Abstract
The study examined joint trajectories of methamphetamine (MA) use and substance abuse treatment utilization and identified differences among pattern groups for a sample of 348 treated for MA use. Results from group-based trajectory modeling showed that treatment utilization during the first 10 years after initiation of MA use could be categorized into three distinctive patterns: about half the MA users have a pattern of low treatment utilization; one-fourth follow a quicker-to-treatment trajectory with higher probability of treatment during the first 5 years of MA use and less treatment in the next 5 years; and one-fourth have a slower-to-treatment trajectory with more treatment during the second half of the 10-year period. Four MA use patterns were identified: consistently low use, moderate, and high use, as well as a decreasing use pattern. Periods of greater likelihood of treatment participation were associated with periods of decreasing or lower frequency of MA use.
Keywords: Treatment patterns, Methamphetamine use patterns, Trajectories, Treatment success, Treatment resistance
1. Introduction
MA has been implicated in serious physical and psychiatric harms including violent behavior, psychosis (Darke et al., 2008), risk-taking, unprotected sex, multiple sex partners, and consequently HIV transmission (Colfax & Shoptaw, 2005). Epidemic increases in methamphetamine (MA) use/abuse in many parts of the United States were seen in the 1990s and early 2000s. For example, a national survey (NSDUH) showed that the number of MA users had tripled from 1995 to 2006 (Maxwell & Rutkowski, 2008). While there were decreases in many MA prevalence and consequence indicators mid-decade (2004-08), recent data suggest that decreases have subsided and increases are again being seen (e.g. Maxwell & Brecht, 2011; Substance Abuse and Mental Health Services Administration, 2012). For example, reported past month MA use increased 60% in the general population from 2008 to 2009 (SAMHSA, 2010); and, of the 10 Western and Mid-western states with the largest percentages of MA admissions to substance abuse treatment (reaching >20% of admissions), all experienced MA admission increases in 2010 and/or 2011 over 2009 levels (SAMHSA, 2012; Maxwell & Brecht, 2011).
MA use has not been restricted to the U.S. As many as 56 million individuals globally are estimated to be users of amphetamine-type substances (United Nations Office on Drugs and Crime [UNODC], 2011), ranking this group of drugs (of which MA is the primary example) as second in world-wide illicit drug use with MA identified as the primary illicit drug threat in Asia (UNODC, 2012). Although the treatment demand for MA varies geographically, the demand in East and Southeast Asia has increased considerably in the last decade from a quarter of treatment demand in 1998 to nearly half in 2009 (UNODC, 2011); and in 2009, MA was the primary drug of abuse among those treated for substance use in Brunei-Darussalam, Korea, and Philippines. In Thailand, 82% of those in substance abuse treatment indicated MA was their primary substance of abuse (UNDOC, 2011), with high rates of sexually transmitted infections among young adult MA users, for example, 24% testing positive for chlamydia and 6% for gonorrhea (Sutcliffe et al., 2009).
With the MA problem continuing, there is a need to better understand treatment utilization and MA use patterns in order to optimize intervention efforts and minimize morbidity and social consequences of MA abuse. Studies have shown that specific types of treatment can be effective in the short term for at least some MA users, especially with longer treatment retention and/or continuing care/self-help (e.g. Brecht, Greenwell, von Mayrhauser, & Anglin, 2006; Gonzalez et al., 2009; Hillhouse et al., 2007) and similar effects have also been documented in large treatment systems for “treatment-as-usual” (Brecht, Greenwell, & Anglin, 2005; Brecht & Urada, 2011). Hser, Huang, Chou, Teruya, & Anglin (2003) examined treatment effects on MA use over a 36 month period (24 months prior to and 12 months following a specific referent treatment episode), and reported that across the sample, being in treatment was associated with a decrease in MA use. However, the short-term nature of effectiveness of MA use treatment is emphasized in a recent study, which found residential treatment significantly reduced MA use frequency at three months, but by one and three years after treatment the vast majority of MA users who received treatment reported similar MA use levels as would be expected had they not received treatment or had only received detoxification (McKetin et al., 2012). Cross-sectional research indicates that overall, treatment utilization among MA users is low (Kenny, Harney, Lee, & Pennay, 2011), but we know little about how longer-term patterns of treatment utilization are associated with patterns of MA use, particularly for periods early in the MA use career.
The current analysis describes patterns of treatment utilization for MA users in conjunction with their patterns of MA use for a 10-year period following their MA use initiation. While previous research has described general long-term patterns of MA use (Brecht et al., 2008), the current study uses group-based trajectory modeling to examine MA use patterns in more detail and in conjunction with patterns of treatment utilization, as well as the relationship of patterns to specific individual and contextual characteristics.
2. Methods
2.1. Sample and Data
Data are from a study of the natural history of MA use and treatment outcomes, for a sample of clients admitted to treatment for MA use in publicly funded Los Angeles County treatment programs. A stratified random sample (by gender, ethnicity, and type of treatment [outpatient, residential]) of admission records was selected from the California Alcohol and Drug Data System (CADDS), primarily from 1996; this sampled treatment episode used for recruitment is termed the “index episode” for which shorter-term outcomes have been assessed in earlier studies (Brecht et al., 2006). Treatment programs attempted to locate these former clients to invite their participation in the study; 75% of the sampled admissions were located, and a 76% interview rate was achieved from those former clients. Study procedures are described in more detail in Brecht, O’Brien, von Mayrhauser, & Anglin, (2004) and von Mayrhauser, Brecht, & Anglin, (2002). The Institutional Review Board at the University of California, Los Angeles approved this study, and participants provided written informed consent.
Subjects were interviewed on two occasions, using the Natural History Interview (NHI) protocol (McGlothlin, Anglin, & Wilson, 1977; also see more recent examples of the NHI at http://www.caldar.org/html/natural-history.html). The first interview (n=350 valid interviews) occurred in 1999-2001, about three years after subjects were admitted to the index treatment episode. The follow-up interview was administered 2-4 years later (n=270), lengthening the drug use histories for the majority of the sample. The current analysis included 348 subjects with relevant data for this analysis.
One segment of the face-to-face NHI interview included questions on sociodemographic and other background factors, substance use, HIV/AIDS risk, criminal behaviors, and physical and mental health. The second segment collected detailed life-course data (retrospective) including use of selected substances and treatment utilization over time, beginning at age 14. Pattern reliability, as well as validity against the Addiction Severity Index, has been established (Anglin, Hser, & Chou, 1993; Chou, Hser, & Anglin, 1996; Hser, Anglin, & Chou, 1992; Murphy, Hser, Huang, Brecht, & Herbeck, 2010). The NHI procedure requires that the interviewer work closely with the respondent to structure the periods of interest, using corroborative information as memory aids (e.g., major life events, historical events). For each episode of behavior or type of event within a domain, the respondent answered several domain-specific questions. For example, for each episode of substance use treatment, the respondent indicated when the treatment episode occurred, general type(s)/modalities of treatment (e.g. residential, outpatient), and primary drug of abuse at admission. NHI data allow construction of a monthly time series history for each of the included domains and for each of five major substances. For example, if a respondent indicated that she had used MA daily from prison release until boyfriend left, this information was translated to a vector of data indicating 30 days/month use for each month within the specified time period.
The analysis sample was 56% male, 44% female; 47% non-Hispanic White, 16% Black, 30% Hispanic, and 6% other ethnicity; and 32% had educational level less than high school graduation. The average age at MA initiation was 19 years and at study interview, 32 years. (Other characteristics are described by trajectory group in Tables 1 and 2.)
Table 1.
Comparison of Treatment Utilization Trajectory Groups (First 10 years after MA initiation)
| Low Treatment (n=171) |
Slower to Treatment (n=82) |
Quicker to Treatment (n=95) |
|
|---|---|---|---|
| Background | |||
| Race/ethnicity, % Black | 14.0 | 12.2 | 24.2 |
| Male, % * | 60.8 | 42.7 | 59.0 |
| Education <high school, % | 26.9 | 35.4 | 36.8 |
| Sexual/physical abuse before age 15, % | 53.8 | 40.2 | 46.3 |
| Comorbid mental disorder, % | 20.5 | 14.6 | 20.0 |
| Arrest before age 18, % | 43.3 | 40.2 | 43.2 |
| Ever arrested, % | 96.5 | 92.9 | 89.5 |
| Ever incarcerated > 30 days, % | 60.2 | 60.0 | 57.9 |
| Any children during 1st 5 yrs of MA trajectory1, %*** | 31.6 | 58.5 | 52.6 |
| Drug Use | |||
| Age first MA use, Mean(SD)*** | 17.6 (4.5) | 20.6 (6.1) | 21.8 (6.7) |
| Initiated MA “for better sex,” % | 19.3 | 18.3 | 19.0 |
| Initiated MA “for fun,”% | 43.3 | 45.7 | 45.3 |
| Initiated MA use “to get high,” % | 51.5 | 51.2 | 46.3 |
| Ever used heroin, % | 22.2 | 20.7 | 19.0 |
| Ever used cocaine, %* | 73.1 | 60.0 | 60.0 |
| Injection drug use, % * | 53.2 | 45.1 | 35.8 |
| 3 or more MA-related problems, % | 35.1 | 36.6 | 44.7 |
| Early Drug Treatment (tx) | |||
| Years from MA initiation to 1st MA tx, Mean(SD)*** | 14.3(5.9) | 6.2(3.8) | 3.1 (3.7) |
| Age 1st MA tx, Mean(SD)*** | 31.1 (6.2) | 26.2 (5.9) | 24.5 (6.6) |
| No. mo. with tx (excl.self-help) in yrs 1-5 after MA initiation, Mean(SD)*** |
0.05 (0.3) | 2.3 (3.5) | 6.6 (6.4) |
| No. mo. with tx (excl.self-help) in yrs 6-10 after MA initiation, Mean(SD)*** |
0.9 (1.9) | 9.0 (6.7) | 0.7 (1.7) |
| No. mo. with self-help in yrs 1-5 after MA initiation, Mean(SD)*** |
0.9 (5.5) | 0.9 (3.5) | 4.2 (7.6) |
| No. mo. with self-help in yrs 6-10 after MA initiation, Mean(SD)*** |
1.3 (5.1) | 6.9 (10.9) | 4.3 (10.2) |
Any children born or still under 18 years of age during first 5 years of MA use; included fathering as well as bearing children.
Significant at p<.05
p<.01
p<.001
Table 2.
Comparison of Methamphetamine Use Trajectory Groups (First 10 years after MA initiation)
| Low MA Use (n=87) |
Moderate MA Use (n=105) |
Decreasing MA Use (n=89) |
High MA Use (n=67) |
|
|---|---|---|---|---|
| Background | ||||
| Race/ethnicity, % Black | 24.1 | 17.1 | 9.0 | 14.9 |
| Male, % ** | 69.0 | 60.0 | 46.1 | 46.3 |
| Education <high school, % | 26.4 | 29.5 | 37.1 | 34.3 |
| Sexual/physical abuse before age15, % ** | 51.7 | 48.6 | 34.8 | 62.7 |
| Comorbid mental disorder, % | 19.5 | 18.1 | 16.9 | 22.4 |
| Arrest before age 18, % | 41.4 | 42.9 | 40.5 | 46.3 |
| Ever arrested, % | 93.1 | 95.2 | 92.1 | 94.0 |
| Ever incarcerated > 30 days, % | 55.2 | 66.7 | 59.6 | 53.7 |
| Any children during 1st 5 yrs of MA traj1, % | 40.2 | 39.1 | 56.2 | 38.8 |
| Drug Use | ||||
| Age first MA use, Mean(SD)** | 20.3 (6.0) | 19.2 (5.7) | 20.4 (6.2) | 17.4 (4.9) |
| Initiated MA “for better sex,” % | 18.4 | 18.1 | 19.1 | 29.9 |
| Initiated MA “for fun,”% | 41.4 | 51.4 | 43.2 | 38.8 |
| Initiated MA use “to get high,” % | 46.0 | 51.4 | 53.9 | 47.8 |
| Ever used heroin, % | 25.3 | 21.0 | 16.9 | 20.9 |
| Ever used cocaine, % | 72.4 | 64.8 | 58.4 | 71.6 |
| Injection drug use, % | 42.5 | 49.5 | 40.5 | 55.2 |
| 3 or more MA-related problems, % | 30.2 | 37.1 | 49.4 | 34.3 |
| Early Drug Treatment (tx) | ||||
| Years from MA initiation to 1st MA tx, Mean(SD)*** | 9.8 (8.6) | 10.3 (6.3) | 6.4 (5.9) | 11.0 (5.9) |
| Age 1st MA tx, Mean(SD)* | 29.6 (7.8) | 28.6 (6.7) | 26.4 (6.2) | 27.6 (6.4) |
| No. mo. with tx (excl.self-help) in yrs 1-5 after MA initiation, Mean(SD)*** |
2.9 (4.5) | 1.9 (4.1) | 3.6 (6.1) | 0.7 (2.1) |
| No. mo. with tx (excl.self-help) in yrs 6-10 after MA initiation, Mean(SD)*** |
1.1 (3.1) | 2.0 (3.8) | 5.2 (6.8) | 2.7 (4.8) |
| No. mo. with self-help in yrs 1-5 after MA initiation, Mean(SD)*** |
3.4 (8.1) | 2.3 (7.2) | 0.7 (2.4) | 0.5 (2.7) |
| No. mo. with self-help in yrs 6-10 after MA initiation, Mean(SD)*** |
3.0 (8.3) | 2.2 (6.6) | 6.6 (12.2) | 1.6 (3.8) |
Any children born or still under 18 years of age during first 5 years of MA use; included fathering as well as bearing children.
Significant at p<.05
p<.01
p<.001
2.2. Measures
Two variables, treatment utilization and MA use, were examined in terms of their trajectories over time (that is, they were the dependent variables in the trajectory analysis). The monthly timelines derived from NHI interview data for these two variables for the first 10 years following MA initiation were summarized into 3-month periods (quarters) to facilitate analysis. Thus, each individual had two vectors of time-ordered data (up to 40 quarterly data points beginning with the month of MA initiation) to be used for pattern identification. MA use during a quarter was considered as the average across the 3 months of the number of days per month with MA use. A study participant was considered as utilizing treatment during a quarter if he/she reported any type of formal treatment participation (not including 12-step or other self-help) for any number of days during that quarter. While respondents reported general type/modality of treatment (e.g. residential, outpatient), the current analysis did not include this level of detail because of potential complexity with some treatment episodes and time periods encompassing multiple types of treatment which is beyond the scope of this paper to assess. (For more information about treatment utilization by modality in publicly-funded California treatment programs, see Rawson, Gonzales, Brecht, Crevecoeur-MacPhail, & Hemberg, 2008). Data were not collected on specific therapeutic approaches since this often is not transparent to the client in many “treatment-as-usual” community-based treatment programs.
Other variables (further described below) were selected from the following three domains to be included in comparisons of the identified trajectory groups: background and potential vulnerability characteristics, MA use and other drug history, and treatment characteristics. Variables from these domains were selected to represent characteristics related in previous studies to drug trajectories or treatment outcomes (e.g. Hser, Huang, Brecht, Li, & Evans, 2008; Brecht, Greenwell, & Anglin, 2005; Brecht, Greenwell, von Mayrhauser, & Anglin, 2006; Gonzalez et al., 2009; Hillhouse et al., 2007; McKetin et al., 2012), as well as for their potential utility in characterizing which trajectory groups might warrant specialized attention and to validate trajectory groupings. Interview responses for these variables were sometimes collapsed or categorized to binary indicators to facilitate the current analysis (while retaining specificity accounting for relationships to MA use found in previous analyses from this study), because of small category sizes, extreme skewness, or lack of relevant differences among certain categories.
Background characteristics included gender, ethnicity, educational level, and potential vulnerabilities. Several categories of self-reported ethnicity (including Hispanic, non-Hispanic White, and other/multi-racial) were collapsed resulting in a binary variable, Black vs. all other ethnicities. Criminal history was represented by three indicators: reported number of arrests and number of arrests before age 18 were collapsed (because of extreme skewness) to binary variables (ever arrested vs. never arrested and ever arrested before age 18 vs. not arrested before age 18); and respondents indicated (no/yes) whether they had ever been incarcerated for a period of more than 30 days. Note that the NHI captured only major periods of incarceration (>30 days), not shorter periods. To assess childhood (occurring before age 15) physical and/or sexual trauma, respondents were asked whether anyone has “ever physically abused you, that is hit or beaten you so hard that you had cuts or bruises, had to stay in bed or had to see a doctor” and whether “anyone ever forced or pressured you to do any sexual acts against your will”; a single variable was created indicating a yes to either or both vs. no to both. To assess comorbid mental disorder, respondents were asked whether they had “ever been diagnosed by a psychiatrist as having schizophrenia, depression, mania or bipolar disorder,” resulting in a single binary no/yes indicator. Also included was a binary indicator of whether the respondent had a child who was under 18 during the early period (first five years) of MA use, calculated from the respondent’s age at interview and of MA initiation and the reported ages of his/her children; this included bearing or fathering a child, so applied to both gender respondents.
Drug use history included age of MA initiation, any past use of heroin or cocaine (no/yes), and any injection drug use (no/yes). To assess motivation for MA initiation, respondents were asked “why did you start using meth?” and could answer no/yes to any/all of 11 specific reasons that applied to them; three of these reasons that might be most challenging for treatment were included in the current analysis: for fun, to get high, for better sex. For example, those who use the drug “for better sex” may find it particularly difficult to stop using the drug without learning new/different sexual behaviors, emotions, perceptions, and lifestyle. Perceived severe negative impact of MA use was indicated (no/yes) by whether respondents reported that their MA use had resulted in (all three) paranoia, hallucinations, and violent behavior. This variable was created from a question to which respondents could answer no/yes to each of 12 specific potential problems or side effects of MA (“did your meth use result in any of the following?”); for this analysis, we selected three of the most severe problems, that might contribute to co-occurring disorders found to be associated with treatment and drug use careers in other studies (e.g. Dennis et al., 2005; Hser et al. 2007).
Treatment characteristics included latency (in years) from first MA use to first treatment for MA use (calculated from NHI timeline data), age at admission to the first MA treatment episode, and total number of months during each of two early stages of MA use (years 1-5 and 6-10 after initiation) with participation in treatment (excluding self-help) and participation in self-help.
2.3. Analysis
There are two parts to the analysis addressed: first, the identification of trajectory groups illustrating patterns of MA use and treatment utilization and, second, the comparison of these identified groups on the selected background, substance use, and treatment-related variables.
In the first part of the analysis, group-based trajectory modeling was used to identify distinctive patterns of treatment utilization and MA use over time (Nagin, 2005; Jones, Nagin & Roeder, 2001; Nagin & Odgers, 2010; see also, Xie, McHugo, He, and Drake, 2010, or Charnigo, Kryscio, Bardo, Lynam, & Zimmerman, 2011, for additional non-mathematical explanations of this approach). This approach partitions subjects into latent classes determined by differences in their trajectory patterns, thus allowing different groups (each with its own growth trajectory) to capture the overall variation over time. This method can provide more detail on trajectories as contrasted with growth model or time series regression approaches which estimate a single average pattern across individuals, with variation considered as random error or captured as random effects around the pattern parameters.
The first stage of the group-based trajectory analysis modeled treatment utilization and MA use patterns separately in unconditional models (that is, modeling treatment utilization as a function of time with no additional covariates or predictors and then following the same procedure for MA use) to determine the complexity of polynomial growth parameters to represent the trajectories (e.g. linear and/or quadratic and/or cubic, etc.) and the optimal number of trajectory groups to account for variability in patterns across individuals. For each variable (treatment utilization and MA use), the analysis considered an increasing number of groups (2, 3, etc.), and models were refined for parsimony by omitting non-significant higher-order pattern parameters. For MA use, analyses used a censored normal model, and results suggested that pattern parameters should include linear, quadratic, and cubic terms. For treatment utilization, a logistic model was used with linear and quadratic terms. The number of groups was selected by comparing models on a combination of a model-fit statistic (BIC adjusted for number of subjects), the interpretability of trajectories and unique information contributed by adding groups, and group size (Nagin & Odgers, 2010; Xie et al., 2010). A 3-group solution was selected for treatment and a 4-group solution for MA use. Note that the approach allows missing data (which was minimal): 75% of the sample had complete data vectors for the 10-year period (40 quarters), and the remainder had valid data for an average of 37.8 quarters.
In the second stage of the group-based trajectory analysis, we re-estimated trajectory groups using a joint model for treatment utilization and MA use trajectories and using the functional form for the optimal number of groups as found in the first stage univariate analysis. Again, these models were not conditional on any other variables or covariates. As a sensitivity analysis, differing numbers of trajectory groups were also examined in the joint model and compared using the adjusted BIC with results similar to the univariate models in the first stage of analysis. From the final joint model, for each individual an estimated probability of membership in each latent trajectory group was calculated by the group-based trajectory procedures, based on how well his/her pattern was represented by the identified trajectory group pattern; and the individual was assigned membership in the trajectory group with the highest probability. Probabilities of assigned group membership (entropy) were .88-.96 for treatment utilization trajectory groups and .96-.99 for MA use groups. Probabilities for non-assigned groups were very low, ranging from <.001 to .05 (that is, for individuals belonging to a trajectory group to which they were not assigned). The high (near 1.0) entropy and low (near zero) probabilities of non-assigned groups indicated that the identified trajectories were successful in representing differences among individuals’ trajectories. Results in this paper are from the joint estimation.
Three sets of probabilities were examined from the joint trajectories: MA use trajectory conditional on treatment trajectory (that is, for a specified treatment trajectory group, what are the probabilities of also being in each of the MA use trajectory groups), treatment conditional on MA use, and the probabilities of joint membership across the 12 unique combinations of treatment utilization and MA use groups. Selected combinations of the joint groups were compared using chi square or ANOVA.
In the second part of the analysis, treatment utilization and MA use trajectory groups (that is, subgroups of MA users with the different types of trajectories found in the first part of the analysis) were compared on the selected background, drug use, and treatment-related characteristics using chi-square or ANOVA. This allowed examination of whether these individual characteristics were associated with the different trajectories of treatment utilization and MA use. Note that these additional variables used in comparisons do not define the trajectory groups, but represent characteristics on which groups (defined by their differential patterns of treatment utilization and/or MA use over time) may differ.
3. Results
3.1. Patterns of Treatment
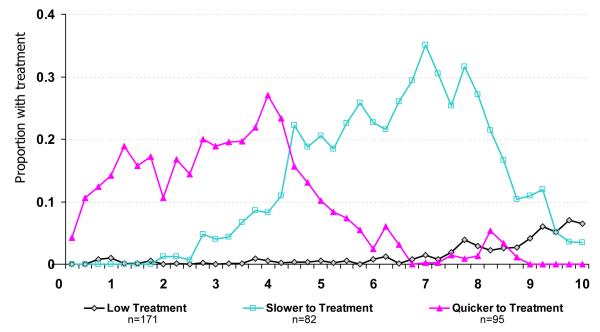
Three general types of distinctive patterns emerged for treatment utilization during the first 10 years after MA initiation (Figure 1). One group of MA users (49.1% of the sample assigned to this group based on observed data) showed a generally “Low Treatment” utilization pattern across the entire period. A second group (27.3% of the sample) showed a pattern of treatment utilization with higher rates of treatment utilization during the first five years and treatment utilization tapering off during the next five years (labeled “Quicker-to-Treatment” for this paper). A third trajectory group (23.6% of the sample) showed a pattern of generally low (but gradually increasing) rates of treatment utilization during the first five years of MA use and substantially higher rates of treatment utilization during the second half of the 10-year period (labeled “Slower-to-Treatment”).
Figure 1.
Trajectories of Treatment Participation During First 10 Years of Methamphetamine Use (graph indicates percentage of trajectory group with any AOD treatment during each 3-month period)
3.2. Characteristics of Treatment Utilization Groups
Comparing the three treatment trajectory groups on background characteristics, we found that the groups differed significantly on gender composition, with the Slower-to-Treatment group having the smallest percentage of males (42.7% vs. 59.0- 60.8% males in the other two groups) and most likely (58.5%) to report having any children under 18 years during this early MA use period. (See Table 1.) The groups did not differ significantly on other background characteristics used in comparisons. In terms of drug use characteristics, the groups differed in their mean age of MA initiation with the Quicker-to-Treatment the oldest at 21.8 years and Low Treatment group the youngest at initiation at 18.3 years. The Low Treatment group was also most likely to have used cocaine/crack (73.1% vs. 60.0% for the other groups) and to have ever injected drugs (53.2% vs. 35.8-45.1% for the other groups).
Considering treatment characteristics, results confirmed the trajectory identification in several ways. As expected, the Quicker-to-Treatment group showed the most number of months in treatment during the first 5 years of MA use (average of 6.6 months), and the Slower-to-Treatment group had the most months in treatment during years 6-10 (9.0). Self-help participation followed the same pattern; note also that the Quicker-to-Treatment group also maintained its average self-help participation during years 6-10. The Low Treatment group was the oldest at first treatment (not including self-help) specifically for MA (31.1 years),the longest time from MA initiation to their first MA treatment (14.3 years), and, as would be expected from pattern characteristics, had the lowest treatment and self-help participation in both the years 1-5 and 6-10 periods.
3.3. Patterns of MA Use
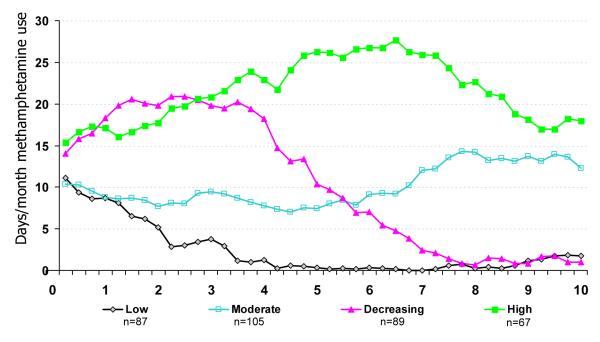
Four MA use trajectories were identified: Low, Moderate, Decreasing, and High use trajectories. (See Figure 2.) The group of MA users with the Low use pattern (25.0% of the sample) generally initiated MA use at a moderate frequency (at an average of about 10 days per month) that declined to very low levels by five years after initiation. The Moderate use group (30.2%) initiated and maintained MA use at a moderate frequency level throughout the 10-year period. The Decreasing use group (25.6%) and the High use group (19.3%) started MA use at slightly higher frequency (closer to 15 days per month on average) and experienced early increases in their frequency of use. The Decreasing group peaked in their MA use during years 2-4 and then decreased to low levels of use, while the High group continued to increase to nearly daily use until about year 7 and then decreased somewhat.
Figure 2.
Trajectories of Methamphetamine Use During First 10 Years of Methamphetamine Use (graph indicates days per month of use averaged across months during each 3-month period)
3.4. Characteristics of MA Trajectory Groups
On background characteristics, MA use groups differed in terms of gender with the Low and Moderate MA use group more predominantly male (69.0% and 60.0%, respectively vs. 46.1% for Decreasing and 46.3% High groups). The Decreasing group had the lowest rates of early sexual/physical abuse (34.6%), while the High use group had the highest rate (62.7%). Only one drug use characteristic, age of first MA use, distinguished the MA trajectory groups. The High use group was, on average, the youngest at MA initiation (17.4 years vs. 19-20 for other groups).
MA trajectory groups differed significantly on several drug treatment-related characteristics. The Decreasing group had the shortest latency between first MA use and first MA treatment (6.4 years compared to 10-11 for other groups), was the youngest at admission to first MA treatment (age 26.4 vs. 28-30 for other groups), and had the highest number of months of treatment (excluding self-help) in both years 1-5 and 6-10 periods (3.6 months and 5.2 months, respectively). The High use group was characterized by the longest latency from first MA use to first MA treatment (11.0 years) and the shortest number of months in self-help (0.5 months) or treatment (0.7 months) during their first 5 years of MA use and for self-help (1.6 months) during years 6-10.
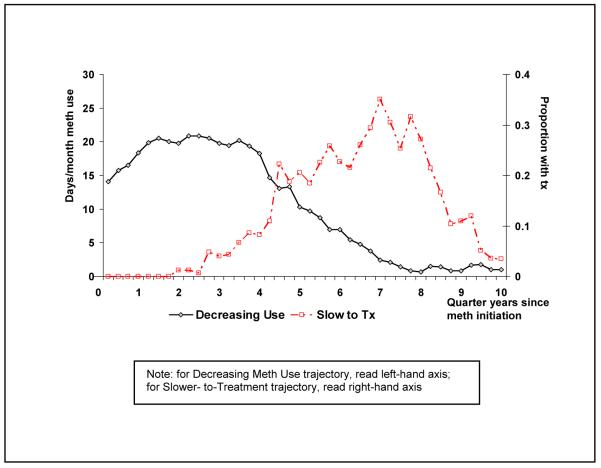
3.5. Association of Treatment Patterns to MA Use Patterns: Conditional and Joint Probabilities
Results showed that the Quicker-to-Treatment utilization pattern was associated with a pattern of early decrease in MA use followed by continuing low levels of use (the Low MA use trajectory group), with a conditional probability of 43.7% (see Table 3.A). The Slower-to-Treatment utilization pattern was most frequently associated with a pattern (the Decreasing MA use group) of initially high levels of MA use with decreases in MA use during the periods of greater treatment utilization, with a conditional probability of 56.5%. Figure 3 illustrates the pattern crossover at about five years into MA use. The Low Treatment utilization group was associated with MA use patterns that maintained consistency over time (Low, Moderate, High), and most specifically with continuing Moderate levels of MA use, with 40.7% of the Low Treatment utilization group in the Moderate MA use group (as compared to an overall 30.5% of the sample in the Moderate MA use group) or with continued High levels of MA use (27.9%, as compared to an overall 19.1% of the sample in the High MA use group).
Table 3.
Conditional and Joint Probabilities of Treatment Utilization and Methamphetamine Use Trajectory Groups
| MA Use Trajectory Group | ||||
|---|---|---|---|---|
|
| ||||
| Low | Moderate | Decreasing | High | |
| Treatment Utilization Trajectory Group | ||||
| 3.A. Probability of MA Use Group Conditional on Treatment Group 1 | ||||
| Low | 23.2 | 40.7 | 8.2 | 27.9 |
| Slower-to-tx | 8.0 | 17.9 | 56.5 | 17.5 |
| Quicker-to-tx | 43.7 | 22.0 | 30.1 | 4.2 |
|
| ||||
| 3.B. Probability of Treatment Group Conditional on MA Use Group 2 | ||||
| Low | 45.7 | 66.7 | 16.1 | 72.8 |
| Slower-to-tx | 7.4 | 13.7 | 51.7 | 21.3 |
| Quicker-to-tx | 46.9 | 19.6 | 32.3 | 6.0 |
|
| ||||
| 3.C. Joint Probability of Treatment and MA Use Group 3 | ||||
| Low | 11.5 | 20.3 | 4.1 | 13.9 |
| Slower-to-tx | 1.9 | 4.2 | 13.1 | 4.1 |
| Quicker-to-tx | 11.8 | 6.0 | 8.2 | 1.1 |
rows add to 100%
columns add to 100%
all entries add to 100%
Figure 3.
Intersection of Slower-to-Treatment and Decreasing Meth Use Trajectories
From the alternative perspective, considering probabilities of treatment trajectory conditional on MA use pattern as shown in Table 3.B, Low MA use was associated with both Low (45.7%) and Quicker-to-Treatment trajectories (46.9%); Moderate MA use was associated with a Low Treatment trajectory (66.7%); Decreasing MA use was associated with a Slower–to-Treatment trajectory (51.7 %); and High MA use was associated with a Low Treatment trajectory (72.8%). Note also that the subgroup with the combination of Low Treatment utilization and continued Moderate MA use comprises 20.3% of the sample, the largest subgroup of the 12 combinations of 3 treatment utilization and 4 MA use trajectory groups (Table 3.C).
3.6 Comparison of Selected Joint Groups
For further comparison of joint trajectory groups, we focused on four joint combinations of potential interest in planning and evaluating prevention and intervention strategies. A “Treatment Avoidant” group comprised those with continuing Moderate or High MA use but with Low Treatment utilization (34.2%; sum of percentages of 20.3 and 13.9 from Table 3.C). An “Early Success” group comprised those who were Quicker-to-Treatment and who managed to keep MA use at Low levels (11.8%). A “Treatment Failure” group comprised those who continued at Moderate or High MA use even while utilizing treatment in the Quicker or Slower-to-Treatment patterns (15.4%). A fourth combination (“Later Success”) was those who, while Slower with their treatment utilization, showed a concomitant Decrease in MA use (13.1%).
As shown in Table 4, the Treatment Failure group was more likely than were other groups to have been arrested as juveniles (55.6%) or have a history of injection drug use (55.6%). The Treatment Avoidant group also had high rates of injection drug use (50.0%), were younger age at first MA use (17.8 years), had the longest latency from MA initiation to first treatment (averaging 13.0 years), and, concordantly, the oldest age at first MA treatment (30.0 years). As would be expected from the pattern description, they also had very low number of months participating in treatment and also with almost no self-help participation. This Treatment Avoidant group was also least likely to have had any children during their early MA trajectory, possibly because of their younger age at initiation. The Early Success group was characterized by being the oldest at MA initiation (average 22.5 years), least likely to have drug injection history (30.0%), and had the most number of months of treatment (6.4 months) or self-help (4.2 months) early in their MA use careers and continued their level of self-help participation in yrs 6-10. The Later Success group was characterized by the highest rate of being parents with children during the first 5 years of MA use (61.7%), lowest rate of early criminal history (29.8%), and highest number of months in treatment (9.2 months) and self-help (9.6 months) in MA use years 6-10.
Table 4.
Comparison of Selected Joint (Treatment Utilization and Methamphetamine Use) Trajectory Groups@ (only characteristics differing at p<.10 shown in table)
| “Treatment Avoidant” Low Tx + Mod/High MA Use (n=118) |
“Early Success” Quick to Tx + Low MA Use (n=70) |
“Treatment Failure” Slow/Quick to Tx + Mod/High MA Use (n=54) |
“Later Success” Slow to Tx + Decrease MA Use (n=47) |
|
|---|---|---|---|---|
| Background | ||||
| Race/ethnicity, % Black ** | 14.4 | 27.1 | 20.4 | 4.3 |
| Arrest before age 18, % * | 39.0 | 35.7 | 55.6 | 29.8 |
| Any children during 5-yr MA traj1, % ** | 33.9 | 52.9 | 50.0 | 61.7 |
| Drug Use | ||||
| Age first MA use, Mean(SD)*** | 17.8 (4.8) | 22.5 (6.7) | 20.1 (6.5) | 20.3 (5.9) |
| Injection drug use, % ** | 50.0 | 30.0 | 55.6 | 36.2 |
| Early Drug Treatment (tx) | ||||
| Years from MA initiation to 1st MA tx, Mean(SD)*** |
13.0 (5.2) | 3.2 (4.0) | 5.3 (4.4) | 5.5 (3.2) |
| Age 1st MA tx, Mean (SD)*** | 30.0 (5.8) | 25.2 (6.4) | 24.4 (6.6) | 25.7 (5.7) |
| No. mo. with tx (excl.self-help) in yrs 1-5 after MA initiation, Mean(SD)*** |
0.01 (0.1) | 6.4 (6.8) | 4.5 (5.0) | 2.1 (3.2) |
| No. mo. with tx (excl.self-help) in yrs 6-10 after MA initiation, Mean(SD)*** |
1.1 (2.1) | 0.6 (1.5) | 4.9 (6.1) | 9.2 (7.2) |
| No. mo. with self-help in yrs 1-5 after MA initiation, Mean(SD)*** |
0.8 (5.8) | 4.2 (8.1) | 3.2 (6.0) | 0.1 (0.7) |
| No. mo. with self-help in yrs 6-10 after MA initiation, Mean(SD)*** |
0.9 (3.0) | 4.1 (9.9) | 4.2 (8.7) | 9.6 (13.0) |
Any children born or still under 18 years of age during first 5 years of MA use; included fathering as well as bearing children.
Significant at p<.05
p<.01
p<.001
note that 59 subjects were not included in this comparison because they were members of the remaining 4 of the joint groupings which did not conceptually fit into the categories compared.
4. Discussion
Study findings indicate a diversity of both treatment and MA use patterns for this sample. While for some purposes, average patterns and relationships are an important and easily interpretable summary (e.g. Brecht, Huang, Evans, & Hser, 2008; Hser, Huang, Chou, Teruya, & Anglin, 2003), more specificity about the differential patterns and related user characteristics may stimulate further development of early intervention and continuing care approaches. Treatment utilization patterns for MA users in the first 10 years after MA use initiation could be categorized into three distinctive trajectories, with about half receiving a consistently Low level of treatment over ten years, about one-fourth following a Quicker-to-Treatment trajectory with greater levels of treatment utilization during the first five years of MA use, and the remaining one-fourth with a Slower-to-Treatment trajectory. The Quicker-to-Treatment group exhibited the relationship found by Dennis et al. (2005) that those older at drug use initiation also have a shorter latency before starting treatment. They also were least likely to inject drugs. The Low Treatment group, which began MA use at an earlier age and were more likely to have used cocaine and injected drugs, poses a particular challenge for intervention efforts.
Considering MA use patterns, results indicated that subgroups of MA users exhibit quite distinctive patterns during their first 10 years of use, including relatively consistent Low, Moderate, or High levels of use across the period, as well as a Decreasing pattern. Patterns for MA users differed somewhat from those found for heroin and other drug users; for example, treated heroin users did not exhibit distinctively Low or Moderate patterns during the first 10 years of use in studies by Grella and Lovinger (2011) or Hser, Huang, Chou, & Anglin (2007). For MA users, females were a majority in both the Decreasing and High use groups, but the High use group was distinguishable as particularly vulnerable in terms of highest rates of sexual/physical abuse. The younger age of MA initiation in the High group is generally consistent with Grella and Lovinger (2011) findings for heroin users. Other background characteristics did not distinguish the pattern groups, differing, e.g., from the Dennis et al. (2005) study which found that co-occurring disorders were associated with continuing substance use (in a sample not including MA users), but similar to Grella & Lovinger (2011) or Hser et al. (2007) studies which found few or inconsistent other background predictors of higher use patterns among heroin users.
Consideration of joint patterns of treatment utilization and MA use provides additional detail on trajectories and characteristics. For example, in the Slower-to-Treatment group, MA use clearly decreased during the period of increasing treatment utilization (generally consistent with findings e.g., from Hser, Huang, Chou, Teruya, & Anglin, 2003). Earlier intervention through a variety of referrals might be able to move the trajectory crossover point closer to MA initiation. A study examining the timing of substance abuse treatment indicates that participating in more treatment episodes early in the course of drug use is associated with reduced risk of mortality (Scott, Dennis, Laudet, Funk, & Simeone, 2011). Another study examining drug use patterns over 10 years found occurrence of first treatment during young adulthood was not associated with patterns of reduced drug use, however receipt of more drug treatment over time was associated with maintenance of a low level of drug use among those first treated as young adults but not among those first treated as older adults (Evans, Li, Grella, Brecht, & Hser, in press). Taken together with our findings, it appears that higher levels of treatment early in the course of MA use and starting in younger versus older adulthood may be critical to attenuating moderate/high MA use trajectories.
Early intervention and assertive outreach may benefit MA users generally, as the majority of our sample could be categorized as receiving a low level of treatment over ten years; but there is a substantial need for early intervention specifically among those who used MA at consistently elevated levels while receiving little treatment (with this joint Treatment Avoidant subgroup comprising one-third of this sample overall). These individuals may be distinguishable from other users in that they initiated MA use at an earlier age, were less likely to have children during their first 5 year of MA use, and were more likely to have engaged in injection drug use. Likewise, those for whom treatment participation was associated with continuing high levels of MA use (the Treatment Failure group) may warrant specialized intervention in conjunction with the criminal justice system; they were distinguished by highest levels of early arrest and injection drug use.
4.1 Limitations and Further Analysis
Treatment utilization data for pattern identification were simplified for analysis to a no/yes indicator for any self-reported treatment participation (excluding self-help) in a given 3- month quarter year; additional analyses should examine whether a more detailed measure of treatment participation (e.g., number of months or weeks during quarters) would produce similar pattern groups. Treatment data were not available to the level of detail of therapeutic approach or number or type of sessions per day (e.g. individual counseling, group sessions, etc.). Also note that data for this analysis were self-reported treatment utilization; future analyses should attempt to replicate these analysis with treatment episode trajectories from actual treatment records. Note that recruitment procedures gave a (random) sample that reflects a snapshot of MA users treated in community-based programs in Los Angeles County during the mid-1990s. While this process captured users with a diversity of treatment, MA use, and personal histories, results may not be generalizable to other user populations (e.g. those recruited from first-time-only treatment admissions or from a specialty treatment protocol, with specific past history durations of use and/or abstinence, or from other geographic areas). Caution is suggested in comparing our results directly to more typical treatment outcome studies. While our results are generally consistent with several cited studies, our analysis has not focused on predictors of outcomes of a single treatment episode, rather on characteristics related to identified longitudinal patterns of MA use and treatment utilization. In addition, future analyses should examine 1) the relationship of treatment trajectories (including timing and frequency of treatment) and additional continuing care and/or self-help to later treatment outcomes including long-term abstinence; 2) the relationship of these trajectories to patterns of use of other drugs, particularly cocaine/crack; and 3) longer trajectories.
5. Conclusions and Implications
Results generally support a relationship between trajectories of treatment utilization with those of MA use, complementing findings from earlier treatment outcome studies (e.g. Hser, Huang, Chou, Teruya, & Anglin, 2003). But our findings also provide more detail about how subgroups of MA users exhibit substantially different patterns over time. While the retrospective design does not allow a causal assessment, results should stimulate discussion about earlier and specifically targeted intervention programs. More specifically, we found that periods of greater treatment utilization were associated with periods of lower frequency of MA use, even within the first 10 years of MA use. Of particular concern are MA users who continue to use MA at moderate or high levels through this 10-year period and have little treatment utilization. These users warrant attention for specialized intervention, and are likely to include individuals who initiate MA use at earlier ages, use cocaine/crack, and inject drugs. Those who are slower to utilize treatment and could potentially benefit from earlier intervention efforts also warrant special attention; this group includes a higher percentage of women and individuals with children. Such efforts might include brief interventions in routine health care contacts, prenatal care, or in venues for parent education; and treatment opportunities should be expanded to better accommodate parenting individuals. Results showing that the treatment failure group was characterized by high rates of arrest before age 18 identify a need for development of more efficacious adolescent treatment and prevention approaches to be linked with the juvenile justice system. Results also suggest that there is a group of MA users who benefited from treatment utilization during their first 5 years after initiation, resulting in considerably decreased MA use. Many long-term consequences of MA use might be minimized if earlier intervention with the Slower-to-Treatment group could hasten decreases in their MA use trajectories; examination of turning points might be helpful in identifying potential related factors.
Acknowledgements
This research was supported by grants from the National Institute on Drug Abuse (R01- DA11020, R01-DA025113, P30-DA016383) and contract 02-06-08 from the California Department of Alcohol and Drug Programs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anglin MD, Hser Y-I, Chou C-P. Reliability and validity of retrospective behavioral self-report by narcotics addicts. Evaluation Review. 1993;17:91–108. [Google Scholar]
- Brecht M-L, Greenwell L, Anglin MD. Methamphetamine treatment: trends and predictors of retention and completion in a large state treatment system (1992-2002) Journal of Substance Abuse Treatment. 2005;29:295–306. doi: 10.1016/j.jsat.2005.08.012. [DOI] [PubMed] [Google Scholar]
- Brecht M-L, Greenwell L, von Mayrhauser C, Anglin MD. Two year outcomes of treatment for methamphetamine use. Journal of Psychoactive Drugs. 2006;38(SARC Suppl 3):415–426. doi: 10.1080/02791072.2006.10400605. [DOI] [PubMed] [Google Scholar]
- Brecht M-L, Huang D, Evans E, Hser Y-I. Polydrug use and implications for longitudinal research: The-year trajectories for heroin, cocaine, and methamphetamine users. Drug & Alcohol Dependence. 2008;96:193–201. doi: 10.1016/j.drugalcdep.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brecht M-L, O’Brien A, von Mayrhauser C, Anglin MD. Methamphetamine use behaviors and gender differences. Addictive Behaviors. 2004;29(1):89–106. doi: 10.1016/s0306-4603(03)00082-0. [DOI] [PubMed] [Google Scholar]
- Brecht M-L, Urada D. Treatment Outcomes for Methamphetamine Users: California Proposition 36 and Comparison Clients. Journal of Psychoactive Drugs. 2011;43:68–76. doi: 10.1080/02791072.2011.602279. [DOI] [PubMed] [Google Scholar]
- Charnigo R, Kryscio R, Bardo M, Lynam D, Zimmerman R. Joint modeling of longitudinal data in multiple behavioral change. Evaluation and the Health Professions. 2011;34:181–200. doi: 10.1177/0163278710392982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou C-P, Hser Y-I, Anglin MD. Pattern reliability of narcotics addicts’ self-reported data: A confirmatory assessment of construct validity and consistency. Substance Use & Misuse. 1996;31:1189–1216. doi: 10.3109/10826089609063972. [DOI] [PubMed] [Google Scholar]
- Colfax, Shoptaw S. The methamphetamine epidemic: implications for HIV prevention and treatment. Current HIV/AIDS Reports. 2005;2:194–99. doi: 10.1007/s11904-005-0016-4. [DOI] [PubMed] [Google Scholar]
- Darke S, Kaye S, McKetin R, Duflou J. Major physical and psychological harms of methamphetamine use. Drug and Alcohol Review. 2008;27:253–62. doi: 10.1080/09595230801923702. [DOI] [PubMed] [Google Scholar]
- Dennis M, Scott C, Funk R, Foss M. The duration and correlates of addiction and treatment careers. Journal of Substance Abuse Treatment. 2005;28:S51–S62. doi: 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Evans E, Li L, Grella C, Brecht M-L, Hser Y-I. Developmental timing of first drug treatment and 10-year patterns of drug use. Journal of Substance Abuse Treatment (in press) 2012 doi: 10.1016/j.jsat.2012.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales R, Ang A, Marinelli-Casey P, Glik D, Iguchi M, Rawson R. Health-related quality of life trajectories of methamphetamine-dependent individuals as a function of treatment completion and continued care over a 1-year period. Journal of Substance Abuse Treatment. 2009;37:353–361. doi: 10.1016/j.jsat.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Grella C, Lovinger K. 30-year trajectories of heroin and other drug use among men and women sampled from methadone treatment in California. Drug & Alcohol Dependence. 2011;118:251–258. doi: 10.1016/j.drugalcdep.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillhouse M, Marinelli-Casey P, Gonzales R, Ang A, Rawson R, Methamphetamine Treatment Project Corporate Authors Predicting in-treatment performance and post-treatment outcomes in methamphetamine users. Addiction. 2007;102(Suppl 1):84–95. doi: 10.1111/j.1360-0443.2007.01768.x. [DOI] [PubMed] [Google Scholar]
- Hser Y-I, Anglin MD, Chou C-P. Reliability of retrospective self-report by narcotics addicts. Psychological Assessment. 1992;4:207–213. [Google Scholar]
- Hser Y-I, Huang D, Chou C-P, Teruya C, Anglin MD. Longitudinal patterns of treatment utilization and outcomes among methamphetamine abusers: a growth curve modeling approach. Journal of Drug Issues. 2007;33:921–938. [Google Scholar]
- Hser Y-I, Huang D, Chou C-P, Anglin MD. Trajectories of heroin addiction: Growth mixture modeling results based on a 33-year follow-up study. Evaluation Review. 2007;31:548–563. doi: 10.1177/0193841X07307315. [DOI] [PubMed] [Google Scholar]
- Hser Y-I, Huang D, Brecht M-L, Li L, Evans E. Contrasting trajectories of heroin, cocaine, and methamphetamine use. Journal of Addictive Diseases. 2008;27:13–21. doi: 10.1080/10550880802122554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser Y-I, Huang D, Chou C-P, Teruya C, Anglin MD. Longitudinal patterns of treatment utilization and outcomes among methamphetamine abusers: a growth curve modeling approach. Journal of Drug Issues. 2003;33:921–938. [Google Scholar]
- Jones B, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29:374–393. [Google Scholar]
- Kenny P, Harney A, Lee NK, Pennay A. Treatment utilization and barriers to treatment: Results of a survey of dependent methamphetamine users. Substance Abuse Treatment, Prevention, and Policy. 2011;6:1–7. doi: 10.1186/1747-597X-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlothlin WH, Anglin MD, Wilson BD. A follow-up of admissions to the California Civil Addict Program. American Journal of Drug and Alcohol Abuse. 1977;4:179–199. doi: 10.3109/00952997709002759. [DOI] [PubMed] [Google Scholar]
- Maxwell J, Brecht M-L. Methamphetamine: here we go again? Addictive Behaviors. 2011;36:1168–73. doi: 10.1016/j.addbeh.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell J, Rutkowski B. The prevalence of methamphetamine and amphetamine abuse in North America: a review of the indicators, 1992-2007. Drug and Alcohol Review. 2008;27:229–235. doi: 10.1080/09595230801919460. [DOI] [PubMed] [Google Scholar]
- McKetin R, Najman JM, Baker A, Lubman DI, Dawe S, Ali R, et al. Evaluating the impact of community-based treatment options on methamphetamine use: findings from the Methamphetamine Treatment Evaluation Study (MATES) Addiction (in press) 2012 doi: 10.1111/j.1360-0443.2012.03933.x. [DOI] [PubMed] [Google Scholar]
- Murphy D, Hser Y-I, Huang D, Brecht M-L, Herbeck D. Self-report of longitudinal substance use: comparison of the UCLA Natural History Interview and the Addiction Severity Index. Journal of Drug Issues. 2010;40:495–516. doi: 10.1177/002204261004000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin D. Group-based modeling of development. Harvard Univ. Press; Cambridge, MA: 2005. [Google Scholar]
- Nagin D, Odgers C. Group-based trajectory modeling in clinical research. Annual Review of Clinical Psychology. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- Rawson R, Gonzales R, Brecht M-L, Crevecoeur-MacPhail D, Hemberg J. Evaluation of the California Outcomes Measurement System (CalOMS) Final Report 2008. UCLA Integrated Substance Abuse Programs; Los Angeles: 2008. Available at http://www.adp.ca.gov/oara/doc/CalOMS_Final_Report_2008. [Google Scholar]; docScott CK, Dennis ML, Laudet A, Funk RR, Simeone RS. Surviving drug addiction: The effect of treatment and abstinence on mortality. American Journal of Public Health. 2011;101:737–744. doi: 10.2105/AJPH.2010.197038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott C, Dennis M, Laudet A, Funk R, Simeone R. Surviving drug addiction: the effect of treatment and abstinence on mortality. American Journal of Public Health. 2011;101:737–744. doi: 10.2105/AJPH.2010.197038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Sutcliff e C, Srirojn B, Latkin CA, Aramratanna A, Celentano DD. Evaluation of a peer network intervention trial among young methamphetamine users in Chiang Mai, Thailand. Soc Sci Med. 2009;68:69–79. doi: 10.1016/j.socscimed.2008.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMHSA] Office of Applied Studies [accessed 7/20/12];Treatment Episode Data Set–data for states. 2012 available on-line at http://wwwdasis.samhsa.gov/webt/newmapv1.htm.
- Substance Abuse and Mental Health Services Administration [SAMHSA] Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. SAMHSA; Rockville, MD: 2010. (Office of Applied Studies, NSDUH Series H-38A, HHS Publication No. SMA 10-4856Findings) [Google Scholar]
- Sutcliffe C, Aramrattana A, Sherman S, Sirirojn B, German D, Wongworapat K, Quan V, Keawvichit R, Celentano D. Incidence of HIV and sexually transmitted infections and risk factors for acquisition among young methamphetamine users in northern Thailand. Sexually Transmitted Diseases. 2009;36:284–289. doi: 10.1097/OLQ.0b013e318191ba17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime [accessed 10/2/12];World Drug Report, Global Illicit Drug Trends. 2011 Available at http://www.unodc.org/unodc/en/data-and-analysis/WDR.html.
- United Nations Office on Drugs and Crime [accessed 10/4/12];World Drug Report, 2012. 2012 Available at http://www.unodc.org/unodc/en/data-and-analysis/WDR-2012.html.
- von Mayrhauser C, Brecht M-L, Anglin MD. Use ecology and drug use motivations of methamphetamine users admitted substance abuse treatment facilities in Los Angeles: An emerging profile. Journal of Addictive Diseases. 2002;21:45–60. doi: 10.1300/j069v21n01_05. [DOI] [PubMed] [Google Scholar]
- Xie H, McHugo G, He X, Drake R. Using the group-based dual trajectory model to analyze two related longitudinal outcomes. Journal of Drug Issues. 2010;40:45–62. [Google Scholar]