Abstract
While antimicrobials are clinically effective in preventing post-operative recurrence, the role for antibiotics in primary therapy for Crohn’s disease (CD) remains unclear. The recent multicenter phase 2 trial by Prantera et al received wide attention because it demonstrated an increase in the week 12 remission rate in patients with moderately active CD treated with rifaximin and renewed interest in microbial manipulation as primary therapy for CD. In this commentary, we discuss aspects of durability, immune cell polarization, and safety of microbial manipulation as primary therapy for CD.
Keywords: Inflammatory bowel disease, Rifaximin, Microbiome
COMMENTARY ON HOT TOPICS
Inflammatory bowel disease (IBD) results from a dysregulated immune response to environmental and microbial antigens in a genetically susceptible host. Although we cannot readily manipulate the host genotypes of our patients, numerous clinical studies have attempted to modulate the inflammatory immune response with prebiotic, probiotic, and antimicrobial therapy. The results of randomized controlled trials of antibiotics, however, have been mixed (Table 1). While antimicrobials have gained traction in preventing post-operative recurrence, the role for antibiotics in primary therapy for Crohn’s disease (CD) remains unclear. Post-hoc analysis of these studies has suggested that antibiotics may be more appropriate in patients with large bowel involvement, but this remains unproven in a randomized controlled trial. Furthermore, despite statistically significant differences in reduction in Crohn’s disease activity index (CDAI) in several studies, the lack of effect on true disease remission (CDAI < 150), the concern for medication side effects, and the increasing rate of antibiotic associated Clostridium difficile (C. difficile) in the IBD population has limited its use in practice.
Table 1.
Randomized controlled trials of antibiotic therapy in inflammatory bowel disease
| Ref. | Antibiotic therapy | Patients (n) | Primary outcome | Results |
| Afdhal et al[12] | Clofazimine | 49 | DAS < 5 | 64% (vs 50% placebo, NS) |
| Sutherland et al[13] | Metronidazole | 105 | ↓CDAI (16 wk) | 81 (vs -1 placebo, P = 0.001) |
| Prantera et al[14] | Ethambutol, rifampicin, clofazimine, dapsone | 45 | Relapse (9 mo) | Likelihood ratio: 4.6 |
| Steinhart et al[15] | Ciprofloxacin, metronidazole | 130 | Remission (8 wk) | 33% (vs 38% placebo, NS) |
| Arnold et al[16] | Ciprofloxacin | 47 | ↓CDAI (6 mo) | 75 (vs 25 placebo, P < 0.001) |
| Prantera et al[17] | Rifaximin | 83 | ↓CDAI < 150 (12 wk) | 52% (vs 33% placebo, NS) |
| Selby et al[18] | Clarithromycin, rifabutin, clofazimine | 213 | Relapse (2 yr) | 66% (vs 50% placebo, P = 0.02) |
| Leiper et al[19] | Clarithromycin | 41 | ↓CDAI < 150 (3 mo) | 26% (vs 27% placebo, NS) |
DAS: Disease Activity Score; CDAI: Crohn’s disease activity index; NS: Not significant.
Given these mixed results, the recent multicenter phase 2 trial by Prantera et al[1] received wide attention because it demonstrated an increase in the week 12 remission rate in patients with moderately active CD treated with 800 mg rifaximin extended release (ER) twice per day (bid) (62% vs 43%, P = 0.005) and renewed interest in microbial manipulation as primary therapy for CD. As we evaluate the implications of this work, several questions arise: What is the durability of this effect both clinically and microbially? How do we select the patients who will derive the most benefit from antimicrobial therapy? Are these therapies safe?
Durability of response is crucial in coordinating medical therapy and prognosticating clinical course. Evidence of mucosal healing in addition to clinical indicators of disease activity represented in the CDAI define a “deep remission” associated with a durable response. While the CDAI data generated by Prantera et al[1] are encouraging, remission and response depended solely on clinical indicators, some of which are subjective and not necessarily reflective of systemic inflammation. Objective endoscopic and serologic endpoints to define local and systemic control of inflammation will be crucial in follow up studies of antibiotics as primary therapy.
The second aspect of durability is the effect of rifaximin on the intestinal microbiome. The intestinal “microbiome” refers to the totality of intestinal bacteria and the collection of genetic data that it encodes is called a metagenome. Advances in sequencing technology over the last decade have enabled broader analysis of the types of bacteria that are present in the intestine. Pioneering work defining the full spectrum of intestinal microbiota in patients with IBD by 16S ribosomal RNA sequence (instead of conventional culture methods)[2] led to the characterization of an IBD microbiome, reflecting a general reduction in bacterial diversity, a decrease in the clostridial family Lachnospiraceae, and an expansion of proteobacteria. More specific characterization of clinical phenotype [ileal Crohn’s disease (ICD), colonic CD, ulcerative colitis] in a cohort of Swedish twins revealed the particular prevalence of Escherichia coli (E. coli) species in ICD with a unique contribution of Ruminococcus gnavus[3]. One interesting finding by Scarpignato et al[4] is that clinical remission was maintained in 63% of the patients in the treatment group up to 12 wk after finishing rifaximin therapy. Prior studies have shown return of pretreatment levels of microbiota within 1-2 wk after discontinuing rifaximin, so it remains unclear whether the durability of this treatment is secondary to a permanent change in the intestinal microbiota or a suppression of a specific pathogenic species. While this analysis is beyond the scope of the study offered by Prantera et al[1], future studies will need to incorporate microbial analysis as well as metatranscriptomic analysis (e.g., what the bacteria are doing) in order to recognize the full diagnostic and therapeutic potential of antimicrobial therapy.
Given rifaximin’s broad spectrum of activity against anaerobic and aerobic gram-negative and gram-positive organisms, it is possible that rifaximin treatment eliminates a particular pathogenic or group of pathogenic bacteria that was unaffected by the antibiotics used in previous investigations. If so, does this explain the lack of a dose response in the study? In contrast to previous studies, Prantera et al[1] show no benefit to colonic location of disease [odds ratio (OR) 0.5, P = 0.004]. Does this mean that a suspected pathogen isn’t restricted to the colon or that colonic localization is not required? Given the distribution of CD throughout the gastrointestinal tract, this may be a reasonable conclusion.
Microbial analysis suggests several candidate bacteria may be involved in the pathophysiology of CD. Notably, adherent-invasive E. coli (AIEC) have been described to be attached to the ileal mucosa of patients with ICD[5]. These invasive bacteria may sustain inflammation in genetically susceptible individuals and generate systemic immune responses (reflected by serologies) (Figure 1). While E. coli are sensitive to rifaximin in vitro, the effect of rifaximin on AIEC populations in vivo has not been clearly defined, but could be studied in this cohort. In addition to AIEC, analysis of a post-operative ICD cohort revealed the correlation of the clostridial species, Faecalibacterium prausnitzii (F. prausnitzii), with a decreased incidence of post-operative recurrence[6]. Clostridium species IV and XIVa (which include F. prausnitzii) have been shown in mouse models to induce the accumulation of regulatory T cells in the colon[7] (Figure 1). Further microbial analysis of primary antimicrobial therapy for CD may offer deeper insight into the mechanism of rifaximin therapy.
Figure 1.
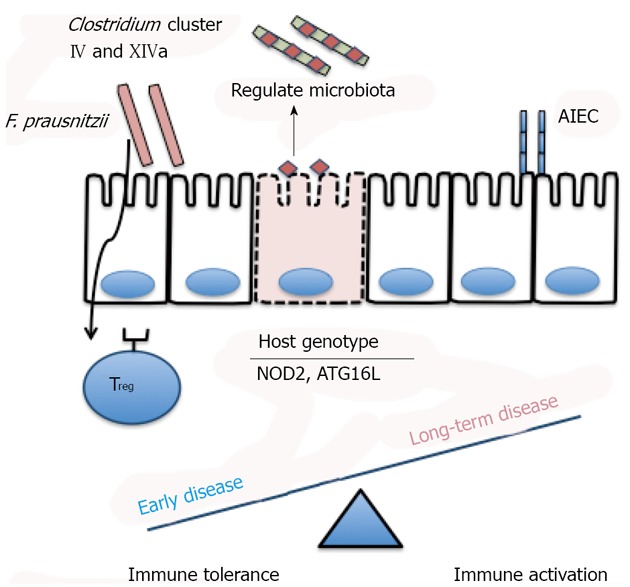
Microbiota regulate immune tolerance and activation in inflammatory bowel disease. Clostridium cluster IV and XIVa can induce regulatory T cell (Treg) polarization in the lamina propria[7]. One member of this cluster, Fecalibacterium prausnitzii (F. prausnitzii), correlates with reduced post-operative recurrence in Crohn’s disease (CD)[6]. Adherent invasive Escherichia coli (AIEC) are found with greater frequency in ileal CD[11]. Interaction with microbial species may differentially modulate the immune response in early inflammatory disease compared to long-term fibrotic disease[8]. Host genotype may regulate luminal microbial species. NOD2: Nucleotide-binding ligomerization domain-containing protein 2; ATG16L: Autophagy-related protein 16-1[9].
If the efficacy of rifaximin depends on microbial mediated disease, perhaps there are clinical or diagnostic parameters that may highlight patients that will derive maximal benefit from antimicrobial therapy? Subgroup analysis by Prantera et al[1] revealed maximal benefit in patients with “early disease”, defined as < 3 years at time of entry into the study (OR 1.7, P = 0.02). Recent data in mice showed that the timing of introduction of microbiota into “germ-free” animals regulates the influx of immune cells into intestinal tissue by modulating the expression of genes involved in recruiting these cells[8]. Perhaps “early disease” maintains immunologic plasticity whereas long-standing disease has already been programmed to support inflammation. Further characterization may reveal distinct microbial components of their cohort. Finally, it would be interesting to know if disease susceptibility alleles correlate with antimicrobial response. A recent study of microbiota in patients with IBD revealed that genetic susceptibility alleles for nucleotide-binding oligomerization domain-containing protein 2 and autophagy-related protein 16-1 correlate with alterations in the microbiome[9]. These clinical and genotypic parameters may improve the targeted use of antibiotic therapy for CD.
The safety of widespread and long-term antibiotics also remains an issue of concern. Rifaximin has minimal systemic absorption. As such, rifaximin does not have notable systemic side effects or interactions associated with imidazole or fluoroquinolone antibiotics. C. difficile remains a major problem in the clinical management of IBD with rising rates of CDI associated with morbidity, mortality and need for colectomy[10]. Although rifaximin may help treat C. difficile, one case of C. difficile was seen in the 800 mg ER bid group. Further studies will be needed to determine the strength of this association. Rifaximin resistance has evolved in AIEC and should be evaluated before widespread use is adopted[11].
In summary, this study by Prantera et al[1] offers important results and safety data for the use of rifaximin and supports the role for this anti-microbial in improving remission rates in mild to moderate CD. Hard endpoints including mucosal healing and measurements of systemic inflammation will enable crucial evaluation of the efficacy of rifaximin in phase 3 trials. Further analysis of the microbial alterations during rifaximin therapy are important in not only understanding the biology of the microbiome in IBD, but also in designing rational therapeutic strategies for microbial manipulation. Disease location, systemic inflammatory markers, host genotype, and intestinal microbial signatures will ultimately guide a personalized medical approach to the clinical use of directed antimicrobial and/or bacteriotherapy. Although many questions of mechanism and durability remain, Prantera et al[1] offer an important step forward in the role for microbial manipulation in the clinical management of IBD.
Footnotes
P- Reviewers Tarnawski AS, Bonino F S- Editor Gou SX L- Editor A E- Editor Xiong L
References
- 1.Prantera C, Lochs H, Grimaldi M, Danese S, Scribano ML, Gionchetti P. Rifaximin-extended intestinal release induces remission in patients with moderately active Crohn’s disease. Gastroenterology. 2012;142:473–481.e4. doi: 10.1053/j.gastro.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 2.Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA. 2007;104:13780–13785. doi: 10.1073/pnas.0706625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Willing BP, Dicksved J, Halfvarson J, Andersson AF, Lucio M, Zheng Z, Järnerot G, Tysk C, Jansson JK, Engstrand L. A pyrosequencing study in twins shows that gastrointestinal microbial profiles vary with inflammatory bowel disease phenotypes. Gastroenterology. 2010;139:1844–1854.e1. doi: 10.1053/j.gastro.2010.08.049. [DOI] [PubMed] [Google Scholar]
- 4.Scarpignato C, Pelosini I. Experimental and clinical pharmacology of rifaximin, a gastrointestinal selective antibiotic. Digestion. 2006;73 Suppl 1:13–27. doi: 10.1159/000089776. [DOI] [PubMed] [Google Scholar]
- 5.Baumgart M, Dogan B, Rishniw M, Weitzman G, Bosworth B, Yantiss R, Orsi RH, Wiedmann M, McDonough P, Kim SG, et al. Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn’s disease involving the ileum. ISME J. 2007;1:403–418. doi: 10.1038/ismej.2007.52. [DOI] [PubMed] [Google Scholar]
- 6.Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux JJ, Blugeon S, Bridonneau C, Furet JP, Corthier G, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA. 2008;105:16731–16736. doi: 10.1073/pnas.0804812105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atarashi K, Tanoue T, Shima T, Imaoka A, Kuwahara T, Momose Y, Cheng G, Yamasaki S, Saito T, Ohba Y, et al. Induction of colonic regulatory T cells by indigenous Clostridium species. Science. 2011;331:337–341. doi: 10.1126/science.1198469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olszak T, An D, Zeissig S, Vera MP, Richter J, Franke A, Glickman JN, Siebert R, Baron RM, Kasper DL, et al. Microbial exposure during early life has persistent effects on natural killer T cell function. Science. 2012;336:489–493. doi: 10.1126/science.1219328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frank DN, Robertson CE, Hamm CM, Kpadeh Z, Zhang T, Chen H, Zhu W, Sartor RB, Boedeker EC, Harpaz N, et al. Disease phenotype and genotype are associated with shifts in intestinal-associated microbiota in inflammatory bowel diseases. Inflamm Bowel Dis. 2011;17:179–184. doi: 10.1002/ibd.21339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ananthakrishnan AN, Binion DG. Impact of Clostridium difficile on inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2010;4:589–600. doi: 10.1586/egh.10.55. [DOI] [PubMed] [Google Scholar]
- 11.Dogan B, Scherl E, Bosworth B, Yantiss R, Altier C, McDonough PL, Jiang ZD, Dupont HL, Garneau P, Harel J, et al. Multidrug Resistance Is Common in Escherichia coli Associated with Ileal Crohn’s Disease. Inflamm Bowel Dis. 2013;19:141–150. doi: 10.1002/ibd.22971. [DOI] [PubMed] [Google Scholar]
- 12.Afdhal NH, Long A, Lennon J, Crowe J, O’Donoghue DP. Controlled trial of antimycobacterial therapy in Crohn’s disease. Clofazimine versus placebo. Dig Dis Sci. 1991;36:449–453. doi: 10.1007/BF01298873. [DOI] [PubMed] [Google Scholar]
- 13.Sutherland L, Singleton J, Sessions J, Hanauer S, Krawitt E, Rankin G, Summers R, Mekhjian H, Greenberger N, Kelly M. Double blind, placebo controlled trial of metronidazole in Crohn’s disease. Gut. 1991;32:1071–1075. doi: 10.1136/gut.32.9.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prantera C, Kohn A, Mangiarotti R, Andreoli A, Luzi C. Antimycobacterial therapy in Crohn’s disease: results of a controlled, double-blind trial with a multiple antibiotic regimen. Am J Gastroenterol. 1994;89:513–518. [PubMed] [Google Scholar]
- 15.Steinhart AH, Feagan BG, Wong CJ, Vandervoort M, Mikolainis S, Croitoru K, Seidman E, Leddin DJ, Bitton A, Drouin E, et al. Combined budesonide and antibiotic therapy for active Crohn’s disease: a randomized controlled trial. Gastroenterology. 2002;123:33–40. doi: 10.1053/gast.2002.34225. [DOI] [PubMed] [Google Scholar]
- 16.Arnold GL, Beaves MR, Pryjdun VO, Mook WJ. Preliminary study of ciprofloxacin in active Crohn’s disease. Inflamm Bowel Dis. 2002;8:10–15. doi: 10.1097/00054725-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Prantera C, Lochs H, Campieri M, Scribano ML, Sturniolo GC, Castiglione F, Cottone M. Antibiotic treatment of Crohn’s disease: results of a multicentre, double blind, randomized, placebo-controlled trial with rifaximin. Aliment Pharmacol Ther. 2006;23:1117–1125. doi: 10.1111/j.1365-2036.2006.02879.x. [DOI] [PubMed] [Google Scholar]
- 18.Selby W, Pavli P, Crotty B, Florin T, Radford-Smith G, Gibson P, Mitchell B, Connell W, Read R, Merrett M, et al. Two-year combination antibiotic therapy with clarithromycin, rifabutin, and clofazimine for Crohn’s disease. Gastroenterology. 2007;132:2313–2319. doi: 10.1053/j.gastro.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 19.Leiper K, Martin K, Ellis A, Watson AJ, Morris AI, Rhodes JM. Clinical trial: randomized study of clarithromycin versus placebo in active Crohn’s disease. Aliment Pharmacol Ther. 2008;27:1233–1239. doi: 10.1111/j.1365-2036.2008.03661.x. [DOI] [PubMed] [Google Scholar]


