Abstract
AIM: To investigate potential therapeutic recommendations for endoscopic and surgical resection of T1a/T1b esophageal neoplasms.
METHODS: A thorough search of electronic databases MEDLINE, Embase, Pubmed and Cochrane Library, from 1997 up to January 2011 was performed. An analysis was carried out, pooling the effects of outcomes of 4241 patients enrolled in 80 retrospective studies. For comparisons across studies, each reporting on only one endoscopic method, we used a random effects meta-regression of the log-odds of the outcome of treatment in each study. “Neural networks” as a data mining technique was employed in order to establish a prediction model of lymph node status in superficial submucosal esophageal carcinoma. Another data mining technique, the “feature selection and root cause analysis”, was used to identify the most important predictors of local recurrence and metachronous cancer development in endoscopically resected patients, and lymph node positivity in squamous carcinoma (SCC) and adenocarcinoma (ADC) separately in surgically resected patients.
RESULTS: Endoscopically resected patients: Low grade dysplasia was observed in 4% of patients, high grade dysplasia in 14.6%, carcinoma in situ in 19%, mucosal cancer in 54%, and submucosal cancer in 16% of patients. There were no significant differences between endoscopic mucosal resection and endoscopic submucosal dissection (ESD) for the following parameters: complications, patients submitted to surgery, positive margins, lymph node positivity, local recurrence and metachronous cancer. With regard to piecemeal resection, ESD performed better since the number of cases was significantly less [coefficient: -7.709438, 95%CI: (-11.03803, -4.380844), P < 0.001]; hence local recurrence rates were significantly lower [coefficient: -4.033528, 95%CI: (-6.151498, -1.915559), P < 0.01]. A higher rate of esophageal stenosis was observed following ESD [coefficient: 7.322266, 95%CI: (3.810146, 10.83439), P < 0.001]. A significantly greater number of SCC patients were submitted to surgery (log-odds, ADC: -2.1206 ± 0.6249 vs SCC: 4.1356 ± 0.4038, P < 0.05). The odds for re-classification of tumor stage after endoscopic resection were 53% and 39% for ADC and SCC, respectively. Local tumor recurrence was best predicted by grade 3 differentiation and piecemeal resection, metachronous cancer development by the carcinoma in situ component, and lymph node positivity by lymphovascular invasion. With regard to surgically resected patients: Significant differences in patients with positive lymph nodes were observed between ADC and SCC [coefficient: 1.889569, 95%CI: (0.3945146, 3.384624), P < 0.01). In contrast, lymphovascular and microvascular invasion and grade 3 patients between histologic types were comparable, the respective rank order of the predictors of lymph node positivity was: Grade 3, lymphovascular invasion (L+), microvascular invasion (V+), submucosal (Sm) 3 invasion, Sm2 invasion and Sm1 invasion. Histologic type (ADC/SCC) was not included in the model. The best predictors for SCC lymph node positivity were Sm3 invasion and (V+). For ADC, the most important predictor was (L+).
CONCLUSION: Local tumor recurrence is predicted by grade 3, metachronous cancer by the carcinoma in-situ component, and lymph node positivity by L+. T1b cancer should be treated with surgical resection.
Keywords: Superficial esophageal cancer, Endoscopic resection, Mucosal infiltration, Submucosal involvement, Recurrent tumor, Controversies in treatment, Squamous cell carcinoma, Adenocarcinoma, Lymphatic invasion, Vascular invasion, Submucosal layer, Superficial submucosal layer, Middle third submucosal layer, Deep third submucosal layer, Esophageal cancer, Endoscopic gastrointestinal surgical procedures, Endoscopic gastrointestinal surgery, Lymph node dissection, Dysplasia
INTRODUCTION
Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD), in addition to local ablation techniques, are now more extensively employed for the management of early adenocarcinoma (ADC) or squamous cell carcinoma (SCC) of the esophagus. The aim of endoscopic resection is to maintain the integrity of the esophagus and avoid the considerable morbidity and mortality of esophagectomy[1].
Several cohort studies[2-5] suggest the use of EMR or ESD for T1a esophageal neoplasia (including high grade dysplasia, adenocarcinoma, or squamous-cell carcinoma) confined to the superficial mucosa and not extending into the muscularis mucosa. Other studies contemplate endoscopic resection, even in muscularis mucosa invasion and in selected cases where upper third submucosal involvement is present[6]. T1b disease may be treated by esophagectomy.
At present, there are no reliable pre-excision molecular, biological or immunohistochemical predictive markers of lymph node metastasis in T1 esophageal cancer. Moreover, the current diagnostic workup has a low diagnostic performance for N1-disease which is considered the most influential predictor of long term prognosis[7].
The pros and cons of each endoscopic resection method have yet to be established, and level I evidence of their safety and efficacy is missing from the literature. Predictive markers of lymph node metastasis in mucosal and submucosal esophageal cancer are also an unsolved issue.
Answers to the aforementioned issues might enable researchers to formulate curative treatment strategies and considerations for neoadjuvant referral in early esophageal carcinoma cases.
The objectives of this study were: (1) to compare the safety and efficacy of EMR and ESD in the management of early esophageal neoplasia; (2) to investigate their role as part of the diagnostic workup; (3) to establish predictors of lymph node status, local recurrence and metachronous cancer development in superficial esophageal carcinoma; and (4) to investigate potential therapeutic recommendations.
MATERIALS AND METHODS
Literature search
Medline, Embase, Pub Med and the Cochrane Library databases were searched for articles in the English language from 1997 up to 2011. The following search terms were used: Early esophageal cancer, esophageal dysplasia, high grade dysplasia, low grade dysplasia, intraepithelial neoplasia, Barrett’s esophagus, superficial esophageal cancer, mucosal esophageal cancer, submucosal esophageal cancer, intramucosal/submucosal carcinoma of the esophagus, esophageal adenocarcinoma, esophageal squamous cell carcinoma, adjuvant treatment, T1a, T1b, T1m and T1sm. Terms were combined with “and/or” and asterisks. References from included studies were examined for additional studies. The main reasons for initial exclusion included animal studies, non-English literature, case reports, reviews and double publications. Figure 1 shows the process and stages throughout the review of the studies included.
Figure 1.
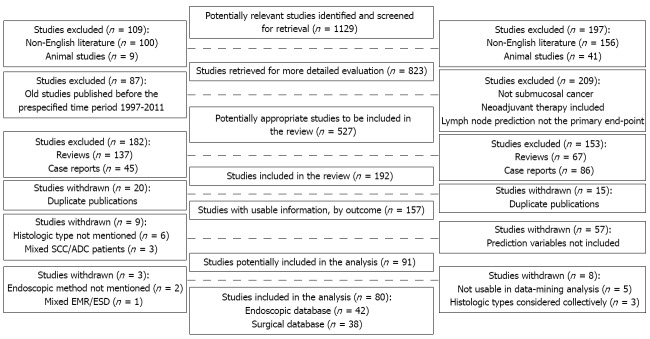
Progress through the stages of study review included. SCC: Squamous cell carcinoma; ADC: Adenocarcinoma; EMR: Endoscopic mucosal resection; ESD: Endoscopic submucosal dissection.
Inclusion and exclusion criteria for the endoscopic database
Inclusion: (1) Application of EMR and/or ESD for early esophageal cancer; (2) Low-grade dysplasia or high grade dysplasia (HGD) in the setting of Barrett’s esophagus as well as early esophageal cancer; and (3) Siewert I and II tumors.
Exclusion: (1) Studies involving previously untreated patients (no neoadjuvant therapy); (2) Studies including patients with Siewert type III, and with metastatic disease; and (3) Studies including patients with tumors other than ADC/SCC.
Inclusion and exclusion criteria for the surgically resected patients’ database
Inclusion: (1) Information from the pathology reports after esophagectomy for submucosal carcinoma with curative intent; (2) Studies including patients with esophagogastric junction carcinoma were eligible for analysis; and (3) Studies providing separate data for SCC and ADC.
Exclusion: (1) Studies administering neo-adjuvant treatment; (2) Studies involving patients with distant metastasis; (3) Case reports; (4) Mixed data for SCC and ADC; and (5) Mixed data for T1a and T1b tumors and/or surveillance of patients with dysplasia.
Data extraction
The two authors independently selected studies for inclusion and exclusion and reached a consensus when there was initial disagreement. The parameters ascertained included authors, journal and year of publication, total number of patients, type of estrogen receptor (ER) involved, final pathology results, histological type, tumor diameter, tumor location, pattern of growth, degree of differentiation, depth of tumor invasion, lymph node status, presence of lymphatic or venous invasion, as well as positive resection margins on the pathology specimen, number of patients with local recurrence, presence of metachronous lesions, and additional therapies necessary beyond ER, including surgery.
Definitions
Submucosal lesions were classified as Sm1 for tumors invading the more superficial layer of the submucosa (corresponding to one-third of its thickness), Sm2 for those invading the middle third, and Sm3 for those invading the deeper submucosal layer[8].
Statistical analysis
For comparisons across studies, each reporting on only one treatment/histologic type, we used a random effects meta-regression of the log-odds of the outcome of treatment in each study. In this case, we estimated the variance of each study-specific log-odds as the sum of the reciprocals of the number of successes and failures. Counts of 0 were replaced by 0.5.
Statistical analysis for comparisons across studies was performed using the “metareg command” of STATA/SE 11. To address multiple testing (calculate P values for covariates) the “permute option” based on a Monte Carlo permutation test of STATA/SE 11 was used.
“Neural networks” as a data mining technique[9] was employed in order to establish a prediction model of lymph node status in superficial submucosal esophageal carcinoma and find a simple model to fit the data better. The definition of a linear network was followed by training of the network. The data set was divided into three subsets: training, selection, and test cases in the proportions 3:1:1 between the training, selection, and test subsets.
Another data mining technique, the “feature selection and root cause analysis”, was used to identify the most important predictors of local recurrence and metachronous cancer development in endoscopically resected patients, and lymph node positivity in SCC and ADC separately in surgically resected patients.
In brief, this test provides extremely useful shortcuts for identifying root causes for the values observed in the outcome variables under investigation (e.g., an indicator of quality or process yield); final selections of predictors are not biased in favor of any particular model (fitted to the data for the selected predictors).
The statistical programs used were: STATA/SE 11 (Statacorp LP 4905 Lakeway Drive College Station TX 77845, United States), the NCSS 2007 and GESS 2006 version 07.1.13, (Kaysville, Utah, United States) and Statistica release 7 (Stat Soft Inc., Tulsa, United States).
RESULTS
Endoscopically resected patients
Forty-two studies[6,10-50] were selected (Table 1) which included a total of 2092 patients. Low grade dysplasia was observed in 4% of patients, high grade dysplasia in 14.6%, carcinoma in situ in 19%, mucosal cancer in 54%, and submucosal cancer in 16% of patients. Histologic types were SCC in 23 studies and ADC in 19 studies.
Table 1.
Forty-two studies were included in the analysis of endoscopically resected patients
| Author | EMR/ESD | Patients | Surgery | ADC/SCC | Positive resection margin | Other therapy | Local recurrence | Meta-chronous | N (+) | L (+) | Re-classification | Grade 3 | In situ | Piecemeal resection |
| Buttar et al[10] | EMR | 17 | 0 | ADC | 3 | PDT | 8 | 0 | ||||||
| Chaves et al[11] | ESD | 5 | SCC | 0 | 0 | 3 | 1 | |||||||
| Chennat et al[12] | EMR | 49 | 3 | ADC | 0 | 22 | 0 | |||||||
| Ciocirlan et al[13] | EMR | 51 | 2 | SCC | 14 | CHEMO | 8 | 2 | 0 | 4 | 36 | |||
| Conio et al[14] | EMR | 39 | 3 | ADC | 0 | 1 | 2 | 10 | 5 | 0 | ||||
| Ell et al[15] | EMR | 64 | 5 | ADC | PDT/APC | 6 | 3 | 6 | 6 | 0 | ||||
| Espinel et al[16] | EMR | 4 | 1 | ADC | 1 | 0 | 0 | |||||||
| Fujishiro et al[17] | ESD | 43 | SCC | 7 | 1 | 1 | 1 | 24 | 0 | |||||
| Gerke et al[18] | EMR | 41 | ADC | 9 | RFA | 3 | 0 | 0 | ||||||
| Goda et al[19] | EMR | 58 | 1 | SCC | CRT | 1 | 0 | |||||||
| Higuchi et al[20] | EMR | 20 | 0 | SCC | 6 | CRT/APC | 0 | 0 | 0 | 6 | 1 | 0 | ||
| Hull et al[52] | EMR | 10 | ADC | 2 | 0 | |||||||||
| Iguchi et al[21] | EMR | 8 | 1 | SCC | 0 | 4 | ||||||||
| Ishihara et al[22] | EMR/ESD | 70 | SCC | CRT | 12 | 0 | 40 | |||||||
| Ishii et al[23] | ESD | 35 | 1 | SCC | 2 | CHEMO | 0 | 1 | 28 | 0 | ||||
| Larghi et al[24] | EMR | 40 | 5 | ADC | PDT/APC | 0 | 6 | 19 | ||||||
| Lewis et al[25] | EMR | 100 | 1 | ADC | 1 | PDT | 1 | 8 | ||||||
| Lin et al[26] | EMR | 9 | 1 | SCC | 0 | 1 | 0 | 0 | 1 | 0 | 7 | |||
| Lopes et al[27] | EMR | 41 | 1 | ADC | APC/CRT | 4 | 2 | 14 | 2 | |||||
| Maish et al[28] | EMR | 7 | 7 | ADC | 1 | 0 | 4 | 0 | ||||||
| Manner et al[6] | EMR/ESD | 21 | 1 | ADC | 27 | APC | 3 | 2 | 0 | 0 | 0 | |||
| Naritaka et al[29] | EMR | 13 | 1 | SCC | 2 | RT | 1 | 7 | 9 | |||||
| Nijhawan et al[30] | EMR | 25 | 2 | ADC | PDT | 0 | 11 | |||||||
| Noguchi et al[31] | EMR | 33 | 5 | SCC | CRT | 0 | 5 | 14 | 15 | |||||
| Nomura et al[32] | EMR | 51 | 1 | SCC | CRT | 4 | 30 | 41 | ||||||
| Nonaka et al[33] | ESD | 25 | 1 | SCC | 3 | RT/CRT | 0 | 10 | 0 | 0 | ||||
| Ohashi et al[90] | EMR | 179 | SCC | 13 | 68 | |||||||||
| Ono et al[34] | ESD | 84 | 9 | SCC | 7 | CRT | 1 | 2 | 2 | 0 | 0 | |||
| Ota et al[35] | EMR | 18 | 0 | SCC | 5 | CRT | 0 | 4 | 11 | 3 | 0 | |||
| Pech et al[3] | EMR/ESD | 39 | SCC | 20 | PDT/CHEMO | 5 | 2 | 7 | 1 | 10 | ||||
| Peters et al[53] | EMR/ESD | 141 | ADC | 37 | 1 | 73 | 14 | |||||||
| Pouw et al[37] | EMR/ESD | 34 | 1 | ADC | APC | 3 | 14 | 10 | ||||||
| Prasad et al[39] | EMR | 25 | 25 | ADC | 17 | 5 | 16 | |||||||
| Repici et al[51] | ESD | 20 | 2 | SCC | 1 | 0 | 0 | 1 | 2 | 3 | 0 | |||
| Scheil-Bertram et al[40] | EMR | 16 | 16 | ADC | 16 | 1 | ||||||||
| Schröder et al[41] | EMR | 16 | ADC/SCC | 9 | 3 | 13 | 1 | |||||||
| Shimizu et al[42] | EMR | 82 | SCC | APC | 2 | 12 | 16 | |||||||
| Takeo et al[44] | EMR | 29 | 5 | 0 | 0 | 15 | 10 | |||||||
| Tanabe et al[46] | EMR | 85 | 0 | SCC | 15 | APC/CRT | 5 | 0 | 41 | |||||
| Teoh et al[47] | EMR/ESD | 28 | SCC | 6 | RT/CRT | 1 | 1 | |||||||
| Urabe et al[48] | EMR/ESD | 122 | SCC | 6 | 56 | |||||||||
| Vieth et al[54] | EMR | 295 | ADC | 210 | 10 | 22 | ||||||||
| Yokoyama et al[49] | EMR | 17 | 0 | SCC | RT | 7 | ||||||||
| Zehetner et al[50] | EMR | 28 | 3 | ADC | 0 | RFA | 5 | 3 | 2 | 2 |
EMR: Endoscopic mucosal resection; ESD: Endoscopic submucosal dissection; SCC: Squamous carcinoma; ADC: Adenocarcinoma; APC: Argon plasma coagulation; PDT: Photodynamic therapy; CRT: Chemoradiation therapy; RFA: Radiofrequency ablation; RT: Radiology; CHEMO: Chemotherapy.
EMR was employed in 29 studies and ESD in 6 studies. Both EMR and ESD were used in 7 studies. Lymphovascular invasion was found to range from 0%-30%, microvascular invasion was observed in 0%-33% of patients, and 7.4% of patients were poorly differentiated.
Argon plasma coagulation (APC) as the only modality was used in 3 studies[6,37,42]. In addition to APC, 2 studies[15,24] also utilized photodynamic therapy (PDT) and 3 studies added chemoradiation therapy (CRT)[20,27,46]. Adjuvant only CRT was administered in 6 studies[19,22,31,32,34,35], radiotherapy only in 2[29,49], radiotherapy and CRT in 2[33,47], PDT only in 3[10,25,30], chemotherapy only in 2[13,23], and PDT/chemotherapy in one study[4]. Radiofrequency ablation was used in 2 studies[18,50]. Mean follow-up time varied from 12 to 62 mo and median follow-up time ranged from 7 to 39 mo.
Lymph node metastasis
Eleven studies[4,20,25,26,28,31,34,35,38,40,51] provided data on lymph node metastasis. Thirty-one patients out of 371 were node-positive. The overall increase in the odds was 5% for ADC and approximately 1% for SCC. No significant differences were observed between either ADC vs SCC or EMR vs ESD patients (Tables 2 and 3). Lymphovascular invasion was found to be the only predictor of lymph node metastasis (F value: 416.45, P < 0.001).
Table 2.
Meta-regression analysis of the methods of endoscopic resection according to the published studies (the random effects model was used)
| EMR vs ESD | Coefficient | 95%CI | P value | Favors |
| Patients submitted to surgery | 0.401 | -2.912964, 3.714436 | 0.806 | None |
| Positive margin | -0.741 | -3.362995, 1.881024 | 0.558 | None |
| Local recurrence | -1.713 | -4.420582, 0.9937198 | 0.201 | None |
| Lymph node metastasis | 0.905 | -5.762587, 7.573427 | 0.762 | None |
| Metachronous cancer | -1.804 | -4.350273, 0.7420371 | 0.143 | None |
| Procedural complications | 1.397 | -1.264597, 4.058631 | 0.289 | None |
| Stenosis | 7.322 | 3.810146, 10.83439 | < 0.001 | EMR |
| Piecemeal resection1 | ||||
| Number of cases | -7.709 | -11.03803, -4.380844 | < 0.001 | ESD |
| Local recurrence | -4.034 | -6.151498, -1.915559 | < 0.01 | ESD |
| Resection margins | 0.837 | -3.725993, 5.39999 | 0.678 | None |
Data available only for squamous cell carcinoma studies. EMR: Endoscopic mucosal resection; ESD: Endoscopic submucosal dissection.
Table 3.
Meta-regression analysis of the outcomes of endoscopic resection according to the histologic type of early esophageal cancer (the random effects model was used)
| Outcome | Histologic type | Log-odds ratio | SE | 95.0% lower confidence limit | 95.0% upper confidence limit | Odds | Favors |
| Patients submitted to surgery | ADC | -2.1206 | 0.6249 | -3.3454 | -0.8958 | 12% | ADC |
| SCC | 4.1356 | 0.4038 | -4.9271 | -3.3440 | 37% | P < 0.05 | |
| Positive margins | ADC | -2.3761 | 1.0181 | -4.3716 | -0.3806 | 9% | None |
| SCC | -2.5689 | 0.6973 | -3.9357 | -1.2022 | 7% | ||
| Local recurrence | ADC | -4.8189 | 0.1469 | -5.1068 | -4.5309 | 0.80% | None |
| SCC | -4.3347 | 0.2792 | -4.8819 | -3.7874 | 1% | ||
| Lymph node metastasis | ADC | -3.0565 | 0.7714 | -4.5685 | -1.5445 | 5% | None |
| SCC | -4.7682 | 0.4413 | -5.6332 | -3.9032 | 0.90% | ||
| Metachronous cancer | ADC | -2.8017 | 0.2384 | -3.2690 | -2.3344 | 6% | None |
| SCC | -4.6030 | 0.6059 | -5.7905 | -3.4155 | 1% | ||
| Pre- vs post-endoscopic tumor stage | ADC | -0.5449 | 0.4316 | -1.3909 | 0.3011 | 53% | - |
| SCC | -0.8267 | 0.3324 | -1.4782 | -0.1752 | 39% |
SCC: Squamous cell carcinoma; ADC: Adenocarcinoma.
Differences between pre- and post-endoscopic resection tumor staging
Eighteen studies[10,12,14-16,24-28,30,31,33,37,38,44,52,53] including 685 patients reported differences between pre- and post-endoscopic resection tumor staging in 235 cases. These differences were mainly due to either the histological assessment (HGD vs carcinoma) and/or tumor depth of invasion (Table 3). Patients treated with both endoscopic methods and subsequently submitted to surgery due to unfavorable tumor characteristics did not differ significantly (Figure 2A), although SCC patients were statistically more likely to be referred for surgery. The combined odds were 53% and 39% for ADC and SCC, respectively.
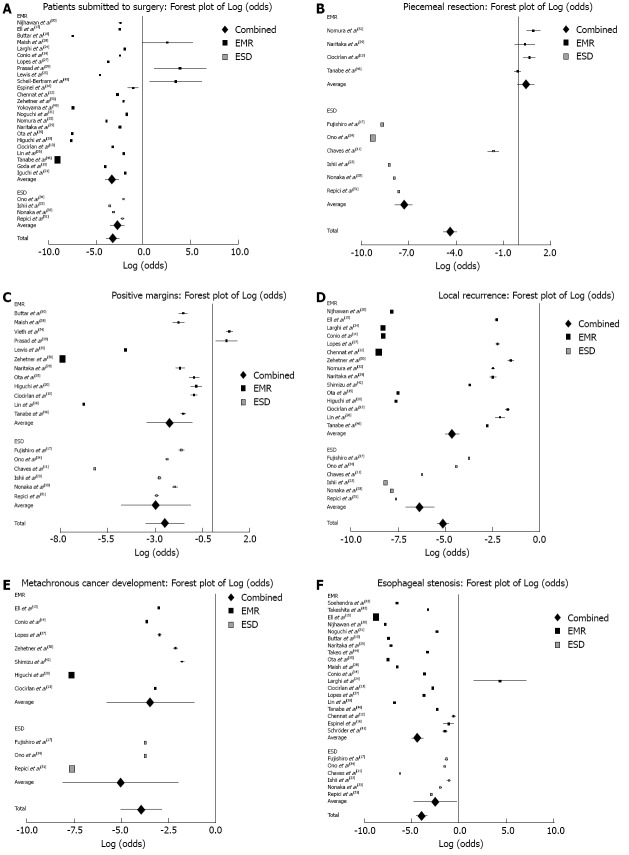
Figure 2.
Forest plot of log-odds in both groups (endoscopic mucosal resection and endoscopic submucosal dissection): No statistically significant differences were observed. A: Forest plot of log-odds patients submitted to surgery; B: Forest plot of log-odds of piecemeal resected patients; C: Forest plot of log-odds of positive resection margins patients; D: Forest plot of log-odds of local recurrence in both groups [endoscopic mucosal resection and endoscopic submucosal dissection (EMR-ESD)]: No statistically significant differences were observed, with the exception of piecemeal resected patients. In this last instance ESD was more efficient; E: Forest plot of log-odds of metachronous cancer development; F: Forest plot of log-odds of esophageal stenosis in both groups (EMR-ESD): EMR was less destructive.
Piecemeal resection
Piecemeal resection was accomplished in 48% (732/1516) of cases. Ten studies[11,13,17,23,29,32-34,46,51] reporting piecemeal resection cases (n = 412) additionally provided the number of lesions (n = 466) per patient, number of patients with positive margins (n = 36) and local recurrence rates (n = 20 patients). All the aforementioned 10 studies enrolled SCC patients. Piecemeal resection and local recurrence rates were statistically significantly lower when performing ESD (Tables 2 and 3; Figure 2B). In contrast, positive margins did not differ significantly between the two endoscopic methods.
Resection margins
Eighteen studies[10,11,13,17,20,23,25,26,28,29,33-35,38,46,50,51,54] reported outcomes concerning specimen margin status. Thirty-three per cent (294/880) of cases demonstrated positive margins. Positive margin data were from primary endoscopic resection. The overall increase in the odds was 9% for ADC and approximately 7% for SCC. No significant differences on positive resection margins were observed between either ADC vs SCC or EMR vs ESD patients (Tables 2 and 3; Figure 2C).
Monte Carlo permutation adjusted testing for meta-regression disclosed that local recurrence in patients with positive resection margins was independent of endoscopic resection modality (EMR/ESD, P = 1.000), histologic type (ADC/SCC, P = 0.972) and type of adjuvant therapy (chemo/CRT/APC/RT/PDT, P = 0.899). Data mining showed that grade 3 was an independent predictor of local recurrence in cases with positive margins (P < 0.001).
Local recurrence
Local recurrence among 30 studies[3,6,11-15,17,20,22-24,26,27,29,30,32-35,37,42,46-48,50,51] which provided relevant data ranged from 0-17%. The combined odds were 0.8% and 1% for ADC and SCC, respectively. No significant differences were observed between either ADC vs SCC or EMR vs ESD patients (Tables 2 and 3; Figure 2D). Data mining showed that grade 3 was an independent predictor of local recurrence (F value: 16.2, P < 0.05). In cases of piecemeal resection, local recurrence was significantly higher when performing EMR (F value: 5.39, P < 0.01).
Development of metachronous lesions
Development of metachronous lesions ranged from 2%-14% in 10 studies[6,13-15,17,20,27,34,42,50,51]. The combined odds were 6% and 1% for ADC and SCC, respectively. No significant differences were observed between either ADC vs SCC or EMR vs ESD patients (Tables 2 and 3; Figure 2E). Data mining showed that the presence of carcinoma in situ was an independent predictor of metachronous lesion development (F value: 62.5, P < 0.01).
Procedural and late morbidity
Twenty-five studies[10-17,23,24,26-31,33-35,41,43-46,51] provided satisfactory data on procedural morbidity and late complications. Procedural morbidity included bleeding managed conservatively in 5.8%, bleeding requiring intervention in 0.6%, perforation 1.8% and pain in 4.2% of patients. Esophageal stenosis was experienced by 12.2% of patients. No significant differences in procedural complications were observed between EMR vs ESD patients. In contrast, esophageal stenosis was statistically more prevalent among patients managed with ESD (P < 0.001) (Tables 2 and 3; Figure 2F).
Surgically resected patients
Of 677 screened studies, 38 studies comprising a total of 2149 participants were finally included[20,31,40,55-86].
The magnitude of kappa (0.86) reflected adequate agreement between the two reviewers. All 38 studies provided data on lymph node metastasis. The histological parameters of patients are presented in Table 4. Eight-hundred and eighty-eight (888) patients among 2149 were node-positive. Significant differences in patients with positive lymph nodes were observed between ADC and SCC (P < 0.01). In contrast, lymphovascular and microvascular invasion and grade 3 patients between histologic types were comparable (Table 5). Grade 3 patients were seen in 24% (158/663) with SCC and in 49% (267/541) with ADC.
Table 4.
Thirty-eight studies were included in the analysis of surgically resected patients
| Study | SCC/ADC | sm | sm1 | sm2 | sm3 | N+ sm | N+ sm1 | N+ sm2 | N+ sm3 | L+ sm | L+ sm1 | L+ sm2 | L+ sm3 | V+ sm | V+ sm1 | V+ sm2 | V+ sm3 | Grade III |
| Amano et al[55] | SCC | 83 | 10 | 10 | 63 | 47 | 4 | 4 | 39 | 15 | 23 | 6 | ||||||
| Araki et al[56] | SCC | 58 | 12 | 18 | 28 | 15 | 1 | 4 | 10 | 12 | 0 | 4 | 8 | 6 | 0 | 2 | 4 | |
| Bollschweiler et al[57] (ADC) | ADC | 22 | 9 | 4 | 9 | 9 | 2 | 0 | 7 | 5 | ||||||||
| Bollschweiler et al[57] (SCC) | SCC | 22 | 3 | 6 | 13 | 11 | 1 | 1 | 9 | 8 | ||||||||
| Buskens et al[58] | ADC | 42 | 16 | 13 | 13 | 12 | 0 | 3 | 9 | 16 | 0 | 4 | 12 | 17 | ||||
| Cen et al[59] | ADC | 51 | 12 | 14 | 20 | |||||||||||||
| Chino et al[91] | SCC | 22 | 5 | 8 | 9 | 11 | 1 | 6 | 4 | 17 | 5 | 6 | 6 | 6 | 0 | 2 | 4 | |
| Eguchi et al[61] | SCC | 364 | 32 | 196 | 17 | 11 | 11 | |||||||||||
| Endo et al[92] | SCC | 121 | 18 | 48 | 55 | 51 | 2 | 15 | 34 | 95 | 6 | 35 | 54 | |||||
| Gockel et al[63] | ADC | 15 | 8 | 2 | 5 | 3 | 1 | 1 | 1 | |||||||||
| Gockel et al[63] | SCC | 15 | 7 | 4 | 4 | 2 | 1 | 1 | 0 | |||||||||
| Goseki et al[64] | SCC | 30 | 15 | 21 | 22 | 8 | ||||||||||||
| Higuchi et al[20] | SCC | 15 | 15 | 3 | 3 | 14 | 14 | 7 | 7 | |||||||||
| Ide et al[65] | SCC | 85 | 26 | 54 | 23 | |||||||||||||
| Ikeda et al[66] | SCC | 45 | 19 | 23 | ||||||||||||||
| Kim et al[67] | SCC | 133 | 36 | 27 | 69 | 39 | 6 | 5 | 28 | 30 | 18 | |||||||
| Kimura et al[68] | SCC | 26 | 9 | 11 | 5 | |||||||||||||
| Kuwano et al[93] | SCC | 26 | 4 | 2 | 20 | 10 | 18 | 10 | 6 | |||||||||
| Liu et al[71] | ADC | 37 | 10 | 15 | 0 | |||||||||||||
| Makuuchi et al[72] | SCC | 81 | 18 | 25 | 38 | 33 | 4 | 11 | 18 | 60 | 13 | 19 | 28 | 31 | 2 | 9 | 20 | |
| Matsumoto et al[73] | SCC | 87 | 15 | 26 | 46 | 41 | 48 | 26 | ||||||||||
| Nakajima et al[74] | SCC | 84 | 9 | 29 | 46 | 33 | 0 | 5 | 28 | 60 | 42 | 9 | ||||||
| Natsugoe et al[75] | SCC | 92 | 21 | 28 | 43 | 42 | 6 | 11 | 25 | 51 | 25 | 21 | ||||||
| Noguchi et al[31] | SCC | 38 | 6 | 10 | 22 | 20 | 1 | 3 | 16 | 31 | 4 | 8 | 19 | 10 | 1 | 1 | 8 | |
| Ohno et al[76] | SCC | 16 | 2 | 6 | 4 | 5 | ||||||||||||
| Paraf et al[77] | ADC | 12 | 1 | 5 | ||||||||||||||
| Rice et al[78] | ADC | 24 | 5 | 123 | ||||||||||||||
| Rice et al[78] | SCC | 3 | 1 | 13 | ||||||||||||||
| Scheil-Bertram et al[40] | ADC | 21 | 7 | 2 | 12 | 5 | 1 | 0 | 4 | 9 | 2 | 0 | 7 | 1 | 1 | 0 | 0 | 12 |
| Schmidt et al[79] | SCC | 5 | 2 | 3 | ||||||||||||||
| Shiozaki et al[81] | SCC | 180 | 21 | 73 | 86 | 92 | 8 | 37 | 47 | 119 | 11 | 51 | 57 | 45 | 3 | 18 | 24 | 54 |
| Soga et al[82] | SCC | 4 | 2 | 3 | 2 | |||||||||||||
| Tomita et al[83] | SCC | 89 | 11 | 10 | 68 | 51 | 5 | 4 | 42 | 32 | 44 | 7 | ||||||
| Tsutsui et al[84] | SCC | 38 | 8 | 17 | ||||||||||||||
| Westerterp et al[85] | ADC | 66 | 25 | 23 | 18 | 18 | 0 | 6 | 12 | 59 | ||||||||
| Yoshikane et al[86] | SCC | 17 | 12 | 11 | 4 | 1 | ||||||||||||
| Sepesi et al[80] | ADC | 29 | 14 | 11 | 4 | 9 | 3 | 4 | 2 | |||||||||
| Leers et al[70] | ADC | 51 | 19 | 9 | 23 | 11 | 4 | 1 | 6 |
SCC: Squamous cell carcinoma; ADC: Adenocarcinoma; L+: Lymphovascular invasion; V+: Microvascular invasion; sm: Submucosal layer.
Table 5.
Meta-regression analysis of histologic parameters between adenocarcinoma and squamous cell carcinoma patients according to the published studies (the random effects model was used)
| Comparison of ADC vs SCC | Coefficient | 95%CI | P value | Better status |
| Positive lymph nodes | 1.890 | 0.3945146, 3.384624 | < 0.01 | ADC |
| Lymphovascular invasion | 0.626 | -0.7032339, 1.956155 | 0.340 | None |
| Microvascular invasion | 1.114 | -0.2682334, 2.496538 | 0.108 | None |
| Grade 3 | 0.305 | -1.584654, 2.195142 | 0.731 | None |
SCC: Squamous cell carcinoma; ADC: Adenocarcinoma.
Setting up a model for prediction of lymph node metastasis
In an endeavor to set up a model to predict lymph node metastasis, we applied Neural Networks as a data mining technique. All included studies provided sufficient information on depth of tumor invasion (Sm1, Sm2, Sm3), lymphatic invasion, vascular invasion, histologic differentiation, and histologic type (SCC, ADC) (Table 6).
Table 6.
Number of patients with lymph node metastasis and lymphatic and vascular invasion according to the depth of tumor in the submucosal layer
| Patients with diseases | |||||||
| Lymph node metastasis | |||||||
| sm (38 studies: n = 2149)1 | sm1 (n = 308) | sm2 (n = 349) | sm3 (n = 624) | ||||
| SCC | ADC | SCC | ADC | SCC | ADC | SCC | ADC |
| 793/1779 (45%) | 95/370 (26%) | 60/224 (27%) | 8/84 (10%) | 107/296 (36%) | 11/53 (21%) | 301/544 (55%) | 39/80 (49%) |
| Lymphovascular invasion | |||||||
| sm (n = 1286)1 | sm1 (n = 134) | sm2 (n = 150) | sm3 (n = 209) | ||||
| 627/1090 (56%) | 76/196 (39%) | 58/111 (52%) | 2/23 (9%) | 88/135 (65%) | 4/15 (27%) | 118/184 (64%) | 19/25 (76%) |
| Microvascular invasion | |||||||
| sm (n = 1194)1 | sm1 (n = 104) | sm2 (n = 185) | sm3 (n = 251) | ||||
| 468/1161 (40%) | 6/33 (18%) | 19/97 (20%) | 1/7 (14%) | 67/183 (37%) | 0/2 (0%) | 114/239 (48%) | 0/12 (0%) |
Total numbers of patients differ since not all studies provide relevant information. sm: Submucosal layer; SCC: Squamous cell carcinoma; ADC: Adenocarcinoma.
The number of patients with positive lymph nodes was set as the dependent variable, while the respective number of patients with Sm1, Sm2, Sm3 invasion, lymphatic invasion, vascular invasion, and poor differentiation were used as continuous independent variables. The histologic type of esophageal cancer was set as a categorical variable. The linear model 5:5-1:1 emerged as the best neural network model according to its regression statistics, with the smallest error: data standard deviation ratio (0.07506; an SD ratio closer to 0.1 generally indicates very good regression performance). This was also true for the close correlation between the prediction of the independent and dependent variables (0.99774). Its format was <type = Linear> <inputs = 5> : <layer 1 = 5> - <layer 2 = 1> : <outputs = 1>, with two layers. Missing values were patched using the mean variable value.
The rank order of importance of the predictors of lymph node positivity was: Grade 3, Sm3 invasion, L(+), V(+), Sm2 invasion and Sm1 invasion, respectively. Histologic type (ADC/SCC) had a ratio network error ≤ 1, and thus should not be considered as a predictor.
Validation of the model
The data set was divided into three subsets: the training, selection, and test cases (3:1:1 in our model) in order to preclude the predictive performance of the linear model being attributed to a data over-fitting phenomenon. The predicted number of patients in various studies with positive lymph nodes by the linear model was almost identical to that observed by the authors.
Predictors of lymph node metastasis in SCC and ADC
Considering only the predictors of lymph node metastasis defined by the aforementioned linear model in each of the two histological entities (SCC, ADC), we applied another data mining technique (Feature selection and root cause analysis).
The best predictors of lymph node positivity in SCC were Sm3 invasion (P < 0.001) and microvascular invasion (P < 0.01). In relation to ADC, the most important predictor was lymphovascular invasion (P < 0.05).
DISCUSSION
According to NCCN guidelines version 1.2011 for esophageal and esophagogastric junction cancers, in the absence of evidence of lymph node metastases, lymphovascular invasion or poor differentiation grade, T1a disease can be treated with full EMR. In cases of unfavorable characteristics, the choice lies between EMR plus ablation or esophagectomy. T1b disease may be treated by esophagectomy.
The present meta-analysis: (1) investigated the particular role of each of the two endoscopic modalities in treating early esophageal cancer; (2) analyzed the issue of local recurrence and metachronous cancer development in patients treated endoscopically; and (3) analyzed for potential unfavorable tumor characteristics (besides those found by imaging) that obviate the need for neoadjuvant or perioperative therapy. To our knowledge, level I evidence related to these issues is missing from the literature. The only published meta-analysis based on retrospective studies (seven full-text and eight abstracts) compares EMR vs ESD for esophageal, gastric, and colorectal neoplasms jointly[87].
In addition to a variety of local ablation techniques, EMR and ESD are now extensively used for the treatment of stage Tis (high-grade dysplasia) and T1a ADC or SCC, aiming to reduce the considerable morbidity and mortality associated with esophagectomy.
The possibility of lymph node metastases, completeness of endoscopic resectability, early and late complications, local recurrence and development of a metachronous cancer, are concerns that should be measured when deciding whether to proceed with EMR, ESD or surgery.
According to our pooled analysis there were no significant differences between EMR and ESD for the following parameters: procedural complications, number of patients submitted to surgery, positive specimen margins, lymph node positivity, local recurrence rates and metachronous cancer development. In instances of piecemeal tumor resection, in particular, ESD performed better since the number of cases was significantly less (P < 0.001); hence, local recurrence rates were significantly lower (P < 0.01). An important point that should be kept in mind is the higher rate of esophageal stenosis observed following ESD (P < 0.001). Data on circumferential spread and tumor size were scarce among the studies.
There were no considerable differences in the application of endoscopic methods to each of the main histologic types of early esophageal cancer, other than the fact that a significantly greater number of SCC patients were submitted for surgery (P < 0.05).
Another significant finding was the high percentage of patient restaging after endoscopic intervention. EUS staging prior to proceeding with mucosal resection in the setting of carcinoma is recommended. In a recent meta-analysis[7], the pooled sensitivity (95%CI) and specificity (95%CI) for regional lymph node metastases was 0.764 (0.741-0.785) and 0.724 (0.693-0.753), respectively. The pooled diagnostic odds ratio (95%CI) was 8.001 (6.369-10.051). Although EUS has a better diagnostic performance compared to computed tomography (CT) scanning and positron emission tomography CT, the question of regional lymph node detection has yet to be satisfactorily addressed.
With regard to preoperative staging, endoscopic resection after endoscopic biopsy plays a key role. The odds for re-classification of tumor stage after endoscopic resection were 53% and 39% for ADC and SCC, respectively. This was possibly due to biopsy sampling failure, lack of adequate specimen and pathologist misinterpretation of the muscular anatomy. This obviates the need to optimize pre-treatment diagnostics and reconsider treatment strategies. The introduction of endoscopic resection in selected cases as part of the diagnostic workup should be strongly taken into consideration. This particular issue is supported by our data mining analysis: local tumor recurrence was best predicted by grade 3 differentiation and piecemeal resection, metachronous cancer development by the carcinoma in situ component and lymph node positivity by lymphovascular invasion. All the aforementioned predictors/histologic features can easily be retrieved from the EMR/ESD sample.
However, ESD is a technically demanding procedure that is not widely available. Although we were not able to perform a direct comparison of the outcomes of ESD vs surgery due to lack of relevant data, the likelihood of lymph node metastases and endoscopic resectability being factors that should be considered in deciding whether to pursue ESD or surgery is high, as stated by some authors[17]. According to our results, the presence of grade 3, piecemeal resection, the carcinoma in situ component and lymphovascular invasion would prompt surgical resection.
Available evidence from our esophagectomy series with radical lymph node dissection database suggests that the frequency of lymph node metastasis increases in proportion with tumor depth.
The diagnostic performance of sentinel lymph node biopsy for esophageal and gastric cardia cancer provides sensitivity between 75%-100% and accuracy between 78%-100%. Albeit applied in only a small number of patients, CT-lymphography seems to be the most promising method[7].
Considering the low incidence of lymph node metastasis (the odds are 5% for ADC and approximately 1% for SCC) and the absence of lymphovascular invasion in neoplasms limited to the mucosa, endoscopic resection is oncologically adequate for well-differentiated cancers, resected completely and lacking in situ foci. With regard to Barrett’s patients in particular, close endoscopic surveillance should be life-long and requires the commitment of both the patient and the physician since according to our results, the odds for lymph node metastasis are 5% and for metachronous cancer development 6%.
When endoscopic therapy for early esophageal cancer is considered, EMR or ESD should be applied first prior to the use of ablative techniques. According to our analysis, the application of ablative techniques has not gained significance as an independent predictor of local recurrence or metachronous cancer development.
Considering studies including surgically resected patients, lymph node positivity was statistically greater in SCC, while lymphovascular and microvascular invasion and grade 3 percentages were comparable between ADC and SCC patients. In rank order of importance, the predictors of lymph node metastasis in the prediction model were: Grade 3, Sm3 invasion, lymphovascular invasion, microvascular invasion, Sm2 invasion and Sm1 invasion, respectively. The best predictors of lymph node positivity in SCC were Sm3 invasion and microvascular invasion. For ADC, the most important predictor was lymphovascular invasion. According to the above, the present study supports the surgical rather than the endoscopic resection of T1b esophageal cancer, since even Sm1 invasion was included in our model. In consequence, Sm1 lesions should not be removed endoscopically. Interestingly, the presence of specific histologic features should prompt consideration of a more aggressive management, such as the use of neoadjuvant or perioperative treatment. This perception also poses the question as to the endorsement of EMR/ESD as part of the diagnostic workup.
Since there is a lack of apposite molecular-biological markers that can predict lymphatic spread in T1a and T1b-esophageal carcinoma with high diagnostic yield and the inconsistent success of the diagnostic work-up, the predictors found in our data mining analysis would possibly be of relevance in clinical decision making.
The analysis of surgically only resected patients is an updated version of an already published study by our group[88]. Although more studies have been included, the results were identical.
The current work is not without its limitations: (1) The report included studies of retrospective case series; thus, a formal meta-analysis could not be applied; (2) Parameters, such as dysplasia grade, segment length of Barrett’s and small areas of intestinal metaplasia hidden underneath neosquamous mucosa, the so-called “buried Barrett’s”, could not be analyzed due to paucity of data; (3) Overall patient survival and disease-free survival could not be assessed due to data inconsistency; (4) the type of resection (en-bloc, transhiatal, Ivor Lewis, minimally invasive) and differences according to the location of the tumor, with regard to lymph node, L and V invasion, may have influenced, to a degree, the prevalence of node positivity; and (5) in some studies, the stratification of data for distribution of the lymphovascular involvement according to the depth of tumor infiltration, and similar stratification for nodal involvement (m1, m2, m3, sm1, sm2 and sm3), were not available.
The value of patient data mining has already been established by The Medical Quality Improvement Consortium[89]. This large clinical data warehouse contains patient data including their problem lists, test results, procedures and medication lists, all of which help identify valid associations.
Currently, the National Comprehensive Cancer Network recommends an esophagectomy over endoscopic therapy for fit patients with T1b cancer. This study suggests the option of neoadjuvant treatment for those patients with unfavorable histological characteristics in terms of tumor histologic entity, aiming at a R0 resection.
In summary, according to this study, there were no significant differences between EMR and ESD concerning procedural complications, number of patients submitted to surgery, positive specimen margins, lymph node positivity, local recurrence rates and metachronous cancer development. In instances of a predicted piecemeal tumor resection, ESD performed better since the number of cases was significantly less and local recurrence rates were therefore significantly lower. A higher rate of esophageal stenosis was observed following ESD.
Local tumor recurrence after endoscopic resection was best predicted by grade 3 differentiation, metachronous cancer development by the carcinoma in situ component, and lymph node positivity by lymphovascular invasion.
T1b esophageal cancer should be managed with surgical resection and systematic lymphadenectomy since even Sm1 invasion was in the constructed model, while the histologic type and presence of specific predictors could likely alter the surgeon’s policy and perspective of multimodality management. The best predictors of lymph node positivity in SCC were Sm3 invasion and microvascular invasion. For ADC, the most important predictor was lymphovascular invasion. Prospective studies, or preferably randomized controlled trials, are needed in order to validate the refinements for patient selection made by this study.
COMMENTS
Background
Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are frequently used to treat early esophageal cancer. Esophagectomy remains the standard of treatment especially in submucosal invasion. However, there is controversy between surgeons and endoscopists as to which is the best treatment option. The literature lacks a satisfactory level of evidence with respect to T1a and T1b esophageal cancer management.
Research frontiers
The present meta-analysis: (1) Investigated the particular role of each of the two endoscopic modalities in the treatment of early esophageal cancer; (2) Analyzed the issue of local recurrence and metachronous cancer development in patients treated endoscopically; and (3) Analyzed for potential tumor lymph node positivity.
Innovations and breakthroughs
Level I evidence related to the endoscopic management of early esophageal cancer is missing from the literature. The only published meta-analysis based on retrospective studies (seven full-text and eight abstracts) compares EMR vs ESD for esophageal, gastric, and colorectal neoplasms jointly.
Applications
Potential unfavorable tumor characteristics as documented in this systematic review and meta-analysis (besides those found by imaging) may obviate the need for neoadjuvant or perioperative therapy.
Terminology
Meta-regression is a tool used in meta-analysis to examine the impact of moderator variables on study effect size using regression-based techniques. Meta-regression is more effective at this task than standard regression techniques. The random or mixed effects model allows for within study variation and between study variation and is therefore the most appropriate model to choose. A neural network is a system of programs and data structures that approximates the operation of the human brain. A neural network generally involves a large number of processors operating in parallel, each with its own small sphere of knowledge and access to data in its local memory. Typically, a neural network is initially “trained” or fed large amounts of data and rules about data relationships.
Peer review
The authors reviewed endoscopic and surgical resection of superficial esophageal neoplasms. The review was well conducted in the topic is very interesting in order to identify selection of treatment implicated in the superficial esophageal cancer.
Footnotes
P- Reviewer Tanaka S S- Editor Gou SX L- Editor Webster JR E- Editor Li JY
References
- 1.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 2.Ell C, May A, Pech O, Gossner L, Guenter E, Behrens A, Nachbar L, Huijsmans J, Vieth M, Stolte M. Curative endoscopic resection of early esophageal adenocarcinomas (Barrett’s cancer) Gastrointest Endosc. 2007;65:3–10. doi: 10.1016/j.gie.2006.04.033. [DOI] [PubMed] [Google Scholar]
- 3.Pech O, Behrens A, May A, Nachbar L, Gossner L, Rabenstein T, Manner H, Guenter E, Huijsmans J, Vieth M, et al. Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut. 2008;57:1200–1206. doi: 10.1136/gut.2007.142539. [DOI] [PubMed] [Google Scholar]
- 4.Pech O, Gossner L, May A, Vieth M, Stolte M, Ell C. Endoscopic resection of superficial esophageal squamous-cell carcinomas: Western experience. Am J Gastroenterol. 2004;99:1226–1232. doi: 10.1111/j.1572-0241.2004.30628.x. [DOI] [PubMed] [Google Scholar]
- 5.Stahl M, Budach W, Meyer HJ, Cervantes A. Esophageal cancer: Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v46–v49. doi: 10.1093/annonc/mdq163. [DOI] [PubMed] [Google Scholar]
- 6.Manner H, May A, Pech O, Gossner L, Rabenstein T, Günter E, Vieth M, Stolte M, Ell C. Early Barrett’s carcinoma with “low-risk” submucosal invasion: long-term results of endoscopic resection with a curative intent. Am J Gastroenterol. 2008;103:2589–2597. doi: 10.1111/j.1572-0241.2008.02083.x. [DOI] [PubMed] [Google Scholar]
- 7.Sgourakis G, Gockel I, Lyros O, Hansen T, Mildenberger P, Lang H. Detection of lymph node metastases in esophageal cancer. Expert Rev Anticancer Ther. 2011;11:601–612. doi: 10.1586/era.10.150. [DOI] [PubMed] [Google Scholar]
- 8.Japanese Society for Esophageal diseases. Guidelines for Clinical and Pathologic Studies: Carcinoma of the Esophagus. 9th ed. Tokyo: Kanehara and Co. Ltd; 2001. [Google Scholar]
- 9.Albrecht RF, Reeves CR, Steele NC. Artificial Neural Nets and Genetic Algorithms. Vienna: Springer-Verlag; 1993. [Google Scholar]
- 10.Buttar NS, Wang KK, Lutzke LS, Krishnadath KK, Anderson MA. Combined endoscopic mucosal resection and photodynamic therapy for esophageal neoplasia within Barrett’s esophagus. Gastrointest Endosc. 2001;54:682–688. doi: 10.1067/gien.2001.0003. [DOI] [PubMed] [Google Scholar]
- 11.Chaves DM, Maluf Filho F, de Moura EG, Santos ME, Arrais LR, Kawaguti F, Sakai P. Endoscopic submucosal dissection for the treatment of early esophageal and gastric cancer--initial experience of a western center. Clinics (Sao Paulo) 2010;65:377–382. doi: 10.1590/S1807-59322010000400005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chennat J, Konda VJ, Ross AS, de Tejada AH, Noffsinger A, Hart J, Lin S, Ferguson MK, Posner MC, Waxman I. Complete Barrett’s eradication endoscopic mucosal resection: an effective treatment modality for high-grade dysplasia and intramucosal carcinoma--an American single-center experience. Am J Gastroenterol. 2009;104:2684–2692. doi: 10.1038/ajg.2009.465. [DOI] [PubMed] [Google Scholar]
- 13.Ciocirlan M, Lapalus MG, Hervieu V, Souquet JC, Napoléon B, Scoazec JY, Lefort C, Saurin JC, Ponchon T. Endoscopic mucosal resection for squamous premalignant and early malignant lesions of the esophagus. Endoscopy. 2007;39:24–29. doi: 10.1055/s-2006-945182. [DOI] [PubMed] [Google Scholar]
- 14.Conio M, Repici A, Cestari R, Blanchi S, Lapertosa G, Missale G, Della Casa D, Villanacci V, Calandri PG, Filiberti R. Endoscopic mucosal resection for high-grade dysplasia and intramucosal carcinoma in Barrett’s esophagus: an Italian experience. World J Gastroenterol. 2005;11:6650–6655. doi: 10.3748/wjg.v11.i42.6650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ell C, May A, Gossner L, Pech O, Günter E, Mayer G, Henrich R, Vieth M, Müller H, Seitz G, et al. Endoscopic mucosal resection of early cancer and high-grade dysplasia in Barrett’s esophagus. Gastroenterology. 2000;118:670–677. doi: 10.1016/s0016-5085(00)70136-3. [DOI] [PubMed] [Google Scholar]
- 16.Espinel J, Pinedo E, Rascarachi G. Endoscopic mucosal resection with a multiband ligator for the treatment of Barrett s high-grade dysplasia and early gastric cancer. Rev Esp Enferm Dig. 2009;101:403–407. doi: 10.4321/s1130-01082009000600005. [DOI] [PubMed] [Google Scholar]
- 17.Fujishiro M, Kodashima S, Goto O, Ono S, Niimi K, Yamamichi N, Oka M, Ichinose M, Omata M. Endoscopic submucosal dissection for esophageal squamous cell neoplasms. Dig Endosc. 2009;21:109–115. doi: 10.1111/j.1443-1661.2009.00837.x. [DOI] [PubMed] [Google Scholar]
- 18.Gerke H, Siddiqui J, Nasr I, Van Handel DM, Jensen CS. Efficacy and safety of EMR to completely remove Barrett’s esophagus: experience in 41 patients. Gastrointest Endosc. 2011;74:761–771. doi: 10.1016/j.gie.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Goda K, Tajiri H, Ikegami M, Yoshida Y, Yoshimura N, Kato M, Sumiyama K, Imazu H, Matsuda K, Kaise M, et al. Magnifying endoscopy with narrow band imaging for predicting the invasion depth of superficial esophageal squamous cell carcinoma. Dis Esophagus. 2009;22:453–460. doi: 10.1111/j.1442-2050.2009.00942.x. [DOI] [PubMed] [Google Scholar]
- 20.Higuchi K, Tanabe S, Koizumi W, Sasaki T, Nakatani K, Saigenji K, Kobayashi N, Mitomi H. Expansion of the indications for endoscopic mucosal resection in patients with superficial esophageal carcinoma. Endoscopy. 2007;39:36–40. doi: 10.1055/s-2006-945148. [DOI] [PubMed] [Google Scholar]
- 21.Iguchi Y, Niwa Y, Miyahara R, Nakamura M, Banno K, Nagaya T, Nagasaka T, Watanabe O, Ando T, Kawashima H, et al. Pilot study on confocal endomicroscopy for determination of the depth of squamous cell esophageal cancer in vivo. J Gastroenterol Hepatol. 2009;24:1733–1739. doi: 10.1111/j.1440-1746.2009.05892.x. [DOI] [PubMed] [Google Scholar]
- 22.Ishihara R, Iishi H, Uedo N, Takeuchi Y, Yamamoto S, Yamada T, Masuda E, Higashino K, Kato M, Narahara H, et al. Comparison of EMR and endoscopic submucosal dissection for en bloc resection of early esophageal cancers in Japan. Gastrointest Endosc. 2008;68:1066–1072. doi: 10.1016/j.gie.2008.03.1114. [DOI] [PubMed] [Google Scholar]
- 23.Ishii N, Horiki N, Itoh T, Uemura M, Maruyama M, Suzuki S, Uchida S, Izuka Y, Fukuda K, Fujita Y. Endoscopic submucosal dissection with a combination of small-caliber-tip transparent hood and flex knife is a safe and effective treatment for superficial esophageal neoplasias. Surg Endosc. 2010;24:335–342. doi: 10.1007/s00464-009-0560-x. [DOI] [PubMed] [Google Scholar]
- 24.Larghi A, Lightdale CJ, Memeo L, Bhagat G, Okpara N, Rotterdam H. EUS followed by EMR for staging of high-grade dysplasia and early cancer in Barrett’s esophagus. Gastrointest Endosc. 2005;62:16–23. doi: 10.1016/s0016-5107(05)00319-6. [DOI] [PubMed] [Google Scholar]
- 25.Lewis JT, Wang KK, Abraham SC. Muscularis mucosae duplication and the musculo-fibrous anomaly in endoscopic mucosal resections for barrett esophagus: implications for staging of adenocarcinoma. Am J Surg Pathol. 2008;32:566–571. doi: 10.1097/PAS.0b013e31815bf8c7. [DOI] [PubMed] [Google Scholar]
- 26.Lin LF, Huang PT, Ho KS, Tung JN. Endoscopic mucosal resection of early esophageal carcinoma--experience of 9 cases. J Chin Med Assoc. 2008;71:347–352. doi: 10.1016/S1726-4901(08)70137-0. [DOI] [PubMed] [Google Scholar]
- 27.Lopes CV, Hela M, Pesenti C, Bories E, Caillol F, Monges G, Giovannini M. Circumferential endoscopic resection of Barrett’s esophagus with high-grade dysplasia or early adenocarcinoma. Surg Endosc. 2007;21:820–824. doi: 10.1007/s00464-006-9187-3. [DOI] [PubMed] [Google Scholar]
- 28.Maish MS, DeMeester SR. Endoscopic mucosal resection as a staging technique to determine the depth of invasion of esophageal adenocarcinoma. Ann Thorac Surg. 2004;78:1777–1782. doi: 10.1016/j.athoracsur.2004.04.064. [DOI] [PubMed] [Google Scholar]
- 29.Naritaka Y, Ogawa K, Shimakawa T, Wagatsuma Y, Katsube T, Kajiwara T, Aiba M. Study on endoscopic esophageal mucosal resection with ligating device. I--Clinical study. Hepatogastroenterology. 2001;48:1015–1017. [PubMed] [Google Scholar]
- 30.Nijhawan PK, Wang KK. Endoscopic mucosal resection for lesions with endoscopic features suggestive of malignancy and high-grade dysplasia within Barrett’s esophagus. Gastrointest Endosc. 2000;52:328–332. doi: 10.1067/mge.2000.105777. [DOI] [PubMed] [Google Scholar]
- 31.Noguchi H, Naomoto Y, Kondo H, Haisa M, Yamatsuji T, Shigemitsu K, Aoki H, Isozaki H, Tanaka N. Evaluation of endoscopic mucosal resection for superficial esophageal carcinoma. Surg Laparosc Endosc Percutan Tech. 2000;10:343–350. [PubMed] [Google Scholar]
- 32.Nomura T, Boku N, Ohtsu A, Muto M, Matsumoto S, Tajiri H, Yoshida S. Recurrence after endoscopic mucosal resection for superficial esophageal cancer. Endoscopy. 2000;32:277–280. doi: 10.1055/s-2000-7379. [DOI] [PubMed] [Google Scholar]
- 33.Nonaka K, Arai S, Ishikawa K, Nakao M, Nakai Y, Togawa O, Nagata K, Shimizu M, Sasaki Y, Kita H. Short term results of endoscopic submucosal dissection in superficial esophageal squamous cell neoplasms. World J Gastrointest Endosc. 2010;2:69–74. doi: 10.4253/wjge.v2.i2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ono S, Fujishiro M, Niimi K, Goto O, Kodashima S, Yamamichi N, Omata M. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest Endosc. 2009;70:860–866. doi: 10.1016/j.gie.2009.04.044. [DOI] [PubMed] [Google Scholar]
- 35.Ota M, Ide H, Hayashi K, Murata Y, Eguchi R, Nakamura T, Narumiya K, Oi I, Takasaki K. Multimodality treatments with endoscopic mucosal resection of esophageal squamous cell carcinoma with submucosal invasion. Surg Endosc. 2003;17:1429–1433. doi: 10.1007/s00464-002-8708-y. [DOI] [PubMed] [Google Scholar]
- 36.Pech O, May A, Gossner L, Rabenstein T, Manner H, Huijsmans J, Vieth M, Stolte M, Berres M, Ell C. Curative endoscopic therapy in patients with early esophageal squamous-cell carcinoma or high-grade intraepithelial neoplasia. Endoscopy. 2007;39:30–35. doi: 10.1055/s-2006-945040. [DOI] [PubMed] [Google Scholar]
- 37.Pouw RE, Peters FP, Sempoux C, Piessevaux H, Deprez PH. Stepwise radical endoscopic resection for Barrett’s esophagus with early neoplasia: report on a Brussels’ cohort. Endoscopy. 2008;40:892–898. doi: 10.1055/s-2008-1077675. [DOI] [PubMed] [Google Scholar]
- 38.Prasad GA, Buttar NS, Wongkeesong LM, Lewis JT, Sanderson SO, Lutzke LS, Borkenhagen LS, Wang KK. Significance of neoplastic involvement of margins obtained by endoscopic mucosal resection in Barrett’s esophagus. Am J Gastroenterol. 2007;102:2380–2386. doi: 10.1111/j.1572-0241.2007.01419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prasad GA, Wu TT, Wigle DA, Buttar NS, Wongkeesong LM, Dunagan KT, Lutzke LS, Borkenhagen LS, Wang KK. Endoscopic and surgical treatment of mucosal (T1a) esophageal adenocarcinoma in Barrett’s esophagus. Gastroenterology. 2009;137:815–823. doi: 10.1053/j.gastro.2009.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scheil-Bertram S, Lorenz D, Ell C, Sheremet E, Fisseler-Eckhoff A. Expression of alpha-methylacyl coenzyme A racemase in the dysplasia carcinoma sequence associated with Barrett’s esophagus. Mod Pathol. 2008;21:961–967. doi: 10.1038/modpathol.2008.73. [DOI] [PubMed] [Google Scholar]
- 41.Schröder W, Wirths K, Gutschow C, Vallböhmer D, Bludau M, Schumacher B, Neuhaus H, Hölscher AH. Transthoracic esophagectomy after endoscopic mucosal resection in patients with early esophageal carcinoma. J Gastrointest Surg. 2009;13:223–229. doi: 10.1007/s11605-008-0719-0. [DOI] [PubMed] [Google Scholar]
- 42.Shimizu Y, Tukagoshi H, Fujita M, Hosokawa M, Kato M, Asaka M. Metachronous squamous cell carcinoma of the esophagus arising after endoscopic mucosal resection. Gastrointest Endosc. 2001;54:190–194. doi: 10.1067/mge.2001.116877. [DOI] [PubMed] [Google Scholar]
- 43.Soehendra N, Binmoeller KF, Bohnacker S, Seitz U, Brand B, Thonke F, Gurakuqi G. Endoscopic snare mucosectomy in the esophagus without any additional equipment: a simple technique for resection of flat early cancer. Endoscopy. 1997;29:380–383. doi: 10.1055/s-2007-1004219. [DOI] [PubMed] [Google Scholar]
- 44.Takeo Y, Yoshida T, Shigemitu T, Yanai H, Hayashi N, Okita K. Endoscopic mucosal resection for early esophageal cancer and esophageal dysplasia. Hepatogastroenterology. 2001;48:453–457. [PubMed] [Google Scholar]
- 45.Takeshita K, Tani M, Inoue H, Saeki I, Hayashi S, Honda T, Kando F, Saito N, Endo M. Endoscopic treatment of early oesophageal or gastric cancer. Gut. 1997;40:123–127. doi: 10.1136/gut.40.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tanabe S, Koizumi W, Higuchi K, Sasaki T, Nakatani K, Hanaoka N, Ae T, Ishido K, Mitomi H, Saigenji K. Clinical outcomes of endoscopic oblique aspiration mucosectomy for superficial esophageal cancer. Gastrointest Endosc. 2008;67:814–820. doi: 10.1016/j.gie.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 47.Teoh AY, Chiu PW, Yu Ngo DK, Wong SK, Lau JY, Ng EK. Outcomes of endoscopic submucosal dissection versus endoscopic mucosal resection in management of superficial squamous esophageal neoplasms outside Japan. J Clin Gastroenterol. 2010;44:e190–e194. doi: 10.1097/MCG.0b013e3181ce52fb. [DOI] [PubMed] [Google Scholar]
- 48.Urabe Y, Hiyama T, Tanaka S, Yoshihara M, Arihiro K, Chayama K. Advantages of endoscopic submucosal dissection versus endoscopic oblique aspiration mucosectomy for superficial esophageal tumors. J Gastroenterol Hepatol. 2011;26:275–280. doi: 10.1111/j.1440-1746.2010.06503.x. [DOI] [PubMed] [Google Scholar]
- 49.Yokoyama A, Ohmori T, Makuuchi H, Maruyama K, Okuyama K, Takahashi H, Yokoyama T, Yoshino K, Hayashida M, Ishii H. Successful screening for early esophageal cancer in alcoholics using endoscopy and mucosa iodine staining. Cancer. 1995;76:928–934. doi: 10.1002/1097-0142(19950915)76:6<928::aid-cncr2820760604>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 50.Zehetner J, DeMeester SR, Hagen JA, Ayazi S, Augustin F, Lipham JC, DeMeester TR. Endoscopic resection and ablation versus esophagectomy for high-grade dysplasia and intramucosal adenocarcinoma. J Thorac Cardiovasc Surg. 2011;141:39–47. doi: 10.1016/j.jtcvs.2010.08.058. [DOI] [PubMed] [Google Scholar]
- 51.Repici A, Hassan C, Carlino A, Pagano N, Zullo A, Rando G, Strangio G, Romeo F, Nicita R, Rosati R, et al. Endoscopic submucosal dissection in patients with early esophageal squamous cell carcinoma: results from a prospective Western series. Gastrointest Endosc. 2010;71:715–721. doi: 10.1016/j.gie.2009.11.020. [DOI] [PubMed] [Google Scholar]
- 52.Hull MJ, Mino-Kenudson M, Nishioka NS, Ban S, Sepehr A, Puricelli W, Nakatsuka L, Ota S, Shimizu M, Brugge WR, et al. Endoscopic mucosal resection: an improved diagnostic procedure for early gastroesophageal epithelial neoplasms. Am J Surg Pathol. 2006;30:114–118. doi: 10.1097/01.pas.0000180438.56528.a0. [DOI] [PubMed] [Google Scholar]
- 53.Peters FP, Brakenhoff KP, Curvers WL, Rosmolen WD, Fockens P, ten Kate FJ, Krishnadath KK, Bergman JJ. Histologic evaluation of resection specimens obtained at 293 endoscopic resections in Barrett’s esophagus. Gastrointest Endosc. 2008;67:604–609. doi: 10.1016/j.gie.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 54.Vieth M, Ell C, Gossner L, May A, Stolte M. Histological analysis of endoscopic resection specimens from 326 patients with Barrett’s esophagus and early neoplasia. Endoscopy. 2004;36:776–781. doi: 10.1055/s-2004-825802. [DOI] [PubMed] [Google Scholar]
- 55.Amano T, Matsumoto T, Hayashi T, Arakawa A, Sonoue H, Kajiyama Y, Tsurumaru M. Subepithelial extension of squamous cell carcinoma in the esophagus: histopathological study using D2-40 immunostaining for 108 superficial carcinomas. Pathol Int. 2007;57:759–764. doi: 10.1111/j.1440-1827.2007.02171.x. [DOI] [PubMed] [Google Scholar]
- 56.Araki K, Ohno S, Egashira A, Saeki H, Kawaguchi H, Sugimachi K. Pathologic features of superficial esophageal squamous cell carcinoma with lymph node and distal metastasis. Cancer. 2002;94:570–575. doi: 10.1002/cncr.10190. [DOI] [PubMed] [Google Scholar]
- 57.Bollschweiler E, Baldus SE, Schröder W, Prenzel K, Gutschow C, Schneider PM, Hölscher AH. High rate of lymph-node metastasis in submucosal esophageal squamous-cell carcinomas and adenocarcinomas. Endoscopy. 2006;38:149–156. doi: 10.1055/s-2006-924993. [DOI] [PubMed] [Google Scholar]
- 58.Buskens CJ, Westerterp M, Lagarde SM, Bergman JJ, ten Kate FJ, van Lanschot JJ. Prediction of appropriateness of local endoscopic treatment for high-grade dysplasia and early adenocarcinoma by EUS and histopathologic features. Gastrointest Endosc. 2004;60:703–710. doi: 10.1016/s0016-5107(04)02017-6. [DOI] [PubMed] [Google Scholar]
- 59.Cen P, Hofstetter WL, Correa AM, Wu TT, Lee JH, Ross WA, Davilla M, Swisher SG, Fukami N, Rashid A, et al. Lymphovascular invasion as a tool to further subclassify T1b esophageal adenocarcinoma. Cancer. 2008;112:1020–1027. doi: 10.1002/cncr.23265. [DOI] [PubMed] [Google Scholar]
- 60.Chino O, Makuuchi H, Machimura T, Mizutani K, Shimada H, Kanno K, Nishi T, Tanaka H, Sasaki T, Tajima T, et al. Treatment of esophageal cancer in patients over 80 years old. Surg Today. 1997;27:9–16. doi: 10.1007/BF01366933. [DOI] [PubMed] [Google Scholar]
- 61.Eguchi T, Nakanishi Y, Shimoda T, Iwasaki M, Igaki H, Tachimori Y, Kato H, Yamaguchi H, Saito D, Umemura S. Histopathological criteria for additional treatment after endoscopic mucosal resection for esophageal cancer: analysis of 464 surgically resected cases. Mod Pathol. 2006;19:475–480. doi: 10.1038/modpathol.3800557. [DOI] [PubMed] [Google Scholar]
- 62.Endo M. Endoscopic resection as local treatment of mucosal cancer of the esophagus. Endoscopy. 1993;25:672–674. doi: 10.1055/s-2007-1010430. [DOI] [PubMed] [Google Scholar]
- 63.Gockel I, Domeyer M, Sgourakis GG, Schimanski CC, Moehler M, Kirkpatrick CJ, Lang H, Junginger T, Hansen T. Prediction model of lymph node metastasis in superficial esophageal adenocarcinoma and squamous cell cancer including D2-40 immunostaining. J Surg Oncol. 2009;100:191–198. doi: 10.1002/jso.21336. [DOI] [PubMed] [Google Scholar]
- 64.Goseki N, Koike M, Yoshida M. Histopathologic characteristics of early stage esophageal carcinoma. A comparative study with gastric carcinoma. Cancer. 1992;69:1088–1093. doi: 10.1002/cncr.2820690503. [DOI] [PubMed] [Google Scholar]
- 65.Ide H, Nakamura T, Hayashi K, Endo T, Kobayashi A, Eguchi R, Hanyu F. Esophageal squamous cell carcinoma: pathology and prognosis. World J Surg. 1994;18:321–330. doi: 10.1007/BF00316810. [DOI] [PubMed] [Google Scholar]
- 66.Ikeda Y, Ozawa S, Ando N, Kitagawa Y, Ueda M, Kitajima M. Meanings of c-erbB and int-2 amplification in superficial esophageal squamous cell carcinomas. Ann Thorac Surg. 1996;62:835–838. doi: 10.1016/s0003-4975(96)00392-x. [DOI] [PubMed] [Google Scholar]
- 67.Kim DU, Lee JH, Min BH, Shim SG, Chang DK, Kim YH, Rhee PL, Kim JJ, Rhee JC, Kim KM, et al. Risk factors of lymph node metastasis in T1 esophageal squamous cell carcinoma. J Gastroenterol Hepatol. 2008;23:619–625. doi: 10.1111/j.1440-1746.2007.05259.x. [DOI] [PubMed] [Google Scholar]
- 68.Kimura H, Konishi K, Maeda K, Yabushita K, Kuroda Y, Tsuji M, Miwa A. Flow cytometric analysis and immunohistochemical staining for the p53 protein and proliferating cell nuclear antigen in submucosal carcinoma of the esophagus. Hepatogastroenterology. 1999;46:285–289. [PubMed] [Google Scholar]
- 69.Kuwano H, Kitamura K, Baba K, Morita M, Matsuda H, Mori M, Sugimachi K. Determination of the resection line in early esophageal cancer using intraoperative endoscopic examination with Lugol staining. J Surg Oncol. 1992;50:149–152. doi: 10.1002/jso.2930500304. [DOI] [PubMed] [Google Scholar]
- 70.Leers JM, DeMeester SR, Oezcelik A, Klipfel N, Ayazi S, Abate E, Zehetner J, Lipham JC, Chan L, Hagen JA, et al. The prevalence of lymph node metastases in patients with T1 esophageal adenocarcinoma a retrospective review of esophagectomy specimens. Ann Surg. 2011;253:271–278. doi: 10.1097/SLA.0b013e3181fbad42. [DOI] [PubMed] [Google Scholar]
- 71.Liu L, Hofstetter WL, Rashid A, Swisher SG, Correa AM, Ajani JA, Hamilton SR, Wu TT. Significance of the depth of tumor invasion and lymph node metastasis in superficially invasive (T1) esophageal adenocarcinoma. Am J Surg Pathol. 2005;29:1079–1085. [PubMed] [Google Scholar]
- 72.Makuuchi H, Shimada H, Mizutani K, Chino O, Nishi T, Tanaka H, Machimura T, Mitomi T, Osamura Y. Clinical pathological analysis of surgically resected superficial esophageal carcinoma to determine criteria for deciding on treatment strategy. Diagn Ther Endosc. 1997;3:211–220. doi: 10.1155/DTE.3.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Matsumoto M, Natsugoe S, Okumura H, Arima H, Yanagita S, Uchikado Y, Yokomakura N, Setoyama T, Ishigami S, Takao S, et al. Overexpression of vascular endothelial growth factor-C correlates with lymph node micrometastasis in submucosal esophageal cancer. J Gastrointest Surg. 2006;10:1016–1022. doi: 10.1016/j.gassur.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 74.Nakajima Y, Nagai K, Miyake S, Ohashi K, Kawano T, Iwai T. Evaluation of an indicator for lymph node metastasis of esophageal squamous cell carcinoma invading the submucosal layer. Jpn J Cancer Res. 2002;93:305–312. doi: 10.1111/j.1349-7006.2002.tb02173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Natsugoe S, Matsumoto M, Okumura H, Ikeda M, Ishigami S, Owaki T, Takao S, Aikou T. Prognostic factors in patients with submucosal esophageal cancer. J Gastrointest Surg. 2004;8:631–635. doi: 10.1016/j.gassur.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 76.Ohno S, Mori M, Tsutsui S, Matsuura H, Kuwano H, Soejima K, Sugimachi K. Growth patterns and prognosis of submucosal carcinoma of the esophagus. A pathologic study. Cancer. 1991;68:335–340. doi: 10.1002/1097-0142(19910715)68:2<335::aid-cncr2820680222>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 77.Paraf F, Fléjou JF, Pignon JP, Fékété F, Potet F. Surgical pathology of adenocarcinoma arising in Barrett’s esophagus. Analysis of 67 cases. Am J Surg Pathol. 1995;19:183–191. doi: 10.1097/00000478-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 78.Rice TW, Zuccaro G, Adelstein DJ, Rybicki LA, Blackstone EH, Goldblum JR. Esophageal carcinoma: depth of tumor invasion is predictive of regional lymph node status. Ann Thorac Surg. 1998;65:787–792. doi: 10.1016/s0003-4975(97)01387-8. [DOI] [PubMed] [Google Scholar]
- 79.Schmidt LW, Dean PJ, Wilson RT. Superficially invasive squamous cell carcinoma of the esophagus. A study of seven cases in Memphis, Tennessee. Gastroenterology. 1986;91:1456–1461. doi: 10.1016/0016-5085(86)90201-5. [DOI] [PubMed] [Google Scholar]
- 80.Sepesi B, Watson TJ, Zhou D, Polomsky M, Litle VR, Jones CE, Raymond DP, Hu R, Qiu X, Peters JH. Are endoscopic therapies appropriate for superficial submucosal esophageal adenocarcinoma? An analysis of esophagectomy specimens. J Am Coll Surg. 2010;210:418–427. doi: 10.1016/j.jamcollsurg.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 81.Shiozaki H, Doki Y, Yamana H, Isono K. A multi-institutional study of immunohistochemical investigation for the roles of cyclin D1 and E-cadherin in superficial squamous cell carcinoma of the esophagus. J Surg Oncol. 2002;79:166–173. doi: 10.1002/jso.10074. [DOI] [PubMed] [Google Scholar]
- 82.Soga J, Tanaka O, Sasaki K, Kawaguchi M, Muto T. Superficial spreading carcinoma of the esophagus. Cancer. 1982;50:1641–1645. doi: 10.1002/1097-0142(19821015)50:8<1641::aid-cncr2820500830>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 83.Tomita N, Matsumoto T, Hayashi T, Arakawa A, Sonoue H, Kajiyama Y, Tsurumaru M. Lymphatic invasion according to D2-40 immunostaining is a strong predictor of nodal metastasis in superficial squamous cell carcinoma of the esophagus: algorithm for risk of nodal metastasis based on lymphatic invasion. Pathol Int. 2008;58:282–287. doi: 10.1111/j.1440-1827.2008.02224.x. [DOI] [PubMed] [Google Scholar]
- 84.Tsutsui S, Kuwano H, Yasuda M, Nozoe T, Watanabe M, Kitamura M, Sugimachi K. Extensive spreading carcinoma of the esophagus with invasion restricted to the submucosa. Am J Gastroenterol. 1995;90:1858–1863. [PubMed] [Google Scholar]
- 85.Westerterp M, Koppert LB, Buskens CJ, Tilanus HW, ten Kate FJ, Bergman JJ, Siersema PD, van Dekken H, van Lanschot JJ. Outcome of surgical treatment for early adenocarcinoma of the esophagus or gastro-esophageal junction. Virchows Arch. 2005;446:497–504. doi: 10.1007/s00428-005-1243-1. [DOI] [PubMed] [Google Scholar]
- 86.Yoshikane H, Tsukamoto Y, Niwa Y, Goto H, Hase S, Shimodaira M, Maruta S, Miyata A, Yoshida M. Superficial esophageal carcinoma: evaluation by endoscopic ultrasonography. Am J Gastroenterol. 1994;89:702–707. [PubMed] [Google Scholar]
- 87.Cao Y, Liao C, Tan A, Gao Y, Mo Z, Gao F. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy. 2009;41:751–757. doi: 10.1055/s-0029-1215053. [DOI] [PubMed] [Google Scholar]
- 88.Sgourakis G, Gockel I, Lyros O, Lanitis S, Dedemadi G, Polotzek U, Karaliotas C, Lang H. The use of neural networks in identifying risk factors for lymph node metastasis and recommending management of t1b esophageal cancer. Am Surg. 2012;78:195–206. [PubMed] [Google Scholar]
- 89.Wright A, Ricciardi TN, Zwick M. Application of information-theoretic data mining techniques in a national ambulatory practice outcomes research network. AMIA Annu Symp Proc. 2005:829–833. [PMC free article] [PubMed] [Google Scholar]
- 90.Ohashi K, Momma K, Yamada Y, Yoshida M, Horiguchi S, Matsubayashi J, Shimizu S, Moriyama S, Hishima T, Funata N, et al. Vertical and horizontal growth features of superficial esophageal squamous cell carcinomas: histopathological evaluation of endoscopically resected specimens. Virchows Arch. 2002;441:350–357. doi: 10.1007/s00428-002-0689-7. [DOI] [PubMed] [Google Scholar]
- 91.Chino O, Makuuchi H, Shimada H, Machimura T, Mitomi T, Osamura RY. Assessment of the proliferative activity of superficial esophageal carcinoma using MIB-1 immunostaining for the Ki-67 antigen. J Surg Oncol. 1998;67:18–24. doi: 10.1002/(sici)1096-9098(199801)67:1<18::aid-jso4>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 92.Endo M, Kawano T. Detection and classification of early squamous cell esophageal cancer. Dis Esophagus. 1997;10:155–158. doi: 10.1093/dote/10.3.155. [DOI] [PubMed] [Google Scholar]
- 93.Kuwano H, Masuda N, Kato H, Sugimachi K. The subepithelial extension of esophageal carcinoma for determining the resection margin during esophagectomy: a serial histopathologic investigation. Surgery. 2002;131:S14–S21. doi: 10.1067/msy.2002.119289. [DOI] [PubMed] [Google Scholar]