Abstract
Arthritis is a disease of joints. The biology of joints makes them very difficult targets for drug delivery in a manner that is specific and selective. This is especially true for proteinaceous drugs (“biologics”). Gene transfer is the only technology that can solve the delivery problem in a clinically reasonable fashion. There is an abundance of pre-clinical data confirming that genes can be efficiently transferred to tissues within joints by intra-articular injection using a variety of different vectors in conjunction with ex vivo and in vivo strategies. Using the appropriate gene transfer technologies, long-term, intra-articular expression of anti-arthritic transgenes at therapeutic concentrations can be achieved. Numerous studies confirm that gene therapy is effective in treating experimental models of rheumatoid arthritis (RA) and osteoarthritis (OA) in the laboratory. A limited number of clinical trials have been completed, which confirm safety and feasibility but only three protocols have reached Phase II; as yet, there is no unambiguous evidence of efficacy in human disease. Only two clinical trials are presently underway, both Phase II studies using allogeneic chondrocytes expressing TGF-β1 for the treatment of OA. Phase I studies using adeno-associated virus to deliver IL-1Ra in OA and IFN-β in RA are going through the regulatory process. It is to be hoped that the recent successes in treating rare, Mendelian diseases by gene therapy will lead to accelerated development of genetic treatments for common, non-Medelian diseases, such as arthritis.
Introduction
Diseases of joints are common, incurable and often difficult to treat. Of the 100 or so forms of arthritis, osteoarthritis (OA) is the most prevalent, affecting 27 million Americans 1; this number will rise as the population ages and gains weight. Although OA is considered a non-lethal disease, it is associated with an elevated risk of death 2. Because OA resists effective therapy, many patients progress to the need for prosthetic joint replacements. In 2004, over 650,000 artificial hips and knees were implanted at a cost of $26 billion. It is predicted that around 2 million hip and knee replacement surgeries will be performed in the year 2015 3. Overall, OA generates medical care expenditures exceeding $185 billion per year 4. OA is also a major clinical problem in veterinary medicine, particularly for horses and dogs.
Rheumatoid arthritis (RA), the next most prevalent form of arthritis, is a systemic autoimmune disease that affects approximately 1.3 million adult Americans 5. A further 294,000 individuals have the juvenile form of the disease. RA is associated with increased mortality 6, but treatment has improved dramatically during the past decade thanks to the introduction of proteinaceous antagonists of tumor necrosis factor (TNF) and other so-called biologics. However, less than 30% of patients show robust responses (ACR 70) to these drugs 7 which, as well as being very expensive, are associated with a number of side-effects related to their systemic mode of delivery. Moreover, even in an otherwise responsive patient, there may remain a number of individual joints that do not respond to the therapy.
The TNF antagonists in clinical use constitute the first wave of new, biologic therapies using proteins as drugs to combat arthritis 8. Although such drugs are delivered systemically by intravenous infusion or subcutaneous injection in RA, their application in OA and other localized forms of arthritis is constrained by the need to deliver the protein locally and specifically to a small number of target joints, and to sustain a therapeutic, intra-articular concentration of the protein for a considerable period 9. As described in more detail in the following sections, gene transfer is the only clinically reasonable technology that can do this 10.
Thus, although the common forms of arthritis are not genetic diseases in the Mendelian sense, they are amenable to gene therapy, using intra-articular gene transfer as a means of delivering therapeutic gene products to joints in a sustained fashion. When we suggested a gene therapy approach to treating arthritis over 20 years ago 11, it was the first non-Mendelian, non-lethal disease to be considered in this fashion. Other such indications have subsequently followed suit.
The essential biology of the arthritic joint
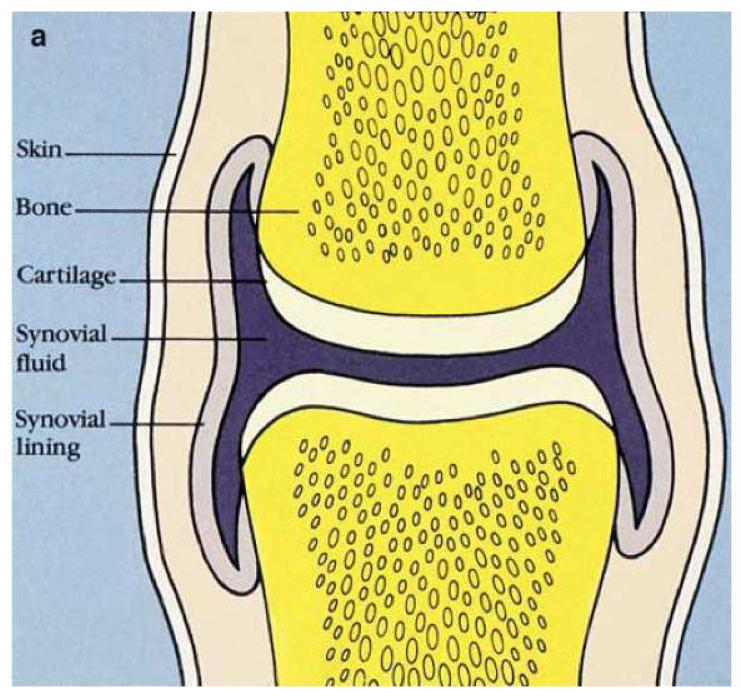
Arthritis is a disease of diarthrodial (moveable) joints. The anatomy of most such joints conforms to a basic plan where the ends of the long bones articulate within a discrete cavity lined by synovium (figure 1). The articulating surfaces of the bones are covered with articular cartilage, which, in conjunction with lubricating functions provided by the synovial fluid, ensures almost frictionless motion. Two fundamental pathological changes commonly occur during arthritis: inflammation and destruction of the articular cartilage.
Figure 1. Basic anatomy of the normal diarthrodial joint.
The articulating surfaces of the long bones are covered in articular cartilage that permits almost frictionless motion within a synovial cavity (joint space) containing a small volume of synovial fluid. The inner surface of the joint space is lined by synovium (synovial lining).
Inflammation in joints is seen as a synovitis and hypertrophy of the synovium, with increased volume and leukocytosis of the synovial fluid. In RA, inflammation is driven by autoimmune mechanisms 12,13. The importance of inflammation in OA, a degenerative condition, is increasingly, but not uniformly, appreciated 14. Where present, it may be driven by wear particles 15, soluble products released from the extracellular matrix of cartilage 16, crystals 17, cytokines 14 or mechanical forces 18.
Loss of articular cartilage is mediated by proteolytic enzymes directed against the major macromolecules of its extracellular matrix 19. In OA, these enzymes are synthesized and secreted by the chondrocytes within the cartilage in response to certain cytokines and mechanical forces. In RA this mechanism is supplemented by direct invasion of the cartilage and adjacent bone, by an enlarged, hyperplastic, destructive synovium. Moreover, inflammatory mediators inhibit the compensatory synthesis of matrix macromolecules by chondrocytes, thereby exacerbating the problem 20. These changes are often accompanied by chondrocyte cell death.
The pharmacokinetics of the joint
The obstacles to delivering drugs to joints in the sustained fashion required of chronic conditions like arthritis are not trivial. When drugs are delivered systemically, they enter the joint via fenestrated synovial capillaries 21. These exert a sieving effect that restricts the entry of larger molecules. Although this effect is reduced when synovitis is present, it still presents a barrier to entry for large proteins 22. Thus, to deliver therapeutic amounts of protein to joints in a sustained fashion via the circulation requires repeated, systemic administrations. With RA, which has important systemic, extra-articular involvement, this may be an advantage, but for everything else it is a disadvantage because such methods do not specifically target drugs to joints. Thus non-target organs are exposed to high concentrations of the drug, increasing the potential for unwanted side-effects as well as greatly increasing the amount of drug that needs to be administered and hence costs.
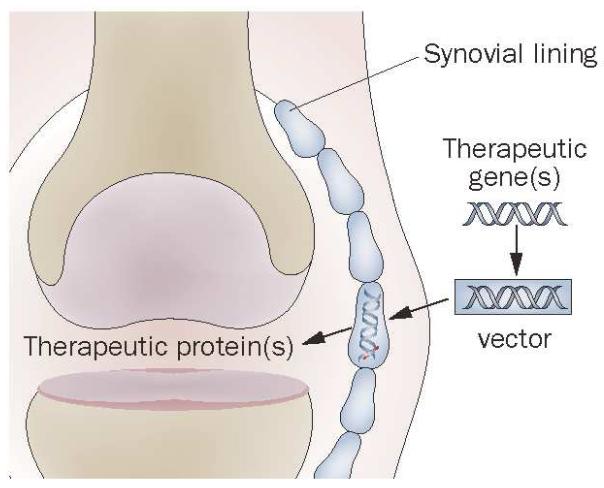
Because they are discrete, accessible cavities, joints lend themselves to direct, intra-articular injection 9. Although direct injection of proteins overcomes physiological barriers to entry, it is a futile therapeutic strategy because macromolecules are rapidly cleared from joints via the lymphatics 22. The intra-articular half-life of a soluble protein is typically a few hours, regardless of its size. Repeated intra-articular injections are not reasonable and the insertion of an infusion pump is not clinically feasible. Barriers to delivery are overcome, however, by the genetic transduction of cells within the joint, whereby the transgene product is synthesized and secreted locally for an extended period, accumulating in the synovial fluid and articular tissues to provide sustained, therapeutic concentrations lacking the peaks and troughs of intermittent application. This is the core logic that underpins arthritis gene therapy 10. The synovium has traditionally been the target tissue for gene transfer within the joint (figure 2) 11 but, as described later in this review, other articular tissues may also be important.
Figure 2. Basic concept behind local, intra-articular gene therapy for arthritis.
Complementary DNA encoding an anti-arthritic product, typically a secreted protein, is introduced into the joint. Cells within the synovium, and elsewhere, become transduced and synthesize the encoded transgene endogenously in a sustained fashion.
From reference 10, with permission.
Pre-clinical research
Several detailed reviews summarize comprehensively the pre-clinical, experimental findings concerning arthritis gene therapy 10,23-25. In essence the data confirm that genes may be transferred to the joints of experimental animals using ex vivo or in vivo strategies in conjunction with a variety of viral and non-viral vectors. If the host immune response is not activated, intra-articular transgene expression can persist for months 26, and possibly years, when using viral vectors. Intra-articular transgene expression using non-viral vectors tends to be low and transient 27.
A variety of different transgenes, reviewed in reference 25 25 have shown convincing efficacy in animal models of OA and RA, providing undeniable proof of principle. The majority of these transgenes encode immunomodulatory and anti-inflammatory cytokines, as well as proteinase inhibitors and growth factors for the protection and repair of cartilage. Those that have advanced into clinical trials, or are at an advanced stage of pre-clinical development, encode the interleukin-1 receptor antagonist (IL-1Ra), etanercept (a fusion protein of TNF soluble receptors and the Fc domain of IgG), transforming growth factor-β1 (TGF-β1) and interferon-β (IFN-β). Progress in their clinical translation will now be described.
Clinical trials – ex vivo delivery
MFG-IRAP
When we first suggested the use of gene therapy to treat arthritis, retrovirus vectors based upon the Moloney murine leukemia virus were the most advanced vectors available for human gene therapy, having been used in the first human clinical trials. Because retrovirus vectors require host cell division for effective transduction, it was necessary to develop an ex vivo strategy. It is a relatively straightforward matter to harvest and establish monolayer cultures of synovial fibroblasts, so these were an obvious choice of cells, especially as surgical synovectomy was a common clinical procedure.
Of the pathophysiological mediators present in arthritic joints, IL-1 seems a promising target. Because of its involvement in inflammation, immune function and cartilage destruction, it has potential involvement in both RA and OA. At the time these studies were starting IL-1Ra, a naturally occurring antagonist of IL-1, had been identified and cloned 28. This molecule has many advantages as a therapeutic molecule: it has no agonist activity, even at very high concentration; its dose-response is an uncomplicated rectangular hyperbola; it is safe; it is a small protein whose full coding sequence is easily cloned into a retrovirus without modification. Using a cDNA encoding the full length, native IL-1Ra molecule reduces the potential for complications with immunogenicity or other emergent properties than can occur with fusion proteins or other novelties.
Human IL-1Ra cDNA was cloned into a derivative of the Moloney murine leukemia virus known as MFG to produce the vector MFG-IRAP. Used in conjunction with autologous synovial fibroblasts, MFG-IRAP successfully transferred IL-1Ra cDNA into the knee joints of rabbits 29, mice 30 and dogs 31, with high levels of intra-articular transgene expression. A similar retrovirus constructed by Makarov’s group achieved this in rats 32. Safety of MFG-IRAP was confirmed in a number of studies, the most compelling of which involved the stable transduction of marrow cells in mice, leading to life-long, high levels of IL-1Ra expression without obvious harm 33.
Efficacy of gene transfer of IL-1Ra was confirmed in animal models of RA including antigen-induced arthritis in rabbits 34, zymosan- and collagen-induced arthritis in mice 30 and streptococcal cell wall-induced arthritis in rats 32. Promise of a therapeutic effect in humans was suggested by experiments in which human cartilage was co-implanted with human, rheumatoid synovium under the kidney capsule of SCID mice. When synovium was first transduced with MFG-IRAP, destruction of the cartilage matrix by chondrocytes was inhibited 35.
Translating these efficacious animal model results into a clinical trial for RA was constrained by the fact that this was the first protocol to come before the authorities proposing to perform human gene therapy for arthritis or any other non-lethal, non-Mendelian disease. Although RA is associated with reduced life-expectancy 6 it is not considered lethal in the conventional sense, a circumstance that considerably skewed the risk:benefit ratio so that safety became of predominant concern. The protocol thus included two important safety features: the recruitment of post-menopausal females to eliminate the possibility of germ-line transgene transmission, and gene delivery to joints that were scheduled for joint replacement surgery 36. We knew from pre-clinical studies that the transduced cells did not migrate from the joints into which they were injected, so joint replacement surgery should remove the genetically modified cells and eliminate the possibility of unpredictable, late responses.
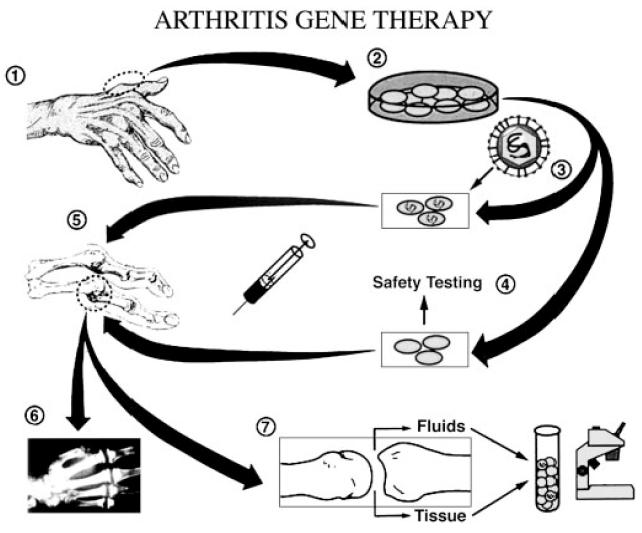
The study that was eventually approved 36 involved the injection of autologous synovial fibroblasts into the metacarpophalangeal (MCP; knuckle) joints 2-5 on one hand of 9 post-menopausal female subjects with RA (figure 3). In a double-blind fashion, two of the 4 MCP joints were injected with unmodified cells and two with transduced cells. The MCP joints are common sites of RA, and before the advent of TNF antagonists they were commonly replaced with sialistic prostheses. Thus it was possible to inject these joints one week before all 4 MCP joints were removed and replaced. This provided tissue for subsequent analysis of gene expression and other functions (figure 3).
Figure 3. Protocol for the first gene transfer to human joints.
Surgery of the joints of the hand or foot (step 1) provided autologous synovium, which was used to establish cultures of synovial fibroblasts (step 2). Half the cells were transduced with the retroviral vector (step 3), and all cells were tested for replication competent retrovirus and adventitious agents (step 4) before injection into MCP joints numbers 2–5 on one hand (step 5). In a double-blinded fashion, two joints received transduced cells, and two received control cells. One week later, the injected joints were surgically removed during total joint replacement surgery (step 6), and the retrieved tissues were analyzed for evidence of successful gene transfer and gene expression (step 7).
From reference 23 with permission.
This study was completed without incident and confirmed that it was possible to transfer genes into human, arthritic joints in a manner that is safe and acceptable to patients 37. The intraarticular expression of an active transgene product was confirmed. Because of the end stage of the disease, the small number of subjects, and the short time between injection and removal of the transgene, the study was not designed to study efficacy. However, several subjects reported symptomatic improvement.
A follow-up study by Wehling et al 38 included outcome measures based on a visual analog pain scale and the diameter of the MCP joint. Their study followed the one described above, but allowed 4 weeks between the injection of the cells and their removal, which was accomplished by synovectomy instead of joint replacement. Although the local ethics committee allowed 6 subjects to be included in the study, adverse events in an unrelated clinical trial of X-linked SCID which also used a derivative of MFG as the vector 39, caused the study to be closed after only two subjects had completed the protocol. One of these two responded in a dramatic fashion 38. The other also reported improvement. Synovial expression of IL-1Ra was confirmed and the expression of matrix metalloproteinase-3 (stromelysin-1) was strongly inhibited. No adverse events were noted.
Collectively, these are very encouraging data but, for a variety of reasons, no further development of this approach has occurred. One issue brought home by these studies was the enormous cost and complexity of ex vivo gene therapy using expanded, autologous cells. Moreover, during the course of these studies the first cases of insertional mutagenesis caused by a retroviral vector were reported 39. This threw the risk:benefit ratio back into high relief and made it even more difficult to apply to non-lethal diseases. Furthermore, the FDA tightened the regulations to require a 12-year follow up for gene therapy trials using an integrating vector. On top of this, the anti-TNFs and other biological drugs made an increasing impact on the treatment of RA 8, reducing (but not eliminating) the scope for a gene therapy. In view of these developments we decided to turn our attention to OA using in vivo gene delivery, as described later.
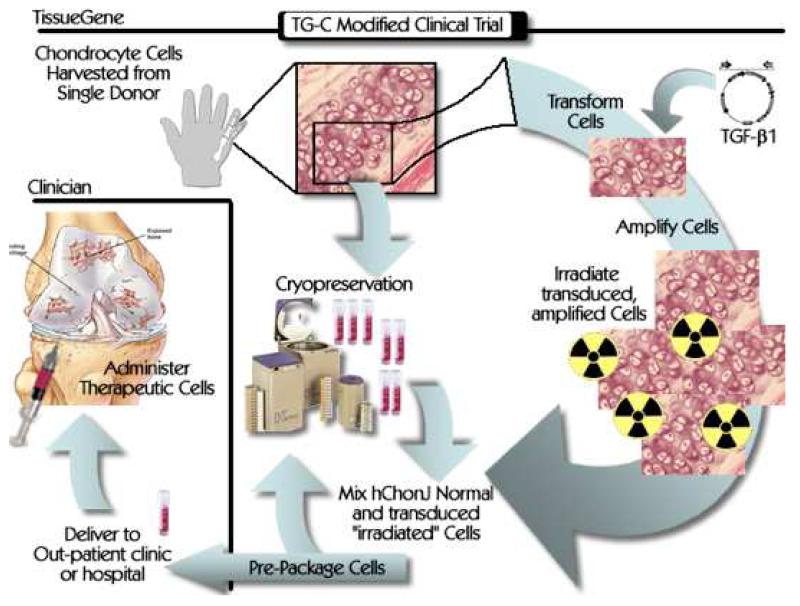
TissueGene-C
One way to make ex vivo gene delivery less cumbersome and expensive is to use an universal donor cell line. This has been accomplished for joints using a line of human chondrocytes established from the cartilage of a new born with polydactyly. These cells have been stably transduced with a retrovirus carrying cDNA encoding TGF-β1 40,41, which is thought to promote the healing of cartilage. The therapy based upon genetically modified chondrocytes is known as “TissueGene-C” or “TG-C”.
In many ways OA is a better target than RA for intra-articular gene therapy because, unlike RA, OA affects a limited number of joints and has no important systemic or other extra-articular components. Moreover, unlike the case with RA, there are no reliably effective treatments for OA.
Because the transduced chondrocytes are aneuploid it is necessary to irradiate the cells prior to injection to eliminate their ability to divide and generate tumors. The irradiated, transduced cells are mixed with untransduced, unirradiated cells prior to injection (figure 4). Two Phase I studies using this protocol have been completed in the USA and Korea. The cells were injected into the knee joints of subjects with OA prior to undergoing surgery to insert an artificial knee. No serious adverse events were reported 42. Phase II studies are now underway and encouraging preliminary data were recently presented 43.
Figure 4. Protocol for use of genetically modified, allogeneic chondrocytes in osteoarthritis.
Transduced chondrocytes expressing TGF-β1 are irradiated and mixed with unmodified cells in a 1:3 ratio. They are delivered to the clinic for intra-articular injection.
From reference 42, with permission.
In vivo delivery – emergence of AAV as the vector of choice
The encumbrances of ex vivo gene delivery to joints were recognized early, and considerable research evaluated vectors derived from adenovirus, herpes virus, high-titer retrovirus, lentivirus and a wide range of non-viral vectors as vehicles for in vivo gene delivery to joints 44-48. However, all of these vectors have shortcomings, and adeno-associated virus (AAV) has emerged as the vector of choice.
The general advantages of recombinant AAV as a vector are well known: wild-type virus causes no known disease; it transduces non-dividing cells; it is thought to have low immunogenicity etc. 49,50 However, only Gouze et al 26 have specifically identified the requirements of a successful vector for achieving long-term expression in joints and demonstrated how AAV uniquely satisfies these requirements.
As part of a study into the factors that limit transgene expression in joints, Gouze et al 26 compared an integrating virus (lentivirus) with a non-integrating virus (adenovirus) in immunocompetent and athymic rats. Green fluorescent protein (GFP) and human IL-1Ra were used as the transgenes, with expression driven by the cytomegalovirus (CMV) or elongation factor 1α promoter. Long-term expression was not achieved in immunocompetent animals. However, GFP and IL-1Ra expressed for the life of the athymic animals, regardless of the vector or promoter. This suggests that long-term transgene expression can be achieved if neither the vector nor the transgene triggers an immune reaction in the host; furthermore, this does not require viral integration. The latter conclusion suggests that enduring populations of quiescent cells exist within joints and sustain transgene expression from a constitutive promoter for extended periods of time.
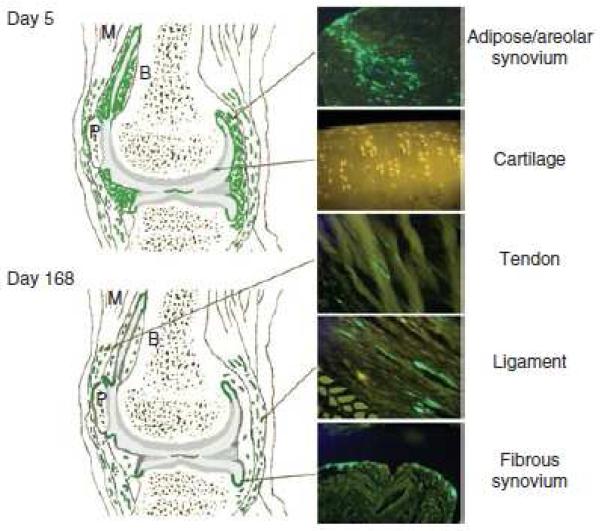
Examination of joints by fluorescence microscopy (figure 5) helped identify the location of such cells. Early after the injection of virus, most of the GFP-fluorescence occurred in the synovium. This was lost with time, possibly due to turnover of the synovial cells. Persistent GFP expression occurred in fibroblasts present in ligaments and capsule, as well as in the region where the synovium meets the cartilage. The persistence of transgene expression in ligaments agrees with older data of Oligino et al 46 using herpes virus vectors.
Figure 5. Fibroblasts resident in fibrous articular tissues support stable expression of exogenous transgenes.
After intra-articular injection of lentiviral or adenoviral vectors containing the cDNA for GFP into the knees of nude rats, groups of animals were killed at days 5 and 168. The knee joints and surrounding tissues were harvested intact, decalcified, and processed for histology. For each joint, the approximate positions of fluorescent cells identified in serial sagittal whole-knee sections were tabulated in green on knee-joint diagrams similar to that shown on the left. On the right, images are characteristic of the appearance of the GFP+ cells in tissue sections at the different times (×20 magnification). Lines indicate the approximate regions represented by the tissue sections. The numbers of GFP+ cells in the synovium and sub-synovium were reduced dramatically at day 168. The density and distribution of GFP+ cells in the tendon, ligament, and fibrous synovium were largely unchanged over the duration of the experiment. No fluorescent cells were seen in the articular cartilage with either virus at any time point.
From reference 26, with permission
Consideration of these findings leads to the conclusion that AAV is about the only clinically reasonable option, at present, for obtaining persistent, therapeutic levels of transgene expression after in vivo delivery to joints. Lentivirus is very powerful 48,51 but, as an integrating retrovirus, raises too many safety issues. Non-integrating lentiviruses have been developed but are not widely available. Adenovirally-transduced cells are cleared by the immune system. Although “gutted” adenovirus vectors lack this limitation, they are difficult to produce and are not readily available. Vectors based on herpes simplex virus are cytotoxic to most of the mesenchymal cells of the joint. Non-viral vectors provide only transient, low levels of transgene expression.
A number of studies confirm the ability of AAV to deliver genes to the joints of small animals in an appropriate fashion 49,52, especially when using self-complementing viruses that avoid the need for second strand DNA synthesis 53-55. Several laboratories have compared different serotypes of AAV for their ability to transduce articular tissues in vitro and in vivo, identifying serotypes 1, 2, 2.5, 5, 8 and 9 as interesting candidates 56-59.
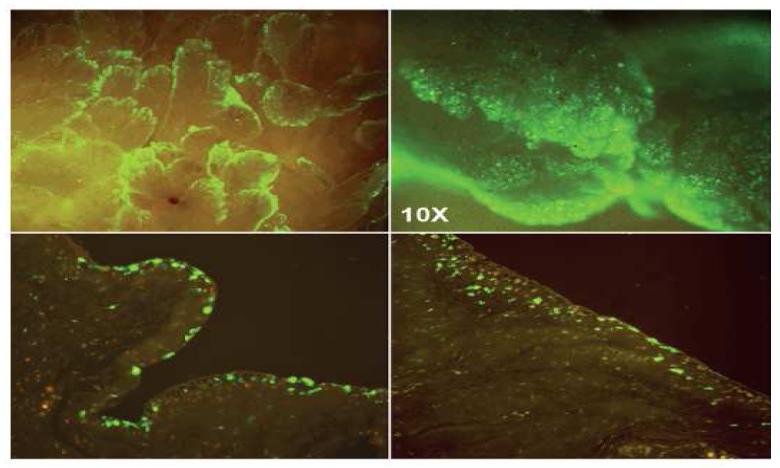
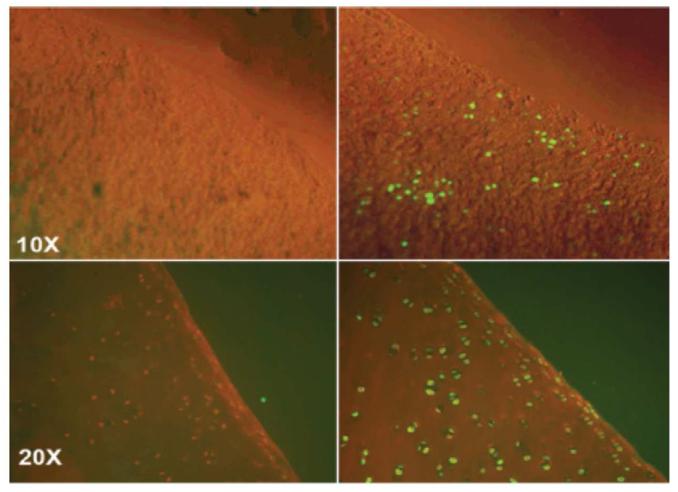
Only one study has investigated gene transfer in large animals with joints that are similar in size to human joints, and thus provide a more reliable indicator of what might occur in human clinical use. Watson et al 59 injected recombinant AAV.GFP into the midcarpal and metacarpophalangeal joints of horses. Fluorescence microscopy revealed impressive transduction of the synovial lining cells (figure 6) and chondrocytes, especially in areas of cartilage damaged by OA (figure 7). Transduction of chondrocytes by AAV was surprising as this had not been observed in the joints of small animals (e.g. figure 5), although the in vitro experiments of Madry et al. 60 suggested that this might be possible. It is of particular relevance to OA where the enhanced transduction of cells within cartilagenous lesions would bring many advantages.
Figure 6. Transgene expression in equine synovium following intraarticular injection of AAV.GFP.
Top two panels: Unprocessed tissue
Bottom two panels: Histological sections
From reference 59, with permission
Figure 7. Transgene expression in equine cartilage following intraarticular injection of AAV.GFP.
Left two panels: control cartilage
Right two panels: cartilage from joints injected with AAV.GFP
From reference 59, with permission
Because equine joints, unlike the joints of small animals, can be aspirated it was possible to gain an accurate measure of IL-1Ra in the synovial fluid; human IL-1Ra was used as the transgene, so it was possible to distinguish this product from endogenous equine IL-1Ra. Synovial fluid concentrations of 1-2 ng/ml were maintained for 5 weeks, after which an immune reaction to the human IL-1Ra eliminated expression 59. Based upon our accumulated experience with these types of experiments, a concentration in this range is predicted to be therapeutic. When the equine IL-1Ra cDNA was used, intraarticular expression was higher and persisted for many months (Ghivizzani et al. unpublished data).
Experience from human clinical trials suggests that immune reaction to AAV can be problematic 61. In agreement with such observations, intra-articular injection of AAV2 into the MCP joints of horses generated a persistent neutralizing antibody response to the vector 62 that would presumably interfere with re-dosing.
As well as providing confidence that these strategies will work in human joints, the equine studies form the basis for veterinary application in using AAV-based, in vivo gene therapy to treat equine OA and, by extension, OA in other domestic species.
Completed and pending clinical trials using AAV
rAAV2-TNFR:Fc (tgAAC94)
Etanercept is a TNF antagonist created by the fusion of two soluble TNF receptors to the Fc domain of immunoglobulin 63. As a recombinant protein, it is widely used to treat patients with RA and certain other inflammatory arthritides, such as psoriatic arthritis. It is delivered by sub-cutaneous self-injection twice per week. A cDNA encoding etanercept has been incorporated into AAV2 to form the vector rAAV2-TNFR:Fc (tgAAC94). Because of the size of etanercept cDNA, this is a single-stranded vector. It is intended to be used in individual symptomatic joints of patients receiving systemic treatment for RA, as well as individual joints suffering from other inflammatory conditions.
The AAV-etanercept vector showed efficacy in rat streptococcal cell wall-induced arthritis 64 and entered a Phase I study involving 14 subjects with RA and one with ankylosing spondylitis 65. Subjects were given a single injection of 1010 or 1011 virions/ml, with the volume depending on the joint; this ranged from 0.5ml for MCP joints to 5ml for knee joints. No adverse events were noted, leading to a Phase II study 66 involving over 100 patients with RA, as well as patients with ankylosing spondylitis and psoriatic arthritis, whose disease was not adequately controlled by standard therapy 67.
In the Phase II study the dose range was expanded to include 1012 and 1013 virions/ml, repeat dosing was allowed and, unlike the case in the Phase I study, concomitant treatment with conventional TNF blockers was also allowed. This study attracted considerable notoriety when a subject died shortly after receiving a second injection of the highest dose of the vector 68,69. The subject died with disseminated histoplasmosis accompanied by a massive retroperitoneal hematoma weighing at least 3.5 kg. Histoplasmosis is a known risk factor associated with the application of anti-TNFs and, controversially, the subject was taking adalimumab, an anti-TNF antibody, during the gene therapy trial. The FDA suspended the trial while these circumstances were investigated, but allowed the study to proceed to completion with minor changes to the consent form and protocol.
Apart from this fatality, which was concluded by the FDA not to be the result of AAV-mediated gene therapy, the trial did not encounter any severe adverse events directly related to the study. However, as with many such studies, there were minor injection site reactions. Viral genomes were not detected in the peripheral blood of subjects receiving the lowest dose of vector, but were detected in 46% of those receiving the middle dose and 61% of those receiving the highest dose. However, viral DNA was no longer detectable in peripheral blood cells after 12-18 weeks. No viral genomes were detected in a range of solid organs, including liver, brain, and heart, obtained at autopsy. Neutralizing antibodies to AAV2 were generated, but there was no evidence of a cell-mediated response. However, clinical responses were modest 67 and it is not clear if further development of this product will occur.
Sc-rAAV2.5IL-1Ra
As noted earlier in this review, our group is now focusing its attention on developing an in vivo gene therapy using recombinant, self-complementing (sc) AAV to deliver IL-1Ra cDNA to joints, with OA as the initial target disease.
Preclinical data in rabbits 53 and horses 59 confirm the ability of scAAV.IL-1Ra to generate therapeutic amounts of IL-1Ra intra-articularly. In horses, intra-articular IL-1Ra expression persists at an undiminished rate for at least several months when the cDNA encodes the equine product (Ghivizzani et al., unpublished), with high transgene expression in synovium and areas of damaged cartilage (figures 6 and 7). A Pre-IND meeting was held with the FDA in December, 2011 and a large pharmacology-toxicology-efficacy study is now underway in rats.
ART-I02 (AAV.IFN-β)
The Dutch company, Arthrogen BV, is developing AAV5 carrying cDNA encoding IFN-β, under the control of an inflammatioñ inducible promoter, as an intra-articular gene therapy for RA. Interest in IFN-β as a treatment for autoimmune diseases such as RA is generated by its immunomodulatory, anti-inflammatory and anti-angiogenic properties 70. When delivered systemically as a recombinant protein, it has shown efficacy in clinical trials for multiple sclerosis 71 but not RA 72. However, repeated application of IFN-β in mice 73 and monkeys 74 with collagen-induced arthritis was efficacious, suggesting that sustained delivery of this cytokine was necessary to produce a therapeutic effect in RA. Evidence in favor of this conclusion was obtained by the i.p. injection of fibroblasts that constitutively secreted IFN-β in rats with adjuvant arthritis, a model of human RA 75. The intra-articular injection of AAV5.IFN-β has also shown efficacy in rats with adjuvant arthritis 76.
Perspectives
Tables 1 and 2 list the arthritis clinical trials to date. For a field that is over 20 years old, the number of trials is modest. Moreover, as described in the preceding text, it is unlikely that the IND-approved products listed in Table 1 will be developed further; as far as we know, only 2 new human studies are in the pipeline.
Table 1. Clinical trials in the gene therapy of rheumatoid arthritis.
| Transgene | Method of delivery |
Phase | Institution or sponsor (principal investigator(s)) |
NIH OBA protocol number |
Number of subject |
Reference |
|---|---|---|---|---|---|---|
| IL-1Ra | Retrovirus, Ex Vivo |
I | University of Pittsburgh (Evans and Robbins) |
9406- 074 |
9 | 37 |
| IL-1Ra | Retrovirus Ex Vivo |
I | University of DŸsseldorf, Germany (Wehling) |
NA | 2 | 38 |
| Etanercept | AAV In Vivo | I | Targeted Genetics (Mease) |
0307- 588* |
15 | 61 |
| Etanercept | AAV In Vivo | I/II | Targeted Genetics (Mease) |
0503- 705** |
127 | 63 |
| INF-β | AAV In Vivo | Pre- Clinical |
Arthrogen (Tak) |
OBA: Office of biotechnology activities
NA: Not applicable
Included one subject with ankylosing spondylitis
Included subjects with ankylosing spondylitis and psoriatic arthritis
Adapted from reference 73
Table 2. Clinical trials in the gene therapy of osteoarthritis.
| Transgene | Vector Ex/In Vivo |
Phase | PI, Institution or Sponsor |
OBA Protocol Number |
Status | Number of subjects |
Ref. |
|---|---|---|---|---|---|---|---|
| TGF-β1 | Retrovirus Ex Vivo |
I | Ha, Kolon Life Sciences, Korea |
NA | Closed | 12 | 42 |
| TGF-β1 | Retrovirus Ex Vivo |
I | Mont TissueGene Inc |
0307-594 | Closed | 9 | |
| TGF-β1 | Retrovirus Ex Vivo |
IIa | Ha, Kolon Life Sciences, Korea |
NA | Closed | 28 | 43 |
| TGF-β1 | Retrovirus Ex Vivo |
II | Mont TissueGene Inc |
0912- 1016 |
Open | 100 | |
| IL-1Ra | AAV In Vivo |
I | Evans | Pre-IND |
Several factors account for this glacial rate of progress 10,77. Funding, of course, is an issue and the clinical translation of arthritis gene therapy is hampered by its lack of appeal to pharmaceutical companies who see long time-lines, questionable return on investment, and risk. Nevertheless, as noted in the acknowledgements to this review article, federal funding agencies have supported our research. But the sums of money now needed to perform the pre-clinical testing required to satisfy the demands of a successful IND application are enormous. Moreover, the regulatory barriers have become much more restrictive, as evidenced by our own experience. Our first gene therapy trial, using the retrovirus MFG-IRAP, took approximately 7 years from concept to injecting the first subject. We have been working on the next one, using AAV.IL-1Ra, for 9 years, and it is still at the Pre-IND stage.
Some optimism can be gained from recent progress in treating a number of genetic diseases by gene therapy. These include adrenal leukodystrophy, β-thalassemia, adenosine deaminase (ADA) deficiency, X-linked SCID, chronic granulomatous disease, Leber congential amaurosis, and lipoprotein lipase deficiency 78. Indeed, an AAV-based gene therapeutic for lipoprotein lipase deficiency has just received marketing approval by the European Medicines Agency as the drug Glybera. According to one newspaper report 79, this could cost as much as $1.6 million for the single injection necessary to confer lifetime therapy. Clearly, this pricing would not be appropriate for a disease as common as arthritis.
All of the above examples of success concern rare, Mendelian diseases. It is to be hoped that success in this domain will generate enthusiasm for using genes to treat common, non-genetic diseases like arthritis.
Acknowledgements
The authors’ work in this area has been funded by NIH grants R01 AR43623, R21 AR049606, R01 AR048566, R01 AR057422, R01 AR051085, X01 NS066865 and by Orthogen AG.
Potential conflicts of interest: CHE and PDR are on the Scientific Advisory Board of TissueGene Inc. PDR and SCG are among the co-founders of Molecular Orthopaedics Inc. All authors have read the journal’s policy on disclosure of potential conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nuesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Juni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011;342:d1165. doi: 10.1136/bmj.d1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim S. Changes in surgical loads and economic burden of hip and knee replacements in the US: 1997-2004. Arthritis Rheum. 2008;59(4):481–8. doi: 10.1002/art.23525. [DOI] [PubMed] [Google Scholar]
- 4.Kotlarz H, Gunnarsson CL, Fang H, Rizzo JA. Insurer and out-of-pocket costs of osteoarthritis in the US: evidence from national survey data. Arthritis Rheum. 2009;60(12):3546–53. doi: 10.1002/art.24984. [DOI] [PubMed] [Google Scholar]
- 5.Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 2008;58(1):15–25. doi: 10.1002/art.23177. [DOI] [PubMed] [Google Scholar]
- 6.Carmona L, Cross M, Williams B, Lassere M, March L. Rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2011;24(6):733–45. doi: 10.1016/j.berh.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Mandema JW, Salinger DH, Baumgartner SW, Gibbs MA. A dose-response meta-analysis for quantifying relative efficacy of biologics in rheumatoid arthritis. Clin Pharmacol Ther. 2011;90(6):828–35. doi: 10.1038/clpt.2011.256. [DOI] [PubMed] [Google Scholar]
- 8.Scott DL. Biologics-based therapy for the treatment of rheumatoid arthritis. Clin Pharmacol Ther. 2011;91(1):30–43. doi: 10.1038/clpt.2011.278. [DOI] [PubMed] [Google Scholar]
- 9.Evans CH, Kraus VB, Setton LA. Progress in intra-articular therapy. Nature Rev Rheumatol. 2013 doi: 10.1038/nrrheum.2013.159. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evans CH, Ghivizzani SC, Robbins PD. Getting arthritis gene therapy into the clinic. Nat Rev Rheumatol. 2010;7(4):244–9. doi: 10.1038/nrrheum.2010.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bandara G, Robbins PD, Georgescu HI, Mueller GM, Glorioso JC, Evans CH. Gene transfer to synoviocytes: prospects for gene treatment of arthritis. DNA Cell Biol. 1992;11(3):227–31. doi: 10.1089/dna.1992.11.227. [DOI] [PubMed] [Google Scholar]
- 12.McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365(23):2205–19. doi: 10.1056/NEJMra1004965. [DOI] [PubMed] [Google Scholar]
- 13.Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. 2010;376(9746):1094–108. doi: 10.1016/S0140-6736(10)60826-4. [DOI] [PubMed] [Google Scholar]
- 14.Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2010;7(1):33–42. doi: 10.1038/nrrheum.2010.196. [DOI] [PubMed] [Google Scholar]
- 15.Evans CH, Mazzocchi RA, Nelson DD, Rubash HE. Experimental arthritis induced by the intra-articular injection of allogeneic cartilagenous particles into rabbit knees. Arthritis Rheum. 1984;27:200–7. doi: 10.1002/art.1780270212. [DOI] [PubMed] [Google Scholar]
- 16.Boniface RJ, Cain PR, Evans CH. Articular responses to purified cartilage proteoglycans. Arthritis Rheum. 1988;31:258–66. doi: 10.1002/art.1780310214. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal AK. Crystals, inflammation, and osteoarthritis. Curr Opin Rheumatol. 2010;23(2):170–3. doi: 10.1097/BOR.0b013e3283432d1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guilak F, Fermor B, Keefe FJ, et al. The role of biomechanics and inflammation in cartilage injury and repair. Clin Orthop Relat Res. 2004;423:17–26. doi: 10.1097/01.blo.0000131233.83640.91. [DOI] [PubMed] [Google Scholar]
- 19.Troeberg L, Nagase H. Proteases involved in cartilage matrix degradation in osteoarthritis. Biochim Biophys Acta. 2011;1824(1):133–45. doi: 10.1016/j.bbapap.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldring MB. Update on the biology of the chondrocyte and new approaches to treating cartilage diseases. Best Pract Res Clin Rheumatol. 2006;20(5):1003–25. doi: 10.1016/j.berh.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Simkin PA. Synovial perfusion and synovial fluid solutes. Ann Rheum Dis. 1995;54(5):424–8. doi: 10.1136/ard.54.5.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wallis WJ, Simkin PA, Nelp WB. Protein traffic in human synovial effusions. Arthritis Rheum. 1987;30(1):57–63. doi: 10.1002/art.1780300108. [DOI] [PubMed] [Google Scholar]
- 23.Evans CH, Ghivizzani SC, Kang R, et al. Gene therapy for rheumatic diseases. Arthritis Rheum. 1999;42(1):1–16. doi: 10.1002/1529-0131(199901)42:1<1::AID-ANR1>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 24.Evans CH, Ghivizzani SC, Robbins PD. Gene therapy of the rheumatic diseases: 1998 to 2008. Arthritis Res Ther. 2009;11(1):209. doi: 10.1186/ar2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghivizzani SC, Gouze E, Gouze JN, et al. Perspectives on the use of gene therapy for chronic joint diseases. Curr Gene Ther. 2008;8(4):273–86. doi: 10.2174/156652308785160638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gouze E, Gouze JN, Palmer GD, Pilapil C, Evans CH, Ghivizzani SC. Transgene persistence and cell turnover in the diarthrodial joint: implications for gene therapy of chronic joint diseases. Mol Ther. 2007;15(6):1114–20. doi: 10.1038/sj.mt.6300151. [DOI] [PubMed] [Google Scholar]
- 27.Ghivizzani SC, Oligino TJ, Glorioso JC, Robbins PD, Evans CH. Direct gene delivery strategies for the treatment of rheumatoid arthritis. Drug Discov Today. 2001;6(5):259–67. doi: 10.1016/s1359-6446(01)01685-3. [DOI] [PubMed] [Google Scholar]
- 28.Hannum CH, Wilcox CJ, Arend WP, et al. Interleukin-1 receptor antagonist activity of a human interleukin-1 inhibitor. Nature. 1990;343(6256):336–40. doi: 10.1038/343336a0. [DOI] [PubMed] [Google Scholar]
- 29.Bandara G, Mueller GM, Galea-Lauri J, et al. Intraarticular expression of biologically active interleukin 1-receptor-antagonist protein by ex vivo gene transfer. Proc Natl Acad Sci U S A. 1993;90(22):10764–8. doi: 10.1073/pnas.90.22.10764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bakker AC, Joosten LA, Arntz OJ, et al. Prevention of murine collagen-induced arthritis in the knee and ipsilateral paw by local expression of human interleukin-1 receptor antagonist protein in the knee. Arthritis Rheum. 1997;40(5):893–900. doi: 10.1002/art.1780400517. [DOI] [PubMed] [Google Scholar]
- 31.Pelletier JP, Caron JP, Evans C, et al. In vivo suppression of early experimental osteoarthritis by interleukin-1 receptor antagonist using gene therapy. Arthritis Rheum. 1997;40(6):1012–9. doi: 10.1002/art.1780400604. [DOI] [PubMed] [Google Scholar]
- 32.Makarov SS, Olsen JC, Johnston WN, et al. Suppression of experimental arthritis by gene transfer of interleukin 1 receptor antagonist cDNA. Proc Natl Acad Sci U S A. 1996;93(1):402–6. doi: 10.1073/pnas.93.1.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boggs SS, Patrene KD, Mueller GM, Evans CH, Doughty LA, Robbins PD. Prolonged systemic expression of human IL-1 receptor antagonist (hIL-1ra) in mice reconstituted with hematopoietic cells transduced with a retrovirus carrying the hIL-1ra cDNA. Gene Ther. 1995;2(9):632–8. [PubMed] [Google Scholar]
- 34.Otani K, Nita I, Macaulay W, Georgescu HI, Robbins PD, Evans CH. Suppression of antigen-induced arthritis in rabbits by ex vivo gene therapy. J Immunol. 1996;156(9):3558–62. [PubMed] [Google Scholar]
- 35.Muller-Ladner U, Roberts CR, Franklin BN, et al. Human IL-1Ra gene transfer into human synovial fibroblasts is chondroprotective. J Immunol. 1997;158(7):3492–8. [PubMed] [Google Scholar]
- 36.Evans CH, Robbins PD, Ghivizzani SC, et al. Clinical trial to assess the safety, feasibility, and efficacy of transferring a potentially anti-arthritic cytokine gene to human joints with rheumatoid arthritis. Hum Gene Ther. 1996;7(10):1261–80. doi: 10.1089/hum.1996.7.10-1261. [DOI] [PubMed] [Google Scholar]
- 37.Evans CH, Robbins PD, Ghivizzani SC, et al. Gene transfer to human joints: progress toward a gene therapy of arthritis. Proc Natl Acad Sci U S A. 2005;102(24):8698–703. doi: 10.1073/pnas.0502854102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wehling P, Reinecke J, Baltzer AW, et al. Clinical responses to gene therapy in joints of two subjects with rheumatoid arthritis. Hum Gene Ther. 2009;20(2):97–101. doi: 10.1089/hum.2008.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hacein-Bey-Abina S, Von Kalle C, Schmidt M, et al. LMO2-associated clonal T cell proliferation in two patients after gene therapy for SCID-X1. Science. 2003;302(5644):415–9. doi: 10.1126/science.1088547. [DOI] [PubMed] [Google Scholar]
- 40.Lee DK, Choi KB, Oh IS, et al. Continuous transforming growth factor beta1 secretion by cell-mediated gene therapy maintains chondrocyte redifferentiation. Tissue Eng. 2005;11(1):2–310. doi: 10.1089/ten.2005.11.310. [DOI] [PubMed] [Google Scholar]
- 41.Noh MJ, Copeland RO, Yi Y, et al. Pre-clinical studies of retrovirally transduced human chondrocytes expressing transforming growth factor-beta-1 (TG-C) Cytotherapy. 2012;12(3):384–93. doi: 10.3109/14653240903470639. [DOI] [PubMed] [Google Scholar]
- 42.Ha CW, Noh MJ, Choi KB, Lee KH. Initial phase I safety of retrovirally transduced human chondrocytes expressing transforming growth factor-beta-1 in degenerative arthritis patients. Cytotherapy. 2012;14(2):247–56. doi: 10.3109/14653249.2011.629645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ha CW, Lee KH, Lee BS, et al. Efficacy of Tissuegene-C (TG-C), a cell mediated gene therapy, in patients with osteoarthritis: A phase IIa clinical study. J Tissue Eng Regen Med. 2012;6(suppl. 1):287. Abstract 48.05. [Google Scholar]
- 44.Nita I, Ghivizzani SC, Galea-Lauri J, et al. Direct gene delivery to synovium. An evaluation of potential vectors in vitro and in vivo. Arthritis Rheum. 1996;39(5):820–8. doi: 10.1002/art.1780390515. [DOI] [PubMed] [Google Scholar]
- 45.Roessler BJ, Allen ED, Wilson JM, Hartman JW, Davidson BL. Adenoviral-mediated gene transfer to rabbit synovium in vivo. J Clin Invest. 1993;92(2):1085–92. doi: 10.1172/JCI116614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oligino T, Ghivizzani S, Wolfe D, et al. Intra-articular delivery of a herpes simplex virus IL-1Ra gene vector reduces inflammation in a rabbit model of arthritis. Gene Ther. 1999;6(10):1713–20. doi: 10.1038/sj.gt.3301014. [DOI] [PubMed] [Google Scholar]
- 47.Ghivizzani SC, Lechman ER, Tio C, et al. Direct retrovirus-mediated gene transfer to the synovium of the rabbit knee: implications for arthritis gene therapy. Gene Ther. 1997;4(9):977–82. doi: 10.1038/sj.gt.3300486. [DOI] [PubMed] [Google Scholar]
- 48.Gouze E, Pawliuk R, Pilapil C, et al. In vivo gene delivery to synovium by lentiviral vectors. Mol Ther. 2002;5(4):397–404. doi: 10.1006/mthe.2002.0562. [DOI] [PubMed] [Google Scholar]
- 49.Goater J, Muller R, Kollias G, et al. Empirical advantages of adeno associated viral vectors in vivo gene therapy for arthritis. J Rheumatol. 2000;27(4):983–9. [PubMed] [Google Scholar]
- 50.Grieger JC, Samulski RJ. Adeno-associated virus vectorology, manufacturing, and clinical applications. Methods Enzymol. 2012;507:229–54. doi: 10.1016/B978-0-12-386509-0.00012-0. [DOI] [PubMed] [Google Scholar]
- 51.Gouze E, Pawliuk R, Gouze JN, et al. Lentiviral-mediated gene delivery to synovium: potent intra-articular expression with amplification by inflammation. Mol Ther. 2003;7(4):460–6. doi: 10.1016/s1525-0016(03)00024-8. [DOI] [PubMed] [Google Scholar]
- 52.Watanabe S, Imagawa T, Boivin GP, Gao G, Wilson JM, Hirsch R. Adeno-associated virus mediates long-term gene transfer and delivery of chondroprotective IL-4 to murine synovium. Mol Ther. 2000;2(2):147–52. doi: 10.1006/mthe.2000.0111. [DOI] [PubMed] [Google Scholar]
- 53.Kay JD, Gouze E, Oligino TJ, et al. Intra-articular gene delivery and expression of interleukin-1Ra mediated by self-complementary adeno-associated virus. J Gene Med. 2009;11(7):605–14. doi: 10.1002/jgm.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Payne KA, Lee HH, Haleem AM, et al. Single intra-articular injection of adeno-associated virus results in stable and controllable in vivo transgene expression in normal rat knees. Osteoarthritis Cartilage. 2011;19(8):1058–65. doi: 10.1016/j.joca.2011.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun J, Hakobyan N, Valentino LA, Feldman BL, Samulski RJ, Monahan PE. Intraarticular factor IX protein or gene replacement protects against development of hemophilic synovitis in the absence of circulating factor IX. Blood. 2008;112(12):4532–41. doi: 10.1182/blood-2008-01-131417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Apparailly F, Khoury M, Vervoordeldonk MJ, et al. Adeno-associated virus pseudotype 5 vector improves gene transfer in arthritic joints. Hum Gene Ther. 2005;16(4):426–34. doi: 10.1089/hum.2005.16.426. [DOI] [PubMed] [Google Scholar]
- 57.Boissier MC, Lemeiter D, Clavel C, et al. Synoviocyte infection with adeno-associated virus (AAV) is neutralized by human synovial fluid from arthritis patients and depends on AAV serotype. Hum Gene Ther. 2007;18(6):525–35. doi: 10.1089/hum.2006.174. [DOI] [PubMed] [Google Scholar]
- 58.Goodrich LR, Choi VW, Carbone BA, McIlwraith CW, Samulski RJ. Ex vivo serotype-specific transduction of equine joint tissue by self-complementary adeno-associated viral vectors. Hum Gene Ther. 2009;20(12):1697–702. doi: 10.1089/hum.2009.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Watson RS, Broome TA, Rice BL, et al. scAAV-mediated gene transfer of interleukin-1-receptor antagonist to synovium and articular cartilage in large mammalian joints. Gene Ther. 2012 doi: 10.1038/gt.2012.81. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Madry H, Cucchiarini M, Terwilliger EF, Trippel SB. Recombinant adeno-associated virus vectors efficiently and persistently transduce chondrocytes in normal and osteoarthritic human articular cartilage. Hum Gene Ther. 2003;14(4):393–402. doi: 10.1089/104303403321208998. [DOI] [PubMed] [Google Scholar]
- 61.Manno CS, Pierce GF, Arruda VR, et al. Successful transduction of liver in hemophilia by AAV-Factor IX and limitations imposed by the host immune response. Nat Med. 2006;12(3):342–7. doi: 10.1038/nm1358. [DOI] [PubMed] [Google Scholar]
- 62.Ishihara A, Bartlett JS, Bertone AL. Inflammation and immune response of intra-articular serotype 2 adeno-associated virus or adenovirus vectors in a large animal model. Arthritis. 2012:735472. doi: 10.1155/2012/735472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kerensky TA, Gottlieb AB, Yaniv S, Au SC. Etanercept: efficacy and safety for approved indications. Expert Opin Drug Saf. 2011;11(1):121–39. doi: 10.1517/14740338.2012.633509. [DOI] [PubMed] [Google Scholar]
- 64.Chan JM, Villarreal G, Jin WW, Stepan T, Burstein H, Wahl SM. Intraarticular gene transfer of TNFR:Fc suppresses experimental arthritis with reduced systemic distribution of the gene product. Mol Ther. 2002;6(6):727–36. doi: 10.1006/mthe.2002.0808. [DOI] [PubMed] [Google Scholar]
- 65.Mease PJ, Hobbs K, Chalmers A, et al. Local delivery of a recombinant adenoassociated vector containing a tumour necrosis factor alpha antagonist gene in inflammatory arthritis: a phase 1 dose-escalation safety and tolerability study. Ann Rheum Dis. 2009;68(8):1247–54. doi: 10.1136/ard.2008.089375. [DOI] [PubMed] [Google Scholar]
- 66.Evans C. Arthritis gene therapy trials reach phase II. J Rheumatol. 2010;37(4):683–5. doi: 10.3899/jrheum.100055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mease PJ, Wei N, Fudman EJ, et al. Safety, tolerability, and clinical outcomes after intraarticular injection of a recombinant adeno-associated vector containing a tumor necrosis factor antagonist gene: results of a phase 1/2 Study. J Rheumatol. 2010;37(4):692–703. doi: 10.3899/jrheum.090817. [DOI] [PubMed] [Google Scholar]
- 68.Evans CH, Ghivizzani SC, Robbins PD. Arthritis gene therapy’s first death. Arthritis Res Ther. 2008;10(3):110. doi: 10.1186/ar2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Frank KM, Hogarth DK, Miller JL, et al. Investigation of the cause of death in a gene-therapy trial. N Engl J Med. 2009;361(2):161–9. doi: 10.1056/NEJMoa0801066. [DOI] [PubMed] [Google Scholar]
- 70.Vervoordeldonk MJ, Aalbers CJ, Tak PP. Interferon beta for rheumatoid arthritis: new clothes for an old kid on the block. Ann Rheum Dis. 2009;68(2):157–8. doi: 10.1136/ard.2008.097899. [DOI] [PubMed] [Google Scholar]
- 71.PRISMS (Prevention of Relapses and Disability by Interferon beta-1a Subcutaneously in Multiple Sclerosis) Study Group Randomised double-blind placebo-controlled study of interferon beta-1a in relapsing/remitting multiple sclerosis. Lancet. 1998;352(9139):1498–504. [PubMed] [Google Scholar]
- 72.van Holten J, Pavelka K, Vencovsky J, et al. A multicentre, randomised, double blind, placebo controlled phase II study of subcutaneous interferon beta-1a in the treatment of patients with active rheumatoid arthritis. Ann Rheum Dis. 2005;64(1):64–9. doi: 10.1136/ard.2003.020347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Holten J, Reedquist K, van Roche P, et al. Treatment with recombinant interferon-beta reduces inflammation and slows cartilage destruction in the collagen-induced arthritis model of rheumatoid arthritis. Arthritis Res Ther. 2004;6(3):R239–49. doi: 10.1186/ar1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tak PP, Hart BA, Kraan MC, Jonker M, Smeets TJ, Breedveld FC. The effects of interferon beta treatment on arthritis. Rheumatology (Oxford) 1999;38(4):362–9. doi: 10.1093/rheumatology/38.4.362. [DOI] [PubMed] [Google Scholar]
- 75.Triantaphyllopoulos KA, Williams RO, Tailor H, Chernajovsky Y. Amelioration of collagen-induced arthritis and suppression of interferon-gamma, interleukin-12, and tumor necrosis factor alpha production by interferon-beta gene therapy. Arthritis Rheum. 1999;42(1):90–9. doi: 10.1002/1529-0131(199901)42:1<90::AID-ANR12>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 76.Adriaansen J, Fallaux FJ, de Cortie CJ, Vervoordeldonk MJ, Tak PP. Local delivery of beta interferon using an adeno-associated virus type 5 effectively inhibits adjuvant arthritis in rats. J Gen Virol. 2007;88(Pt 6):1717–21. doi: 10.1099/vir.0.82603-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Evans CH, Ghivizzani SC, Robbins PD. Orthopedic gene therapy--lost in translation? J Cell Physiol. 227(2):416–20. doi: 10.1002/jcp.23031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sheridan C. Gene therapy finds its niche. Nat Biotechnol. 2011;29(2):121–8. doi: 10.1038/nbt.1769. [DOI] [PubMed] [Google Scholar]
- 79.Whalen J. Gene-therapy approval marks major milestone. Wall Street Journal. 2012 Nov 3rd;2012:B3. [Google Scholar]