mean age, 50–59 y† | 1.68 (1.25–2.25) | 1.78 (1.33–2.38) | 1.80 (1.34–2.42) | 1.92 (1.39–2.66) | 1.73 (1.26–2.38) | 1.82 (1.14–2.58) |
| Remote past: mean age, 40–49 y† | 1.48 (1.07–2.07) | 1.57 (1.13–2.17) | 1.60 (1.08–2.36) | 1.54 (0.96–2.45) | 1.30 (0.88–1.91) | 1.50 (0.88–2.56) |
| Baseline Age of 70 y | ||||||
| 130 Ischemic strokes in 1875 subjects | 101 Ischemic strokes in 1174 subjects | |||||
| Current: age, 70 y | 1.67 (1.44–1.94) | 1.49 (1.27–1.75) | 1.53 (1.31–1.78) | 1.53 (1.28–1.83) | 1.08 (0.89–1.31) | 1.66 (1.39–1.99) |
| Recent past: mean age, 60–69 y† | 1.66 (1.28–2.14) | 1.44 (1.11–1.88) | 1.72 (1.31–2.27) | 1.30 (0.97–1.75) | 1.14 (0.84–1.54) | 1.37 (0.99–1.90) |
| Remote past: mean age, 50–59 y† | 1.41 (1.17–1.69) | 1.47 (1.23–1.75) | 1.52 (1.20–1.93) | 1.45 (1.14–1.86) | 1.42 (1.13–1.80) | 1.51 (1.10–2.08) |
| Baseline Age of 80 y | ||||||
| 81 Ischemic strokes in 791 subjects | 37 Ischemic strokes in 412 subjects | |||||
| Current: age, 80 y | 1.40 (1.13–1.73) | 1.14 (0.91–1.43) | 1.37 (1.10–1.69) | 1.25 (0.92–1.71) | 0.99 (0.71–1.38) | 1.30 (0.95–1.77) |
| Recent past: mean age, 70–79 y† | 1.19 (0.84–1.70) | 1.21 (0.86–1.70) | 1.12 (0.75–1.67) | 1.25 (0.76–2.04) | 1.32 (0.79–2.21) | 1.12 (0.67–1.87) |
| Remote past: mean age, 60–69 y† | 1.05 (0.79–1.42) | 1.14 (0.86–1.51) | 1.01 (0.69–1.49) | 1.25 (0.81–1.93) | 1.20 (0.80–1.79) | 1.26 (0.74–2.16) |
Data are given as relative risk (95 % confidence interval). All relative risks are presented per SD change in blood pressure component at baseline age and are adjusted for diabetes mellitus and smoking status. The mean ± SD values of the baseline, recent past, and remote past blood pressure measurements are given in Table 1.
Relative risks for antecedent blood pressure measurements are also adjusted for current (baseline) blood pressure measurements.
This article also showed that 28% of all ABI’s occurred on subjects whose current BP was in the non-hypertensive range, i.e. even if blood pressure is normal at the time of the clinic visit, antecedent hypertension (both recent and remote) could be used to identify those who remain at high risk of future stroke. In addition, risk estimates of antecedent blood pressure span a 30year period of observation for risk estimation, which underscore the importance of blood pressure assessments in midlife to impact risk of stroke even 30years later. Given that life expectancy is increasing in the United States, the implications of this study in public health are highly significant. Blood pressure assessment and resulting treatment modifications for patients during midlife in order to prevent future stroke needs to be emphasized.
Atrial Fibrillation (AF) and risk of stroke
An additional contribution of the Framingham Study for stroke prevention is the elucidation of non-valvular AF as an independent strong risk factor for stroke. C. Miller Fisher, M.D., had made the clinical and pathological association of AF to stroke in 1951.13 Although valvular AF with rheumatic heart disease had been long recognized as the basis for cerebral embolism, Dr. Fisher’s observation strongly suggested that established AF in the absence of mitral stenosis was an important source for cerebral embolism. In 1978 Dr Wolf and colleagues published a seminal article relating non-valvular AF to stroke risk .14 Following the procedures previously outlined for the surveillance of stroke in the Framingham study, they determined incidence rates of stroke in 4969 participants free of AF, and among participants with AF, in those with non-valvular and valvular AF. The observed-to-expected ratio of stroke incidence was provided, adjusted for blood pressure and age in each sex. After 24year of follow up, 345 strokes occurred, (168 men, 177 women). ABI accounted for 59% of all strokes, cerebral embolism accounted for 14%, and the remaining were classified as other 3%, TIA 9%, intracerebral hemorrhage 5% and subarachnoid hemorrhage 10%.
The authors found that independent of age and hypertension, participants with non-valvular AF had stroke incidence rates 5.6-fold greater than those without AF. The article also details the clinical features of an embolic stroke, which have guided clinicians in making judgments for the mechanism of stroke: “abrupt onset, often while active, of focal neurologic dysfunction, reaching its maximum in moments”, and the neuropathological findings consistent with cerebral embolism, validating their clinical impressions. Eleven of 20 participants with idiopathic AF died showing the high mortality carried by such strokes, and 6 underwent neuropathological examination of the brain: “cerebral infarct corresponded in location and age to the clinical event. Infarction was multiple in one case and associated with atrial thrombus and an old splenic infarct in another. The arteries were patent in two cases, and in one of these the infarct was hemorrhagic”.
A follow up publication by Wolf et al. elucidated the relations of age and risk of stroke in participants with AF.15 After attaining 30years of follow-up, the authors compared stroke incidence rates in participants who developed AF versus those without AF. Atrial fibrillation-associated strokes represented 14.7% of the total 462 initial stroke events during the observation period. Incident AF was detected in 303 participants (163 men, 140 women), and increased with age in both sexes from 0.4 and 0.0 per 1000 at age 30 to 39 years to 45.9 and 35.8 per 1000 at age 80 to 89 years in men and women respectively. Strokes occurred in 68 persons with AF and in 394 participants without AF. The two-year, age-specific incidence rates of stroke increased in parallel with age. The proportion of atrial fibrillation-associated stroke to total stroke was clearly related to age, increasing steadily from 6.7% for ages 50 to 59 years to 36.2% for ages 80 to 89 years. This report also notes the strength of effect of AF on risk of stroke in the elderly, compared to other prominent risk factors including hypertension, heart failure and coronary heart disease. While all of these factors contributed independently to stroke risk in younger participants, their effect declined with age, and in participants between ages 80 and 89 years, only AF remained a significant risk factor after accounting for the others. The risk of stroke attributed to AF increased with age, from 7.3% in subjects aged 60 to 69 years to 30.8% in those aged 80 to 89 years, even after adjusting for the effect of systolic blood pressure, heart failure and coronary heart disease. Table 3 shows the proportion of strokes attributed to AF compared to those attributed to coronary heart disease and heart failure. Since there is increasing longevity in the US population, and now there are several available treatments for stroke risk reduction in patients with AF, the relevance of FHS contributions to reduce the burden of stroke, particularly in the elderly are obvious.
Table 3.
(Source Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Archives of internal medicine. Sep 1987;147(9):1561–1564, Table 4, page 1563).
Percent of strokes attributed to non-rheumatic chronic atrial fibrillation, coronary heart disease and cardiac failure, men and women combined.
| Attribution of Strokes, % |
||||
|---|---|---|---|---|
| Age Group, y |
Coronary Heart Disease |
Cardiac Failure |
Nonrheumatic Chronic Atrial Fibrillation† |
|
| Unadjusted | Adjusted | |||
| 50–59 | 19.5 (9.9, 29.1) | 9.4 (3.1, 15.7) | 6.2 (0.9, 11.5) | …‡ |
| 60–69 | 17.2 (9.3, 25.3) | 9.1 (4.2, 14.0) | 6.4 (2.1, 10.7) | 7.3 (2.8, 11.8) |
| 70–79 | 19.5 (9.9, 29.1) | 13.9 (7.6, 20.2) | 17.4 (10.5, 24.3) | 16.5 (9.8, 23.2) |
| 80–89 | 10.6 (0.0, 29.5) | 11.1 (0.0, 23.1) | 28.9 (14.0, 43.8) | 30.8 (15.1, 46.5) |
Thirty-year follow-up, the Framingham study.
Significant increase with age before and later adjusting for systolic blood pressure (P<.05). Numbers in parentheses indicate 95% confidence limits.
Insufficient data.
Genetic risk factors and stroke risk
The careful prospective ascertainment of stroke occurrence and methodic classification of stroke type in the FHS Original and Offspring cohorts over an extended period placed the FHS in a unique advantage point to clarify the role of family history on stroke risk. Previously, parental history of stroke remained a controversial factor in terms of its contribution to stroke risk in the Offspring, mostly due to several issues leading to misclassification of stroke events, and limitations in detection of stroke events. In a study including 3443 stroke-free Framingham offspring participants with verified parental stroke status by 65 years of age, incident stroke was ascertained in the offspring over a follow up of 8 years after a baseline examination, yielding up to 11 029 person-observation periods (77 534 person-years).16 Stroke was documented in 106 parents and 128 offspring participants, with 74 parental and 106 offspring strokes being ischemic. In multivariable Cox regression analyses adjusted for age, sex, sibship, and baseline stroke risk factors, the authors observed that parental history of both all stroke in general and ischemic subtype in particular, was associated with an increased risk of incident stroke of the same type in the offspring (hazard ratio, 2.79; 95% confidence interval, 1.68 to 4.66; P<0.001 for all stroke; and hazard ratio, 3.15; 95% confidence interval, 1.69 to 5.88; P<0.001 for ischemic stroke). The higher risk (HR) in offspring with parental stroke was seen across all quintiles of baseline Framingham Stroke Risk Profile score, showing the independent contribution of parental history of stroke. Both, paternal and maternal history of stroke, were related to risk of stroke in the offspring. This study exemplifies one of the major strengths of the FHS, which is the careful assessment of three generations of participants for incident stroke, and provided important evidence of the role of genetic factors in stroke risk in the offspring.
The advances in technologies for mapping of the human genome have been incorporated in the FHS, allowing for the performance of genome wide association studies of genetic determinants of stroke. Given that stroke is a complex disease, where multiple genetic risk factors are likely each contributing in small amounts to stroke risk, large samples are required to detect such genetic factors. FHS investigators have lead a collaborative effort along with four other major epidemiological studies, the Cohorts for Heart and Aging Research in Genomic Epidemiology –CHARGE- Consortium, in order to attain a sufficient sample size to study the underlying genetic determinants of the most common stroke types. In a recent publication,17 a GWAS was carried including 19,602 white persons (mean [±SD] age, 63±8 years) in the context of the CHARGE consortium. A total of 1544 incident strokes (1164 ischemic strokes) occurred over a period of 11 years. The authors identified two intergenic single-nucleotide polymorphisms (SNPs) on chromosome 12p13 associated with stroke at GWAS significance levels (P<5×10−8). The SNPs were in proximity to the NINJ2 gene, which encodes an adhesion molecule expressed in glia and shows increased expression after nerve injury, and the WINK1 gene which has been implicated in blood pressure levels and severity of hypertension. The risk of total (i.e., all types) and ischemic stroke was increased with hazard ratios of 1.30 (95% confidence interval [CI], 1.19 to 1.42) and 1.33 (95% CI, 1.21 to 1.47), respectively, with population attributable risks of 11% and 12% total stroke and 14 to 17% for ischemic stroke in the discovery cohorts. The results were replicated in three independent cohorts, including a cohort of 2430 black persons with 215 incident strokes (191 ischemic strokes), another cohort of 574 black persons with 85 incident strokes (68 ischemic strokes), and 652 Dutch persons with ischemic stroke and 3613 unaffected persons.
Genetic epidemiology methods and knowledge are advancing at a fast pace, and the FHS is at the forefront of such research efforts. FHS investigators will continue to provide much needed insight of the role of genetic factors in risk of stroke in general, and specific stroke subtypes in particular, which will enable eventual use of this information in preventive clinical care.
Clinical Perspective
Undoubtedly the FHS has contributed to, and in many ways led the practice of preventive cardiovascular medicine. The epidemiological observations made over the course of nearly seven decades of follow up have clarified erroneous concepts in the medical community and introduced many others to shape clinical practice. The case of the relation of blood pressure and cerebrovascular disease is no different. The reports in the first 20 to 30years of the FHS contributed greatly to dispel erroneous concepts and to advance our knowledge of the relation between various BP components and stroke in general and ABI in particular. Specifically, FHS data showed that 1) mean SBP is more closely related to stroke risk that DBP. Dr Kannel and colleagues disproved the existent concept that DBP was the main BP component causing hypertensive organ damage by showing that the risk of ABI was more strongly related to SBP than DBP. Further, MAP or DBP did not add significantly to stroke risk prediction compared to SBP alone. While both BP components were thought to cause vascular damage, it was shown that SBP was the main driving force as regards stroke risk. 2) The work by Kannel et al. elucidated the modifications of the relation of hypertension and stroke risk by sex and age. The risk increased for both men and women with age, but there was a change with increasing age such that men had higher risk in middle age and women had higher risk in advanced age. In addition, the observation that the impact of BP in stroke risk did not decrease with age clearly showed that hypertension is not innocuous in the elderly. 3) Kannel and colleagues also clarified the absence of a critical threshold in the relation of BP and stroke risk, but rather a continuum in risk for both men and women; indeed, the risk of stroke has been shown to increase almost linearly with BP level, even with measurements considered normal. At the same time, the investigators noted that hypertension is more strongly associated to risk of stroke than risk of other major cardiovascular outcomes including coronary heart disease and peripheral arterial disease.
In 2001, using data acquired over 50 years into the study, FHS investigators published a remarkable study showing that 1) midlife detection of elevated BP affects future stroke risk even 3 decades later, and 2) antecedent hypertension is helpful to further stratify risk of persons with current normotension. The risk of stroke was increased by antecedent hypertension (recent and remote) after adjusting for current BP measurements, and in normotensive persons, the risk of stroke was significantly higher in the presence of antecedent hypertension. The benefit of these observations is clear for a practicing clinician: to demonstrate long term effects of blood pressure, highlight the importance of blood pressure surveillance and early detection of hypertension, and for patient education, which is essential for effective preventive medicine. In addition, this article emphasizes the fact that, regardless of age, history of antecedent hypertension aids to select patients for treatment and stroke risk reduction. In 2008, about 60years into the Framingham Heart Study and 4 decades following Dr Kannel’s initial report, the hypertension in the very elderly trial (HYVET) was published,18 demonstrating that treatment of hypertensive persons older than 80 years reduces the risk of stroke, death from stroke and other cardiovascular outcomes and is well tolerated.
Concerning the role of AF in stroke, the Framingham Study investigators have provided crucial epidemiological data, proving the strong association of cerebral embolism with non-valvular AF, and further clarifying the age and sex relations between non-valvular AF and incident stroke. Importantly, Framingham investigators noted the increasing incidence of AF with age, and the higher proportion of strokes attributed to AF in the elderly. These observations contributed significantly to subsequent clinical trials of stroke prevention treatments in persons with AF. Given the increasing population reaching older groups in the United States, and the now widely available treatments for stroke prevention in patients with AF, the Framingham Study observations regarding the role of AF in stroke in the elderly are of major public health impact. The original Framingham papers have provided major contributions to the shift in the practice of cerebrovascular preventive medicine. Current treatment guidelines are founded on data from the Framingham Study as regards hypertension and stroke prevention, and heavily influenced by Framingham data concerning AF and prevention of stroke, and set the stage for the future of preventive cerebrovascular medicine.
Lastly, in the wakes of the era of individualized preventive medicine, FHS investigators are leading the way to further our understanding of the contribution of genetic factors to stroke susceptibility. Important advances have been made, and continued efforts will likely help elucidate how information about genetic factors can be used in clinical practice to prevent cerebrovascular disease in individuals.
Acknowledgments
Funding/Support: This work was supported by contract N01-HC-25195 from the National Heart, Lung, and Blood Institute, the National Institute of Neurological Disorders and Stroke (R01NS17950), and the National Institutes of Aging grants R01AG08122, R01AG16495 and K23AG038444.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Keith NM, Wagener HP, Kernohan JW. The Syndrome of Malignant Hypertension. Archives of internal medicine. 1928;41(2):48. [Google Scholar]
- 2.Moser M. Historical perspectives on the management of hypertension. Journal of clinical hypertension. 2006 Aug;8(8) Suppl 2:15–20. doi: 10.1111/j.1524-6175.2006.05836.x. quiz 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA : the journal of the American Medical Association. 1967 Dec 11;202(11):1028–1034. [PubMed] [Google Scholar]
- 4.Stokes JB., 3rd The national high blood pressure education program. J Am Pharm Assoc. 1974 Apr;14(4):172–176. doi: 10.1016/s0003-0465(16)32942-1. [DOI] [PubMed] [Google Scholar]
- 5.Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. A cooperative study. JAMA : the journal of the American Medical Association. 1977 Jan 17;237(3):255–261. [PubMed] [Google Scholar]
- 6.Elias MF, Wolf PA, D'Agostino RB, Cobb J, White LR. Untreated blood pressure level is inversely related to cognitive functioning: the Framingham Study. American journal of epidemiology. 1993 Sep 15;138(6):353–364. doi: 10.1093/oxfordjournals.aje.a116868. [DOI] [PubMed] [Google Scholar]
- 7.Wolf PA. Contributions of the Framingham Heart Study to stroke and dementia epidemiologic research at 60 years. Archives of neurology. 2012 May;69(5):567–571. doi: 10.1001/archneurol.2011.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolf PA. Fifty Years at Framingham: Contributions to Stroke Epidemiology. Vol 92. Lippincott, Williams & Wilkins; 2003. [PubMed] [Google Scholar]
- 9.Kannel WB, Wolf PA, Verter J, McNamara PM. Epidemiologic assessment of the role of blood pressure in stroke. The Framingham study. JAMA : the journal of the American Medical Association. 1970 Oct 12;214(2):301–310. [PubMed] [Google Scholar]
- 10.Lassen NA. Epidemiologic assessment of the role of blood pressure in stroke. JAMA : the journal of the American Medical Association. 1996 Oct 16;276(15):1279–1280. [PubMed] [Google Scholar]
- 11.Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke; a journal of cerebral circulation. 2011 Jan;42(1):227–276. doi: 10.1161/STR.0b013e3181f7d043. [DOI] [PubMed] [Google Scholar]
- 12.Seshadri S, Wolf PA, Beiser A, et al. Elevated midlife blood pressure increases stroke risk in elderly persons: the Framingham Study. Archives of internal medicine. 2001 Oct 22;161(19):2343–2350. doi: 10.1001/archinte.161.19.2343. [DOI] [PubMed] [Google Scholar]
- 13.Fisher M, Adams RD. Observations on brain embolism with special reference to the mechanism of hemorrhagic infarction. Journal of neuropathology and experimental neurology. 1951 Jan;10(1):92–94. [PubMed] [Google Scholar]
- 14.Wolf PA, Dawber TR, Thomas HE, Jr, Kannel WB. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study. Neurology. 1978 Oct;28(10):973–977. doi: 10.1212/wnl.28.10.973. [DOI] [PubMed] [Google Scholar]
- 15.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Archives of internal medicine. 1987 Sep;147(9):1561–1564. [PubMed] [Google Scholar]
- 16.Seshadri S, Beiser A, Pikula A, et al. Parental occurrence of stroke and risk of stroke in their children: the Framingham study. Circulation. 2010 Mar 23;121(11):1304–1312. doi: 10.1161/CIRCULATIONAHA.109.854240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ikram MA, Seshadri S, Bis JC, et al. Genomewide association studies of stroke. The New England journal of medicine. 2009 Apr 23;360(17):1718–1728. doi: 10.1056/NEJMoa0900094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. The New England journal of medicine. 2008 May 1;358(18):1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]