Abstract
Microbial cellulose is a natural polymer that can hold a quantity of water without any disconformities. Therefore, it is proposed for use as wound dressing material. We report a case of 28% total body surface area partial-thickness flame burn: approximately 4.5% superficial partial-thickness burns on anterior face and 23.5% combined superficial and deep partial-thickness burns on both upper arms and anterior trunk. A microbial cellulose dressing, Nanocell (Thai Nano Cellulose Co Ltd, Bangkok, Thailand), was applied to the face wound only once, without any further dressing change. Progress of healing, until full epithelialization on the face, was observed for 2 weeks. During the treatment period, the patient did not show any irritation or allergic reaction to this new dressing, and wound swab culture showed no evidence of bacteria presence. This innovative material can be an alternative dressing for superficial partial-thickness burn wounds.
Keywords: Burn, Microbial cellulose, Partial-thickness wound
Introduction
The types of burn injuries described by the American Burn Association are first-, second-, and third-degree burns. First-degree burns involve only the epidermis. Second-degree (partial-thickness) burns involve the epidermis and some of the dermal layer and can be subcategorized into superficial partial-thickness and deep partial-thickness wounds. Third-degree burns have injuries extending to the whole dermis layer and affect some of the tissues below the skin. Superficial partial-thickness burns are characteristically red, moist, and painful. The wounds are moist because the epidermis loses its barrier function. Pain and redness exist because of the presence of the dermal nerves and blood vessels.1 The initial stage is the topical application of medication to the wound 1 to 2 times daily. One of the common drugs used in these wounds is 1% silver sulfadiazine; however, silver sulfadiazine necessitates frequent dressing changes (at least once daily), and dressing changes can cause pain and local maceration, can be cytotoxic to keratinocytes as well as fibroblasts, and induce bacterial resistance.2 Microbial cellulose is a natural polymer synthesized by Acetobactor xylinum. In 1886, A. J. Brown published an article on the cellulose-producing activity of these bacteria.3 The cellulose has a leathery, thick membrane that can hold a quantity of water without any disconformities. As a result, it is considered to be a biomedical material suitable as a wound dressing. Nowadays, intensive research efforts have revealed the effectiveness of this type of dressing when used on ulcers, including burn wounds. Hemicellulose dressings can induce adhesion and sustain the proliferation of fibroblasts in the human skin. The dressing may have highly desirable characteristics as an ideal skin substitute.4 Moreover, it has remarkable moistening and cooling properties. It may be used on superficial burn wounds in order to balance wound moisture and protect wounds from bacterial invasion. The aim of this report is to document our experience with the use of the microbial cellulose dressing called Nanocell (Thai Nano Cellulose Co Ltd, Bangkok, Thailand) in a case of superficial burn wound from fire.
Case Report
This is a case report of a 54-year-old woman who suffered a second-degree burn on face, both upper arms, and anterior trunk. The total of body surface area burned was 28%. The burn wounds were 23.5% combined superficial and deep partial-thickness (both upper arms and anterior trunk) and 4.5% superficial partial-thickness burns (face). She did not have any comorbidities or past medical or surgical history. She was referred from a rural hospital and admitted to the burn unit at Siriraj Hospital, Bangkok, Thailand. The incident was caused by burn from flames from a gas explosion. Apparently, the gas canister inside a gas stove had exploded while she was cooking in the kitchen. After the initial explosion, the gas from the canister, which was covered, was still burning. The flames then wrapped around her and burned her face and body. Her first vital signs showed a blood pressure of 140/98 mm Hg, pulse rate of 120 beats per minute, respiratory rate of 25 breaths per minute, and body temperature of 37.5°C. She weighed 64 kg, measured 162 cm in height, and her body mass index was 24.39 kg/cm2. Tests from laboratory analysis showed the following results: sodium, 155 mmol/L; potassium, 4.5 mmol/L; chloride, 102 mmol/L; serum urea nitrogen, 15 mg/dL; creatinine, 1.2 mg/dL; complete blood cell count: hemoglobin, 12.8 g/dL; hematocrit, 40%; mean corpuscular volume, 90 fL; mean corpuscular hemoglobin, 29.5 pg; mean corpuscular hemoglobin concentration, 32 g/dL; white blood cell count, 13.5 × 103/μL; and platelet count, 200 × 103/μL. Parkland formula fluid resuscitation (4 mL/kg per percentage of total body surface area burn) was used as initial fluid replacement. She was administered adequate nutrition via nasogastric tube and also received analgesics (tramadol hydrochloride, 50 mg, 3 times daily) for pain relief.
On the day after admission to our burn unit, the burn wounds were cleaned with normal saline solution. The patient was then transferred to the operating room for tangential debridement of deep partial-thickness burn on her upper limbs and body. One percent silver sulfadiazine was used as topical medication. Dressing change was done daily, and the attending surgical team visited her twice daily. Microbial cellulose dressing was applied to the superficial partial-thickness wound. It adhered well to the wound, and use of other bandages was not necessary (Figure 1).
Figure 1.

Superficial partial thickness wound applying with microbial cellulose dressing.
During the treatment, the patient did not show any irritation or allergic reaction to this new dressing, and wound culture showed no evidence of bacteria presence. Observations by the surgeon team showed progression of healing until full epithelialization on day 12. The dressing proved to induce healing on its own, and peeling off was easy on day 13. The wound exhibited complete epithelialization (Figure 2). Lab analysis results showed no abnormality, so the patient was discharged on day 16 after burn wound closure. Figure 3 was a picture taken 3 weeks after discharge.
Figure 2.

Complete epithelialization within two weeks.
Figure 3.

Face of patient at 3 weeks after discharge home.
Pain score was also evaluated from point of admission by means of a visual analog scale. The maximum score, 10, indicates that the patient has severe pain, and the minimum, 0, implies no pain. The patient had a pain score of 8 on the first day and gradually decreased to a pain score of 2 on the day of discharge. She had less pain after dressing application, especially on her face. The pain score for each day is shown in Figure 4.
Figure 4.
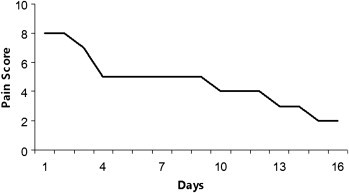
Visual pain analog score in each day.
Discussion
One of the major aims of burn treatments is to quickly accomplish wound closure in order to increase the rate of healing and to provide immediate pain relief.5-7 In addition, proper wound management must avoid any infection or dehydration.1,6
Second-degree burns are defined as those burns in which the entire epidermis and variable portions of the dermis layer are destroyed. A superficial second-degree (partial-thickness) burn is characterized by heat injury to the upper one-third of the dermis, leaving a good blood supply. This type of burn usually heals within 10 to 14 days. Deep partial-thickness or deep second-degree burns extend well into the dermal layer, and fewer viable epidermal cells remain. The initial nonsurgical management is debridement of loose dead tissue and application of a silver-based cream or dressing. If silver sulfadiazine cream is used, the wounds need to be gently washed daily to remove the old cream, and the cream must be reapplied, followed by a secondary dressing. If the deep partial-thickness wound does not heal in 3 weeks, early surgical skin closure with skin graft is often the preferred treatment.1,6
Because the follicular region is not injured, cell growth is possible and sebaceous glands and hair follicles are developed in the new epidermis. However, the patient will experience severe pain because the sensory nerves in the dermal layer are not injured. Winter reported in 1962 that the wound-healing process, especially re-epithelization, is accelerated in moist wounds.7 It is now commonly accepted that a moist wound environment hastens the healing of both acute and chronic wounds and promotes the growth of new tissues. A balanced moist surface in acute wounds facilitates the action of growth factors, cytokines, and chemokines, thus promoting cellular growth and the construction of a wound matrix.8 A treatment that has moisturizing and cooling effects on the burn wound may be beneficial to the patient.
Microbial cellulose may be a novel dressing for partial-thickness burn wounds. Its accelerated wound-healing properties have been investigated in only a few clinical studies but have shown effective results.9 The dressing is derived from a bacterium named A xylinum and cultured in liquid medium. The structure of its cellulose from complex processes differs from other plant cellulose. An ultrafine network of cellulose nanofibers can hold a large amount of water while displaying great elasticity, a high degree of wet strength, and conformity.10 This network may be suitable for providing a moist environment in burn wounds in order to promote wound healing.
The procedure for applying this material is similar to the procedure for applying others: Sterile dressings are removed from the packaging, placed directly on the wound surface, and then covered with gauze. The dressing needs to be applied to the wound only once, and no other dressings are required. With the dressing’s cooling property, patient acceptance is good, and the pain score gradually reduces each day.
Fontana et al11 and Mayall et al12 studied this cellulose dressing in burns and chronic ulcers. This wound dressing material is more effective than others. It provides pain relief, protects the wound against infections, and accelerates wound healing. Another study revealed that microbial cellulose dressings proved to be more effective than conventional wound dressing materials in the treatment of chronic venous ulcers.13
In this case study, we report the use of microbial cellulose as a dressing to heal clean burn wounds. The application on our patient resulted in complete resolution of a moist environment for healing, protected from additional injury from scratching, and accelerated wound healing. In addition, it may have an advantage over an allogenic amnion, a primitive treatment for temporary wound coverage, because it is sterilized and comfortable to use. We believe that the microbial cellulose properties contribute to the wound-healing process in burn patients. Use of additional materials, such as antibiotics for infection prophylaxis, will further promote wound repair. Jung et al reported that silver nanoparticles combined with bacterial cellulose exhibited antimicrobial activity.14 If microbial cellulose can be clearly proven to have positive results in wound healing, it can be used in new products with a wide range of clinical applications.
Conclusion
The use of microbial cellulose dressing in partial-thickness burn wounds provides a moist environment, a cooling effect, and activation of wound healing, as well as improvement in pain reduction. This innovative material will be an alternative dressing in partial-thickness burn wounds.
Footnotes
Conflict of interest: The authors report no conflicts of interest.
References
- 1.Pham T., Gibran N., Heimbach D. Evaluation of the burn wound management decisions. In: Herdon D.N., editor. Total Burn Care. 3rd ed. WB Saunders Co; New York: 2007. pp. 119–126. [Google Scholar]
- 2.Muangman P., Pundee C., Opasanon S., Muangman S. A prospective, randomized trial of silver containing hydrofiber dressing versus 1% silver sulfadiazine for the treatment of partial thickness burns. Int Wound J. 2010;7(4):271–276. doi: 10.1111/j.1742-481X.2010.00690.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown A.J. On an acetic ferment which forms cellulose. Trans J Chem Soc. 1886;49:432–439. [Google Scholar]
- 4.Ferreira L.M., Sobral C.S., Blanes L., Ipolito M.Z., Horibe E.K. Proliferation of fibroblasts cultured on a hemi-cellulose dressing. J Plast Reconstr & Aesthetic Surg. 2010;63:865–869. doi: 10.1016/j.bjps.2009.01.086. [DOI] [PubMed] [Google Scholar]
- 5.Greenhalgh D.G. Wound healing. In: Herdon D.N., editor. Total Burn Care. 3rd ed. WB Saunders Co; New York: 2007. pp. 578–595. [Google Scholar]
- 6.Demling R.H., DeSanti L. Management of partial thickness facial burns (comparison of topical and bio-engineered skin substitutes) Burns. 1999;25:256–261. doi: 10.1016/s0305-4179(98)00165-x. [DOI] [PubMed] [Google Scholar]
- 7.Winter G.D. Formation of a scab and the rate of epithelialization of superficial wounds in the skin of the young domestic pig. Nature. 1962;193:293–294. doi: 10.1038/193293a0. [DOI] [PubMed] [Google Scholar]
- 8.Alvarez O.M., Mertz P.M., Eaglstein W.H. The effect of occlusive dressings on collagen synthesis and re-epithelialisation in superficial wounds. J Surg Res. 1983;35:142–148. doi: 10.1016/0022-4804(83)90136-1. [DOI] [PubMed] [Google Scholar]
- 9.Solway DR, Consalter M, Levinson DJ. Microbial cellulose wound dressing in the treatment of skin tears in the frail elderly. Wounds. Available at: http://www.woundsresearch.com/content/microbial-cellulose-wound-dressing-treatment-skin-tears-frail-elderly. Accessed October 20, 2010. [PubMed]
- 10.Brown R.M., Jr., Willison J.H.M., Richardson C.L. Cellulose biosynthesis in Acetobacter xylinum: Visualization of the site of synthesis and direct measurement of the in vivo process. Proc Nat Acad Sci. 1976;73(12):4565–4569. doi: 10.1073/pnas.73.12.4565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fontana J.D., de Souza A.M., Fontana C.K. Acetobacter cellulose pellicle as a temporary skin substitute. Appl Biochem Biotechnol. 1990;24-25:253–264. doi: 10.1007/BF02920250. [DOI] [PubMed] [Google Scholar]
- 12.Mayall R.C., Mayall A.C., Mayall L.C., Rocha H.C. The treatment of trophic ulcers of the limbs with a new skin substitute. Rev Braz Cir. 1990;80:257–283. [Google Scholar]
- 13.Alvarez O., Patel M., Booker J., Markowitz L. Effectiveness of a biocellulose wound dressing for the treatment of chronic venous leg ulcers: Results of a single center randomized study involving 24 patients. Wounds. 2004;16(7):224–233. [Google Scholar]
- 14.Jung R., Kim Y., Kim H.S., Jin H.J. Antimicrobial properties of hydrated cellulose membranes with silver nanoparticles. J Biomater Sci Polym Ed. 2009;20(3):311–324. doi: 10.1163/156856209X412182. [DOI] [PubMed] [Google Scholar]


