Abstract
Aims
To assess age variation in correlates of drinking cessation.
Design
Prospective study of a U.S. general population sample.
Setting
Face-to-face household interviews.
Participants
Past-year ≥monthly drinkers interviewed at baseline and 3-year follow-up (n=14,885).
Measurements
Baseline values and selected changes over follow-up in alcohol consumption, alcohol use disorder (AUD), sociodemographic and health characteristics, other substance use and psychiatric comorbidity were used to predict drinking cessation in three age groups.
Findings
Correlates of drinking cessation varied over the life course, with pregnancy/presence of an infant, nicotine or drug use disorder, incident AUD, cluster A personality disorder, liver disease and incident retirement being important at younger ages and high-school graduation, family income ≥$70,000, volume of ethanol intake, Asian race/ethnicity, mood disorder and incident cardiovascular disease being significant at older ages. Age-invariant correlates included smoking cessation over follow-up, OR=2.82 (95% CI=1.62–4.92) to 3.45 (2.20–5.39); college education, OR=0.42 (0.27–0.65) to 0.54 (0.36–0.83); Black and Hispanic race/ethnicity, OR = 1.74 (1.18–2.29) to 1.88 (1.21–2.93) and 1.58 (1.11–1.25) to 1.73 (0.83–3.63), respectively, and months since last drink, OR=1.24 (1.13–1.36) to1.29 (1.19–1.39).
Conclusions
Factors associated with ceasing alcohol use in US adults appear to differ over the life course, reflecting age variation in both their prevalence and impact and supporting the importance of role transitions and health problems (the “sick quitter” effect). The most consistent correlates of drinking cessation included factors reflecting ability/inability to give up potentially addictive substances and factors associated with perceived acceptability of drinking and subgroup-specific drinking contexts that might facilitate/impede continued drinking.
Keywords: drinking cessation, former drinkers, sick quitters
INTRODUCTION
Former drinkers are often thought to be “sick quitters” who, if combined with lifetime abstainers, may yield a reference group that distorts the apparent health consequences associated with different drinking levels [1–3]. Prospective studies distinguishing former drinkers and lifetime abstainers have tended to support the “sick quitter” hypothesis, generally showing higher health risks among former drinkers than lifetime abstainers or light drinkers [4–7]. Despite the importance of understanding drinking cessation for interpreting alcohol-related health risks, few studies have characterized former drinkers or prospectively identified correlates of drinking cessation in the general population. Most studies of drinking changes have examined limited subpopulations, including adolescents and young adults, the middle-aged and/or elderly, and individuals with alcohol dependence/drinking problems.
Studies of drinking trajectories from adolescence to early/mid-adulthood have implicated sociodemographic factors and other substance use in drinking changes, showing transitions out of heavy episodic drinking (HED) to be more common among women [8,9], nonwhites [8,10–11], nonsmokers [10,12] and individuals who get and/or remain married [11,13–16], have college educations [10,17,18] and with negative family histories of alcoholism or whose parents did not drink heavily [9,10,19]. In contrast, studies of middle-aged and elderly populations have more consistently implicated health problems as predictors of drinking reduction/cessation [20–26], although sociodemographic factors [22–25], smoking [22,24,27], depression [22,27], religiosity [22] and retirement [20,27] also have demonstrated associations with decreased consumption. In prospective, population-based studies of individuals with alcohol dependence or drinking problems, drinking reduction/cessation has been positively associated with nonwhite race-ethnicity [28–30], presence of young children in the home [28], religiosity/spirituality [28,30], some types of alcohol treatment [28,29,31] and severity of alcohol problems [22,29,32] and negatively associated with male sex [29,32] and income [29].
In a study of the total adult population, former drinkers had more chronic conditions and poorer physical and psychological functioning than current drinkers or lifelong abstainers and higher rates of smoking and depression than light-to-moderate drinkers [33]. Pooled data from the 2004 and 2007 Australian National Drug Strategy Household Surveys indicated that former drinkers were more likely to report their overall health status as poor and to have diagnosed diabetes and heart disease than current drinkers [34]. Two studies based on a nine-year follow-up of Dutch adults found that getting married and becoming a parent were associated with decreased volume of consumption and frequency of HED; among women only, marital disruption was associated with an increase in HED [35]. However, these transitions were significant and in the expected direction only when they occurred at young ages. Role transitions more commonly occurring at older ages, retirement and widowhood, were not significantly associated with consumption changes among older respondents [36].
A comparison of individuals who stopped and continued drinking in a longitudinal sample of U.S. adults interviewed in 1971–74 and 1982–84 found that those who stopped drinking were older, more likely to be nonwhite and to be unemployed and had less education than those who continued drinking. Among women only, they also were less likely to be current smokers [37]. Individuals drinking less than 12 drinks per year were treated as nondrinkers in the survey upon which this analysis was based, the National Health and Nutrition Examination Survey (NHANES). In another study based on three waves of NHANES data, smoking cessation and getting married were associated with a reduction in HED [38].
In summary, identifying factors associated with drinking cessation is complicated by several issues. First, many existing studies have focused on selected age ranges. Although comparisons across studies yield an approximate picture of how correlates of drinking cessation vary across age, these comparisons are confounded by differences among samples and in the range of potential correlates examined, i.e., in level of adjustment. Second, many prospective studies of drinking changes have examined reduction in drinking volume or HED as the outcome or have combined drinking reduction and cessation. Given differences between abstainers and light drinkers [33] and the importance of distinguishing them for understanding the impact of “sick quitters” on mortality and morbidity risk curves [3], it is important to examine drinking cessation apart from reduced consumption.
The following study was designed to address these issues. Using data from a nationally representative longitudinal sample of U.S. adults large enough to address age variation for a broad range of drinking cessation correlates, it compared drinkers who continued and stopped drinking over a three-year follow-up interval. Correlates common across age, unique to specific ages or whose effects sizes varied by age were ascertained in separate models for individuals 18–34, 35–54 and ≥55 years of age at baseline and by testing age interactions in a single model for all ages combined. Based on available evidence, we hypothesized that transitions reflecting adoption of adult roles would diminish in importance with age, whereas the impact of physical illness as a drinking deterrent would increase with age. Because the meaning and significance of drinking cessation are ambiguous for infrequent drinkers, i.e., difficult to distinguish from a slightly longer than usual interval between drinks, we restricted our analyses to individuals who drank alcohol at least once a month during the year preceding baseline, hereinafter referred to as regular drinkers.
METHODS
Sample
This study used data from Waves 1 and 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The nationally representative 2001–2002 Wave 1 sample contained 43,093 U.S. adults 18 and older living in households and noninstitutional group quarters (response rate = 81.0%). The 2004–2005 Wave 2 follow-up sample comprised 34,653 of the original respondents, 86.7% of those eligible for reinterview (cumulative response rate = 70.2%). Detailed information on the sample design and weighting is available elsewhere [39–41]. Informed consent was obtained after potential respondents were informed in writing about the nature of the survey, uses of the survey data, voluntary nature of participation and confidentiality of identifiable survey information. The research protocol received full ethical review and approval. This study is based on a subsample of respondents who participated in both waves of the NESARC and consumed alcohol at least once a month in the year preceding the Wave 1 interview (n=14,885).
Measures
Drinking cessation
Drinking cessation was coded as positive if respondents had consumed alcohol at least once a month in the year preceding the Wave 1 interview but did not consume any alcohol in the year preceding the Wave 2 interview.
Baseline covariates
In addition to age and sex, baseline sociodemographic characteristics included marital status (married/cohabiting, widowed, divorced/separated, never married), educational attainment (<high school, high school graduate, attended/completed college), past-year pregnancy or presence of a natural/adoptive/step/foster child ≤1 year of age, activity status (coded hierarchically from multiple-choice items as employed, unemployed, retired, student, homemaker), family income (<$35,000, $35000–69,999, ≥$70,000) and major financial problems (unemployed and seeking employment for ≥one month or major financial crisis/bankruptcy/unable to pay bills on time).
In addition to self-perceived general health (good/fair/poor versus excellent/very good), the specific past-year medical conditions of liver disease (cirrhosis or other), hypertension, cardiovascular disease (CVD, i.e., arteriosclerosis, angina pectoris, tachycardia, myocardial infarction or other) and gastric disease (gastritis/peptic ulcer) were derived from a list of chronic and acute conditions for which respondents had to report confirmation by a health professional. Past-year mood disorder and anxiety disorder conformed to DSM-IV [42] criteria, as did lifetime Cluster A (odd/eccentric), B (dramatic/emotional/erratic) and C (anxious/fearful) personality disorders (PD). The derivation, reliability and validity of these diagnoses have been described elsewhere [43–47].
Past-year tobacco use comprised any of five types of tobacco, distinguishing users with and without DSM-IV nicotine dependence [44–45]; past-year drug use comprised illicit use of any of 10 types of drugs, distinguishing use with and without DSM-IV drug use disorder [46–49]. Past-year volume of ethanol intake [50] equaled the larger of four beverage-specific volumes summed or the independently-ascertained volume for all beverage types combined. Interval since first drink was the difference between ages at baseline and first drink (not counting sips). Interval since last drink and frequency of drinking 5+ drinks in a single day were asked directly.
Individuals were classified with an alcohol use disorder (AUD) if they satisfied ≥1 of the DSM-IV criteria for alcohol abuse or ≥3 of the DSM-IV alcohol dependence criteria [49,51] within a common one-year time frame. AUD history comprised no history of AUD; former AUD with a full stable remission (≥3 years since offset of all symptoms), former AUD with a recent/partial remission (<3 years since offset of all symptoms or residual, subclinical past-year symptoms), and past-year AUD (continuing and new cases). Alcohol treatment comprised any of 12 sources of assistance that were queried with respondents who reported ever going anywhere to get help for their drinking problems.
Follow-up interval covariates
New cases of hypertension, CVD, liver and gastric disease comprised those coded positive at Wave 2 but negative at Wave 1. Other events occurring over follow-up included having a child, becoming widowed, getting divorced or separated, and retiring. In addition, we included incident AUD whose onset occurred over follow-up but before the year preceding the Wave 2 interview and smoking cessation, coded positive for individuals who were smokers at baseline but not during the year preceding Wave 2.
Analysis
We used chi-square and t-tests of differences in means and proportions to compare characteristics of individuals who stopped and continued drinking within three age groups: 18–34, 35–54 and ≥55. Differences across age groups were assessed using Cochran-Mantel-Haenszel tests and linear regression models testing interactions between drinking cessation and age group. Multivariate associations were estimated in logistic regression models predicting drinking cessation for each age group. We entered covariates in four blocks: baseline sociodemographic/health factors; other substance use and psychiatric disorders; alcohol use, AUD and treatment; and events occurring during follow-up. Each block was manually reduced to exclude correlates with p-values >.10 before adding the next block. The final reduced models retained covariates with p-values <.05 or whose inclusion was required to maintain the proper referent for multicategorical variables. To test whether odds ratios (ORs) varied across age groups, we estimated a logistic regression model for all age groups combined that assessed interactions of each covariate with age. As a sensitivity analysis to see whether the inclusion of a covariate for smoking cessation over follow-up might have mediated the effects of other covariates potentially associated in similar ways with smoking and drinking cessation, we re-estimated the age-stratified models with smoking cessation omitted.
Statistical analyses employed SUDAAN software to obtain variance estimates that accounted for complex, multi-stage sample designs [52]. Exact p-values are shown in all tables. Because of the multiple bivariate associations tested, a p-value of <.005 was required for citing as statistically significant; in multivariate analyses, covariates and age interactions were cited as significant at a p-value of <.05.
RESULTS
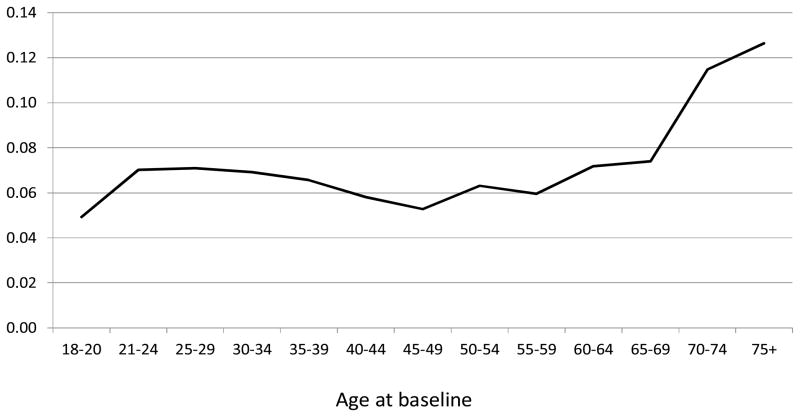
The rate of drinking cessation over follow-up increased from 4.9% among those 18–20 years of age to 12.6% of those 75 years of age and older at baseline (Figure 1), with the sharpest increases at ages <21 and ≥65. Rates of drinking cessation were considerably lower for the regular drinkers examined in this study than for baseline infrequent drinkers (data not shown), among whom they varied from 12.0% to 40.8%.
Figure 1.
Proportion of baseline regular drinkers who stopped drinking over a 3-year follow-up interval, by age at baseline
Whites, individuals with high levels of education and income, and individuals with current AUD or stable remission of former AUD were underrepresented among those who stopped drinking in all age groups (Table 1), and individuals who stopped drinking had longer intervals since last drink at baseline. Other characteristics, e.g., age, main activity, financial problems, good/fair/poor health, interval since first drink, volume of ethanol intake, incident divorce/separation, incident AUD and smoking cessation over follow-up, demonstrated significant (p<.005) associations within limited age groups. Most of these characteristics, in addition to race-ethnicity, marital status, education, income, Cluster A PD and AUD history, demonstrated significant (p<.005) differences in their associations with drinking cessation across age groups.
Table 1.
Selected characteristics of baseline past-year drinkers who stopped and continued drinking over a 3-year follow-up interval, by age at baseline: U.S. regular drinkers 18 and older at Wave 1
| Ages 18–34 | Ages 35–54 | Ages 55+ | p-value effect variation by age | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stopped | Continued | p | Stopped | Continued | p | Stopped | Continued | p | |||
| Baseline past-year characteristics: | |||||||||||
| Mean age | 26.5 (0.3) | 26.2 (0.1) | .455 | 43.9 (0.3) | 44.0 (0.1) | .720 | 68.8 (0.6) | 65.7 (0.2) | .000 | .000 | |
| % Male | 59.5 (3.2) | 59.2 (0.8) | .932 | 59.7 (2.8) | 58.5 (0.9) | .666 | 59.3 (3.0) | 58.1 (1.1) | .692 | .599 | |
| %Race/ethnicity: | .000 | .000 | .003 | 000 | |||||||
| White | 51.6 (3.3) | 70.1 (1.7) | 60.2 (3.7) | 78.2 (1.3) | 75.4 (3.6) | 88.5 (0.9) | . | ||||
| Black | 16.7 (2.7) | 9.9 (0.8) | 15.7 (2.0) | 8.6 (0.6) | 9.8 (1.6) | 4.7 (0.5) | |||||
| Native American | 3.3 (1.6) | 1.8 (0.3) | 1.1 (0.5) | 2.1 (0.3) | 1.4 (0.7) | 1.6 (0.3) | |||||
| Asian/Pacific islander | 4.7 (1.5) | 3.8 (0.5) | 5.6 (1.7) | 2.6 (0.4) | 3.4 (1.3) | 1.1 (0.4) | |||||
| Hispanic | 23.7 (2.9) | 13.8 (1.3) | 17.4 (2.6) | 8.5 (0.9) | 9.9 (3.1) | 4.1 (0.6) | |||||
| %Marital status: | .719 | .007 | .015 | .002 | |||||||
| Married/cohabiting | 43.0 (3.2) | 42.6 (1.0) | 65.0 (2.3) | 74.1 (0.7) | 64.9 (2.8) | 73.7 (0.9) | |||||
| Widowed | 0.1 (0.1) | 0.2 (0.1) | 2.2 (0.7) | 1.1 (0.1) | 19.3 (2.2) | 11.8 (0.6) | |||||
| Divorced or separated | 6.1 (1.2) | 6.1 (1.4) | 20.3 (2.1) | 15.0 (0.5) | 11.3 (1.5) | 10.7 (0.6) | |||||
| Never married | 50.8 (3.3) | 51.1 (1.1) | 12.5 (1.6) | 9.8 (0.5) | 4.5 (1.2) | 3.7 (0.4) | |||||
| % Pregnant/infant ≤1 year of age | 6.7 (1.3) | 9.3 (0.5) | .091 | 1.7 (0.7) | 1.6 (0.2) | .947 | 0.0 (0.0) | 0.0 (0.0) | .139 | ||
| %Main activity: | .010 | .017 | .000 | .000 | |||||||
| Employed | 74.7 (2.9) | 76.9 (0.9) | 84.3 (1.9) | 88.1 (0.5) | 26.0 (2.7) | 42.7 (1.1) | |||||
| Unemployed | 9.4 (2.0) | 4.9 (0.4) | 6.6 (1.4) | 3.7 (0.3) | 1.5 (0.8) | 1.4 (0.2) | |||||
| Retired | 1.0 (0.4) | 0.4 (0.1) | 4.5 (1.2) | 2.8 (0.2) | 66.0 (2.9) | 49.6 (1.1) | |||||
| Student | 9.6 (2.1) | 14.7 (0.8) | 0.2 (0.1) | 0.8 (0.1) | 0.0 (0.0) | 0.1 (0.1) | |||||
| Homemaker | 5.4 (1.3) | 3.1 (0.3) | 4.4 (1.2) | 4.6 (0.3) | 6.5 (1.6) | 6.2 (0.5) | |||||
| %Educational attainment: | .000 | .000 | .000 | .000 | |||||||
| <High school graduate | 15.9 (2.4) | 9.6 (0.6) | 17.4 (2.4) | 6.6 (0.5) | 27.4 (3.0) | 9.6 (0.6) | |||||
| High school graduate | 34.1 (3.1) | 23.6 (0.9) | 30.5 (2.6) | 23.7 (0.8) | 26.9 (2.7) | 28.1 (1.1) | |||||
| Attended/completed college | 50.1 (3.3) | 66.8 (1.0) | 52.1 (3.1) | 69.7 (0.9) | 45.7 (3.4) | 62.3 (1.1) | |||||
| %Family income: | .005 | .000 | .000 | .000 | |||||||
| Less than $35,000 | 56.9 (3.2) | 44.9 (1.1) | 38.7 (2.6) | 22.0 (0.8) | 55.7 (3.4) | 37.3 (1.1) | |||||
| $35,000–69,999 | 25.6 (2.6) | 32.8 (0.8) | 35.8 (2.7) | 33.3 (0.9) | 33.1 (3.1) | 33.9 (1.0) | |||||
| $70,000+ | 17.5 (2.4) | 22.3 (1.0) | 25.5 (2.4) | 44.7 (1.2) | 11.2 (2.3) | 28.8 (1.3) | |||||
| %Major financial problems | 31.2 (3.2) | 27.5 (0.9) | .279 | 27.2 (2.5) | 17.7 (0.6) | .001 | 7.5 (1.6) | 6.4 (0.5) | .520 | .003 | |
| % Good/fair/poor health | 26.9 (2.7) | 22.6 (0.8) | .134 | 42.7 (3.0) | 27.3 (0.8) | .000 | 61.6 (2.9) | 41.9 (1.1) | .000 | .000 | |
| % Liver disease | 1.4 (0.8) | 0.2 (0.1) | .147 | 1.4 (0.6) | 0.6 (0.1) | .173 | 0.9 (0.5) | 0.5 (0.1) | .431 | .033 | |
| % Cardiovascular disease | 2.9 (1.0) | 2.1 (0.2) | .432 | 4.9 (1.0) | 4.1 (0.4) | .448 | 14.5 (2.5) | 12.9 (0.7) | .572 | .258 | |
| % Hypertension | 4.1 (1.1) | 3.6 (0.4) | .716 | 16.2 (2.1) | 13.0 (0.5) | .153 | 40.9 (3.0) | 34.3 (0.9) | .041 | .011 | |
| % Gastric disease | 3.5 (1.2) | 2.7 (0.3) | .522 | 7.4 (1.6) | 4.7 (0.3) | .103 | 10.2 (2.0) | 6.0 (0.5) | .048 | .015 | |
| % Any mood disorder | 12.7 (2.2) | 13.4 (0.6) | .756 | 11.5 (2.1) | 7.7 (0.4) | .086 | 6.6 (2.1) | 3.8 (0.3) | .203 | .141 | |
| % Any anxiety disorder | 12.0 (2.0) | 12.9 (0.7) | .650 | 14.3 (2.4) | 11.2 (0.5) | .230 | 9.7 (2.3) | 7.4 (0.5) | .365 | .335 | |
| % Cluster A personality disorder | 16.3 (2.3) | 12.0 (0.6) | .057 | 11.6 (2.0) | 7.7 (0.4) | .055 | 7.6 (1.4) | 4.2 (0.4) | .032 | .002 | |
| % Cluster B personality disorder | 23.6 (2.7) | 21.3 (0.8) | .398 | 14.7 (2.2) | 13.2 (0.6) | .510 | 6.9 (1.3) | 7.1 (0.6) | .903 | .331 | |
| % Cluster C personality disorder | 11.9 (2.1) | 10.7 (0.6) | .598 | 11.0 (2.5) | 9.5 (0.5) | .520 | 5.8 (1.3) | 7.5 (0.5) | .194 | .705 | |
| %Smoking status: | .567 | .267 | .670 | .992 | |||||||
| Nonsmoker | 61.2 (3.3) | 57.9 (1.0) | 60.8 (3.2) | 65.7 (0.9) | 76.7 (0.9) | 78.4 (2.9) | |||||
| Nondependent smoker | 18.6 (2.5) | 21.1 (0.8) | 18.5 (2.6) | 14.8 (0.7) | 6.7 (1.6) | 8.2 (0.6) | |||||
| Dependent smoker | 20.2 (2.7) | 20.9 (0.7) | 20.7 (2.2) | 19.6 (0.6) | 14.9 (2.5) | 15.1 (0.8) | |||||
| % Drug status: | .012 | .334 | .822 | .106 | |||||||
| Non drug user | 87.4 | (2.2) | 80.9 (0.8) | 93.7 (1.4) | 92.7 (0.4) | 97.4 (1.5) | 97.6 (0.4) | ||||
| Nondependent drug user | 11.8 (2.1) | 16.9 (0.8) | 5.2 (1.3) | 6.8 (0.4) | 2.4 (1.5) | 2.3 (0.3) | |||||
| Dependent drug user | 0.8 (0.4) | 2.2 (0.3) | 1.1 (0.5) | 0.5 (0.1) | 0.2 (0.2) | 0.1 (0.1) | |||||
| %Alcohol use disorder history (AUD) | .004 | .000 | .000 | .000 | |||||||
| Former AUD, full stable remission | 9.2 (2.0) | 14.0 (0.7) | 17.8 (2.4) | 27.0 (0.8) | 17.7 (2.7) | 21.6 (1.1) | |||||
| Former AUD, recent/partial remission | 12.2 (2.2) | 9.7 (0.6) | 4.3 (1.0) | 6.9 (0.4) | 5.3 (1.5) | 5.7 (0.5) | |||||
| Current AUD | 19.0 (2.4) | 27.8 (0.9) | 11.9 (1.9) | 15.9 (0.7) | 1.5 (0.7) | 6.3 (0.5) | |||||
| No history of AUD | 59.3 (3.4) | 48.6 (1.1) | 66.0 (2.9) | 50.2 (1.2) | 75.4 (3.0) | 66.4 (1.3) | |||||
| %Any alcohol treatment | 4.1 (1.3) | 1.8 (0.2) | .081 | 3.1 (0.8) | 1.5 (0.2) | .060 | 1.0 (0.7) | 0.5 (0.1) | .497 | .009 | |
| Mean years since first drink | 8.2 (0.4) | 8.5 (0.1) | .472 | 23.7 (0.5) | 25.2 (0.1) | .004 | 45.1 (1.0) | 44.6 (0.2) | .597 | .001 | |
| Mean months since last drink | 1.2 (0.1) | 0.4 (0.0) | .000 | 0.9 (0.1) | 0.3 (0.0) | .000 | 0.7 (0.1) | 0.2 (0.0) | .000 | .008 | |
| Mean ADV ethanol intake (oz.) | 0.9 (0.1) | 1.1 (0.0) | .427 | 1.2 (0.4) | 0.9 (0.1) | .355 | 0.4 (0.1) | 0.7 (0.0) | .000 | .327 | |
| Mean frequency drinking 5+ drinks | 30.0 (4.6) | 38.7 (1.4) | .069 | 31.6 (5.9) | 26.7 (1.4) | .416 | 8.8 (2.7) | 14.3 (1.2) | .061 | .026 | |
| Events during follow-up: | |||||||||||
| Got divorced/separated | 3.5 (1.1) | 4.1 (0.3) | .621 | 4.3 (1.0) | 5.0 (0.3) | .525 | 0.0 (0.0) | 0.9 (0.2) | .000 | .222 | |
| Became widowed | 0.0 (0.0) | 0.1 (0.1) | .119 | 0.6 (0.5) | 0.4 (0.1) | .683 | 2.0 (1.0) | 2.8 (0.4) | .490 | .627 | |
| Became retired | 3.1 (1.2) | 0.4 (0.1) | .030 | 7.0 (1.5) | 3.4 (0.3) | .018 | 12.4 (2.1) | 13.0 (0.7) | .781 | .017 | |
| Had children | 27.9 (2.9) | 23.6 (0.8) | .155 | 4.1 (1.2) | 6.0 (0.4) | .154 | 0.4 (0.3) | 0.5 (0.1) | .619 | .530 | |
| New case of liver disease | 0.0 (0.0) | 0.2 (0.1) | .076 | 2.5 (0.8) | 0.9 (0.2) | .076 | 0.7 (0.5) | 0.6 (0.2) | .834 | .118 | |
| New case of cardiovascular disease | 2.0 (0.8) | 2.2 (0.3) | .885 | 5.3 (1.3) | 4.5 (0.3) | .525 | 15.9 (2.4) | 9.1 (0.6) | .010 | .022 | |
| New case of hypertension | 5.6 (1.5) | 3.8 (0.4) | .223 | 10.8 (1.6) | 8.1 (0.4) | .097 | 13.0 (2.0) | 14.1 (0.7) | .618 | .194 | |
| New case of gastric disease | 1.4 (0.7) | 1.9 (0.2) | .453 | 5.4 (1.4) | 3.2 (0.3) | .113 | 4.9 (1.3) | 4.4 (0.4) | .732 | .269 | |
| Incident AUD | 2.4 (0.9) | 10.3 (0.6) | .000 | 2.7 (0.8) | 5.3 (0.4) | .009 | 2.7 (1.1) | 3.2 (0.4) | .654 | .000 | |
| Stopped smoking | 18.8 (2.7) | 10.3 (0.5) | .000 | 15.6 (2.1) | 7.4 (0.4) | .000 | 10.4 (2.2) | 5.3 (0.5) | .024 | .000 | |
Note: Figures in parentheses are standard errors of estimates. Bolded figures represent statistically significant differences (p<.005 before rounding) between individuals who stopped and continued drinking or indicate that the association between the characteristic and drinking cessation varies significantly (p<.005) across age categories.
Within the three age-stratified models (Table 2), correlates that were highly significant (p<.005) and of similar magnitude in all age groups included attending college vs. not completing high school (OR = 0.42–0.54), months since last drink (OR = 1.24–1.29) and smoking cessation over follow-up (OR = 2.82–3.45). When the broadly overlapping ORs for Blacks and Hispanics were combined (OR = 1.65–1.80, data not shown), their effect was highly significant (p=.001) at ages 18–54 but marginally significant (p=.015) at ages 55+. Similarly, current vs. no history of AUD at baseline had a consistent effect across age groups (OR = 0.30–0.60) that was highly significant at ages 18–24 (p=.001) but of marginal significance (p=.021) at ages 35+.
Table 2.
Odds ratios for associations of selected characteristics with drinking cessation over a 3-year follow-up interval, by age category: U.S. regular drinkers 18 and older at baseline
| Ages 18–34 | Ages 35–54 | Ages 55+ | p-value Δ age | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | ||
| Baseline past-year characteristics: | ||||||||||
| Age (log) | --- | --- | --- | --- | --- | --- | 1.03 | (1.01–1.05) | .002 | NA |
| Male | --- | --- | --- | --- | --- | --- | 1.43 | (1.06–1.93) | .018 | --- |
| Blacka | 1.74 | (1.18–2.29) | .006 | 1.77 | (1.26–2.50) | .001 | 1.88 | (1.21–2.93) | .006 | --- |
| Native Americana | 2.72 | (0.96–7.71) | .059 | 0.61 | (0.22–1.68) | .337 | 1.04 | (0.38–2.86) | .938 | --- |
| Asiana | 1.59 | 0.80–3.14) | .182 | 2.44 | (1.26–4.73) | .009 | 5.25 | (2.36–11.69) | .000 | .017 |
| Hispanica | 1.58 | (1.11–1.25) | .011 | 1.62 | (1.09–2.40) | .017 | 1.73 | (0.83–3.63) | .142 | --- |
| Pregnant/had infant ≤1 year of age | 0.41 | (0.24–0.68) | .001 | --- | --- | --- | --- | --- | --- | --- |
| Unemployed, retired, homemakerb | --- | --- | --- | 1.15 | (0.81–1.64) | .436 | 1.47 | (1.03–2.09) | .033 | --- |
| Studenta | --- | --- | --- | 0.36 | (0.14–0.93) | .036 | * | * | * | --- |
| High school graduatec | 0.92 | (0.61–1.37) | .665 | 0.64 | (0.40–1.02) | .060 | 0.43 | (0.29–0.63) | .000 | .001 |
| Attended/completed collegec | 0.54 | (0.36–0.83) | .005 | 0.43 | (0.26–0.74) | .002 | 0.42 | (0.27–0.65) | .000 | --- |
| Family income $35,000–69,999d | 0.68 | (0.50–0.92) | .015 | 0.80 | (0.59–1.08) | .135 | 1.05 | (0.73–1.51) | .785 | --- |
| Family income ≥$70,000d | 0.80 | (0.54–1.18) | .258 | 0.50 | (0.36–0.69) | .000 | 0.44 | (0.24–0.80) | .008 | .010 |
| Good/fair/poor health | --- | --- | --- | --- | --- | --- | 1.44 | (1.07–1.93) | .016 | .036 |
| Liver disease | 5.30 | (1.39–20.19) | .015 | --- | --- | --- | --- | --- | --- | --- |
| Any mood disorder | --- | --- | --- | 1.62 | (1.04–2.52) | .034 | 2.21 | (1.01–4.84) | .047 | --- |
| Cluster A personality disorder | 1.49 | (1.03–2.15) | .033 | --- | --- | --- | --- | --- | --- | --- |
| Nondependent smokere | 0.70 | (0.46–1.07) | .100 | 1.03 | (0.71–1.49) | .890 | --- | --- | --- | --- |
| Dependent smokere | 0.51 | (0.33–0.79) | .003 | 0.61 | (0.40–0.92) | .020 | --- | --- | --- | --- |
| Nondependent drug userf | 0.68 | (0.43–1.08) | .103 | --- | --- | --- | --- | --- | --- | --- |
| Dependent drug userf | 0.22 | (0.07–0.70) | .011 | --- | --- | --- | --- | --- | --- | --- |
| Years since first drink (log) | --- | --- | --- | --- | --- | --- | 0.60 | (0.45–0.80) | .001 | .012 |
| Months since last drink | 1.25 | (1.17–1.35) | .000 | 1.29 | (1.19–1.39) | .000 | 1.24 | (1.13–1.36) | .000 | --- |
| Average daily volume of ethanol intake (log oz.) | --- | --- | --- | 0.85 | (0.77–0.95) | .003 | 0.74 | (0.67–0.81) | .000 | .001 |
| Former AUD, stable full remissiong | 0.64 | (0.38–1.10) | .106 | 0.61 | (0.43–0.86) | .006 | 0.83 | (0.53–1.29) | .400 | --- |
| Former AUD, recent/partial remissiong | 1.03 | (0.66–1.60) | .909 | 0.53 | (0.30–0.93) | .027 | 0.90 | (0.45–1.79) | .757 | --- |
| Current AUDf | 0.53 | (0.37–0.76) | .001 | 0.60 | (0.39–0.92) | .021 | 0.30 | (0.11–0.83) | .021 | --- |
| Any alcohol treatment | 3.02 | (1.30–7.03) | .011 | --- | --- | --- | --- | --- | --- | --- |
| Events during follow-up: | ||||||||||
| Became retired | 6.35 | (2.54–15.86) | .000 | 1.94 | (1.14–3.28) | .015 | --- | --- | --- | .009 |
| Incident CVD | --- | --- | --- | --- | --- | --- | 1.87 | (1.242–2.82) | .003 | .025 |
| Incident AUD | 0.21 | (0.10–0.46 | .000 | --- | --- | --- | --- | --- | --- | .000 |
| Stopped smoking | 3.24 | (2.03–5.17) | .000 | 3.45 | (2.20–5.39) | .000 | 2.82 | (1.62–4.92) | .000 | --- |
Note: Bolded figures indicate p-values <.05.
Referents:
White
Employed;
Did not complete high school;
Income <$35,000;
Non-smoker;
Non drug user;
No history of AUD at baseline
Too few cases to estimate odds ratio.
Covariates whose ORs were of similar magnitude across age but statistically significant for limited age groups included: a) positive associations with liver disease, cluster A PD, and alcohol treatment and negative associations with pregnancy or an infant in the household and drug use disorder at ages 18–34 only; b) a negative association with nicotine dependence at ages 18–54 only; c) a negative association with being a student and being in stable remission from a former AUD at ages 35–54 only; d) a positive association with mood disorder at ages 35+ only; and e) positive associations with male sex and being unemployed, retired or a homemaker at ages 55+ only. Most of these associations were of marginal statistical significance.
The final group of correlates comprised those whose associations with drinking cessation demonstrated significant variation in magnitude across age. Highly significant (P <0.005) age variation was observed for high school graduation versus not graduating (ORs becoming increasingly negative with age and significant only at ages 55+), volume of ethanol intake (ORs increasingly negative with age and significant only at ages 35+) and incident AUD (significant at 18-34 only). Age variation of more marginal statistical significance (0.005 <P <0.05) was observed for Asian race/ethnicity, family income ≥ $70,000, good/fair/poor health, interval since first drink and incident CVD and retirement.
When the models for the three age groups were re-estimated without the variable for smoking cessation over follow-up (data not shown), the results were similar, except that the negative association of nicotine dependence with drinking cessation, formerly significant at ages 18–54, was no longer significant in any age group. In addition, a few associations that had been of marginal significance fell just short of significance, including the effect of Cluster A PD at ages 18–34 and the effects of mood disorder and being unemployed, retired or a homemaker at ages 55+.
DISCUSSION
We initially hypothesized that transitions related to adopting adult role responsibilities would play a predominant role in drinking cessation during the early adult years, with health problems assuming more prominence later in life. Our results provided partial support for these hypotheses, demonstrating an increasingly positive association for good/fair/poor (versus very good/excellent) health and mood disorder with increasing age. In addition, incident CVD was positively related to drinking cessation only at ages 55+. However, a positive association with liver disease was significant only in the youngest age group. Compared to individuals 18–34 years of age with liver disease, those in the older age groups were far more likely to assess their health as good, fair or poor. Thus, any impact of liver disease among older adults may have been subsumed under the effects of self-perceived health, which also may have mediated the effects of some of the other specific diseases for which positive associations reported in earlier studies were not replicated in this analysis [22,23,26,34].
In terms of role transitions and responsibilities, we did not find that marrying or having a child increased the odds of drinking cessation at younger ages. Indeed, drinkers already pregnant or parents of infants at baseline were at reduced risk of drinking cessation, not having stopped prior to baseline arguably marking a lack of propensity to react to these events. Whereas being unemployed, retired or a housewife was positively associated with drinking cessation only at ages 55+, becoming retired over follow-up showed a positive association with drinking cessation only at ages 18–54, when it is a more selective phenomenon, possibly related to leaving the job force because of disability (or to care for children). One reason why role transitions showed so little effect in this study may be the nature of the sample, which was not restricted to heavy drinkers or individuals with AUD. It may be the additional structure and lifestyle restrictions associated with getting married and having children are sufficiently compatible with moderate drinking that they do not imply any need to stop.
The factors that were most strongly and consistently associated with drinking cessation in this study reflected neither role transitions nor health. Across all age groups, the odds of drinking cessation were roughly tripled among individuals who stopped smoking during the follow-up interval. Similar findings have been reported elsewhere [38] and are consistent with the inverse association of drinking cessation with current smoking noted in numerous studies [10,12,22,24,27,37]. Individuals who stopped smoking may be those for whom health concerns prompted medical advice to cease use of both substances (thus also possibly contributing to the lack of association found for various medical conditions). Alternatively, smoking cessation could be seen as a marker of the ability to give up a psychoactive and potentially addictive substance, much as current alcohol use disorder (which reduced the odds of drinking cessation in all age groups) and nicotine dependence and drug use disorder (which reduced the odds of drinking cessation in younger age groups) indicate the inability to do so.
Irrespective of age, individuals of Black, Asian or Hispanic race-ethnicity were more likely than Whites to stop drinking, whereas individuals who attended or completed college were less likely to stop drinking. Similar findings have been reported in numerous other U.S. samples [8,10,17,18,20,22,28] and may reflect differences in the perceived acceptability of drinking, particularly among women, or subgroup-specific drinking contexts. For example, subpopulations in which drinking is integrated into daily life, e.g., via routine consumption of wine with meals, may be more likely to continue drinking than those in which drinking occurs on a more sporadic basis such as at bars or sporting events. Interestingly, the association of high school graduation with drinking cessation became increasingly negative with advancing age and was significant only at ages 55+. This may indicate that high school graduation represented a more significant academic achievement and thus a more meaningful demarcation of social status within older compared to the younger age groups.
Prior studies of drinking cessation have reported inconsistent effects of gender, with some showing men and women equally likely to stop/reduce drinking [22,24], some showing men less likely to do so [21] and others [23] including the present study showing men more likely to do so. These inconsistencies may reflect varying levels of adjustment for gender differences in alcohol consumption and AUD. Although the gender gap may be narrowing [53,54], women are still more likely to be light and infrequent drinkers and start drinking later than men [55,56]. This study found that the odds of drinking cessation increased with months since last drink (i.e., were greater for infrequent drinkers) at all ages and decreased with volume of consumption and interval since first drink in the older age groups, where these factors became increasingly indicative of atypically heavy and long-standing drinking habits.
Limitations of this study include self-report of medical conditions versus verification through medical records, possible recall problems for measures such as age at first drink, and the underreporting of alcohol consumption common to all surveys. The follow-up interval was brief in comparison to long-term longitudinal samples, which have found that intermediate or temporary abstinent phases are a frequent component of lifetime drinking histories [57–59]. Thus, correlates identified in the present study may not be indicative of permanent, stable drinking cessation. Whereas the brief three-year follow-up interval limited the number of cases of drinking cessation and thus the likelihood of identifying significant correlates, it was sufficiently long that some individuals may have stopped and resumed drinking, possibly resulting in underestimation of ORs for factors associated with short-term abstinence, e.g., pregnancy or temporary disability. Finally, the number of potential correlates considered was large, increasing the likelihood of spurious findings.
These limitations notwithstanding, this study was able to examine the independent associations of drinking cessation with a wide range of sociodemographic, health, comorbidity and alcohol use measures, using a prospective study design and a nationally representative general population sample large enough to assess age variation in these associations. Its results supported an extant literature demonstrating that drinking cessation is a dynamic process, variously influenced by diverse factors whose prevalence and impact vary over the life course. Despite the wide range of significant correlates identified in this study, they explained only a small portion of the variance in drinking cessation, ranging from 5% to 8% with increasing age. Thus, it is critical that future research investigate factors not considered in this study, including drinking context and motivation, peer drinking attitudes and behavior, arrests for driving under the influence, formal or informal discouragement of drinking in different types of student or retirement housing, and access issues related to aging, e.g., no longer driving. Finally, population-attributable fractions of drinking cessation due to health versus other factors would be invaluable for quantifying the impact of “sick quitters” on alcohol-related harm.
Acknowledgments
The study on which this paper is based, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), is sponsored by the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health, U.S. Department of Health and Human Services, with supplemental support from the National Institute on Drug Abuse. This research was supported in part by the Intramural Program of the National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism.
Footnotes
The views and opinions expressed in this paper are those of the author and should not be construed to represent the views of any of the sponsoring organizations, agencies or the U.S. government.
References
- 1.Shaper AG. Alcohol and mortality: A review of prospective studies. Br J Addict. 1990;85:837–847. doi: 10.1111/j.1360-0443.1990.tb03710.x. [DOI] [PubMed] [Google Scholar]
- 2.Shaper AG, Wannamethee SG, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. 1988;2(8623):1267–127. doi: 10.1016/s0140-6736(88)92890-5. [DOI] [PubMed] [Google Scholar]
- 3.Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W. Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses. Ann Epidemiol. 2007;17(5 Suppl):S16–S23. doi: 10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 4.Fillmore KM, Golding JM, Graves KL, Kniep S, Leino EV, Romelsjö A, Shoemaker C, Ager CR, Allebeck P, Ferrer HP. Alcohol consumption, mortality I. Characteristics of drinking groups. Addiction. 1998;93:183–203. doi: 10.1046/j.1360-0443.1998.9321834.x. [DOI] [PubMed] [Google Scholar]
- 5.Gmel G, Gutjahr E, Rehm J. How stable is the risk curve between alcohol and all-cause mortality and what factors influence the shape? A precision-weighted hierarchical meta-analysis. Eur J Epidemiol. 2003;18:631–642. doi: 10.1023/a:1024805021504. [DOI] [PubMed] [Google Scholar]
- 6.Roerecke M, Rehm J. Ischemic heart disease mortality and morbidity rates in former drinkers: a meta-analysis. Am J Epidemiol. 2011;173:245–258. doi: 10.1093/aje/kwq364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rostron B. Alcohol consumption and mortality risks in the USA. Alcohol Alcohol. 2012;47:334–339. doi: 10.1093/alcalc/agr171. [DOI] [PubMed] [Google Scholar]
- 8.Costanzo PR, Malone PS, Belsky D, Kertesz S, Pletcher M, Sloan FA. Longitudinal differences in alcohol use in early adulthood. J Stud Alcohol Drugs. 2007;68:727–737. doi: 10.15288/jsad.2007.68.727. [DOI] [PubMed] [Google Scholar]
- 9.Jackson KM, Sher KJ, Gotham HJ, Wood PK. Transitioning into and out of large-effect drinking in young adulthood. J Abnorm Psychol. 2001;110:378–391. doi: 10.1037//0021-843x.110.3.378. [DOI] [PubMed] [Google Scholar]
- 10.Merline AC, Schulenberg JE, O’Malley PM, Bachman JG, Johnston LD. Substance use in marital dyads: premarital assortment and change over time. J Stud Alcohol Drugs. 2008;69:352–361. doi: 10.15288/jsad.2008.69.352. [DOI] [PubMed] [Google Scholar]
- 11.Schulenberg J, O’Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: trajectories of frequent binge drinking during the transition to young adulthood. J Stud Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- 12.Jackson KM, Sher KJ, Cooper ML, Wood PK. Adolescent alcohol and tobacco use: onset, persistence and trajectories of use across two samples. Addiction. 2002;97:517–531. doi: 10.1046/j.1360-0443.2002.00082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labouvie E. Maturing out of substance use: selection and self-correction. J Drug Issues. 1996;26:457–476. [Google Scholar]
- 14.Leino EV, Ager CR, Fillmore KM, Johnstone BM. A meta-analysis of multiple longitudinal studies from the Collaborative Alcohol-Related Longitudinal Project. Am J Addict. 1995;4:141–149. [Google Scholar]
- 15.Merline A, Jager J, Schulenberg JE. Adolescent risk factors for adult alcohol use and abuse: stability and change of predictive value across early and middle adulthood. Addiction. 2008;103(Suppl 1):84–99. doi: 10.1111/j.1360-0443.2008.02178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prescott CA, Kendler KS. Associations between marital status and alcohol consumption in a longitudinal study of female twins. J Stud Alcohol. 2001;62:589–604. doi: 10.15288/jsa.2001.62.589. [DOI] [PubMed] [Google Scholar]
- 17.Lanza ST, Collins LM. A mixture model of discontinuous development in heavy drinking from ages 18 to 30: the role of college enrollment. J Stud Alcohol. 2006;67:552–561. doi: 10.15288/jsa.2006.67.552. [DOI] [PubMed] [Google Scholar]
- 18.Muthén BO, Muthén LK. The development of heavy drinking, alcohol-related problems from ages 18 to 37 in a US, national sample. J Stud Alcohol. 2000;61:290–300. doi: 10.15288/jsa.2000.61.290. [DOI] [PubMed] [Google Scholar]
- 19.Casswell S, Pledger M, Pratap S. Trajectories of drinking from 18 to 26 years: identification and prediction. Addiction. 2002;97:1427–1437. doi: 10.1046/j.1360-0443.2002.00220.x. [DOI] [PubMed] [Google Scholar]
- 20.Brennan PL, Schutte KK, Moos RH. Retired status and older adults’ 10-year drinking trajectories. J Stud Alcohol Drugs. 2010;71:165–168. doi: 10.15288/jsad.2010.71.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Molander RC, Yonker JA, Krahn DD. Age-related changes in drinking patterns from mid-to-older age: Results from the Wisconsin longitudinal study. Alcohol Clin Exp Res. 2010;34:1182–1192. doi: 10.1111/j.1530-0277.2010.01195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Platt A, Sloan FA, Costanzo P. Alcohol-consumption trajectories and associated characteristics among adults older than age 50. J Stud Alcohol Drugs. 2010;71:169–179. doi: 10.15288/jsad.2010.71.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pringle KE, Heller DA, Ahern FM, Gold CH, Brown TV. The role of medication use and health on the decision to quit drinking among older adults. J Aging Health. 2006;18:837–851. doi: 10.1177/0898264306293583. [DOI] [PubMed] [Google Scholar]
- 24.Satre DD, Areán PA. Effects of gender, ethnicity, and medical illness on drinking cessation in older primary care patients. J Aging Health. 2005;17:70–84. doi: 10.1177/0898264304272785. [DOI] [PubMed] [Google Scholar]
- 25.Shaw BA, Krause N, Liang J, McGeever K. Age differences in long-term patterns of change in alcohol consumption among aging adults. J Aging Health. 2011;23:207–227. doi: 10.1177/0898264310381276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wannamethee G, Shaper AG. Changes in drinking habits in middle-aged British men. J R Coll Gen Pract. 1988;38:440–442. [PMC free article] [PubMed] [Google Scholar]
- 27.Bobo JK, Greek AA. Increasing, decreasing alcohol use trajectories among older women in the US, across a 10-year interval. Int J Environ Res Public Health. 2011;8:3263–3276. doi: 10.3390/ijerph8083263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dawson DA, Goldstein RB, Ruan WJ, Grant BF. Correlates of recovery from alcohol dependence: A prospective study over a 3-year follow-up interval. Alcohol Clin Exp Res. 2012;36:1268–1277. doi: 10.1111/j.1530-0277.2011.01729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delucchi KL, Kaskutas LA. Following problem drinkers over eleven years: understanding changes in alcohol consumption. J Stud Alcohol Drugs. 2010;71:831–836. doi: 10.15288/jsad.2010.71.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matzger H, Kaskutas LA, Weisner C. Reasons for drinking less and their relationship to sustained remission from problem drinking. Addiction. 2005;100:1637–1646. doi: 10.1111/j.1360-0443.2005.01203.x. [DOI] [PubMed] [Google Scholar]
- 31.Delucchi KL, Matzger H, Weisner C. Dependent and problem drinking over 5 years: a latent class growth analysis. Drug Alcohol Depend. 2004;74:235–244. doi: 10.1016/j.drugalcdep.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 32.Brennan PL, Schutte KK, Moos BS, Moos RH. Twenty-year alcohol-consumption and drinking- problem trajectories of older men and women. J Stud Alcohol Drugs. 2011;72:308–321. doi: 10.15288/jsad.2011.72.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Green CA, Polen MR. The health and health behaviors of people who do not drink alcohol. Am J Prev Med. 2001;21:298–305. doi: 10.1016/s0749-3797(01)00365-8. [DOI] [PubMed] [Google Scholar]
- 34.Liang W, Chikritzhs T. Reduction in alcohol consumption and health status. Addiction. 2011;106:75–81. doi: 10.1111/j.1360-0443.2010.03164.x. [DOI] [PubMed] [Google Scholar]
- 35.Hajema KJ, Knibbe RA. Changes in social roles as predictors of changes in drinking behavior. Addiction. 1998;93:1717–1727. doi: 10.1046/j.1360-0443.1998.931117179.x. [DOI] [PubMed] [Google Scholar]
- 36.Neve RJ, Lemmens PH, Drop MJ. Changes in alcohol use and drinking problems in relation to role transitions in different stages of the life course. Subst Abus. 2000;21:163–178. doi: 10.1080/08897070009511430. [DOI] [PubMed] [Google Scholar]
- 37.Fillmore KM, Kerr WC, Bostrom A. Changes in drinking status, serious illness and mortality. J Stud Alcohol. 2003;64:278–285. doi: 10.15288/jsa.2003.64.278. [DOI] [PubMed] [Google Scholar]
- 38.Karlamangla A, Zhou K, Reuben D, Greendale G, Moore A. Longitudinal trajectories of heavy drinking in adults in the United States of America. Addiction. 2006;101:91–9. doi: 10.1111/j.1360-0443.2005.01299.x. [DOI] [PubMed] [Google Scholar]
- 39.Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 40.Grant BF, Kaplan K, Moore T, Kimball J. 2004–2005 Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions: Source and Accuracy Statement. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2007. [Google Scholar]
- 41.Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. (DSM-IV) [Google Scholar]
- 43.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 44.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:1107–15. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 45.Pulay AJ, Stinson FS, Ruan WJ, Smith SM, Pickering RP, Dawson DA, Grant BF. The relationship of DSM-IV personality disorders to nicotine dependence: results from a national survey. Drug Alcohol Depend. 2010;108:141–145. doi: 10.1016/j.drugalcdep.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence, co-occurrence of substance use disorders, independent mood, anxiety disorders Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 47.Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol, drug use disorders, personality disorders in the United States Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- 48.Stinson FS, Grant BF, Dawson DA, Ruan WJ, Huang B, Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2005;80:105–116. doi: 10.1016/j.drugalcdep.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 49.Grant BF, Dawson DA, Stinson FS, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Schedule (AUDADIS): Reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- 50.Dawson DA. Methodological issues in measuring alcohol use. Alc Res Health. 2003;27:18–29. [PMC free article] [PubMed] [Google Scholar]
- 51.Grant BF, Dawson DA, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 52.Research Triangle Institute. SUDAAN Language Manual, Release 10.0. Research Triangle Park, NC: Research Triangle Institute; 2008. [Google Scholar]
- 53.Keyes KM, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: a review and synthesis. Alcohol Clin Exp Res. 2011;35:2101–2112. doi: 10.1111/j.1530-0277.2011.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holmila M, Raitasalo K. Gender differences in drinking: why do they still exist? Addiction. 2005;100:1763–1769. doi: 10.1111/j.1360-0443.2005.01249.x. [DOI] [PubMed] [Google Scholar]
- 56.National Institute on Alcohol Abuse and Alcoholism. Alcohol Use and Alcohol Use Disorders in the United States: Main Findings from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2006. [Google Scholar]
- 57.Neve RJM, Lemmens PH, Drop MJ. Drinking careers of older male alcoholics in treatment as compared to younger alcoholics and to older social drinkers. J Stud Alcohol. 1997;58:303–311. doi: 10.15288/jsa.1997.58.303. [DOI] [PubMed] [Google Scholar]
- 58.Vaillant GE. A 60-year follow-up of alcoholic men. Addiction. 2003;98:1043–1051. doi: 10.1046/j.1360-0443.2003.00422.x. [DOI] [PubMed] [Google Scholar]
- 59.York JL. Progression of alcohol consumption across the drinking career in alcoholics and social drinkers. J Stud Alcohol. 1995;56:328–336. doi: 10.15288/jsa.1995.56.328. [DOI] [PubMed] [Google Scholar]