Abstract
Purpose
To validate an algorithm based upon International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes for acute myocardial infarction (AMI) documented within the Mini-Sentinel Distributed Database (MSDD).
Methods
Using an ICD-9-CM-based algorithm (hospitalized patients with 410.x0 or 410.x1 in primary position), we identified a random sample of potential cases of AMI in 2009 from 4 Data Partners participating in the Mini-Sentinel Program. Cardiologist reviewers used information abstracted from hospital records to assess the likelihood of an AMI diagnosis based on criteria from the joint European Society of Cardiology and American College of Cardiology Global Task Force. Positive predictive values (PPVs) of the ICD-9-based algorithm were calculated.
Results
Of the 153 potential cases of AMI identified, hospital records for 143 (93%) were retrieved and abstracted. Overall, the PPV was 86.0% (95% confidence interval; 79.2%, 91.2%). PPVs ranged from 76.3% to 94.3% across the 4 Data Partners.
Conclusions
The overall PPV of potential AMI cases, as identified using an ICD-9-CM-based algorithm, may be acceptable for safety surveillance; however, PPVs do vary across Data Partners. This validation effort provides a contemporary estimate of the reliability of this algorithm for use in future surveillance efforts conducted using the FDA’s MSDD.
Keywords: Myocardial infarction, coronary artery disease, validation, administrative data, Food and Drug Administration, Mini-Sentinel
INTRODUCTION
Through the Sentinel Initiative launched in May 2008, the U.S. Food and Drug Administration (FDA) is developing a national electronic system for postmarket risk identification and analysis of medical product safety that will use automated healthcare data to complement its existing surveillance systems.(1, 2) The Mini-Sentinel pilot (www.mini-sentinel.org) – an FDA-funded project designed to inform development of the Sentinel Initiative – is a collaborative effort between FDA and a number of Academic and Data Partners.(3) The success of the Sentinel Initiative’s surveillance efforts depends in part on the ability to accurately identify health outcomes of interest using automated healthcare databases.
Automated healthcare databases are frequently used to conduct epidemiologic research,(4-6) but the accuracy of a diagnosis from these data sources can be uncertain. In recognition of this uncertainty, FDA has requested that the Mini-Sentinel develop procedures for conducting outcome validation and use these procedures to validate the diagnostic criteria for several important health outcomes, beginning with acute myocardial infarction (AMI).
AMI was selected as the first health outcome to be validated because AMI is an important adverse outcome for FDA to be able to monitor. Drug-induced myocardial infarction has been difficult to identify through existing passive surveillance mechanisms.(1) Validation of an AMI algorithm within the Mini-Sentinel Distributed Database (MSDD) would enhance the FDA’s ability to conduct needed surveillance efforts. The primary goal of this validation activity was to assess the positive predictive value (PPV) of an algorithm based upon International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes for AMI documented within the MSDD. The MSDD currently comprises the administrative and claims data of 17 Data Partners formatted into a common data model.(7) An additional goal of this project was to develop the procedures needed to conduct an outcome validation in the setting of public health surveillance. A recent paper(8) describes the development of those procedures in detail.
METHODS
We studied patients enrolled in health plans represented by 4 large and geographically diverse Data Partners: the HMO Research Network, Humana, HealthCore, Inc. and Kaiser Permanente Center for Effectiveness and Safety Research (CESR). Due to the project’s inclusion in the FDA’s Sentinel Initiative, it was not under the purview of the Office of Human Research Protection and, therefore, did not require Institutional Review Board (IRB) approval (8-11). Each Data Partner was provided with a privacy packet prepared by the Mini-Sentinel Privacy Panel. This packet included: 1) the Mini-Sentinel Privacy Panel White Paper describing data privacy issues in Mini-Sentinel (9); 2) a letter from the Department of Health and Human Services Office for Human Research Protections (OHRP) to the FDA stating that the regulations OHRP administers do not apply to the Sentinel Initiative (OHRP oversees all IRBs); and 3) a letter from the FDA to the Mini-Sentinel Principal Investigator explaining FDA’s legal authority to obtain data for use in its Sentinel and Mini-Sentinel activities. The privacy packet described the legal basis for determining that the work of the Mini-Sentinel pilot is not under the purview of IRBs.
Source Population
The source population included patients hospitalized for electronically identified AMI between January 1, 2009 and December 31, 2009. All patients were required to be enrollees of the health plan for the entire duration of hospitalization (no patient was excluded due to this criterion). To increase generalizability, there were no restrictions on age, sex, or other patient characteristics. There was no baseline period required and there were no exclusions based on previous disease.
Case identification
Patients with claims evidence of AMI were identified by selecting those with an ICD-9-CM code for AMI (410.x0, 410.x1) in the principal or primary position on facility claims for hospitalizations. Participating Data Partners executed a distributed SAS program (SAS version 9.1, SAS Institute, Cary, North Carolina) designed to query their own locally maintained administrative and claims databases to identify a random sample of AMI cases and the hospitals in which they received care. Using this program, we achieved our goal of identifying a random sample of at least 100 AMI cases for validation. A sample of 100 cases would allow determination of the PPV of the diagnostic coding algorithm with a 95% confidence interval (CI) of ± 0.10, assuming a PPV of 50%.
Data Partners subsequently retrieved and redacted records of potential AMI cases, including hospital transfer records where available. These redacted records were made available for full text medical chart review by trained nurse abstractors.
Since this was the first validation activity to be conducted using the FDA MSDD, there was no precedent for our expected retrieval rate of AMI cases. A rate of 66% was projected as a conservative estimate based on the diversity of hospital sites and the anticipated complexities; a minimum of 150 charts requested was therefore deemed sufficient to obtain at least 100 cases of AMI. In order to distribute chart requests equally among 4 sites, 38 charts were requested from each Data Partner with the exception of one which was splitting its chart retrieval among 3 sites (13 charts per site) and therefore provided 39 in total. In sum, a total of 153 charts with a diagnosis of AMI were requested from participating Data Partners.
Case Confirmation
Two trained nurse abstractors reviewed records provided by the 4 Data Partners and completed a standardized data abstraction form (Appendix A) which had been developed to provide information on sex, age, race, length of hospital stay and transfer to or from another hospital, as well as clinical information pertinent to the diagnosis of AMI. Abstracted clinical information included EKG images, cardiac biomarkers, information on ischemic symptoms and results of cardiac diagnostic tests (Appendix A). Both abstractors gathered data from the first 10 cases. This abstracted information was reviewed together by both nurse abstractors to ensure high inter-rater reliability on items critical for the adjudication process. In consultation with FDA staff and individuals with clinical and epidemiologic expertise relevant to cardiovascular disease, the lead team created an adjudication protocol (Appendix B) based on standardized criteria from the joint European Society of Cardiology and American College of Cardiology Global Task Force(12, 13) and based on the literature on troponin standardization.(14)
Abstracted information was reviewed independently by two cardiologists. Cardiologist adjudicators were provided with copies of EKGs and copies of all cardiac tests and procedure reports of all likely AMI cases. The adjudicators did not review discharge summaries but were instead provided with abstracted case information. They then classified cases of possible AMI as either: (1) definite MI; (2) probable MI; (3) no MI; or (4) unable to determine. The adjudicators were provided criteria for AMI (Appendix B) but were not instructed on specific criteria for distinguishing definite from probable cases of AMI. They were asked to use their clinical judgment to make this determination.
An AMI was considered to be present if both cardiologist adjudicators categorized the case as definite or probable. When the adjudicators disagreed on the classification of a case (i.e. if one adjudicator indicated definite or probable and one indicated no MI or unable to determine), they met and reached consensus; consensus was reached in all cases. The initial assessment of the adjudicators was compared and inter-rater reliability was calculated using Cohen’s kappa statistic.(15)
A positive predictive value (PPV) was calculated as the percentage of confirmed cases (definite or probable) of AMI among all hospitalizations identified. The PPVs (overall and according to Data Partner, patient demographics [sex, age, race], and characteristics of hospital stay [length of hospital stay, transfer to or from another hospital]) were estimated. Because specific identification of Data Partners was not necessary for the purpose of the analysis, we present PPVs stratified by Data Partner (table 1) but do not identify Data Partners by name.
Table 1.
Calculated positive predictive value (PPV) and 95% confidence interval for acute myocardial infarction (AMI) by Data Partner.
| Data Partner | Number of charts requested | Charts obtained (%) | AMI confirmed | AMI not confirmed | Insufficient information in medical chart | PPV (%) | 95 % CI |
|---|---|---|---|---|---|---|---|
| Data Partner 1 | 38 | 32 (84.2) | 26 | 4 | 2 | 81.3 | 63.6, 92.8 |
| Data Partner 2 | 38 | 38 (100) | 29 | 1 | 8 | 76.3 | 59.8, 88.6 |
| Data Partner 3 | 38 | 35 (92.1) | 33 | 0 | 2 | 94.3 | 80.1, 99.3 |
| Data Partner 4 | 39 | 38 (97.4) | 35 | 1 | 2 | 92.1 | 78.6, 98.3 |
|
| |||||||
| Overall | 153 | 143 (93.5) | 123 | 6 | 14 | 86.0 | 79.2, 91.2 |
RESULTS
Of the 153 potential cases of AMI identified from health plan administrative data, hospital records for 143 (93%) were available for review. Medical record information for 7 cases could not be obtained due privacy concerns. Hospital IRBs in these cases required a patient signature to release charts. This occurred despite the information provided to Data Partners indicating that the FDA Sentinel Initiative activities are not under the purview of the OHRP and do not require IRB approval. Medical records for 3 potential cases could not be located. Retrieval rates across the Data Partners ranged from 84% to 100% of cases identified from health plan data.
The mean age of patients for whom records were abstracted was 69.5 years (range 27-94) and 47% were female. Of the 143 cases, 14 cases required joint review by the two cardiologists; they reached consensus in all cases and ultimately determined that 123 cases were either definite or probable AMIs (118 were classified by at least one cardiologist as definite; 5 were characterized by both as probable).
There were 20 cases that were judged not to be consistent with a definite or probable AMI, either because one or both cardiologists felt that there was insufficient information available to confirm or deny the presence of an AMI (14 cases) or because both cardiologists agreed that there was sufficient information available to indicate that the case was not an AMI (6 cases). The kappa score for inter-rater reliability, based on initial assessment of the cardiologist adjudicators, was found to be 0.60 (95% CI: 0.42, 0.78), which indicates moderate agreement.
Overall, the PPV was 86.0% (95% CI: 79.2%, 91.2%). PPVs ranged from 76.3% to 94.3% across the Data Partners (Table 1). Several different subgroups defined a priori were examined (Table 2), but PPV estimates were imprecise due to the small sample size.
Table 2.
The positive predictive value and 95% confidence interval of acute myocardial infarction (AMI) by patient characteristics
| Total (n) | AMI present (n) | No MI (n) | Unable to determine (n) | Positive predictive value (%) | 95 % Confidence Interval | |
|---|---|---|---|---|---|---|
| Total | 143 | 123 | 6 | 14 | 86.0 | 79.2 to 91.2 |
| Age <75 years | 74 | 70 | 2 | 2 | 94.6 | 86.7 to 98.5 |
| Age 75+ | 53 | 42 | 3 | 8 | 79.3 | 65.9 to 89.2 |
| Age Unavailable | 16 | 11 | 1 | 4 | 68.8 | 41.3 to 89.0 |
| Male | 76 | 71 | 2 | 3 | 93.4 | 85.3 to 97.8 |
| <75 | 45 | 43 | 1 | 1 | 95.6 | 84.9 to 99.5 |
| 75+ | 26 | 23 | 1 | 2 | 88.5 | 69.9 to 97.6 |
| Age unavailable | 5 | 5 | 0 | 0 | 100 | |
| Female | 67 | 52 | 4 | 11 | 77.6 | 65.8 to 86.9 |
| <75 | 29 | 27 | 1 | 1 | 93.1 | 77.2 to 99.2 |
| 75+ | 27 | 19 | 2 | 6 | 70.4 | 49.8 to 86.3 |
| Age unavailable | 11 | 6 | 1 | 4 | 54.6 | 23.4 to 83.3 |
| White | 73 | 64 | 4 | 5 | 87.7 | 77.9 to 94.2 |
| Nonwhite | 14 | 11 | 1 | 2 | 78.6 | 49.2 to 95.3 |
| Length of stay <3 days | 15 | 13 | 1 | 1 | 86.7 | 59.5 to 98.3 |
| Length of stay ≥3 days | 115 | 97 | 5 | 13 | 84.4 | 76.4 to 90.5 |
| Transferred from or to another hospital | 62 | 54 | 1 | 7 | 87.1 | 76.2 to 94.3 |
| Not transferred | 81 | 69 | 5 | 7 | 85.2 | 75.6 to 92.1 |
DISCUSSION
Our results suggest that AMI can be reliably identified in the MSDD. Rates of record retrieval were higher than expected across all Data Partners. This was attributed in part to successful relationship building with hospital partners, distribution of comprehensive informational packets and frequent follow-up on all chart requests. The project’s status as an FDA Sentinel Initiative effort may also have contributed to high rates of chart return. We had the opportunity to review over 90% of possible cases, demonstrating that the MSDD was capable of yielding a retrieval rate comparable to that of previous AMI validation efforts.(17, 19, 23, 31)
Previous validation studies(16-33) have found AMI to be a reliably coded event.(34) Published AMI validation studies frequently report PPV’s of 90% or greater,(19, 21, 24, 26, 27, 29, 31-33) although some studies report values lower than this range.(18, 23) With a slightly lower PPV than past validation studies, our project provides an update to previously published studies in several important ways. We drew on a broader patient population, validating cases through medical record review and using a contemporary definition of AMI.(12, 13) We found that the PPV rate varied across the 4 Data Partners. Our small sample size leads us to interpret all between-group comparisons with caution.
A number of prior studies validating the diagnosis of AMI in different patient samples have been limited to a single state or province,(18, 19, 21, 29, 33) although several studies conducted outside the U.S. incorporated a broader segment of the study country’s population. (24, 27, 32) In addition, other studies used exclusion criteria based on age(29) or included only Medicaid,(19) Medicare(21) or Veterans Administration(33) populations. We drew potential cases from multiple Data Partners across the U.S. and we did not exclude any cases based on age or other patient characteristics. With the exception of one study by Yeh et al.,(29) our validation approach differed from those of previous studies due to our decision to conduct chart reviews and due to the validation criteria we used. Several prior studies did not conduct chart reviews but relied instead on linking data to a cardiac registry database(18, 24) or on questionnaires sent to patients’ primary providers for confirmation of the identified AMI.(32) Where chart reviews were conducted, validation criteria included World Health Organization criteria,(21, 26, 35) Women’s Health Initiative criteria (19, 36) and 2003 criteria from the American Heart Association.(27, 37) Yeh et al. used similar validation criteria to ours as well as an identical case definition and found a PPV of 96.7% for MIs occurring in members of a single health plan, Kaiser Permanente Northern California, between 1999 and 2008. Our inclusion of a broader population may provide a more generalizable PPV estimate for future FDA surveillance efforts nationwide.
Limitations of our validation activity include our small sample size. While we sampled from a broad segment of the insured U.S. population, our small overall number of records makes it difficult to draw conclusions about PPV in various patient subgroups. The study population also consisted only of patients with health insurance.
This validation project demonstrated high rates of record retrieval from hospitals nationwide and employed vigorous validation criteria, including the use of expert, board-certified cardiologist reviewers to adjudicate using updated criteria for the definition of AMI. Our PPV for AMI was somewhat lower than had been previously suggested by the literature, but provides a contemporary estimate of the reliability of this ICD-9-CM-based algorithm for use in future surveillance efforts conducted in the MSDD.
CONCLUSIONS
The overall PPV of potential AMI cases, as identified using an ICD-9-CM-based algorithm, may be acceptable for safety surveillance purposes; however, PPVs varied across the 4 Data Partners included in this validation activity. Our investigation provides a contemporary estimate of the reliability of this ICD-9-based algorithm for use in future surveillance efforts conducted in the Mini-Sentinel program.
Key points.
Acute Myocardial Infarction (AMI) can be reliably identified for medical product safety surveillance in the Food and Drug Administration’s (FDA’s) Mini-Sentinel Distributed Database (MSDD), using an ICD9-CM-based algorithm and contemporary validation criteria.
The positive predictive value (PPV) of this AMI algorithm in the MSDD is 86%, slightly lower than observed in other published studies.
This validation activity demonstrates high medical record retrieval rates in the setting of an FDA-funded public health surveillance effort conducted in a distributed system of electronic healthcare databases.
Acknowledgments
The authors would like to thank the following Data Partners for their input into the validation process and their tireless efforts to obtain and prepare charts:
HealthCore, Inc. Jenni (Jie) Li, Amanda Rodriguez, and Tom Puenpatom
-
HMO Research Network
Group Health Research Institute –Danelle Wallace
Meyers Primary Care Institute/Fallon Community Health Plan – Susan Andrade
Humana –Mary Costantino
Kaiser Permanente Center for Effectiveness and Safety Research – Daniel Jaynes
Kaiser Permanente Hawaii –Yee Hwa Daida
In addition, the authors would like to thank Dr. Karen Hicks (Division of Cardiovascular and Renal Products, Center for Drug Evaluation and Research, FDA) for her assistance in developing the abstraction and adjudication tools; Dr. Jorge Yarzebski for assistance in obtaining and abstracting charts; Dr. Guillermo Talero; Michaela Richardson, RN; and Catherine Emery, RN for their careful chart abstraction work.
Funding information: This project was supported through funding from contract HHSF223200910006I from the U.S. Food and Drug Administration (FDA). Dr. Sarah Cutrona is supported by Award Number KL2RR031981 from the National Center for Research Resources (NCRR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCRR or the National Institutes of Health.
Appendix A



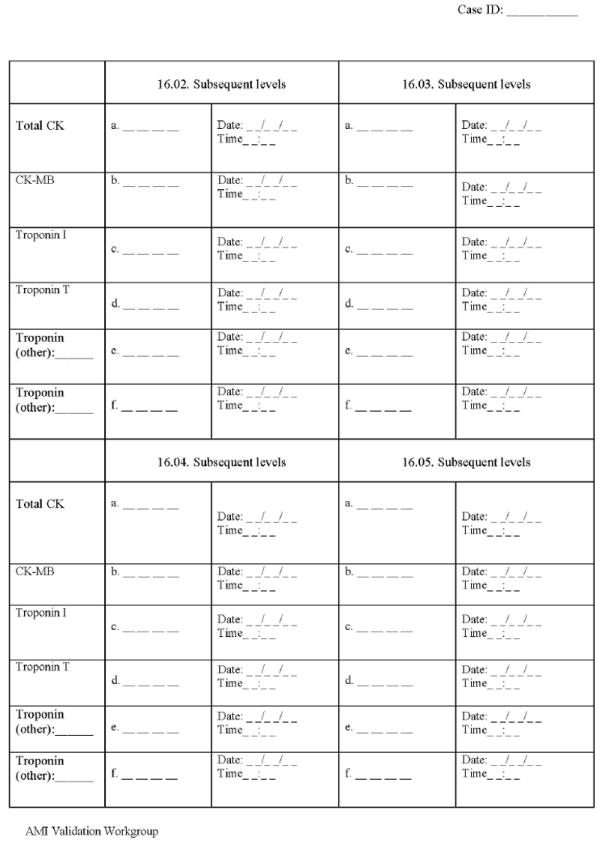
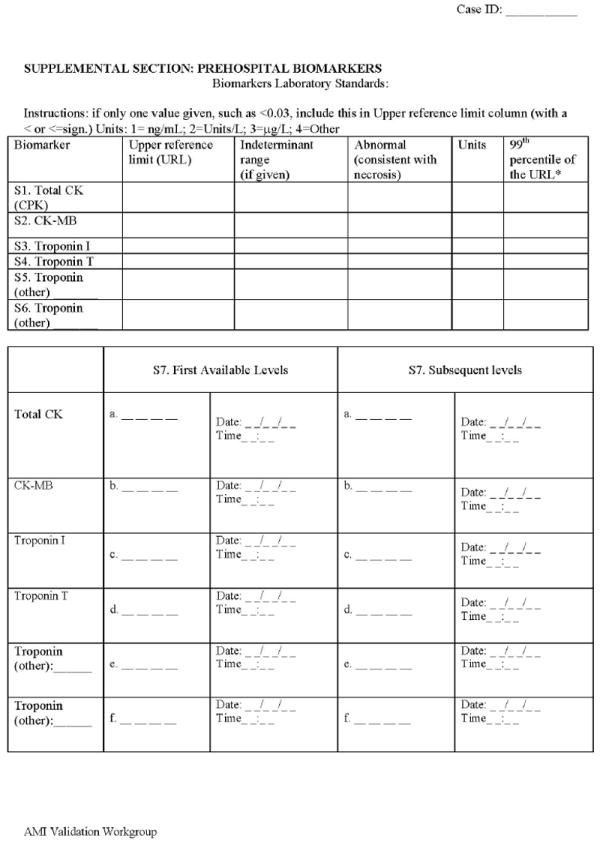
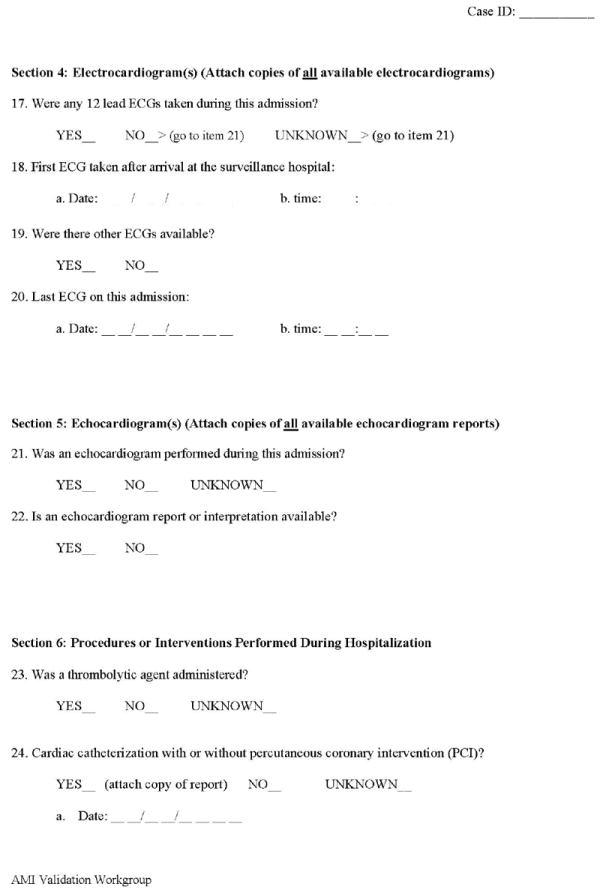
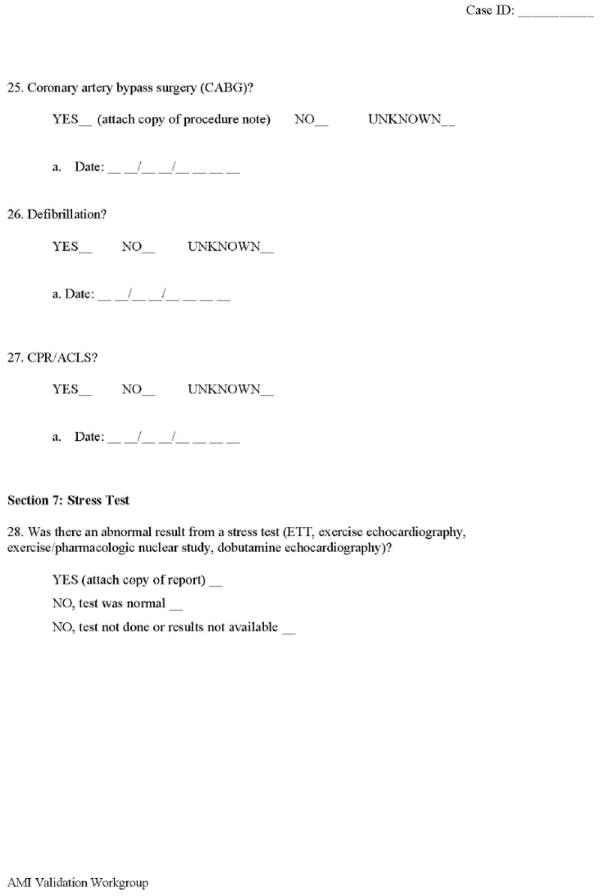

Mini-Sentinel acute myocardial infarction validation: Abstraction form
Appendix B


Mini-Sentinel acute myocardial infarction validation: Adjudication for
Footnotes
COI statement: Authors have no conflicts of interest to report.
References
- 1.Behrman RE, Benner JS, Brown JS, McClellan M, Woodcock J, Platt R. Developing the Sentinel System--a national resource for evidence development. N Engl J Med. Feb 10;364(6):498–9. doi: 10.1056/NEJMp1014427. [DOI] [PubMed] [Google Scholar]
- 2.Robb MA, Racoosin JA, Sherman RE, Gross TP, Ball R, Reichman ME, et al. The US Food and Drug Administration’s Sentinel Initiative: expanding the horizons of medical product safety. Pharmacoepidemiol Drug Saf. 2012 Jan;21(Suppl 1):9–11. doi: 10.1002/pds.2311. [DOI] [PubMed] [Google Scholar]
- 3.Platt R, Carnahan RM, Brown JS, Chrischilles E, Curtis LH, Hennessy S, et al. The U.S. Food and Drug Administration’s Mini-Sentinel program: status and direction. Pharmacoepidemiol Drug Saf. 2012 Jan;21(Suppl 1):1–8. doi: 10.1002/pds.2343. [DOI] [PubMed] [Google Scholar]
- 4.Goff SL, Feld A, Andrade SE, Mahoney L, Beaton SJ, Boudreau DM, et al. Administrative data used to identify patients with irritable bowel syndrome. J Clin Epidemiol. 2008 Jun;61(6):617–21. doi: 10.1016/j.jclinepi.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Andrade SE, Gurwitz JH, Chan KA, Donahue JG, Beck A, Boles M, et al. Validation of diagnoses of peptic ulcers and bleeding from administrative databases: a multi-health maintenance organization study. J Clin Epidemiol. 2002 Mar;55(3):310–3. doi: 10.1016/s0895-4356(01)00480-2. [DOI] [PubMed] [Google Scholar]
- 6.Andrade SE, Graham DJ, Staffa JA, Schech SD, Shatin D, La Grenade L, et al. Health plan administrative databases can efficiently identify serious myopathy and rhabdomyolysis. J Clin Epidemiol. 2005 Feb;58(2):171–4. doi: 10.1016/j.jclinepi.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Curtis LH, Weiner MG, Boudreau DM, Cooper WO, Daniel GW, Nair VP, et al. Design considerations, architecture, and use of the Mini-Sentinel distributed data system. Pharmacoepidemiol Drug Saf. 2012 Jan;21(Suppl 1):23–31. doi: 10.1002/pds.2336. [DOI] [PubMed] [Google Scholar]
- 8.Cutrona SL, Toh S, Iyer A, Foy S, Cavagnaro E, Forrow S, et al. Design for validation of acute myocardial infarction cases in Mini-Sentinel. Pharmacoepidemiol Drug Saf. 2012 Jan;21(Suppl 1):274–81. doi: 10.1002/pds.2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services, Office of the Secretary. Standards for Privacy of Individually Identifiable Health Information. Final Rule 45 CFR Parts 160 and 164: Federal Register. 2002:53182–273. [PubMed] [Google Scholar]
- 10.Rosati K, Evans B, McGraw D. HIPAA and Common Rule Compliance in the Mini-Sentinel Pilot. [8 May 2012];Unpublished White Paper. http://minisentinel.org/work_products/About_Us/HIPAA_and_CommonRuleCompliance_in_the_Mini-SentinelPilot.pdf.
- 11.McGraw D, Rosati K, Evans B. A policy framework for public health uses of electronic health data. Pharmacoepidemiol Drug Saf. 2012 Jan;21(Suppl 1):18–22. doi: 10.1002/pds.2319. [DOI] [PubMed] [Google Scholar]
- 12.Alpert JS, Thygesen K, Jaffe A, White HD. The universal definition of myocardial infarction: a consensus document: ischaemic heart disease. Heart. 2008 Oct;94(10):1335–41. doi: 10.1136/hrt.2008.151233. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007 Nov 27;50(22):2173–95. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 14.Tate JR, Bunk DM, Christenson RH, Katrukha A, Noble JE, Porter RA, et al. Standardisation of cardiac troponin I measurement: past and present. Pathology. 42(5):402–8. doi: 10.3109/00313025.2010.495246. [DOI] [PubMed] [Google Scholar]
- 15.Fleiss JL, Cohen J, Everitt BS. Large sample standard errors of kappa and weighted kappa. Psychological Bulletin. 1969;72:323–7. [Google Scholar]
- 16.Kachroo S, Jones N, Reynolds M. Final report prepared for the Foundation for the National Institutes of Health via the Observational Medical Outcomes Partnership (OMOP) Lexington, MA: United Biosource Corporation; 2009. Systematic literature review for evaluation of myocardial infarction. [Google Scholar]
- 17.Lux L, Jarrett N, West S. Systematic evaluation of health outcome of interest definitions in observational studies and clinical definitions for the Observational Medical Outcomes Partnership: Myocardial infarction report. Research Triangle Park, NC: RTI International; 2009. [Google Scholar]
- 18.Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002 Aug;144(2):290–6. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- 19.Choma NN, Griffin MR, Huang RL, Mitchel EF, Jr, Kaltenbach LA, Gideon P, et al. An algorithm to identify incident myocardial infarction using Medicaid data. Pharmacoepidemiol Drug Saf. 2009 Nov;18(11):1064–71. doi: 10.1002/pds.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hammar N, Alfredsson L, Rosen M, Spetz CL, Kahan T, Ysberg AS. A national record linkage to study acute myocardial infarction incidence and case fatality in Sweden. Int J Epidemiol. 2001 Oct;30(Suppl 1):S30–4. doi: 10.1093/ije/30.suppl_1.s30. [DOI] [PubMed] [Google Scholar]
- 21.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004 Jul;148(1):99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 22.Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M. The validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol. 2003 Feb;56(2):124–30. doi: 10.1016/s0895-4356(02)00591-7. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen-Khoa BA, Goehring EL, Jr, Werther W, Gower EW, Do DV, Jones JK. Hospitalized cardiovascular diseases in neovascular age-related macular degeneration. Arch Ophthalmol. 2008 Sep;126(9):1280–6. doi: 10.1001/archopht.126.9.1280. [DOI] [PubMed] [Google Scholar]
- 24.Pajunen P, Koukkunen H, Ketonen M, Jerkkola T, Immonen-Raiha P, Karja-Koskenkari P, et al. The validity of the Finnish Hospital Discharge Register and Causes of Death Register data on coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2005 Apr;12(2):132–7. doi: 10.1097/00149831-200504000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Petersen LA, Wright S, Normand SL, Daley J. Positive predictive value of the diagnosis of acute myocardial infarction in an administrative database. J Gen Intern Med. 1999 Sep;14(9):555–8. doi: 10.1046/j.1525-1497.1999.10198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Solomon DH, Schneeweiss S, Glynn RJ, Kiyota Y, Levin R, Mogun H, et al. Relationship between selective cyclooxygenase-2 inhibitors and acute myocardial infarction in older adults. Circulation. 2004 May 4;109(17):2068–73. doi: 10.1161/01.CIR.0000127578.21885.3E. [DOI] [PubMed] [Google Scholar]
- 27.Varas-Lorenzo C, Castellsague J, Stang MR, Tomas L, Aguado J, Perez-Gutthann S. Positive predictive value of ICD-9 codes 410 and 411 in the identification of cases of acute coronary syndromes in the Saskatchewan Hospital automated database. Pharmacoepidemiol Drug Saf. 2008 Aug;17(8):842–52. doi: 10.1002/pds.1619. [DOI] [PubMed] [Google Scholar]
- 28.Wahl PM, Rodgers K, Schneeweiss S, Gage BF, Butler J, Wilmer C, et al. Validation of claims-based diagnostic and procedure codes for cardiovascular and gastrointestinal serious adverse events in a commercially-insured population. Pharmacoepidemiol Drug Saf. Jun;19(6):596–603. doi: 10.1002/pds.1924. [DOI] [PubMed] [Google Scholar]
- 29.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. Jun 10;362(23):2155–65. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 30.Varas-Lorenzo C, Rodriguez LA, Maguire A, Castellsague J, Perez-Gutthann S. Use of oral corticosteroids and the risk of acute myocardial infarction. Atherosclerosis. 2007 Jun;192(2):376–83. doi: 10.1016/j.atherosclerosis.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 31.Garcia Rodriguez LA, Tacconelli S, Patrignani P. Role of dose potency in the prediction of risk of myocardial infarction associated with nonsteroidal anti-inflammatory drugs in the general population. J Am Coll Cardiol. 2008 Nov 11;52(20):1628–36. doi: 10.1016/j.jacc.2008.08.041. [DOI] [PubMed] [Google Scholar]
- 32.Hammad TA, McAdams MA, Feight A, Iyasu S, Dal Pan GJ. Determining the predictive value of Read/OXMIS codes to identify incident acute myocardial infarction in the General Practice Research Database. Pharmacoepidemiol Drug Saf. 2008 Dec;17(12):1197–201. doi: 10.1002/pds.1672. [DOI] [PubMed] [Google Scholar]
- 33.Warner JJ, Weideman RA, Kelly KC, Brilakis ES, Banerjee S, Cunningham F, et al. The risk of acute myocardial infarction with etodolac is not increased compared to naproxen: a historical cohort analysis of a generic COX-2 selective inhibitor. J Cardiovasc Pharmacol Ther. 2008 Dec;13(4):252–60. doi: 10.1177/1074248408323136. [DOI] [PubMed] [Google Scholar]
- 34.Platt R, Wilson M, Chan KA, Benner JS, Marchibroda J, McClellan M. The new Sentinel Network--improving the evidence of medical-product safety. N Engl J Med. 2009 Aug 13;361(7):645–7. doi: 10.1056/NEJMp0905338. [DOI] [PubMed] [Google Scholar]
- 35.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994 Jul;90(1):583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 36.Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, et al. Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Ann Epidemiol. 2003 Oct;13(9 Suppl):S122–8. doi: 10.1016/s1047-2797(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 37.Luepker RV, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D, et al. Circulation. 20. Vol. 108. AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute; 2003. Nov 18, Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; pp. 2543–9. [DOI] [PubMed] [Google Scholar]


