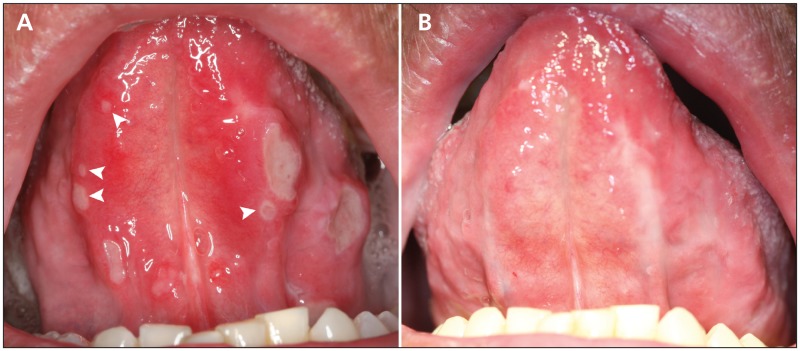
A 44-year-old man with cutaneous T-cell lymphoma presented with an 18-month history of recurrent painful oral ulcers that predated the lymphoma diagnosis. Examination revealed ulcers on the ventral surface of his tongue (Figure 1A). The clinical appearance and histopathologic features of the ulcers were consistent with aphthous stomatitis. Topical and intralesional corticosteroid therapy proved ineffective, but treatment with systemic pentoxifylline resulted in substantial resolution of the ulcers within one month (Figure 1B). The patient continues to take pentoxifylline for recurrent ulceration.
Figure 1:
(A) Multiple symptomatic minor and major aphthous ulcers on the lateral and ventral surfaces of the patient’s tongue. The arrows indicate the aphthous ulcers that have a classic clinical appearance. (B) Substantial resolution of the ulcers was seen after one month of pentoxifylline treatment
Recurrent aphthous stomatitis is a common oral condition, often beginning in childhood, that affects up to 25% of the general population.1 Minor aphthous stomatitis is the most common form, affecting 80% of patients with aphthous stomatitis, and consists of ulcers of less than 1 cm in diameter that heal within two weeks without scarring.1–3 Major aphthous stomatitis is defined as ulcers greater than 1 cm that are present for more than two weeks and often heal with scarring.1–3 The etiopathogenesis of this condition remains unclear and is often multifactorial.1–3 Typically, it is observed clinically on nonkeratinized oral mucosa as round ulcers covered by a white or yellow pseudomembrane with an erythematous halo.2,3 According to expert opinion, additional diagnostic testing may be warranted if patients present with increasing severity of disease as they get older, the clinical appearance of the lesions is atypical, or if underlying systemic diseases, such as inflammatory bowel disease, systemic vasculitis and HIV infection, are to be ruled out.3
Treatment is determined by frequency, distribution and severity of symptoms.1,3 Based on expert opinion and limited data from randomized clinical trials, topical high-potency corticosteroids are used as initial therapy, while systemic medications, such as pentoxifylline, have shown effectiveness in managing recalcitrant cases.1–3 Patients taking systemic medications must be closely monitored for possible adverse effects.1,3
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
References
- 1.Scully C. Aphthous ulceration. N Engl J Med 2006;355:165–72 [DOI] [PubMed] [Google Scholar]
- 2.Chattopadhyay A, Shetty KV. Recurrent aphthous stomatitis. Otolaryngol Clin North Am 2011;44:79–88 [DOI] [PubMed] [Google Scholar]
- 3.Messadi DV, Younai F. Aphthous ulcers. Dermatol Ther 2010; 23:281–90 [DOI] [PubMed] [Google Scholar]