Abstract
Healing large chronic and acute wounds is a challenging task for wound care providers. It requires numerous visits and frequent dressing changes and often involves expensive therapeutic modalities. Our primary and ultimate goal is to heal these wounds as quickly as possible. In a prepared wound bed, covered with granulation tissue and free of infection, skin graft is the gold standard procedure to achieve this goal. One should keep in mind that not all patients are good candidates for surgery.
Keywords: Acute wound, Chronic wounds, Gold standard for wound closure, Skin grafts, Split-thickness skin grafts
Introduction
Healing large chronic and acute wounds is a challenging task for wound care providers. It requires numerous visits and frequent dressing changes, often involving expensive therapeutic modalities. Some patients, especially those who have debilitating wounds or are on narcotics, experience significant amounts of pain, which limits their ability to travel, drive, or work. Our primary and ultimate goal is to heal these wounds as quickly as possible. In a prepared wound bed, covered with granulation tissue and free of infection, skin graft is the gold standard procedure to achieve this goal. For wounds with exposed vessels, nerves, or bone, a flap closure should be used instead.
In this article we present a variety of acute and chronic wounds, with different etiologies, that were treated successfully with one application of split- thickness skin grafts (STSGs).
Case Presentations
Case 1
A 55 year old female had an incarcerated ventral hernia that was repaired with a mesh. The patient had postoperative wound infection and dehiscence that required multiple operative debridements. After a month of negative pressure wound therapy (NPWT), the wound bed was ready to receive the STSG, after which the wound healed in 3 weeks. See Figure 1.
Figure 1.
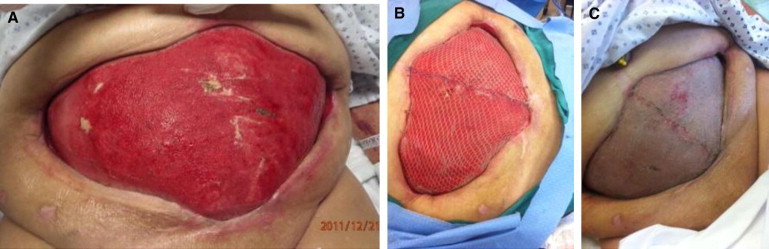
Wound Treatment for Woman Aged 55 Years With Postoperative Wound Infection and Dehiscence of Incarcerated Ventral Hernia Repaired With a Mesh. (A) Preoperative view of the wound; (B) intraoperative view of split-thickness skin graft placement; (C) healed abdominal wound 3 weeks post graft.
Case 2
A 65 year old male with left knee replacement had intraoperative injury to the popliteal artery, with compartment syndrome. This required left leg fasciotomies and arterial repair. After wound care with NPWT, the wound bed was covered with granulation tissue. STSG was then performed to close the wound, which healed in 1 month. See Figure 2.
Figure 2.
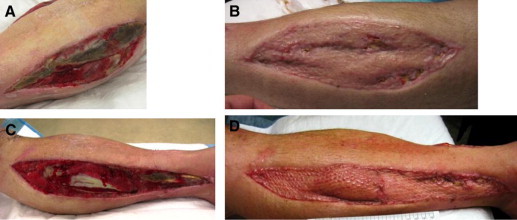
Left Leg Fasciotomy and Arterial Repair for a Man Aged 65 Years With Left Knee Replacement Who Presented With Intraoperative Injury to the Popliteal Artery With Compartment Syndrome. After wound care with negative pressure wound therapy, split-thickness skin graft was performed. (A) Pregraft lateral leg wound; (B) 1 month post graft, healed lateral leg wound; (C) pregraft medial leg wound; (D) 1 month post graft, healed medial leg wound.
Case 3
A 67 year old female with a history of obesity with lymphedema and chronic venous insufficiency had a nonhealing ulcer. After adequate compression therapy and wound bed preparation, the patient was taken to the operating room for surgical debridement and application of STSG. NPWT was applied as a bolster protective dressing. The wound healed 3 weeks later. See Figure 3.
Figure 3.

Treatment for Nonhealing Ulcer of a Woman Aged 67 Years With History of Obesity With Lymphedema and Chronic Venous Insufficiency. (A) Pregraft medial ankle wound; (B) intraoperative split-thickness skin graft placement; (C) healed wound, 3 months post graft.
Case 4
A 44 year old female with diabetes and Charcot arthropathy presented with infected medial ankle wound with skin necrosis. The patient underwent wound debridement with application of NPWT. She was also placed on antibiotic therapy. Three weeks later, when a healthy granular bed was achieved, an STSG was placed, and the wound healed in 4 weeks. See Figure 4.
Figure 4.

Treatment for Infected Medial Ankle Wound and Skin Necrosis in a Woman, Aged 44 Years, With Diabetes and Charcot Arthropathy. (A) Initial presentation with necrotic infected wound; (B) intraoperative view of split-thickness skin graft placement 3 weeks later, after healthy granular bed achieved via wound debridement, negative pressure wound therapy, and antibiotic therapy; (C) healed wound 4 weeks later.
Case 5
A 27 year old male with end stage renal disease and on hemodialysis, was admitted with necrotizing fasciitis to his right thigh and groin. After surgical debridement, NPWT, and antibiotic therapy, an STSG was applied, along with NPWT over the graft for coverage. His wound healed in 3 weeks. See Figure 5.
Figure 5.
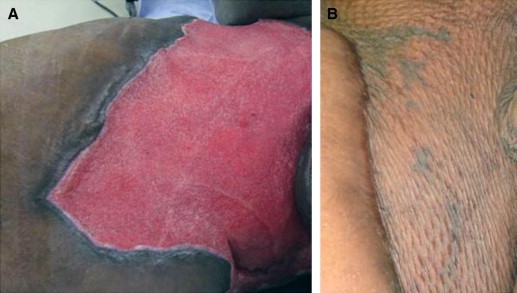
Treatment for Necrotizing Fasciitis to Right Thigh and Groin of Man Aged 27 Years on Hemodialysis for End-Stage Renal Disease. (A) right thigh wound before split-thickness skin graft; (B) healed wound 2 months post graft.
Case 6
An 18 year old cook assistant male, spilled boiling oil on his torso, sustaining a third-degree burn. After surgical excision of his eschar, STSGs were applied for permanent coverage of his resulting wounds. His torso was healed at 6 weeks. See Figure 6.
Figure 6.

Treatment for Third-Degree Boiling Oil Burn on Torso of Man Aged 18 Years. (A) Third-degree burn wound before split-thickness skin graft; (B) 5 days post tangential excision of the eschar and skin grafting; (C) healed torso wound 6 weeks post graft.
Case 7
91 year old female who presented to the office with a foul-smelling, bleeding, large basal cell carcinoma of the scalp. The carcinoma was excised in the operating room down to the pericranium, which was not involved on frozen section, and an STSG with a bolster dressing was applied. Her wound healed in 5 weeks. See Figure 7.
Figure 7.

Treatment for Foul-Smelling, Bleeding, Large Basal Cell Carcinoma of the Scalp of Woman Aged 91 Years. (A) Scalp basal cell carcinoma on presentation; (B) intraoperative view of split-thickness skin graft placement, with xeroform bolster dressing, after excision of carcinoma; (C) healed wound, 5 weeks post graft.
Discussion
Skin grafts are classified as either STSGs, which contain only a portion of the dermis with the entire epidermis, or full-thickness skin graft (FTSGs), which contain all skin layers, including some of the skin appendages. FTSGs have limited donor sites and have less long-term contracture and scar formation. These grafts are reserved for small defects located on the face, hands, and feet. The donor sites are closed primarily.
STSGs have are suitable for large donor sites, including thighs, buttocks, and back. STSG donor sites heal by epithelialization 10 to 14 days post graft.
Meshing STSGs increases the graft surface area and improves graft take by preventing fluid accumulation beneath the graft. The initial graft survival phase is avascular, and it depends on plasmatic imbibition. During this phase the graft survives on nutrient diffusion from local transudate. The second phase is characterized by the alignment of capillary buds between the graft and the wound bed to form new vascular connections, a process called inosculation. A tie-over bolster dressing or NPWT dressing is used to secure graft take and prevent shear forces, mobility, desiccation, and fluid accumulation, which may lead to graft failure. Other conditions that must be provided for successful graft take are a well-prepared wound bed with healthy granulation tissue and without devitalized tissue and infection. Research has shown that the application of NPWT over a skin graft improve graft take and healing by removing edema and speeding the disappearance of the plan of separation between the graft and the recipient wound bed.1
STSGs may be used as sheet grafts in large wounds or as pinch grafts in smaller wounds, especially when glabrous specialized skin is needed. In this case the applied pinch grafts reach confluence and cover the entire wound bed.2
STSGs and FTSGs are part of the reconstructive ladder of wound closure and should be considered by the surgeon when all appropriate conditions and indications are met.3
In this case study, we presented a variety of relatively large acute and chronic wounds that were successfully covered with sheets of STSGs, leading to wound healing. The patients experienced fast wound healing, which ultimately minimized long-term wound care, along with the pain and cost involved. Thus the patients could go on to their normal lives or to the needed rehabilitation. One should keep in mind that not all patients are good candidates for surgery. Associated medical conditions should be addressed prior to surgery. Unstable patients may not be good candidates for surgery. Most of the patients presented here needed medical clearance prior to surgery.
Footnotes
Conflict of interest: The authors report no conflicts of interest.
References
- 1.Simman R., Forte R., Silverberg B., Moriera-Gonzalez A., Williams F. A comparative histological pilot study of skin graft take with tie-over bolster dressing versus vacuum assisted closure in a pig model. Wounds. 2004;16(2):76–80. [Google Scholar]
- 2.Simman R. Medial plantar arch pinch grafts are an Effective technique to resurface palmar and plantar wounds. Ann Plast Surg. 2004;53(3):256–260. doi: 10.1097/01.sap.0000116247.68396.35. [DOI] [PubMed] [Google Scholar]
- 3.Simman R. Wound closure and the reconstructive ladder in plastic surgery. J Am Coll Cert Wound Spec. 2009;1(1):6–11. doi: 10.1016/j.jcws.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


