Abstract
Sweet taste receptor subunits and α-gustducin found in enteroendocrine cells of the small intestine have been implicated in release of the incretin hormones glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) in response to glucose and noncaloric sweeteners. α-Gustducin has also been found in colon, although its function there is unclear. We examined expression of α-gustducin, GLP-1, and GIP throughout the intestine. The number of α-gustducin-expressing cells and those coexpressing α-gustducin together with GLP-1 and/or GIP increased from small intestine to colon. α-Gustducin also was coexpressed with fatty acid G protein-coupled receptor (GPR) 40, GPR41, GPR43, GPR119, GPR120, and bile acid G protein-coupled receptor TGR5 in enteroendocrine cells of the colon. In colon, GPR43 was coexpressed with GPR119 and GPR120, but not with TGR5. Treatment of colonic mucosa isolated from wild-type mice with acetate, butyrate, oleic acid, oleoylethanolamide, or lithocholic acid stimulated GLP-1 secretion. However, GLP-1 release in response to these fatty acids was impaired in colonic tissue from α-gustducin knockout mice.
Keywords: α-gustducin, glucose-dependent insulinotropic polypeptide, glucagon-like peptide 1, fatty acid receptors, enteroendocrine cell
the incretin hormones glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) are estimated to account for ∼50–70% of total insulin release after oral glucose administration (13, 30, 59). The meal-related GLP-1 response in type 2 diabetes is decreased, which may contribute to the decreased incretin effect in this population (58, 86).
The sweet taste receptor subunits T1r2 and T1r3, and the G protein α-subunit α-gustducin, initially found in taste cells (48, 54, 55, 60, 91), have also been shown to be present in enteroendocrine and brush cells of the small intestine (3, 14, 29, 51). α-Gustducin and T1r receptors are also present in the small intestine's L- and K-type enteroendocrine cells, which release GLP-1 and GIP, respectively, in response to glucose in the gut lumen (35). In response to glucose gavage, α-gustducin null mice do not show the elevation of serum levels of GLP-1 found in gavaged wild-type mice (35). Furthermore, sweetener-stimulated GLP-1 release from L cell lines can be inhibited by small-interfering RNA against α-gustducin or pharmacological blocking of the T1r2+T1r3 sweet receptor (35, 51). In addition, other mechanisms independent of α-gustducin and T1rs, including sodium glucose cotransporter-1 (SGLT1) and ATP-sensitive K+ channels (KATP), are known to regulate GLP-1 release from primary L cells (69).
α-Gustducin is also expressed with peptide YY (PYY) and GLP-1 in L cells of the human colon (74), although its functions in these cells are unknown. The lumen of the colon lacks dietary sugars, but is filled with microbiota, nondigestible matter, and fermentation products, such as short-chain fatty acids (SCFAs), ammonia, phenols, amines, and bile acids (12, 23, 50, 84). Medium- and long-chain fatty acids (LCFAs) are also detected in fecal content from patients with small bowel resection on a high-fat diet (36) and from colectomized patients (1). Interestingly, the SCFA receptor G protein-coupled receptor (GPR) 43 (6, 47) is coexpressed with GLP-1 in both human and rat colon L cells (37). The LCFA receptors GPR40 and GPR120, the G protein-coupled bile acid receptor TGR5, and oleoylethanolamide (OEA) receptor GPR119 have been detected in L cells and/or in L-type enteroendocrine cell lines; agonist stimulation of these receptors promotes GLP-1 secretion (8, 15, 28, 38, 46, 69, 85). However, whether these receptors couple to α-gustducin in native cells is unknown.
Given α-gustducin's involvement with sweetener-stimulated GLP-1 release from L cells of the small intestine and its unexplained presence in L cells of the colon, we examined coexpression of α-gustducin with fatty acid receptors in colon. Here, we show that α-gustducin is coexpressed with SCFA receptors GPR43 and GPR41, LCFA receptors GPR40 and GPR120, OEA receptor GPR119, and bile acid receptor TGR5. In addition, using α-gustducin null mice, we show that α-gustducin is involved in GLP-1 release mediated by these fatty acid receptors. α-Gustducin is likely to contribute to colonic release of incretins to augment insulin release from pancreas.
MATERIALS AND METHODS
Tissue preparation.
All experimental protocols and procedures were approved by Monell's Institutional Animal Care and Use Committee in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Adult male C57BL/6 mice (2–10 mo old) were killed by cervical dislocation, and the entire small intestine and proximal colon were removed quickly. The duodenum, jejunum, ileum, and proximal colon were flushed with phosphate-buffered saline (PBS, pH 7.4). For in situ hybridization, tissues were freshly frozen in Tissue-Tek optimum cutting temperature (OCT) mounting media (Sakura) and then sectioned within 1 h. For immunohistochemistry, tissues were fixed for 2 h in 4% (wt/vol) paraformaldehyde/1× PBS and then cryoprotected in 20% (wt/vol) sucrose/1× PBS overnight at 4°C before embedding in OCT. Sections (8–12 μm thick) were prepared using a CM3050S cryostat (Leica Microsystems) and placed on precoated microscope slides (Superfrost plus; Fisher Scientific). Sections were dried at 40°C for 20 min before immunohistochemistry.
In situ hybridization.
In situ hybridization was performed as previously described (96). Briefly, tissues were freshly frozen in Tissue-Tek OCT mounting media (Sakura) and then sectioned within 1 h. Next, the sections were fixed for 10 min in 4% paraformaldehyde and then permeabilized in 10 μg/ml proteinase K (Boehringer Mannheim) solution. After postfixation and acetylation, the slides were treated with DNase and then prehybridized for 1 h at room temperature in prehybridization solution containing 50% (vol/vol) deionized formamide, 5× saline/sodium citrate (SSC), 5× Denhardt's solution, 500 μg/ml salmon sperm DNA, 250 μl/ml of yeast tRNA, and 2.5 M EDTA in diethyl pyrocarbonate-treated water. Digoxigenin (DIG)-labeled RNA probe was incubated at 65°C overnight for hybridization. Next, the slides were incubated with anti-DIG-alkaline phosphatase (1:1,000; Boehringer) after blocking with 10% (vol/vol) heat-inactivated normal goat serum. Alkaline phosphate labeling was detected by a nitroblue tetrazolium plus 5-bromo-4-chloro-3 indolyl-phosphate mixture (Roche) with levamisole (Sigma). Antisense and sense RNA probes were used at equivalent concentrations and run in parallel in the same experiment to ensure equivalent conditions. For each experiment, in situ hybridization with positive controls with T1r3 or α-gustducin antisense probes was done on taste tissue to ensure the hybridization worked properly. The following primers were used to make RNA probes: GPR40 RNA probes, 5′-AGTGTCCCACGCTAAACTGC-3′ (forward) and 5′-TGAGTCCCAACTTCCTCCAG-3′ (reverse); GPR41 RNA probes, 5′-ATGGGGACAAGCTTCTTTCTTGGC-3′ (forward) and 5′-TCTGAGTGACAGCAATGTCTGC-3′ (reverse); GPR43 RNA probes, 5′-ATGACCCCAGACTGGCACAGTTC-3′ (forward) and 5′-TCTAGGTGGCATTTCCAAGC-3′ (reverse). The cloned product was verified by DNA sequencing and then used for making the DIG-labeled probes by DIG-RNA kit (Roche).
Immunohistochemistry.
Double indirect immunohistochemistry techniques were performed as previously described (96). Briefly, frozen sections were rehydrated with PBS. Nonspecific binding was blocked with a blocking buffer [3% (vol/vol) BSA, 0.3% Triton X-100, 2% (vol/vol) donkey serum in 1× PBS] at room temperature for 1–2 h. Sections were incubated with two of the following primary antibodies from different species: rabbit anti-α-gustducin (1:250; sc-395), goat anti-GLP-1 (1:150; sc-7782), goat anti-GIP (1:300; sc-23554), goat anti-GPR40 (1:200; sc-28416), goat anti-GPR41 (1:200; sc-131166), and goat anti-GPR43 (1:200; sc-28424) from Santa Cruz Biotechnology; rabbit anti-GPR120 (1:150; NLS2004) or rabbit anti-GPR119 (1:200; NB110–92716) from Novus Biologicals; or rabbit anti-TGR5 (1:500; ab72608) from Abcam. Incubations with primary antibodies were carried out overnight at 4°C in a humidified chamber. After three 15-min washes with 1× PBS with 0.1% Tween 20 (PBST), the following secondary antibodies were added to the sections: Alexa488 donkey anti-rabbit and Alexa594 donkey anti-goat or Alexa647 donkey anti-goat (1:800–1:1,000; Invitrogen) for 2 h at room temperature in the dark. Next, the slides were washed three times with PBS and mounted with Vectashield mounting medium (Vector). Negative controls (e.g., minus primary antibody, plus blocking peptide, or comparison with nonimmune serum) were included for antibodies against fatty acid receptors (see Supplemental Figs. 1 and 2).1 Antibodies against α-gustducin (sc-395) (35, 51), GLP-1 (sc-7782) (35), and GIP (sc-23554) (24, 95) have been validated previously in the above-mentioned papers from our laboratory and/or from others.
For double-immunofluorescent labeling using primary antibodies from the same species, after the first primary incubation, the slides were incubated for 1 h at room temperature with secondary Fab donkey anti-rabbit antibody conjugated to Alexa488 (1:250; Jackson ImmunoResearch). Rabbit serum (10%) was applied for 1 h at room temperature to cover the first primary antibody. The slides were washed and incubated with an excess of unconjugated Fab anti-rabbit antibody for 2 h at room temperature. Next, the second primary antibody was applied overnight at 4°C after three washes with PBST. The slides were then incubated with the second secondary Fab donkey anti-goat conjugated to Alexa594 (1:250; Jackson ImmunoResearch) for 1 h at room temperature. Negative controls included the omission of both primary antibodies and the omission of the second primary antibody to confirm complete blocking of the first primary antibody. Only green fluorescence was observed when the second primary antibody was omitted.
Imaging.
Image visualization and capture were performed as previously described (96). Briefly, bright-field images were visualized using a SPOT digital camera (Diagnostic Instruments) attached to a Nikon SA Microphot microscope and processed using Image-Pro Plus image analysis software (Media Cybernetics). Acquisition parameters were held constant for in situ hybridization with both antisense and sense probes. Fluorescence images were captured with Ar, GeNe, and HeNe lasers as well as appropriate excitation spectra. Scanware software (Leica Microsystems) was used to acquire z-series stacks captured at a step size of 0.25–0.35 μm. Digital images were arranged using Photoshop CS (Adobe Systems).
Cell counting.
Quantitative measurements were conducted to determine the percentage of α-gustducin-labeled cells that coexpressed incretins GLP-1, GIP, or fatty acid receptors GPR40, GPR41, GPR43, GPR119, GPR120, and TGR5, and vice versa. The coexpression of GPR43 with GPR119, GPR120, or TGR5 was also quantified. The sections were visualized using a Nikon DXM1200C digital camera attached to a Nikon eclipse 80i fluorescence microscope. Only those cells for which the entire cell bodies could be visualized were counted. The data were expressed as the mean percentage from three sections ± SE.
Secretion of GLP-1 from proximal colon mucosa.
The protocol of Jang et al. (35) was modified to assess GLP-1 release from proximal colon mucosa. In brief, mucosa was obtained from the proximal colon by scraping with mild pressure from the short edge of a glass slide. The isolated tissue was allowed to settle at the bottom of a tube on ice and then washed three times with Dulbecco's PBS. After the final wash, purified mucosal tissue was suspended in serum-free Dulbecco's modified Eagle's medium (DMEM) with antibiotics and 20 μl/ml dipeptidyl peptidase IV inhibitor, separated into aliquots, and incubated with fatty acid agonists diluted in glucose-free Hanks' buffered salt solution with 10 mM HEPES (pH 7.0) in 5% CO2 for 2 h at 37°C. In a control set of experiments, ∼80% of cells were viable based on trypan blue staining after incubation for 2 h with 32 μM bile acids. The media were collected, and the released active GLP-1 levels were measured. At the end of experiment, the tissue was centrifuged and lysed with lysis buffer with dipeptidyl peptidase IV inhibitor. Levels of active GLP-1 in the supernatant were measured as a fraction of the cell GLP-1 content. GLP-1 secretion was calculated as the stimulated GLP-1 content of medium normalized for the total amount of GLP-1 in the medium plus cells. Dilutions were carried out so that active GLP-1 levels could be measured within the standard range of an ELISA (Millipore).
Statistical analysis.
GLP-1 data presented are means ± SEM. Data were analyzed, as appropriate for the data set, by ANOVA with Dunnett's post test, or by unpaired two-tailed Student's t-test (GraphPad Prism). P < 0.05 was considered significant.
RESULTS
Coexpression of α-gustducin with incretins in colon.
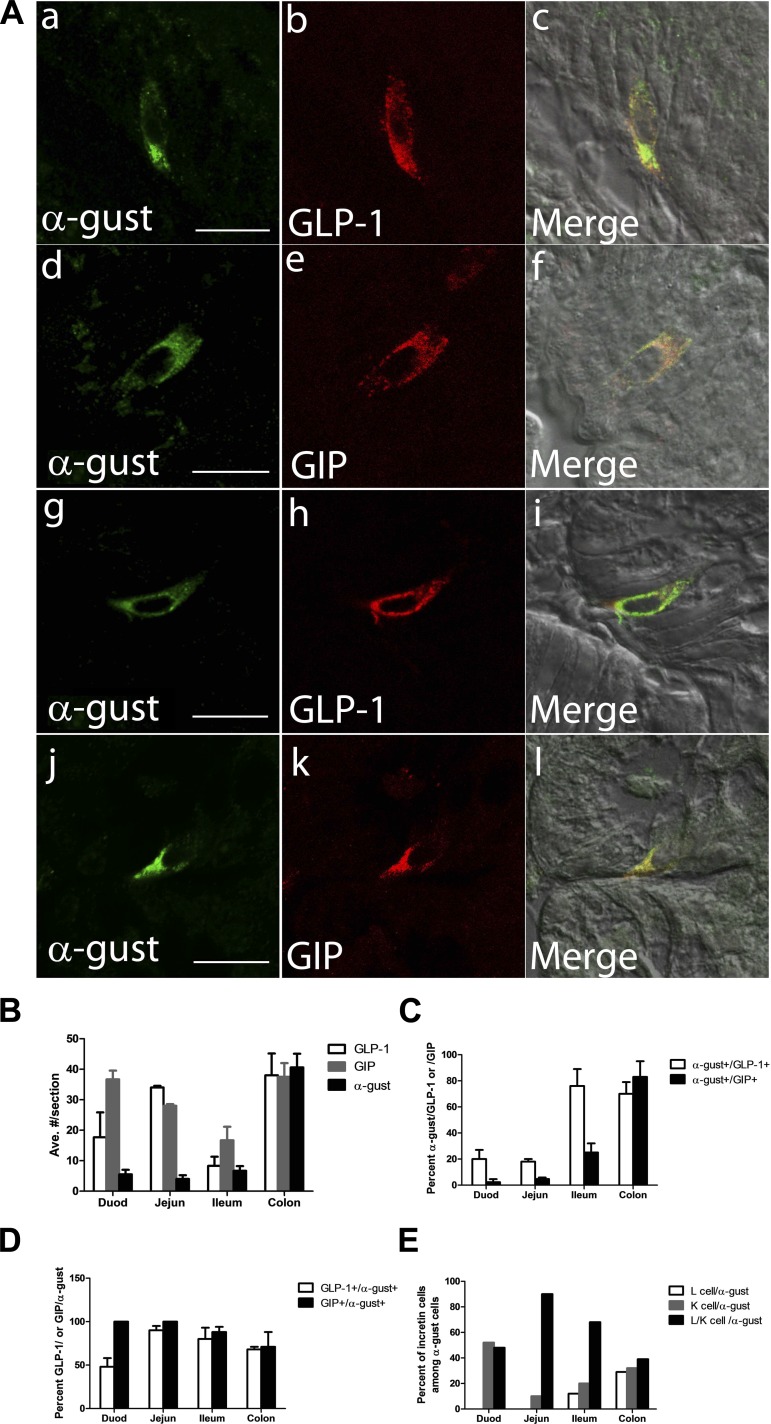
We examined coexpression of α-gustducin with GLP-1 and GIP in enteroendocrine cells ranging from duodenum to proximal colon. α-Gustducin immunofluorescence was detected in the mucosal epithelium of both small intestine and colon and some α-gustducin-expressing cells costained with GLP-1 and/or GIP (Fig. 1A). The number of α-gustducin-positive enteroendocrine cells increased markedly from duodenum (5.5 ± 1.5/section) to proximal colon (40.6 ± 4.5/section). More GLP-1-expressing cells were located in duodenum (17.7 ± 8.2/section), jejunum (34 ± 0.6/section), and proximal colon (38 ± 7.2/section); fewer were found in ileum (8.3 ± 3.0/section) (Fig. 1B). Similar results were found with GIP-positive cells: higher in duodenum (36.7 ± 2.9/section), jejunum (28 ± 0.6/section), and proximal colon (37.5 ± 4.5/section) but fewer in ileum (16.7 ± 4.5/section) (Fig. 1B). From duodenum to colon, both GLP-1-positive and GIP-positive cells showed increased coexpression with α-gustducin (α-gustducin+/GLP-1+ cells increased from 20 ± 7 to 70 ± 9%; α-gustducin+/GIP+ cells increased from 2.3 ± 2.3 to 83 ± 12%) (Fig. 1C). In small intestine, almost all α-gustducin-positive cells coexpressed GIP; in colon, ∼71 ± 17% of α-gustducin-positive cells coexpressed GIP; 90 ± 5% of α-gustducin-positive cells coexpressed GLP-1 in jejunum, the highest level of coexpression in gut. The lowest coexpression occurred in duodenum, where 48 ± 10% of α-gustducin-positive cells coexpressed GLP-1 (Fig. 1D). In small intestine, α-gustducin was mainly located in L/K cells and K cells, with relatively few L cells. However, in colon α-gustducin expression was nearly evenly distributed among L, K, and L/K cells (Fig. 1E).
Fig. 1.
Coexpression of α-gustducin with glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) in small intestine and colon. A: indirect immunofluorescent confocal imaging showing coexpression of α-gustducin (α-gust) with GLP-1 and GIP in jejunum (a–f) and proximal colon (g–l) (scale bar, 16 μm). B: quantitation of cells positive for GLP-1, GIP, and α-gustducin in different segments of gut. C: percentage of GLP-1- or GIP-positive cells in mouse proximal colon coexpressing α-gustducin. Values are means ± SE from three sections. D: percentage of α-gustducin-positive cells in mouse proximal colon coexpressing GLP-1 or GIP. Values are means ± SE from three sections. E: calculation of α-gustducin distribution in enteroendocrine L (GLP-1+), K (GIP+), and L/K (GLP-1+/GIP+) cells. The calculation was based on the same data set used to generate Fig. 1D.
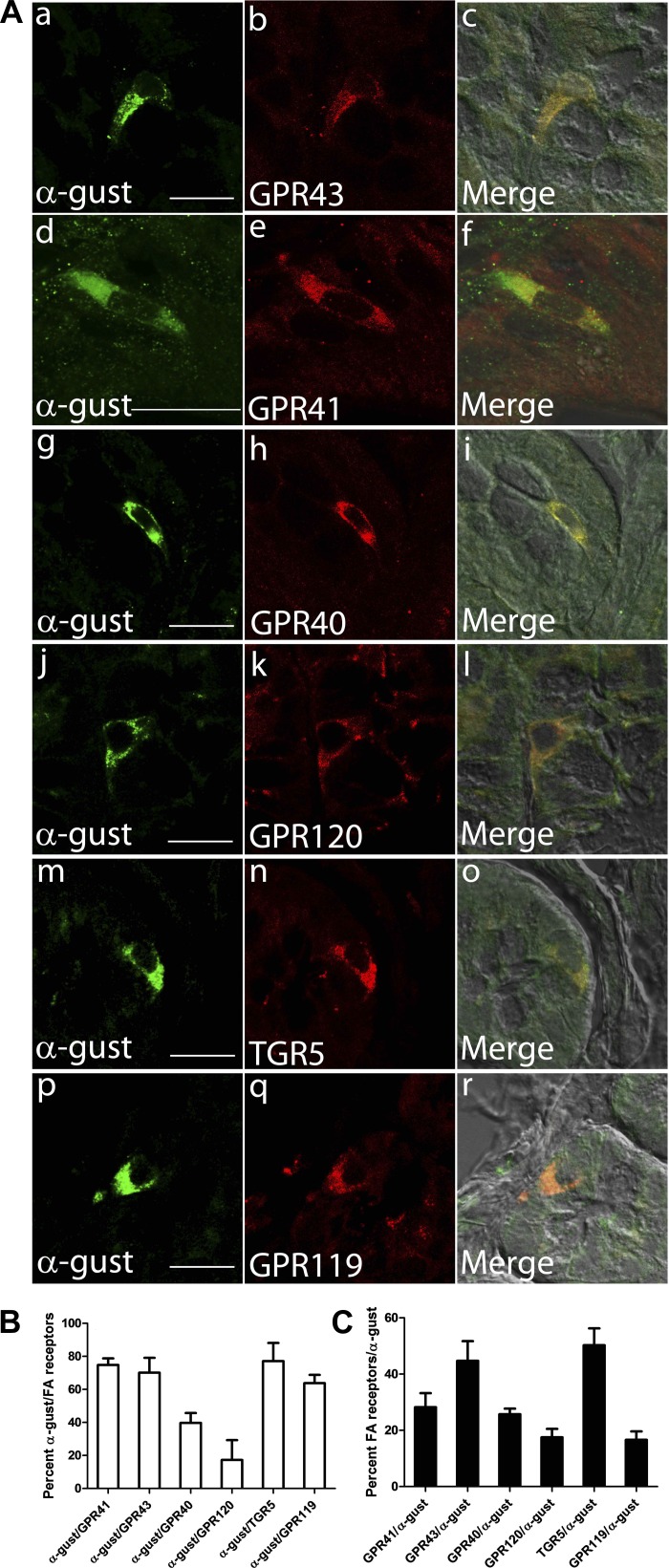
Coexpression of α-gustducin with fatty acid receptors in colon.
Given the chemosensory function of α-gustducin in taste buds and small intestine, we speculated that, in colon, α-gustducin could be involved in luminal sensation through interactions with one or more G protein-coupled receptors. Because of the large quantity of SCFAs in the lumen of the colon (50), the known expression of SCFA receptors in L cell lines (37), and the expression of α-gustducin in L cells, we examined coexpression of SCFA receptors with α-gustducin in colon. Double-immunofluorescence confocal microscopy confirmed the presence of GPR43-positive cells in colon, ∼70% of which expressed α-gustducin (Fig. 2). We extended our studies to the other SCFA receptor, GPR41, and other receptors with agonists found in colon: LCFA receptors GPR40 and GPR120, bile acid receptor TGR5, and OEA receptor GPR119 (Fig. 2). Approximately 45% of α-gustducin-positive colon cells were also positive for GPR43 or TGR5, and <20% of those cells expressed GPR120 or GPR119 (Fig. 2C). Because in colon over 70% of α-gustducin-positive cells expressed GLP-1 and/or GIP (Fig. 1D), then we can infer that, as long as >30% of α-gustducin-positive cells express fatty acid receptors, expression of these fatty acid receptors must also overlap with that of GLP-1 and/or GIP. Thus, cells coexpressing fatty acids and α-gustducin are most likely endocrine cells expressing one or both of these gut hormones. Specificity controls for the antibodies are shown in Supplemental Figs. 1 and 2. Quantitation of the colon endocrine cells coexpressing α-gustducin and these receptors showed that >60% of GPR41-, TGR5-, and GPR119-positive cells coexpressed α-gustducin, 40% of GPR40-positive cells coexpressed α-gustducin, and 17% of GPR120-positive cells coexpressed α-gustducin (Fig. 2B).
Fig. 2.
Coexpression of α-gustducin with fatty acid and bile acid receptors in mouse colon. A: immunofluorescent detection of α-gustducin (green) and short-chain fatty acid (SCFA) G protein-coupled receptor (GPR) 43 and GPR41, long-chain fatty acid (LCFA) receptors GPR40 and GPR120, bile acid receptor TGR5, and oleoylethanolamide (OEA) receptor GPR119 (red) in mouse proximal colon (scale bar, 16 μm). B: percentage of fatty acid or bile acid receptor-positive cells in mouse proximal colon coexpressing α-gustducin. Values are means ± SE from three sections. C: percentage of α-gustducin-positive cells in mouse proximal colon coexpressing fatty acid or bile acid receptors. Values are means ± SE from three sections.
To independently confirm that these fatty acid receptors are expressed in mouse colon, we performed in situ hybridization for SCFA receptors GPR41 and GPR43 and LCFA receptor GPR40. mRNAs for the GPR40, GPR41, and GPR43 receptors were found to be expressed in a subset of epithelial cells in mouse colon (Supplemental Fig. 3). Note that the number of positive cells for GPR41 mRNA was much lower than that of GPR40 and GPR43. Taken together, the frequent coexpression of α-gustducin with fatty acid and bile acid receptors suggests that, in colon, α-gustducin might couple to these receptors to mediate signal transduction.
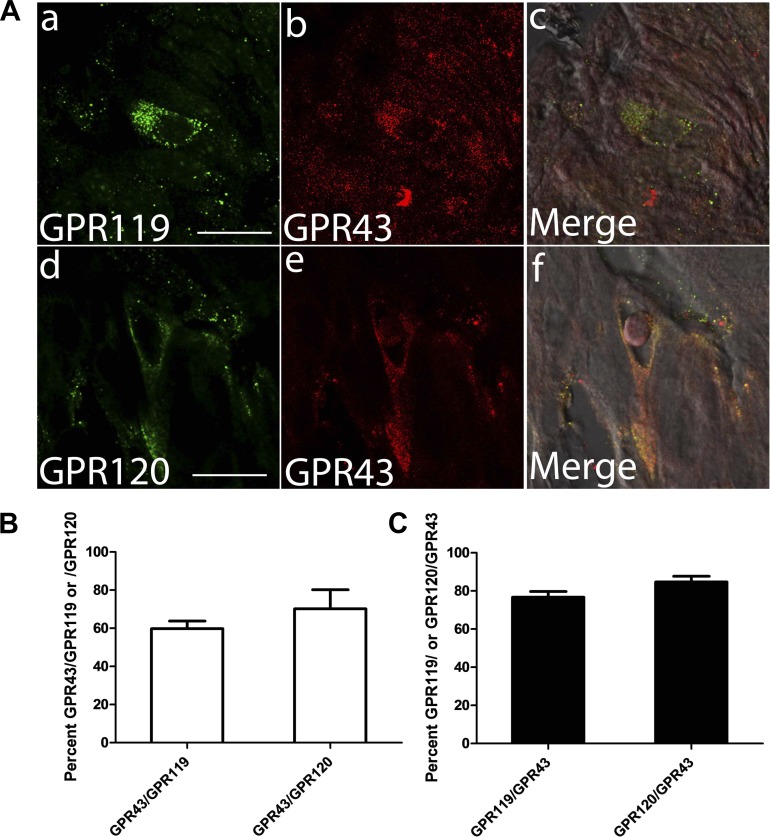
Coexpression of GPR43 with GPR120 and GPR119 but not with TGR5 in colon.
Next we examined whether these fatty acid and bile acid receptors were coexpressed in colon epithelial cells. Because of the high percentage of cells coexpressing GPR43 and α-gustducin, and limitations from the species of origin of our primary antibodies, double-labeled immunofluorescence was performed only with primary antibodies against GPR43 (raised from goat) and GPR120, GPR119, or TGR5 (all raised from rabbit). As shown in Fig. 3A, a subset of GPR43-positive cells also expressed GPR119 and GPR120. More than 60% of GPR119- and GPR120-positive cells expressed GPR43, and ∼80% of GPR43-staining cells also expressed GPR119 or GPR120 (Fig. 3, B and C). These data suggest that multiple fatty acid-sensing pathways could be present in a single cell. Note, however, that we found GPR43 and TGR5 to not be coexpressed together in mouse colon epithelial cells (Supplemental Fig. 4).
Fig. 3.
GPR43 is coexpressed with GPR119 and GPR120. A: immunofluorescent detection in mouse proximal colon of SCFA receptor GPR43 (red) and OEA receptor GPR119 or LCFA receptor GPR120 (green) (scale bar, 16 μm). B: percentage of GPR119-positive or GPR120-positive cells coexpressing GPR43. Values are means ± SE from three sections. C: percentage of GPR43-positive cells coexpressing GPR119 or GPR120. Values are means ± SE from three sections.
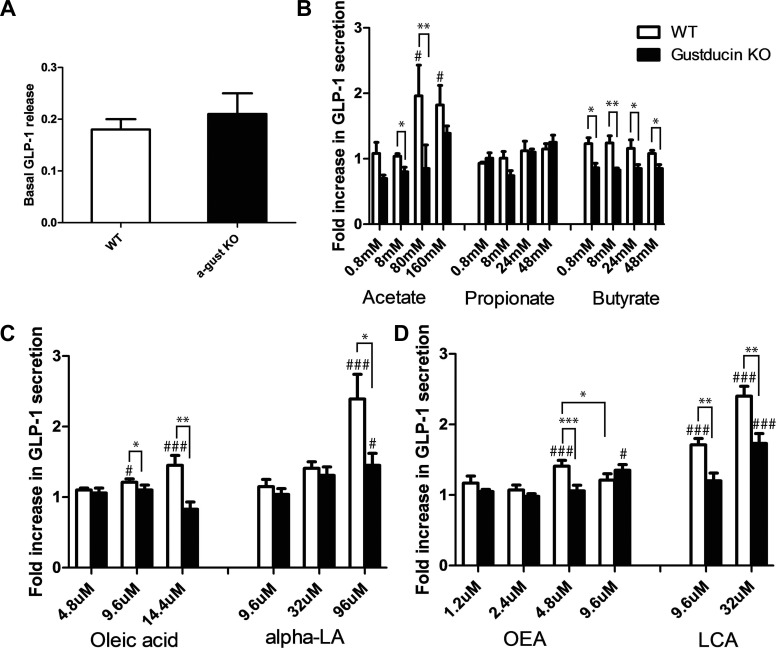
GLP-1 release in response to fatty acids in colonic tissue from α-gustducin knockout mice.
Given the coexpression of α-gustducin and GLP-1 with fatty acid or bile acid receptors, we hypothesized that activation of one or more of these receptors could couple to α-gustducin to induce secretion of GLP-1. To examine this hypothesis, GLP-1 secretion in response to fatty acids and bile acids was measured in colonic tissue isolated from wild-type and α-gustducin knockout mice. Basal GLP-1 release was not significantly different between the two groups (Fig. 4A). Treatment of wild-type tissue with acetate (80 or 160 mM), oleic acid (9.6 or 14.4 μM), α-linolenic acid (α-LA, 96 μM), OEA (4.8 μM), and lithocholic acid (LCA, 9.6 and 32 μM) stimulated GLP-1 secretion significantly compared with the nontreated group (Fig. 4, B–D). In contrast, α-gustducin knockout colon tissue did not display any increase of GLP-1 release in response to the tested SCFAs and LCFA oleic acid (Fig. 4, B and C). α-LA (96 μM), a potent agonist for both LCFA receptors GPR40 and GPR120 (28, 34), only slightly increased release of GLP-1 in α-gustducin knockout colon tissue (Fig. 4C). Surprisingly, with the concentrations of propionate and butyrate tested, we did not observe an increase of GLP-1 secretion from wild-type tissue. This contrasts with receptor activation seen in heterologous cell lines cotransfected with GPR41 or GPR43 and Giα (6, 47). This difference could be because of higher expression in heterologous systems or differences in ligand response due to coupling of the receptors to α-gustducin in primary colon tissue vs. Giα in the cell lines.
Fig. 4.
Impaired GLP-1 secretion from colon tissue of α-gustducin knockout mice in response to fatty acids. A: basal GLP-1 release in glucose-free, BSA-free Hanks' buffered salt solution from colon mucosa of α-gustducin knockout (filled bar) vs. wild-type (open bar) mice. B–D: GLP-1 secretion in response to SCFAs, LCFAs, OEA, and bile acids from colon mucosa of α-gustducin knockout (filled bar) vs. wild-type (open bar) mice. Data were generated in triplicate for each mouse, with n = 3–6 mice for each genotype, and are expressed as means ± SE. Statistical significance was determined by ANOVA and Student's unpaired two-tailed t-test. *P < 0.05, **P < 0.01, and ***P < 0.001, gustducin knockout vs. wild-type mice. #P < 0.05 and ###P < 0.001, fatty acid-treated vs. basal GLP-1 release.
OEA at high concentration (9.6 μM), but not at low concentration (4.8 μM), decreased GLP-1 secretion from colon tissue of wild-type mice (Fig. 4D). A similar trend has been shown in an L-type enteroendocrine cell line (46), increasing GLP-1 release at a low dose (5–10 μM) and decreasing it at a high dose (15 μM), although the primary colonic tissue in our study exhibited higher sensitivity to OEA, with an inhibition of GLP-1 secretion at 9.6 μM. The opposite effect was observed in α-gustducin knockout colon tissue where the high concentration of OEA (9.6 μM) induced GLP-1 secretion (Fig. 4D). This could be because of a right shift of the OEA response curve in the α-gustducin knockout tissue to become less sensitive to the low concentration (4.8 μM) of OEA. The bile acid LCA increased GLP-1 secretion in colon tissue from both wild-type and α-gustducin null mice. However, colon tissue from α-gustducin null mice showed a significantly lower fold increase in the GLP-1 response to LCA compared with that of wild-type tissue (Fig. 4D).
DISCUSSION
The G protein subunit α-gustducin is expressed in ∼20% of taste receptor cells, where it is a key mediator of bitter, sweet, and umami (glutamate) taste transduction (27, 55, 91). α-Gustducin is also present in enteroendocrine cells and brush cells of the gastrointestinal tract in both humans and rodents (3, 29, 74, 82). In enteroendocrine cells of the small intestine, α-gustducin is frequently coexpressed with the incretin hormones GLP-1 and GIP (35, 51). α-Gustducin is also present in GLP-1-positive enteroendocrine cells in colon (3, 74). Mice lacking α-gustducin display impaired GLP-1 secretion in response to glucose gavage (35). Furthermore, sweetener-stimulated GLP-1 release from isolated small intestine from α-gustducin null mice is deficient. Experiments with enteroendocrine cell lines implicate both α-gustducin and the T1r2+T1r3 sweet receptor in GIP and GLP-1 release (35, 51).
GLP-1 is secreted from intestinal endocrine L cells, which are located mainly in the distal ileum and colon. In contrast, GIP is released from intestinal K cells, which are localized to more proximal regions (duodenum and jejunum) of the small intestine. However, endocrine cells that produce either GLP-1 or GIP, as well as cells that produce both peptides (L/K cells), can be found throughout all regions of the small intestine (see review in Refs. 2 and 30). In the present study, we find that there are many more α-gustducin-expressing cells in colon than in small intestine. In colon, α-gustducin is frequently coexpressed with GLP-1, GIP, or both. Interestingly, in duodenum and jejunum, very few of the α-gustducin-expressing cells were found to be L cells (i.e., expressed only GLP-1), instead these cells expressed either GIP (K cells) or both GIP and GLP-1 (L/K cells). Importantly, the percentage of L-type cells among the α-gustducin-expressing cells increased from near 0% in small intestine to ∼29% in colon, suggesting that colonic L cells could histologically and functionally differ from the L cells in the small intestine.
In human subjects with ileostomies, the circulating GLP-1 levels after a fat load are significantly reduced compared with healthy control subjects, suggesting that loss of colonic endocrine tissue is an important determinant in regulating postprandial GLP-1 levels (72). In vivo studies of rodents and humans have shown that increased SCFA production after dietary fiber ingestion increases GLP-1 levels (19, 70, 97). A recent study has found that SCFAs trigger secretion of GLP-1 by increasing cytosolic Ca2+ in L cells in primary culture. Mice lacking SCFA receptors GPR41 or GPR43 exhibit reduced SCFA-triggered GLP-1 secretion in vivo and ex vivo (88). These studies suggest that direct stimulation of colonic L cells with SCFAs could promote GLP-1 secretion.
GPR41 and GPR43 mRNAs are widely expressed in various tissues, including adipose tissue, intestine, and immune cells (6, 22, 31, 41, 47, 52, 61). In addition, GPR43 is expressed in GLP-1-positive colon cells in both humans and rats (37). In vivo studies have shown that GPR41 is tightly involved in energy homeostasis by stimulating leptin production (93), reducing caloric extraction (76), and promoting activity of the sympathetic nervous system (41). GPR43-deficient mice display exacerbated inflammation in dextran sulfate sodium-induced colitis (52) and are protected from high-fat-diet-induced metabolic syndrome (4). Ex vivo studies show that activation of GPR43 leads to neutrophil chemotaxis (47, 89) and inhibition of lipolysis in adipocytes (22, 31). Human GPR41 and GPR43 receptors can be activated by short carboxylic acids containing one to six carbons (6, 47, 61). In heterogeneously expressed cell lines, activation of GPR41 or GPR43 inhibits cAMP accumulation and induces inositol trisphosphate formation, intracellular Ca2+ release, and phosphorylation of p42/44 mitogen-activated protein (MAP) kinase (6, 47). In addition, pertussis toxin abolishes the Ca2+ response elicited by GPR41 but not that of GPR43. This suggests that GPR43 may activate Gq in addition to Gi family G proteins that include gustducin and the transducins (6, 47).
The LCFA receptor GPR40 is highly expressed in pancreatic β-cells (5, 18, 34, 42) and also found in endocrine cells in gut where it is frequently coexpressed with gastrin, the incretin hormones GLP-1 and GIP, ghrelin, cholecystokinin (CCK), PYY, secretin, or serotonin (15). GPR40 plays a role in acute free fatty acid (FFA)-induced secretion of insulin (15, 34, 43, 45, 57, 77, 78, 81), GIP, GLP-1 (15), and CCK (49). Medium-chain fatty acids and LCFAs activate GPR40, which in cell lines and rat β-cells couples to insulin release via a Gq-phospholipase C (PLC)-Ca influx pathway (5, 21, 34, 42, 77, 78). In addition, activation of GPR40 by FFA also reduces the voltage-gated K+ current in rat β-cells through protein kinase A, leading to an increase in intracellular Ca2+ and insulin secretion (16).
GPR120 is highly expressed in mature adipocytes, macrophages, enteroendocrine GLP-1-positive cells, and K cells (28, 63, 65). GPR120 is involved in adipogenic processes (25), inhibition of cytokine release (63), and secretion of GLP-1 and CCK from enteroendocrine cell lines (28, 32, 83). GPR120-deficient mice on a high-fat diet display more severe insulin resistance (63), obesity, and liver steatosis (33), suggesting a protective role of GPR120 in metabolic syndrome. In addition, GPR120 and GPR40 are also expressed in taste papillae of mice: GPR120 is mainly in type II taste cells (53); GPR40 is in type I and type II cells (7). In vivo studies have shown that GPR40 and GPR120 mediate the taste of fatty acids (7). Medium- and long-chain FFAs activate GPR120 and evoke a rise in intracellular Ca2+ and increase the amount of phosphorylated extracellular signal-regulated p42/44 MAP kinase in heterogeneously expressed cell lines and in the STC-1 enteroendocrine cell line (28). However, FFA-induced GLP-1 secretion in GLUTag cells is involved in PKCζ but not protein kinase B, MAP kinase, or Ca2+ responses (32), suggesting that GPR120 could couple to diverse downstream signaling elements to mediate GLP-1 release.
High levels of TGR5 mRNA are detected in spleen, lung, liver, stomach, intestine, adipose tissue, gallbladder, and bone marrow in human and mouse (39, 66). Activation of TGR5 induces GLP-1 secretion in vivo and ex vivo (20, 38, 85), improves glucose tolerance and enhances insulin secretion (85), and prevents and reverses diet-inducing obesity (85, 90). In addition, TGR5 inhibits cytokine production in macrophages and inhibits macrophage foam cell formation, reduces vascular lesion formation (66), and attenuates colon inflammation in rodent models of colitis (10). Activation of TGR5 in response to bile acids induces cAMP production and increases MAP kinase activity in heterogeneously transfected cell lines (39, 40, 90), suggesting that it couples via a G protein to increase cAMP.
GPR119 is expressed in β-cells of pancreatic islets (9, 44) and GLP-1-positive cells in the gastrointestinal tract (8). In vivo studies have shown that activation of GPR119 stimulates GLP-1 and GIP release, improves glucose tolerance, and increases insulin release (8, 11, 17, 46). In addition, GPR119 also plays a role in decreasing food intake and body weight gain in diet-induced obese rats (64), reducing gastric emptying (17), and inhibiting Cl− secretion in colonic mucosa (11). OEA, the most efficacious ligand for both human and mouse GPR119, increases cAMP levels in heterogeneous cells (64). Activation of GPR119 increases insulin secretion in pancreatic β-cell lines via both cAMP accumulation and increased intracellular Ca2+ (62, 80) and stimulates GLP-1 release from intestinal cell lines via cAMP accumulation (8, 46).
In the present study, we have found that intestinal α-gustducin is coexpressed with several fatty acid receptors and the bile acid receptor TGR5. In taste cells, heterotrimeric gustducin decreases cAMP (via α-subunit activation of phosphodiesterase) (56, 75) and increases intracellular Ca2+ levels (via βγ-subunits' actions on PLC) (94). It is likely that gustducin is involved in GLP-1 release from intestinal cells in response to SCFAs and LCFAs. This is supported by our observation of impaired GLP-1 release in mucosal tissue from α-gustducin knockout mice in response to fatty acids. We also found that intestinal tissue from α-gustducin knockout mice displayed impaired GLP-1 release in response to OEA and bile acid, suggesting that α-gustducin also participates in GPR119- and TGR5-activated pathways in enteroendocrine cells. Coexpression of multiple fatty acid receptors together with α-gustducin in intestine suggests that multiple sensing pathways are present in endocrine cells in the gut for efficient stimulation of GLP-1 release. Given the broad range of fatty acids in colon lumen under physiological conditions, a combination of SCFAs and LCFAs could act additively as potent agonists to induce GLP-1 secretion.
After oral nutrient ingestion, plasma GLP-1 levels rise in a biphasic pattern starting with an early phase (peak within 10–15 min) followed by a longer (30–60 min) second phase. Two models to explain GLP-1 release after meal ingestion have been proposed: a proximal-distal loop and a direct stimulation of L cells by luminal sugars (87). The proximal-distal loop proposes that nutrient detectors located in upper regions of the gastrointestinal tract control the release of GLP-1 from distal L cells by neural, most likely vagal (73), or hormonal (for example, GIP) (71) mechanisms. The potential mechanisms underlying direct stimulation of L cells by luminal sugars include KATP (68), SGLT1 (26, 69), and sweet taste receptors (35). Given the abundance of GLP-1-positive cells in the colon, GLP-1 release in response to local fatty acids could contribute to the plasma GLP-1 increase after a meal. Meals can induce colon motor activity within 10 min through the gastrocolic reflex (67, 79, 92). This reflex could change the colonic fatty acid concentrations and stimulate L cells in colon to release GLP-1 during the early phase of a meal.
Our data indicate that α-gustducin in colon is a key signaling molecule coupling fatty acid and bile acid receptors to GLP-1 secretion. Agonists that enhance GLP-1 secretion from the α-gustducin-expressing colon cells that respond to FFAs may serve as a novel target for the treatment of diabetes.
GRANTS
This research was supported by National Institutes of Health (NIH) Grant DK-081421 to R. F. Margolskee. Imaging was performed at the Monell Histology and Cellular Localization Core, which is supported, in part, by funding from the NIH Core Grant 1P30DC-011735–01.
DISCLOSURES
The authors declare that they have no conflicts of interest.
AUTHOR CONTRIBUTIONS
Author contributions YL, ZK, BM and RFM designed experiments; YL collected and analyzed data; all authors contributed to writing the manuscript.
ACKNOWLEDGMENTS
We thank Dr. Karen K. Yee for confocal microscopy training.
Footnotes
Readers are herein alerted to the fact that supplementary figures for this paper may be found at the institutional website of one of the authors, which at the time of publication they indicate is: [http://www.monell.org/supplemental/rm0113]. These materials are not a part of this manuscript, and have not undergone peer review by the American Physiological Society (APS). APS and the journal editors take no responsibility for these materials, for the website address, or for any links to or from it.
REFERENCES
- 1. Almendingen K, Hostmark AT, Larsen LN, Fausa O, Bratlie J, Aabakken L. Relationship between fecal content of fatty acids and cyclooxygenase mrna expression and fatty acid composition in duodenal biopsies, serum lipoproteins, and dietary fat in colectomized familial adenomatous polyposis patients (Abstract). J Nutr Metab 2010: 862569, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology 132: 2131– 2157, 2007 [DOI] [PubMed] [Google Scholar]
- 3. Bezencon C, le Coutre J, Damak S. Taste-signaling proteins are coexpressed in solitary intestinal epithelial cells. Chem Senses 32: 41– 49, 2007 [DOI] [PubMed] [Google Scholar]
- 4. Bjursell M, Admyre T, Goransson M, Marley AE, Smith DM, Oscarsson J, Bohlooly YM. Improved glucose control and reduced body fat mass in free fatty acid receptor 2-deficient mice fed a high-fat diet. Am J Physiol Endocrinol Metab 300: E211– E220, 2011 [DOI] [PubMed] [Google Scholar]
- 5. Briscoe CP, Tadayyon M, Andrews JL, Benson WG, Chambers JK, Eilert MM, Ellis C, Elshourbagy NA, Goetz AS, Minnick DT, Murdock PR, Sauls HR, Jr, Shabon U, Spinage LD, Strum JC, Szekeres PG, Tan KB, Way JM, Ignar DM, Wilson S, Muir AI. The orphan G protein-coupled receptor GPR40 is activated by medium and long chain fatty acids. J Biol Chem 278: 11303– 11311, 2003 [DOI] [PubMed] [Google Scholar]
- 6. Brown AJ, Goldsworthy SM, Barnes AA, Eilert MM, Tcheang L, Daniels D, Muir AI, Wigglesworth MJ, Kinghorn I, Fraser NJ, Pike NB, Strum JC, Steplewski KM, Murdock PR, Holder JC, Marshall FH, Szekeres PG, Wilson S, Ignar DM, Foord SM, Wise A, Dowell SJ. The Orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem 278: 11312– 11319, 2003 [DOI] [PubMed] [Google Scholar]
- 7. Cartoni C, Yasumatsu K, Ohkuri T, Shigemura N, Yoshida R, Godinot N, le Coutre J, Ninomiya Y, Damak S. Taste preference for fatty acids is mediated by GPR40 and GPR120. J Neurosci 30: 8376– 8382, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chu ZL, Carroll C, Alfonso J, Gutierrez V, He H, Lucman A, Pedraza M, Mondala H, Gao H, Bagnol D, Chen R, Jones RM, Behan DP, Leonard J. A role for intestinal endocrine cell-expressed g protein-coupled receptor 119 in glycemic control by enhancing glucagon-like peptide-1 and glucose-dependent insulinotropic Peptide release. Endocrinology 149: 2038– 2047, 2008 [DOI] [PubMed] [Google Scholar]
- 9. Chu ZL, Jones RM, He H, Carroll C, Gutierrez V, Lucman A, Moloney M, Gao H, Mondala H, Bagnol D, Unett D, Liang Y, Demarest K, Semple G, Behan DP, Leonard J. A role for beta-cell-expressed G protein-coupled receptor 119 in glycemic control by enhancing glucose-dependent insulin release. Endocrinology 148: 2601– 2609, 2007 [DOI] [PubMed] [Google Scholar]
- 10. Cipriani S, Mencarelli A, Chini MG, Distrutti E, Renga B, Bifulco G, Baldelli F, Donini A, Fiorucci S. The bile acid receptor GPBAR-1 (TGR5) modulates integrity of intestinal barrier and immune response to experimental colitis. PLoS One 6: e25637, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cox HM, Tough IR, Woolston AM, Zhang L, Nguyen AD, Sainsbury A, Herzog H. Peptide YY is critical for acylethanolamine receptor Gpr119-induced activation of gastrointestinal mucosal responses. Cell Metab 11: 532– 542, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cummings JH. Short chain fatty acids in the human colon. Gut 22: 763– 779, 1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Drucker DJ. The role of gut hormones in glucose homeostasis. J Clin Invest 117: 24– 32, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dyer J, Salmon KS, Zibrik L, Shirazi-Beechey SP. Expression of sweet taste receptors of the T1R family in the intestinal tract and enteroendocrine cells. Biochem Soc Trans 33: 302– 305, 2005 [DOI] [PubMed] [Google Scholar]
- 15. Edfalk S, Steneberg P, Edlund H. Gpr40 is expressed in enteroendocrine cells and mediates free fatty acid stimulation of incretin secretion. Diabetes 57: 2280– 2287, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Feng DD, Luo Z, Roh SG, Hernandez M, Tawadros N, Keating DJ, Chen C. Reduction in voltage-gated K+ currents in primary cultured rat pancreatic beta-cells by linoleic acids. Endocrinology 147: 674– 682, 2006 [DOI] [PubMed] [Google Scholar]
- 17. Flock G, Holland D, Seino Y, Drucker DJ. GPR119 regulates murine glucose homeostasis through incretin receptor-dependent and independent mechanisms. Endocrinology 152: 374– 383, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Flodgren E, Olde B, Meidute-Abaraviciene S, Winzell MS, Ahren B, Salehi A. GPR40 is expressed in glucagon producing cells and affects glucagon secretion. Biochem Biophys Res Commun 354: 240– 245, 2007 [DOI] [PubMed] [Google Scholar]
- 19. Freeland KR, Wilson C, Wolever TM. Adaptation of colonic fermentation and glucagon-like peptide-1 secretion with increased wheat fibre intake for 1 year in hyperinsulinaemic human subjects. Br J Nutr 103: 82– 90, 2010 [DOI] [PubMed] [Google Scholar]
- 20. Friedlander RS, Moss CE, Mace J, Parker HE, Tolhurst G, Habib AM, Wachten S, Cooper DM, Gribble FM, Reimann F. Role of phosphodiesterase and adenylate cyclase isozymes in murine colonic glucagon-like peptide 1 secreting cells. Br J Pharmacol 163: 261– 271, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fujiwara K, Maekawa F, Yada T. Oleic acid interacts with GPR40 to induce Ca2+ signaling in rat islet β-cells: mediation by PLC and L-type Ca2+ channel and link to insulin release. Am J Physiol Endocrinol Metab 289: E670– E677, 2005 [DOI] [PubMed] [Google Scholar]
- 22. Ge H, Li X, Weiszmann J, Wang P, Baribault H, Chen JL, Tian H, Li Y. Activation of G protein-coupled receptor 43 in adipocytes leads to inhibition of lipolysis and suppression of plasma free fatty acids. Endocrinology 149: 4519– 4526, 2008 [DOI] [PubMed] [Google Scholar]
- 23. Gibson GR, Roberfroid MB. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr 125: 1401– 1412, 1995 [DOI] [PubMed] [Google Scholar]
- 24. Gorboulev V, Schurmann A, Vallon V, Kipp H, Jaschke A, Klessen D, Friedrich A, Scherneck S, Rieg T, Cunard R, Veyhl-Wichmann M, Srinivasan A, Balen D, Breljak D, Rexhepaj R, Parker HE, Gribble FM, Reimann F, Lang F, Wiese S, Sabolic I, Sendtner M, Koepsell H. Na(+)-d-glucose cotransporter SGLT1 is pivotal for intestinal glucose absorption and glucose-dependent incretin secretion. Diabetes 61: 187– 196, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gotoh C, Hong YH, Iga T, Hishikawa D, Suzuki Y, Song SH, Choi KC, Adachi T, Hirasawa A, Tsujimoto G, Sasaki S, Roh SG. The regulation of adipogenesis through GPR120. Biochem Biophys Res Commun 354: 591– 597, 2007 [DOI] [PubMed] [Google Scholar]
- 26. Gribble FM, Williams L, Simpson AK, Reimann F. A novel glucose-sensing mechanism contributing to glucagon-like peptide-1 secretion from the GLUTag cell line. Diabetes 52: 1147– 1154, 2003 [DOI] [PubMed] [Google Scholar]
- 27. He W, Danilova V, Zou S, Hellekant G, Max M, Margolskee RF, Damak S. Partial rescue of taste responses of alpha-gustducin null mice by transgenic expression of alpha-transducin. Chem Senses 27: 719– 727, 2002 [DOI] [PubMed] [Google Scholar]
- 28. Hirasawa A, Tsumaya K, Awaji T, Katsuma S, Adachi T, Yamada M, Sugimoto Y, Miyazaki S, Tsujimoto G. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med 11: 90– 94, 2005 [DOI] [PubMed] [Google Scholar]
- 29. Hofer D, Puschel B, Drenckhahn D. Taste receptor-like cells in the rat gut identified by expression of alpha-gustducin. Proc Natl Acad Sci USA 93: 6631– 6634, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev 87: 1409– 1439, 2007 [DOI] [PubMed] [Google Scholar]
- 31. Hong YH, Nishimura Y, Hishikawa D, Tsuzuki H, Miyahara H, Gotoh C, Choi KC, Feng DD, Chen C, Lee HG, Katoh K, Roh SG, Sasaki S. Acetate and propionate short chain fatty acids stimulate adipogenesis via GPCR43. Endocrinology 146: 5092– 5099, 2005 [DOI] [PubMed] [Google Scholar]
- 32. Iakoubov R, Izzo A, Yeung A, Whiteside CI, Brubaker PL. Protein kinase Czeta is required for oleic acid-induced secretion of glucagon-like peptide-1 by intestinal endocrine L cells. Endocrinology 148: 1089– 1098, 2007 [DOI] [PubMed] [Google Scholar]
- 33. Ichimura A, Hirasawa A, Poulain-Godefroy O, Bonnefond A, Hara T, Yengo L, Kimura I, Leloire A, Liu N, Iida K, Choquet H, Besnard P, Lecoeur C, Vivequin S, Ayukawa K, Takeuchi M, Ozawa K, Tauber M, Maffeis C, Morandi A, Buzzetti R, Elliott P, Pouta A, Jarvelin MR, Korner A, Kiess W, Pigeyre M, Caiazzo R, Van Hul W, Van Gaal L, Horber F, Balkau B, Levy-Marchal C, Rouskas K, Kouvatsi A, Hebebrand J, Hinney A, Scherag A, Pattou F, Meyre D, Koshimizu TA, Wolowczuk I, Tsujimoto G, Froguel P. Dysfunction of lipid sensor GPR120 leads to obesity in both mouse and human. Nature 483: 350– 354, 2012 [DOI] [PubMed] [Google Scholar]
- 34. Itoh Y, Kawamata Y, Harada M, Kobayashi M, Fujii R, Fukusumi S, Ogi K, Hosoya M, Tanaka Y, Uejima H, Tanaka H, Maruyama M, Satoh R, Okubo S, Kizawa H, Komatsu H, Matsumura F, Noguchi Y, Shinohara T, Hinuma S, Fujisawa Y, Fujino M. Free fatty acids regulate insulin secretion from pancreatic beta cells through GPR40. Nature 422: 173– 176, 2003 [DOI] [PubMed] [Google Scholar]
- 35. Jang HJ, Kokrashvili Z, Theodorakis MJ, Carlson OD, Kim BJ, Zhou J, Kim HH, Xu X, Chan SL, Juhaszova M, Bernier M, Mosinger B, Margolskee RF, Egan JM. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc Natl Acad Sci USA 104: 15069– 15074, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jeppesen PB, Mortensen PB. The influence of a preserved colon on the absorption of medium chain fat in patients with small bowel resection. Gut 43: 478– 483, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kaji I, Karaki S, Tanaka R, Kuwahara A. Density distribution of free fatty acid receptor 2 (FFA2)-expressing and GLP-1-producing enteroendocrine L cells in human and rat lower intestine, and increased cell numbers after ingestion of fructo-oligosaccharide. J Mol Histol 42: 27– 38, 2011 [DOI] [PubMed] [Google Scholar]
- 38. Katsuma S, Hirasawa A, Tsujimoto G. Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Commun 329: 386– 390, 2005 [DOI] [PubMed] [Google Scholar]
- 39. Kawamata Y, Fujii R, Hosoya M, Harada M, Yoshida H, Miwa M, Fukusumi S, Habata Y, Itoh T, Shintani Y, Hinuma S, Fujisawa Y, Fujino M. A G protein-coupled receptor responsive to bile acids. J Biol Chem 278: 9435– 9440, 2003 [DOI] [PubMed] [Google Scholar]
- 40. Keitel V, Donner M, Winandy S, Kubitz R, Haussinger D. Expression and function of the bile acid receptor TGR5 in Kupffer cells. Biochem Biophys Res Commun 372: 78– 84, 2008 [DOI] [PubMed] [Google Scholar]
- 41. Kimura I, Inoue D, Maeda T, Hara T, Ichimura A, Miyauchi S, Kobayashi M, Hirasawa A, Tsujimoto G. Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41). Proc Natl Acad Sci USA 108: 8030– 8035, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kotarsky K, Nilsson NE, Flodgren E, Owman C, Olde B. A human cell surface receptor activated by free fatty acids and thiazolidinedione drugs. Biochem Biophys Res Commun 301: 406– 410, 2003 [DOI] [PubMed] [Google Scholar]
- 43. Lan H, Hoos LM, Liu L, Tetzloff G, Hu W, Abbondanzo SJ, Vassileva G, Gustafson EL, Hedrick JA, Davis HR. Lack of FFAR1/GPR40 does not protect mice from high-fat diet-induced metabolic disease. Diabetes 57: 2999– 3006, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lan H, Vassileva G, Corona A, Liu L, Baker H, Golovko A, Abbondanzo SJ, Hu W, Yang S, Ning Y, Del Vecchio RA, Poulet F, Laverty M, Gustafson EL, Hedrick JA, Kowalski TJ. GPR119 is required for physiological regulation of glucagon-like peptide-1 secretion but not for metabolic homeostasis. J Endocrinol 201: 219– 230, 2009 [DOI] [PubMed] [Google Scholar]
- 45. Latour MG, Alquier T, Oseid E, Tremblay C, Jetton TL, Luo J, Lin DC, Poitout V. GPR40 is necessary but not sufficient for fatty acid stimulation of insulin secretion in vivo. Diabetes 56: 1087– 1094, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lauffer LM, Iakoubov R, Brubaker PL. GPR119 is essential for oleoylethanolamide-induced glucagon-like peptide-1 secretion from the intestinal enteroendocrine L-cell. Diabetes 58: 1058– 1066, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Le Poul E, Loison C, Struyf S, Springael JY, Lannoy V, Decobecq ME, Brezillon S, Dupriez V, Vassart G, Van Damme J, Parmentier M, Detheux M. Functional characterization of human receptors for short chain fatty acids and their role in polymorphonuclear cell activation. J Biol Chem 278: 25481– 25489, 2003 [DOI] [PubMed] [Google Scholar]
- 48. Li X, Staszewski L, Xu H, Durick K, Zoller M, Adler E. Human receptors for sweet and umami taste. Proc Natl Acad Sci USA 99: 4692– 4696, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Liou AP, Lu X, Sei Y, Zhao X, Pechhold S, Carrero RJ, Raybould HE, Wank S. The G-protein-coupled receptor GPR40 directly mediates long-chain fatty acid-induced secretion of cholecystokinin. Gastroenterology 140: 903– 912, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Macfarlane GT, Gibson GR, Cummings JH. Comparison of fermentation reactions in different regions of the human colon. J Appl Bacteriol 72: 57– 64, 1992 [DOI] [PubMed] [Google Scholar]
- 51. Margolskee RF, Dyer J, Kokrashvili Z, Salmon KS, Ilegems E, Daly K, Maillet EL, Ninomiya Y, Mosinger B, Shirazi-Beechey SP. T1R3 and gustducin in gut sense sugars to regulate expression of Na+-glucose cotransporter 1. Proc Natl Acad Sci USA 104: 15075– 15080, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Maslowski KM, Vieira AT, Ng A, Kranich J, Sierro F, Yu D, Schilter HC, Rolph MS, Mackay F, Artis D, Xavier RJ, Teixeira MM, Mackay CR. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461: 1282– 1286, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Matsumura S, Eguchi A, Mizushige T, Kitabayashi N, Tsuzuki S, Inoue K, Fushiki T. Colocalization of GPR120 with phospholipase-Cbeta2 and alpha-gustducin in the taste bud cells in mice. Neurosci Lett 450: 186– 190, 2009 [DOI] [PubMed] [Google Scholar]
- 54. Max M, Shanker YG, Huang L, Rong M, Liu Z, Campagne F, Weinstein H, Damak S, Margolskee RF. Tas1r3, encoding a new candidate taste receptor, is allelic to the sweet responsiveness locus Sac. Nat Genet 28: 58– 63, 2001 [DOI] [PubMed] [Google Scholar]
- 55. McLaughlin SK, McKinnon PJ, Margolskee RF. Gustducin is a taste-cell-specific G protein closely related to the transducins. Nature 357: 563– 569, 1992 [DOI] [PubMed] [Google Scholar]
- 56. Moriyama K, Bakre MM, Ahmed F, Spickofsky N, Max M, Margolskee RF. Assaying G protein-phosphodiesterase interactions in sensory systems. Methods Enzymol 345: 37– 48, 2002 [DOI] [PubMed] [Google Scholar]
- 57. Nagasumi K, Esaki R, Iwachidow K, Yasuhara Y, Ogi K, Tanaka H, Nakata M, Yano T, Shimakawa K, Taketomi S, Takeuchi K, Odaka H, Kaisho Y. Overexpression of GPR40 in pancreatic beta-cells augments glucose-stimulated insulin secretion and improves glucose tolerance in normal and diabetic mice. Diabetes 58: 1067– 1076, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Nauck M, Stockmann F, Ebert R, Creutzfeldt W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29: 46– 52, 1986 [DOI] [PubMed] [Google Scholar]
- 59. Nauck MA, Homberger E, Siegel EG, Allen RC, Eaton RP, Ebert R, Creutzfeldt W. Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. J Clin Endocrinol Metab 63: 492– 498, 1986 [DOI] [PubMed] [Google Scholar]
- 60. Nelson G, Hoon MA, Chandrashekar J, Zhang Y, Ryba NJ, Zuker CS. Mammalian sweet taste receptors. Cell 106: 381– 390, 2001 [DOI] [PubMed] [Google Scholar]
- 61. Nilsson NE, Kotarsky K, Owman C, Olde B. Identification of a free fatty acid receptor, FFA2R, expressed on leukocytes and activated by short-chain fatty acids. Biochem Biophys Res Commun 303: 1047– 1052, 2003 [DOI] [PubMed] [Google Scholar]
- 62. Ning Y, O'Neill K, Lan H, Pang L, Shan LX, Hawes BE, Hedrick JA. Endogenous and synthetic agonists of GPR119 differ in signalling pathways and their effects on insulin secretion in MIN6c4 insulinoma cells. Br J Pharmacol 155: 1056– 1065, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Oh DY, Talukdar S, Bae EJ, Imamura T, Morinaga H, Fan W, Li P, Lu WJ, Watkins SM, Olefsky JM. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell 142: 687– 698, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Overton HA, Babbs AJ, Doel SM, Fyfe MC, Gardner LS, Griffin G, Jackson HC, Procter MJ, Rasamison CM, Tang-Christensen M, Widdowson PS, Williams GM, Reynet C. Deorphanization of a G protein-coupled receptor for oleoylethanolamide and its use in the discovery of small-molecule hypophagic agents. Cell Metab 3: 167– 175, 2006 [DOI] [PubMed] [Google Scholar]
- 65. Parker HE, Habib AM, Rogers GJ, Gribble FM, Reimann F. Nutrient-dependent secretion of glucose-dependent insulinotropic polypeptide from primary murine K cells. Diabetologia 52: 289– 298, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Pols TW, Nomura M, Harach T, Lo Sasso G, Oosterveer MH, Thomas C, Rizzo G, Gioiello A, Adorini L, Pellicciari R, Auwerx J, Schoonjans K. TGR5 activation inhibits atherosclerosis by reducing macrophage inflammation and lipid loading. Cell Metab 14: 747– 757, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Rao SS, Kavelock R, Beaty J, Ackerson K, Stumbo P. Effects of fat and carbohydrate meals on colonic motor response. Gut 46: 205– 211, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Reimann F, Gribble FM. Glucose-sensing in glucagon-like peptide-1-secreting cells. Diabetes 51: 2757– 2763, 2002 [DOI] [PubMed] [Google Scholar]
- 69. Reimann F, Habib AM, Tolhurst G, Parker HE, Rogers GJ, Gribble FM. Glucose sensing in L cells: a primary cell study. Cell Metab 8: 532– 539, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Reimer RA, McBurney MI. Dietary fiber modulates intestinal proglucagon messenger ribonucleic acid and postprandial secretion of glucagon-like peptide-1 and insulin in rats. Endocrinology 137: 3948– 3956, 1996 [DOI] [PubMed] [Google Scholar]
- 71. Roberge JN, Brubaker PL. Regulation of intestinal proglucagon-derived peptide secretion by glucose-dependent insulinotropic peptide in a novel enteroendocrine loop. Endocrinology 133: 233– 240, 1993 [DOI] [PubMed] [Google Scholar]
- 72. Robertson MD, Livesey G, Morgan LM, Hampton SM, Mathers JC. The influence of the colon on postprandial glucagon-like peptide 1 (7–36) amide concentration in man. J Endocrinol 161: 25– 31, 1999 [DOI] [PubMed] [Google Scholar]
- 73. Rocca AS, Brubaker PL. Role of the vagus nerve in mediating proximal nutrient-induced glucagon-like peptide-1 secretion. Endocrinology 140: 1687– 1694, 1999 [DOI] [PubMed] [Google Scholar]
- 74. Rozengurt N, Wu SV, Chen MC, Huang C, Sternini C, Rozengurt E. Colocalization of the α-subunit of gustducin with PYY and GLP-1 in L cells of human colon. Am J Physiol Gastrointest Liver Physiol 291: G792– G802, 2006 [DOI] [PubMed] [Google Scholar]
- 75. Ruiz-Avila L, McLaughlin SK, Wildman D, McKinnon PJ, Robichon A, Spickofsky N, Margolskee RF. Coupling of bitter receptor to phosphodiesterase through transducin in taste receptor cells. Nature 376: 80– 85, 1995 [DOI] [PubMed] [Google Scholar]
- 76. Samuel BS, Shaito A, Motoike T, Rey FE, Backhed F, Manchester JK, Hammer RE, Williams SC, Crowley J, Yanagisawa M, Gordon JI. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proc Natl Acad Sci USA 105: 16767– 16772, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Schnell S, Schaefer M, Schofl C. Free fatty acids increase cytosolic free calcium and stimulate insulin secretion from beta-cells through activation of GPR40. Mol Cell Endocrinol 263: 173– 180, 2007 [DOI] [PubMed] [Google Scholar]
- 78. Shapiro H, Shachar S, Sekler I, Hershfinkel M, Walker MD. Role of GPR40 in fatty acid action on the beta cell line INS-1E. Biochem Biophys Res Commun 335: 97– 104, 2005 [DOI] [PubMed] [Google Scholar]
- 79. Snape WJ, Jr, Wright SH, Battle WM, Cohen S. The gastrocolic response: evidence for a neural mechanism. Gastroenterology 77: 1235– 1240, 1979 [PubMed] [Google Scholar]
- 80. Soga T, Ohishi T, Matsui T, Saito T, Matsumoto M, Takasaki J, Matsumoto S, Kamohara M, Hiyama H, Yoshida S, Momose K, Ueda Y, Matsushime H, Kobori M, Furuichi K. Lysophosphatidylcholine enhances glucose-dependent insulin secretion via an orphan G-protein-coupled receptor. Biochem Biophys Res Commun 326: 744– 751, 2005 [DOI] [PubMed] [Google Scholar]
- 81. Steneberg P, Rubins N, Bartoov-Shifman R, Walker MD, Edlund H. The FFA receptor GPR40 links hyperinsulinemia, hepatic steatosis, and impaired glucose homeostasis in mouse. Cell Metab 1: 245– 258, 2005 [DOI] [PubMed] [Google Scholar]
- 82. Sutherland K, Young RL, Cooper NJ, Horowitz M, Blackshaw LA. Phenotypic characterization of taste cells of the mouse small intestine. Am J Physiol Gastrointest Liver Physiol 292: G1420– G1428, 2007 [DOI] [PubMed] [Google Scholar]
- 83. Tanaka T, Katsuma S, Adachi T, Koshimizu TA, Hirasawa A, Tsujimoto G. Free fatty acids induce cholecystokinin secretion through GPR120. Naunyn Schmiedebergs Arch Pharmacol 377: 523– 527, 2008 [DOI] [PubMed] [Google Scholar]
- 84. Thomas C, Pellicciari R, Pruzanski M, Auwerx J, Schoonjans K. Targeting bile-acid signalling for metabolic diseases. Nat Rev Drug Discov 7: 678– 693, 2008 [DOI] [PubMed] [Google Scholar]
- 85. Thomas C, Gioiello A, Noriega L, Strehle A, Oury J, Rizzo G, Macchiarulo A, Yamamoto H, Mataki C, Pruzanski M, Pellicciari R, Auwerx J, Schoonjans K. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab 10: 167– 177, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Toft-Nielsen MB, Damholt MB, Madsbad S, Hilsted LM, Hughes TE, Michelsen BK, Holst JJ. Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 86: 3717– 3723, 2001 [DOI] [PubMed] [Google Scholar]
- 87. Tolhurst G, Reimann F, Gribble FM. Nutritional regulation of glucagon-like peptide-1 secretion. J Physiol 587: 27– 32, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Tolhurst G, Heffron H, Lam YS, Parker HE, Habib AM, Diakogiannaki E, Cameron J, Grosse J, Reimann F, Gribble FM. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes 61: 364– 371, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Vinolo MA, Ferguson GJ, Kulkarni S, Damoulakis G, Anderson K, Bohlooly YM, Stephens L, Hawkins PT, Curi R. SCFAs induce mouse neutrophil chemotaxis through the GPR43 receptor. PLoS One 6: e21205, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Watanabe M, Houten SM, Mataki C, Christoffolete MA, Kim BW, Sato H, Messaddeq N, Harney JW, Ezaki O, Kodama T, Schoonjans K, Bianco AC, Auwerx J. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature 439: 484– 489, 2006 [DOI] [PubMed] [Google Scholar]
- 91. Wong GT, Gannon KS, Margolskee RF. Transduction of bitter and sweet taste by gustducin. Nature 381: 796– 800, 1996 [DOI] [PubMed] [Google Scholar]
- 92. Wright SH, Snape WJ, Jr, Battle W, Cohen S, London RL. Effect of dietary components on gastrocolonic response. Am J Physiol Gastrointest Liver Physiol 238: G228– G232, 1980 [DOI] [PubMed] [Google Scholar]
- 93. Xiong Y, Miyamoto N, Shibata K, Valasek MA, Motoike T, Kedzierski RM, Yanagisawa M. Short-chain fatty acids stimulate leptin production in adipocytes through the G protein-coupled receptor GPR41. Proc Natl Acad Sci USA 101: 1045– 1050, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Yan W, Sunavala G, Rosenzweig S, Dasso M, Brand JG, Spielman AI. Bitter taste transduced by PLC-β2-dependent rise in IP3 and α-gustducin-dependent fall in cyclic nucleotides. Am J Physiol Cell Physiol 280: C742– C751, 2001 [DOI] [PubMed] [Google Scholar]
- 95. Ye DZ, Kaestner KH. Foxa1 and Foxa2 control the differentiation of goblet and enteroendocrine L- and D-cells in mice. Gastroenterology 137: 2052– 2062, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Yee KK, Sukumaran SK, Kotha R, Gilbertson TA, Margolskee RF. Glucose transporters and ATP-gated K+ (KATP) metabolic sensors are present in type 1 taste receptor 3 (T1r3)-expressing taste cells. Proc Natl Acad Sci USA 108: 5431– 5436, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Zhou J, Martin RJ, Tulley RT, Raggio AM, McCutcheon KL, Shen L, Danna SC, Tripathy S, Hegsted M, Keenan MJ. Dietary resistant starch upregulates total GLP-1 and PYY in a sustained day-long manner through fermentation in rodents. Am J Physiol Endocrinol Metab 295: E1160– E1166, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]