Abstract
Formal guidelines for mentoring faculty members in pharmacy practice divisions of colleges and schools of pharmacy do not exist in the literature. This paper addresses the background literature on mentoring programs, explores the current state of mentoring programs used in pharmacy practice departments, and provides guidelines for colleges and schools instituting formal mentoring programs. As the number of pharmacy colleges and schools has grown, the demand for quality pharmacy faculty members has dramatically increased. While some faculty members gain teaching experience during postgraduate residency training, new pharmacy practice faculty members often need professional development to meet the demands of their academic responsibilities. A mentoring program can be 1 means of improving faculty success and retention. Many US colleges and schools of pharmacy have developed formal mentoring programs, whereas several others have informal processes in place. This paper discusses those programs and the literature available, and makes recommendations on the structure of mentoring programs.
Keywords: mentoring, faculty development, mentor, pharmacy practice, faculty
INTRODUCTION
As the number of pharmacy colleges and schools has grown in the last decade, the demand for quality pharmacy faculty members has dramatically increased as well. While some new faculty members gained teaching experience by completing a residency program before entering academia, new pharmacy practice faculty members often need professional development to prepare them to meet their various academic responsibilities. A mentoring program can be one means to improve faculty success and retention.
Whereas many US colleges and schools of pharmacy have developed formal mentoring programs and several others have informal processes in place, formal guidelines for mentoring faculty members do not exist. This paper addresses the background literature on mentoring programs, explores the current state of mentoring programs used in pharmacy practice departments, and provides guidelines for those colleges hoping to institute formal mentoring programs at their institutions.
Mentoring is defined as a “nurturing process, in which a more skilled or more experienced person, serving as a role model, teaches, sponsors, encourages, counsels, and befriends a less skilled or less experienced person for the purpose of promoting the latter’s professional and personal development.”1 The personal relationship between mentor and mentee allows the program to be individualized for the specific needs of the faculty member being mentored. The role of faculty mentoring in academia is an integral component in retaining junior faculty members, reducing workload stress, and encouraging long-term growth and success.2 Whether formal or informal, mentoring is a method of cultivating and building new leaders in an institution; it is a process that benefits mentees, mentors, and ultimately the academic institution. Mentors may become more engaged in their work and see this as a unique opportunity to impact another faculty member’s career and growth.3-5 Mentoring can also lead to increased job satisfaction and enhanced quality of life through development of a relationship with the mentee.3-5 For mentees, the mentoring relationship assists in the transition into their new role as academicians.4 Mentees are likely to experience greater satisfaction with their jobs, a lower risk of “burn-out” and job-related stress, and greater opportunities for success within the institution.3 Ultimately, mentoring is a symbiotic relationship between mentor and mentee6 that allows them to learn from one another, self-reflect, create opportunities for self-improvement, and ultimately contribute to the institution.
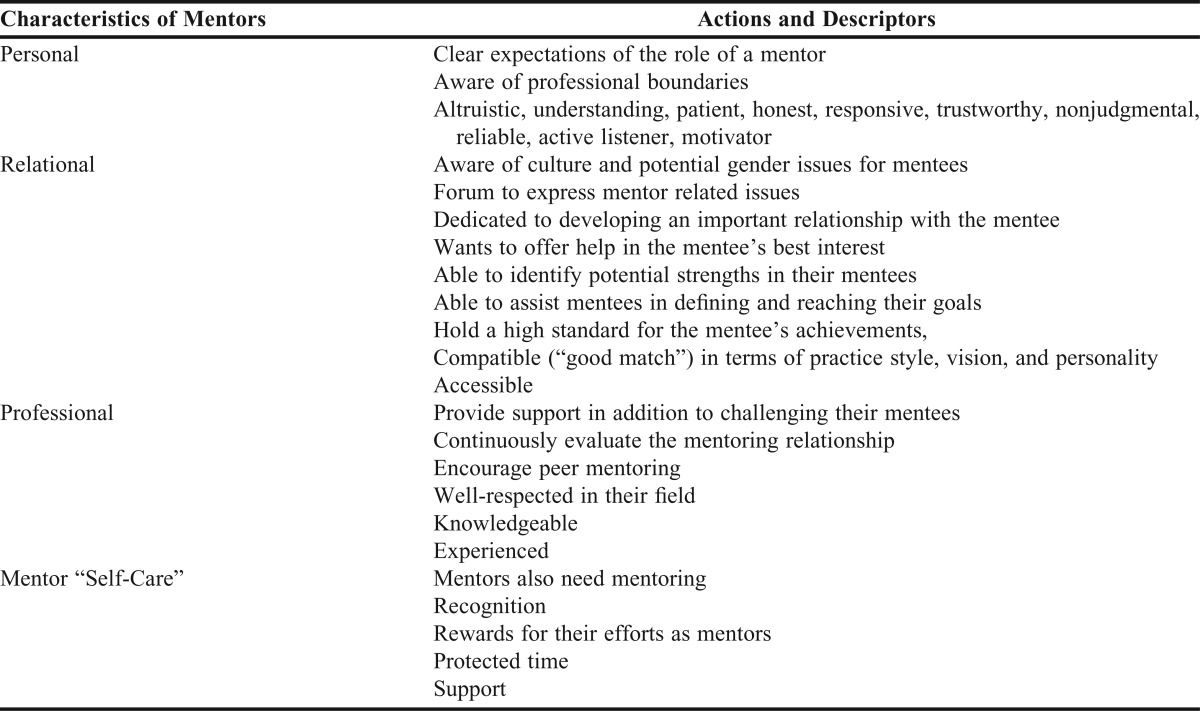
The primary attribute of a mentor is being a good role model for the mentee. According to Sambunjak and colleagues, mentors should be established faculty members who are capable of being sincere in their interactions with mentees, listening well, and providing constructive comments while understanding the needs of a mentee.7 Mentors should exhibit attributes related to their personality, relationships, and professional roles, such as patience, responsiveness, reliability, trustworthiness, ability to motivate, knowledge, and ability to assist mentees in identifying and accomplishing their goals.8-11 According to Ramani and colleagues who identified 12 areas that should be addressed to increase the ability and effectiveness of a mentor, mentors need to be confident, competent, and committed to the mentor-mentee relationship. 12,13 The better prepared and comfortable mentors are with their own strengths and weaknesses, the more likely they are to be effective mentors (Table 1).
Table 1.
Characteristics of Mentors7,12
The success of a mentor-mentee relationship is also shaped by the characteristics of the mentee. Attributes that have been identified as facilitating the likelihood of mentee success in a mentorship program include willingness to participate in development opportunities, recognition of the need for self-growth, self-awareness, ability to self-assess strengths and weaknesses, and receptiveness to feedback and coaching. They should have a record of seeking and accepting challenging assignments, be able to perform in more than 1 major skill area, understand the complexities of an academic career, and be trusting of the mentor.14
In the book Mentoring at Work: Developmental Relationships in Organizational Life, Kram describes the mentoring/mentee relationship as having 4 phases: initiation, cultivation, separation, and transformation.15 Early during the initiation phase, mutual interests may be identified while the mentor and mentee are getting comfortable with each other. The cultivation phase, which occurs over years, is the most robust aspect of the relationship. During this time, the relationship is highly productive and meaningful, and a strong personal and professional connection develops. The separation phase follows, bringing a change in the dynamic because of factors such as promotion, modification of the role or responsibility of the mentor or mentee resulting from the mentee’s professional maturation, and the mentee’s desire to be more independent. These factors have the potential to disrupt the relationship between a mentor and mentee. The redefinition phase outlines a new focus and goal for the mentor/mentee relationship. The nature of the relationship becomes one of peers working together rather than a senior faculty member assisting a junior faculty member. Kram identifies the mentor as providing both a vocational (educating, coaching, sponsoring) and psychosocial (acting as a role model, providing encouragement, counseling, and colleagueship) function. The goal of the vocational role is to promote advancement of the mentee, while the goal of the psychosocial role is to provide the mentee with a sense of identity, competence, and confidence.15
Mentors may provide guidance on a variety of academic areas including but not limited to teaching activities within the classroom and during clinical experiences; dealing with practice site issues; assisting with examination question development; offering guidance with scholarship endeavors; providing advice on how to get involved with service opportunities both inside the institution and externally to patients and professional organizations; and preparing for the promotion and tenure process. Ultimately, mentors serve as a resource and guide to encourage and assist mentees on the path to success.
Mentoring programs can be either formal or informal. In formalized programs, new faculty members are assigned to senior faculty members and written procedures are followed. Informal mentoring, which lacks written procedures, occurs when 2 individuals with similar interests develop a relationship over time.16 Although informal mentoring relationships may be more likely to last, the mutual selection process of informal mentoring is left to chance and takes time to develop. Formal mentoring offers the initial advantage of providing structure to the process and includes helping mentees learn the institution’s structure and framework. Later, mentees can seek out mentors who share their vocational and psychosocial interests.2 Formal mentoring programs and informal mentoring that occur between colleagues are not mutually exclusive.
The typical mentor is 15 to 20 years older than the mentee. Because of the intensity of the relationship, most mentor-mentee pairs are exclusive during the cultivation phase. Mentors and mentees are typically of the same sex. Although male faculty members usually form mentoring relationships with other male faculty members, female faculty members often report that they have difficulty forming mentoring relationships and frequently find that the most suitable mentor candidates are male faculty members. Although they can be successful, cross-gender mentor-mentee relationships are potentially problematic.17,18 Minorities, particularly African-American and Latino faculty members, also report challenges forming mentoring relationships.14 Formal mentoring programs help reduce the barriers to mentorship faced by women and monitories. Data suggesting 1 model over another are lacking. Sambunjak and colleagues, who performed a large systematic review of 39 studies to evaluate evidence about the prevalence of mentorship and its relationship to career development, found that the self-reported prevalence of mentorship among faculty members in academic and health institutions ranged from 16% to 95%.7 Mentoring was reported to have an important influence on personal development, career guidance, career choice, and research productivity. However, the study left many questions unanswered, including whether mentors should be assigned or self-selected and whether mentors and mentees should be of the same gender.
While there is widespread acceptance of the value of mentorship, relatively few studies have evaluated mentoring program outcomes. Mentorship can foster behavioral, attitudinal, health-related, relational, motivational, and career outcomes.14 In an American College of Clinical Pharmacy White Paper, Boyce and coauthors stated that mentoring should be an integral part of a comprehensive faculty development program and that evaluation of the mentoring program success should include both self-assessment by the mentee and peer-assessment by mentor and mentee of each other.19 This approach allows the relationship to grow and strengthen over time. Assessments should be shared with faculty administrators, such as department chairs and program coordinators, to reward faculty mentors and encourage ongoing personal development. Outcomes data regarding effectiveness in scholarship productivity, faculty morale, and success during the promotion and/or tenure process also should be collected.
At the completion of the annual cycle of the Massachusetts College of Pharmacy and Health Sciences School of Pharmacy-Boston faculty mentor program, participants attended a luncheon and workshop that involved sharing feedback, recognizing mentor service, and completing a self-assessment questionnaire.16 Since the start of the program, 93 mentees and 73 mentors have participated. Thirty-two mentees and 16 mentors took part in the pre- and post-survey, which indicated that participation in the faculty mentor program improved mentees’ self-perceived ability in conducting academia-related research, grant submission, manuscript preparation, and scholarly presentation.
While career outcomes are inherently embedded in academic mentorship programs, successful mentoring likely embodies many, if not all, of the other stated outcomes. Meta-analyses of mentoring programs suggest that programs do promote positive outcomes, although with relatively small effect size.20,21 A 2004 meta-analysis of mentoring programs within an organizational setting, excluding student mentoring, evaluated both objective and subjective career outcomes.21 Objective outcomes included salary growth and promotions, whereas subjective outcomes included career satisfaction, career commitment, expectation for advancement, and intention to remain with the current employer. In comparing objective career outcomes, mentored individuals were more likely to be promoted and to have salary growth compared with nonmentored individuals. Similarly, career satisfaction, belief in opportunities for career advancement, and career commitment were better correlated with individuals in mentoring programs. However, a significant correlation was not found between intent to remain with the current employer and presence of a mentoring program. Although the overall effect size was small, this study also found that the greatest effect of mentoring was in subjective rather than objective outcomes. A subsequent meta-analysis corroborated these results, finding a significant but small effect size regarding the correlation of mentorship with behavioral, attitudinal, health-related, relational, motivational, and career outcomes.20 Similarly, the largest effect size was seen with mentee attitudes (eg, career satisfaction, career expectations) and less effect was found with respect to career outcomes (eg, promotion, success, skill competence). While providing useful information, neither of these meta-analyses was specific to academic faculty mentorship and, thus, may not be an accurate representation of academic pharmacy outcomes.
Most studies evaluating mentorship programs have used questionnaires and survey instruments of faculty participants detailing their perceptions of the program. Faculty members who have participated as a mentee placed the highest value on mentors’ ability to assist in preparation for promotion, assist in developing an independent academic identity, be an active listener, set high performance standards, and address personal and professional issues.18 Other studies have additionally valued increased access to department information and resources, a greater feeling of support, and having a role model.22
Some studies have provided more objective evidence of successful mentorship programs. A study of faculty members from the University of California, San Diego’s School of Medicine documented a high rate of faculty retention (85%) and faculty members remaining in academia (93%), and a self-assessed increase (20% to 76%) in confidence in teaching, research, and leadership, based on pre- and post-program evaluations.23 Based on national data of faculty turnover in academic medicine, the authors estimated that the program prevented a loss of 4 faculty members over a 20-year period, resulting in a 49% return on investment for their faculty mentoring program. This estimate was derived from costs associated with the loss of faculty members, eg, faculty recruitment and start-up packages. From a research perspective, focused aspects, such as confidence in knowledge of and skill in writing grant proposals, increased significantly from approximately 25% to 60%-65%, based on pre- and post-program self-evaluations.24
Although the benefits of mentoring programs are many, some barriers have been identified. Straus and colleagues identified the amount of time spent by both the mentor and mentee to be the single most important barrier to mentorship.11 Additionally, lack of academic recognition for mentors and the perception that mentors’ work was not recognized in annual activity reviews or promotion criteria were noted. Other barriers noted by mentees included lack of financial incentive to mentorship, lack of appropriate skills to serve as a mentor, and “authoritative boss-employee relationship.”11 Institutions should attempt to overcome these barriers when designing and implementing mentorship programs.
PHARMACY FACULTY MENTORING
Prior to making recommendations on mentoring programming for colleges and schools of pharmacy, the American Association of Colleges of Pharmacy (AACP) Section of Pharmacy Practice Faculty Development Committee felt that the current state of mentoring programs should be assessed, so they conducted an electronic survey of all US colleges and schools of pharmacy. The AACP Pharmacy Practice Section Faculty Development Committee created the 13-item survey instrument, which was sent electronically to 129 faculty members identified as department chairs or division heads of pharmacy practice departments at US colleges or schools of pharmacy. Data were collected in spring 2011. The survey remained open for a 4-week period, during which time 1 reminder e-mail was sent to survey recipients.
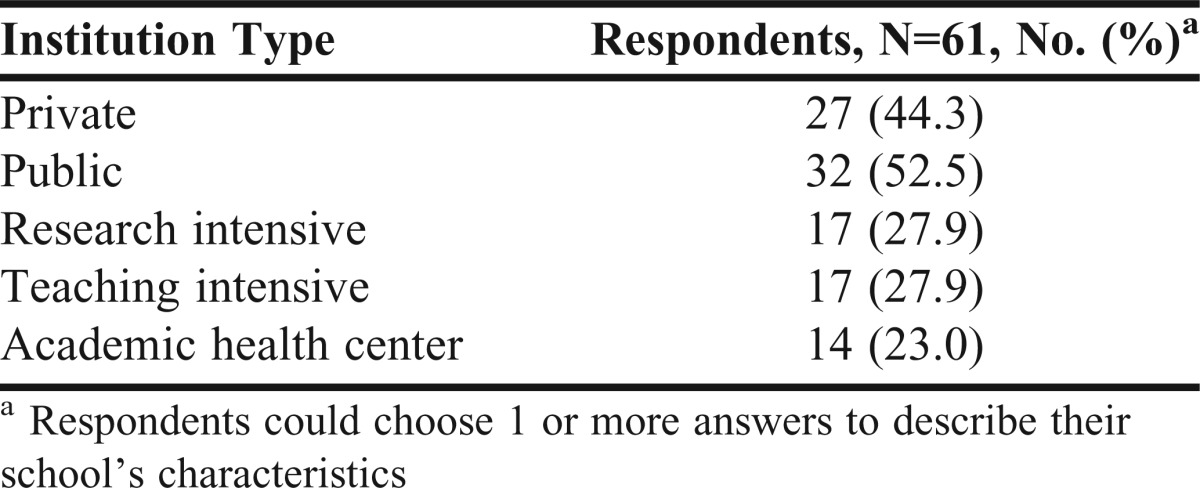
Respondents from 69 colleges and schools completed the survey instrument for a response rate of 53.4%. Four other questionnaires were submitted that were mostly blank and, therefore, unusable. Additionally, not all respondents answered every question posed. The majority of respondents (61) identified the institutions that housed their colleges or schools of pharmacy as public institutions (Table 2). Most respondents (53.6%) described their departments as consisting of 21 to 40 faculty members. The majority of faculty members in the department were on either a nontenure or clinical track. Tenure-track and adjunct faculty members comprised a smaller proportion of the department.
Table 2.
Characteristics of Pharmacy Colleges and Schools with Faculty Mentoring Programs
Ninety-one percent of the study respondents stated that their college or school of pharmacy offered a faculty mentoring program. Half of the respondents stated that the faculty mentoring program was a hybrid, consisting of both formal and informal elements. The majority (53.4%) of respondents stated that participating in the mentoring program was not mandatory. Open-response feedback from respondents suggested that the mentoring programs are geared to junior faculty members.
There was no predominant method used for pairing mentors with mentees. Approximately 44% percent of respondents stated that mentees were assigned to a mentor, while 28% stated that mentees were permitted to select their own mentors. The remaining 28% indicated a response of “other” and provided further feedback. In this open-ended feedback, many respondents indicated that faculty members were paired with a senior faculty member, based on characteristics such as similar career goals, areas of practice and expertise, and research interests. Respondents indicated that mentees who select their own mentors do so based on level of comfort with the mentor as well as similarities in career goals, areas of practice, and research interests. Some respondents reported that faculty members are assigned to multiple mentors. Approximately 52% of respondents stated that not all pharmacy practice mentees are paired with mentors within the department of pharmacy practice, ie, some may be paired with faculty members in other departments within the college or school of pharmacy.
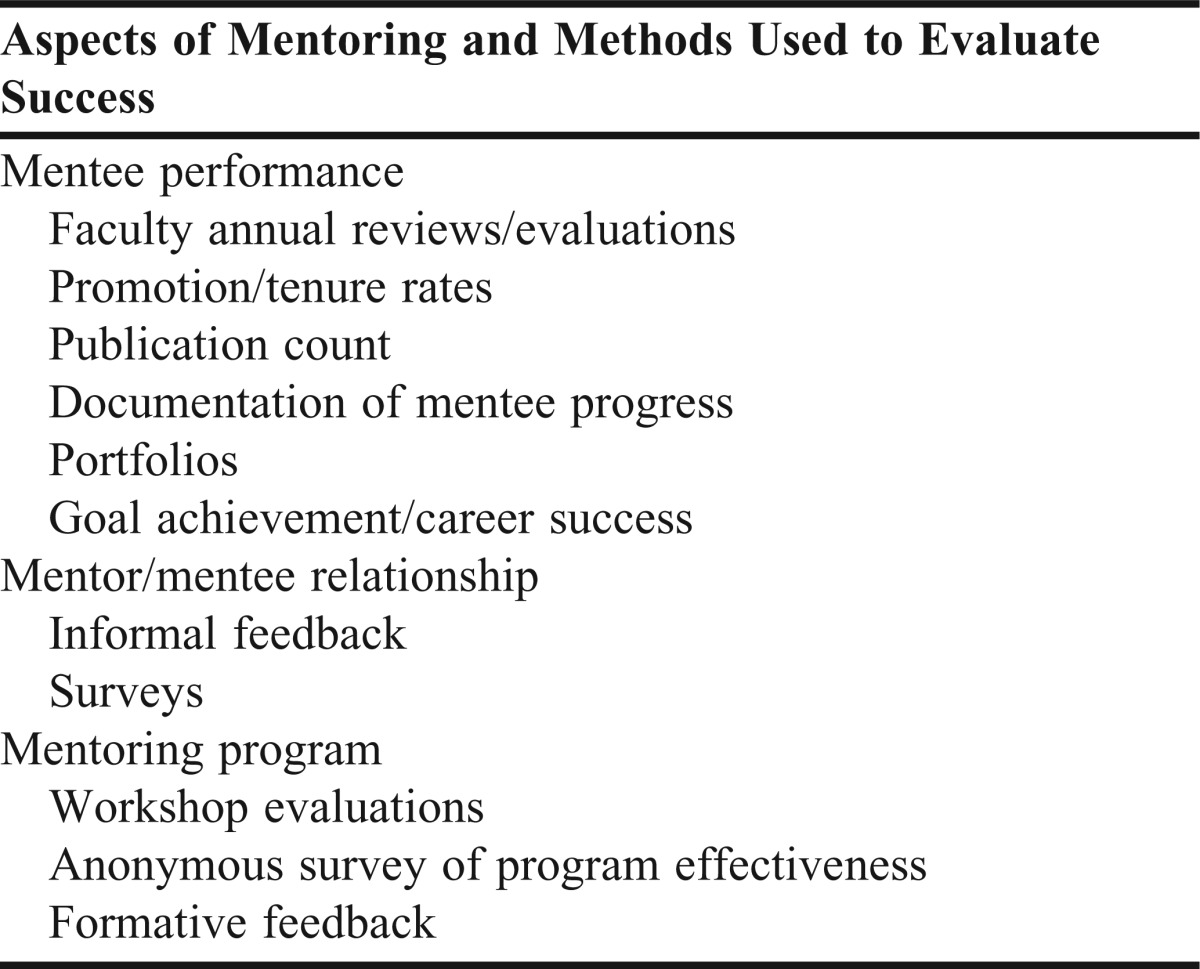
The topics reported as most commonly discussed between mentees and mentors included establishing research agendas, classroom teaching, and balancing responsibilities (Table 3). Other discussion topics, such as service responsibilities and collegiality, were also mentioned. A large proportion (77%) of respondents reported that topics discussed are decided between the mentee and mentor. Although the majority of respondents (71%) did not have a formal method in place to measure the success of the mentoring program, they did report multiple informal methods that have been implemented to do so. The reported ways in which the programs were evaluated fall into 3 categories; mentee performance, mentor/mentee relationship, and mentoring program (Table 4). These are based on open-ended feedback obtained from the survey question regarding measures of success.
Table 3.
Topics Discussed Between Mentees and Mentors
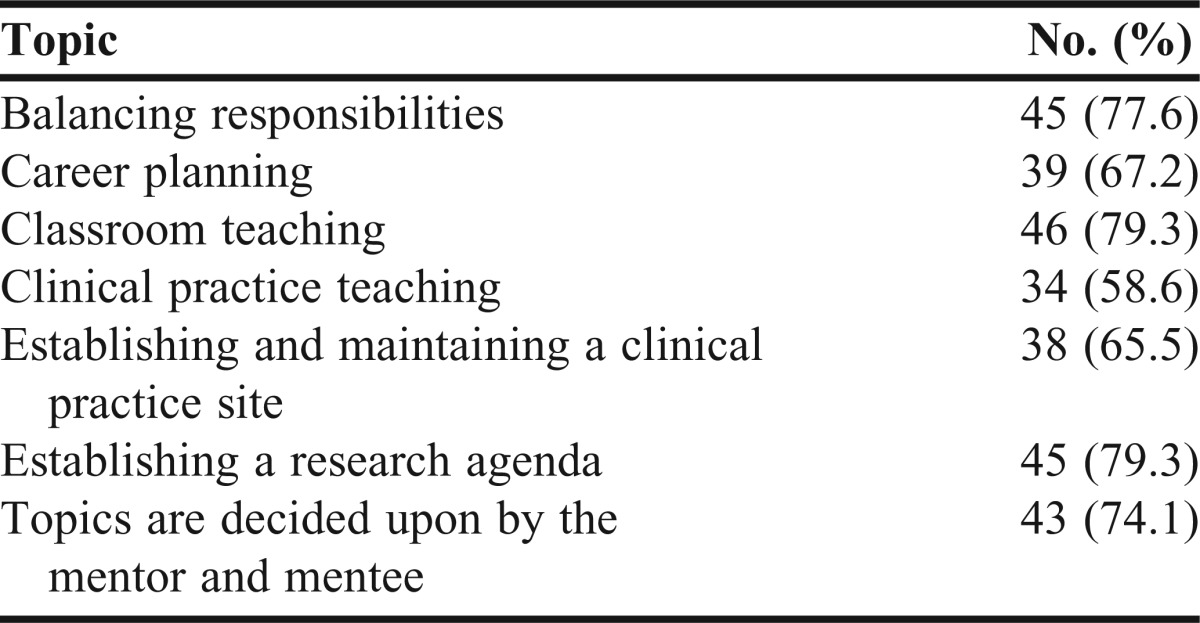
Table 4.
Methods Used to Measure Success of Various Aspects of Existing Mentoring Programs
ESSENTIAL ELEMENTS OF A MENTORING PROGRAM
While there are many aspects to consider in starting an effective mentoring program, 3 key areas should be addressed. Each institution considering a mentoring program should create 1 that is unique for the given institution, depending on factors such as the institution’s mission, resources, and size. Because the literature regarding pharmacy practice mentoring programs is lacking, these recommendations are based on general principles and practices from existing literature, including nonpharmacy literature.
Although the structure of a mentoring program can take on different formats for success, it should involve the pairing of junior and senior faculty members to share feedback on projects and advice on incorporation of scholarship, teaching, and service activities into academic responsibilities. This pairing could be assigned by a dean or department chair or initiated by the mentor or mentee. Some data suggest that self-selection is preferred but assigned mentors are an acceptable alternative. One possible solution would be for the department chair to allow the mentee to suggest a mentor, and if he or she had no preference, then the department chair could assign one.
During initial planning for a mentoring program, colleges and schools of pharmacy should adopt a definition of scholarship that aligns with their academic institution’s culture of scholarship. Clarifying promotion and tenure guidelines for both clinical and tenure-track faculty members is another important step. Potential matching of a mentor/mentee pair who are in the same track could be a good recommendation, as the mentor would be more likely to understand the demands the mentee will face as they progress toward a faculty appointment. The mentor should understand the institution’s promotion and tenure guidelines and use them to guide the mentee in a direction that will lead to efficient and effective work balance to enhance promotion and tenure.
When starting a mentoring program, it is important to help senior faculty members develop the skills they need to be effective mentors and to recognize their contributions. The characteristics of exemplary mentors should be reviewed and prioritized (Table 1). Some of these characteristics may be engrained into the mentor’s current practice, but encouragement and guidance for their development should be provided by the individual institution’s leadership team.
Recognition of a mentor’s contribution could occur as a service credit that would aid in the mentor’s promotion or tenure or as a monetary stipend for faculty development or further training to enhance the mentor’s skills. Recognition awards also could be developed to acknowledge an institution’s exemplary mentors. Evaluating the effectiveness of a mentoring program by measuring its outcomes is an important component of any mentoring program. There are many ways to assess and evaluate program outcomes. Mentor-mentee satisfaction survey instruments and other various indices can provide additional, qualitative measurements of program success.
CONCLUSION
With the growing number of new colleges and schools of pharmacy comes an increasing number of junior faculty members with limited experience. Mentoring programs designed to develop academicians are integral to helping new faculty members cope with the challenges of balancing personal, teaching, practice, research, and service responsibilities while developing skills. These programs can lead to increased productivity and job satisfaction for both junior and senior academicians. Although institutions may use different methods of evaluating the success of their program, the development of an effective mentoring program at any institution is a core component of enhancing its culture of teaching and scholarship, and ensuring the success of its academicians.
REFERENCES
- 1.Anderson E, Shannon A. Toward a conceptualization of mentoring. In: Kerry T, Mayes A, editors. Issues in Mentoring. New York: Routledge; 1995. pp. 25–34. [Google Scholar]
- 2.Fuller K, Maniscalco-Feichtl M, Droege M. The role of the mentor in retaining junior pharmacy faculty members. Am J Pharm Educ. 2008;72(2):Article 41. doi: 10.5688/aj720241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray M. Beyond the Myths and Magic of Mentoring: How to Facilitate an Effective Mentoring Process. San Francisco: Jossey-Bass; 2001. pp. 47–70. [Google Scholar]
- 4.Noe RA. An investigation of the determinants of successful assigned mentoring relationships. Pers Psychol. 1988;41(3):457–479. [Google Scholar]
- 5.Mullen EJ, Noe RA. The mentoring information exchange: when do mentors seek information from their protégés? J Org Behav. 1999;20(2):233–243. [Google Scholar]
- 6.Haines ST. The mentor-protégé relationship. Am J Pharm Educ. 2003;67(3):Article 82. [Google Scholar]
- 7.Sambunjak D, Straus S, Marusic A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med. 2010;25(1):72–78. doi: 10.1007/s11606-009-1165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson VA, Palepu A, Szalacha L, Caswell C, Carr PL, Inui T. Having the right chemistry: a qualitative study of mentoring in academic medicine. Acad Med. 2003;78(3):328–334. doi: 10.1097/00001888-200303000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Leslie K, Lingard L, Whyte S. Junior faculty experiences with informal mentoring. Med Teach. 2005;27(8):693–698. doi: 10.1080/01421590500271217. [DOI] [PubMed] [Google Scholar]
- 10.Williams LL, Levine JB, Malhotra S, Holtzheimer P. The good-enough mentoring relationship. Acad Psychiatry. 2004;28(2):111–115. doi: 10.1176/appi.ap.28.2.111. [DOI] [PubMed] [Google Scholar]
- 11.Straus SE, Chatur F, Taylor M. Issues in the mentor-mentee relationship in academic medicine: qualitative study. Acad Med. 2009;84(1):135–139. doi: 10.1097/ACM.0b013e31819301ab. [DOI] [PubMed] [Google Scholar]
- 12.Ramani S, Gruppen L, Kachur EK. Twelve tips for developing effective mentors. Med Teach. 2006;28(5):404–408. doi: 10.1080/01421590600825326. [DOI] [PubMed] [Google Scholar]
- 13.Morton-Cooper A, Palmer A. In: Mentoring in practice. Mentoring, Preceptorship, and Clinical Supervision. Morton-Cooper A, Palmer A, editors. Oxford: Blackwell Science; 2000. pp. 59–62. [Google Scholar]
- 14.Desselle SP, Peirce GL, Crabtree BL, et al. Pharmacy faculty workplace issues: findings from the 2009-2010 COD-COF Joint Task Force on Faculty Workforce Am J Pharm Educ. 2011754Article 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kram KE. Mentoring at Work: Developmental Relationships in Organizational Life. Glenview, IL: Scott Foresman; 1985. [Google Scholar]
- 16.Zeind CS, Zdanowicz M, MacDonald K, Parkhurst C, King C, Wizwer P. Developing a sustainable faculty mentoring program. Am J Pharm Educ. 2005;69(5):Article 100. [Google Scholar]
- 17.Garman KA, Wingard DL, Reznik V. Development of junior faculty's self-efficacy: outcomes of a National Center of Leadership in Academic Medicine. Acad Med. 2001;76(10 Suppl):S74–S76. doi: 10.1097/00001888-200110001-00025. [DOI] [PubMed] [Google Scholar]
- 18.Feldman MD, Arean PA, Marshall SJ, Lovett M, O’Sullivan P. Does Mentoring matter: results from a survey of faculty mentees at a large health sciences university. Med Educ Online. 2010;15:5063. doi: 10.3402/meo.v15i0.5063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyce EG, Burkiewicz JS, Haase MR, et al. Essential components of a faculty development program for pharmacy practice faculty. Pharmacotherapy. 2008;28(2):245–268. doi: 10.1592/phco.29.1.127. [DOI] [PubMed] [Google Scholar]
- 20.Eby LT, Allen TD, Evans SC, Ng T, DuBois D. Does mentoring matter? A multidisciplinary meta-analysis comparing mentored and non-mentored individuals. J Vocat Behav. 2008;72(2):254–267. doi: 10.1016/j.jvb.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Allen TD, Eby LT, Poteet ML, Lentz E, Lima L. Career benefits associated with mentoring for protégés: a meta-analysis. J Appl Psychol. 2004;89(1):127–136. doi: 10.1037/0021-9010.89.1.127. [DOI] [PubMed] [Google Scholar]
- 22.Tracy EE, Jagsi R, Starr R, Tarbell NJ. Outcomes of a pilot faculty mentoring program. Am J Obstet Gynecol. 2004;191(6):1846–1850. doi: 10.1016/j.ajog.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 23.Wingard DL, Garman KA, Reznik V. Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine. Acad Med. 2004;79(10 Suppl):S9–S11. doi: 10.1097/00001888-200410001-00003. [DOI] [PubMed] [Google Scholar]
- 24.Thorndyke LE, Gusic ME, Milner RJ. Functional mentoring: a practical approach with multilevel outcomes. J Contin Educ Health Prof. 2008;28(3):157–164. doi: 10.1002/chp.178. [DOI] [PubMed] [Google Scholar]


