Abstract
Objective. To assess health care providers’ perceptions of student pharmacists involved as members of a general medicine team.
Methods. A brief, anonymous, online survey instrument was distributed to 134 health care providers at 4 major medical centers in Massachusetts who interacted with Northeastern University student pharmacists during inpatient general medicine advanced pharmacy practice experiences beginning in March 2011. The survey instrument assessed health care provider perception of student pharmacists’ involvement, preparedness, clinical skills, and therapeutic recommendations.
Results. Of the 79 providers who responded, 96.2% reported that student pharmacists were prepared for medical rounds and 87.3% reported that student pharmacists were active participants in patient care. Also, 94.9% and 98.7% of providers indicated that student pharmacist recommendations were appropriate and accurate, respectively. The majority (61.8%) of providers believed that student pharmacist involvement on internal medicine teams was beneficial.
Conclusions. Provider perceptions regarding student pharmacist participation on general medicine practice experiences were mostly positive.
Keywords: experiential education, perception, pharmacy, student pharmacist
INTRODUCTION
To improve patient outcomes and to be actively involved in patient-centered care under the direct supervision of a pharmacist preceptor, it is common for student pharmacists to assess patient medication profiles and recommend medication therapy alterations, perform medication reconciliation, educate patients through discharge medication counseling, and provide clinical presentations to medical teams. Additionally, student pharmacists may provide recommendations involving intravenous to oral medication interchange, provide therapeutic drug monitoring, and act as a clinical drug information resource. The contribution of the student pharmacist on daily rounds has been described quantitatively in the literature using various endpoints such as the total number of interventions performed, percentage of recommendations accepted, type of interventions, time spent, and cost avoidance/savings.1 The participation of pharmacy personnel, including students, during medical rounds may add additional value by facilitating relationships with the medical, nursing, and other allied health care staff, while addressing unmet needs and increasing efficiency within the pharmacy department.2
Doctor of pharmacy students at Northeastern University are required to complete at least 1 of their advanced pharmacy practice experiences (APPEs) within a hospital inpatient general medicine setting. The general medicine APPE is a 6-week assignment during which students are exposed to a variety of disease states including cardiac, endocrine, hematologic, infectious, and respiratory disorders. Student pharmacists completing this APPE often serve as the primary source of pharmacy contact for a medical team comprised of physicians, nurses, medical students, and other health care professionals.
On most APPEs, the student pharmacists are formally assessed on their knowledge, skills, and abilities in the general medicine setting by their assigned pharmacy preceptor(s). Physicians and other health care providers do not routinely contribute to the student pharmacists’ evaluation process, despite the large proportion of time student pharmacists spend interacting with these providers within this setting. Without their support and input in the evaluation process, preceptors may be concerned that a disconnect between the perceptions of the student pharmacists and preceptor and those of the health care provider(s) exist.
A review of available, published, literature did not identify any reports of health care provider perception regarding the impact of student pharmacist participation on an inpatient general medicine team. Given the paucity of published literature on this subject and the authors’ desire to quantify provider perception of APPE students, this study was undertaken. The study objective was to qualitatively assess health care providers’ perceptions about the extent of student pharmacists’ contribution to and added value of student pharmacists on the general medicine team.
METHODS
At the time of this study, Northeastern University’s School of Pharmacy employed faculty members who served as primary preceptors for students on their inpatient general medicine APPE at several institutions, including 4 medical centers in and around Boston, Massachusetts: Beth Israel Deaconess Medical Center; Boston Medical Center; Brigham and Women’s Hospital; and Lahey Clinic Medical Center. Each of these institutions is a tertiary care, academic medical center, although the number of patient beds and patient demographics differ slightly among the facilities.
APPE students at each site were responsible for pre-rounding and rounding on patients admitted to their respective inpatient general medicine teams from Monday through Friday each week. Additional activities included attending medical and pharmacy conferences, presenting and discussing patient cases with preceptor(s) and other students, and participating in topic discussions and projects, including journal clubs and patient case presentations. In addition to these activities, APPE students could participate in medication reconciliation and discharge counseling programs, but these 2 activities were not standardized across each of the 4 institutions surveyed.
A brief, anonymous, online survey instrument was developed using SurveyMonkey software (SurveyMonkey.com, Palo Alto, CA). Six consecutive 6-week APPE blocks encompassing 14 APPE offerings by 4 faculty members to 52 students were selected and the health care professionals who interacted with the student pharmacists at each of the 4 sites between March and December of 2011 were identified. The APPE preceptor at each institution sent an e-mail containing an invitation to participate in the survey and a link to the survey instrument to the health care providers at their institution via a secured e-mail service. Participation was voluntary and no remuneration was provided.
Prior to distribution, the survey instrument was reviewed by 3 health care providers at 1 of the hospital sites. Feedback was solicited and updates were made before widespread distribution to all health care providers. Respondents were asked to provide personal demographic data such as: degree(s) earned, current position, and history of any previous interaction with student pharmacists. Using a 5-point Likert scale ranging from “strongly agree” to “unable to comment,” providers were asked to classify the level of preparation and participation of student pharmacists related to daily medical rounding activities. Furthermore, providers were asked to rate their level of comfort with the appropriateness and accuracy of therapeutic recommendations made by student pharmacists using a 4-point Likert scale (comfortable, somewhat comfortable, somewhat uncomfortable, uncomfortable). Finally, providers were asked to comment on how likely they were to make changes to patient care plans based on the student pharmacist’s recommendations; the overall perceived benefit of the student pharmacist to the medical team; and the students pharmacist’s impact on patient care. This project was reviewed by the Northeastern University Institutional Review Board and given exemption status as this study did not directly involve an intervention with human subjects.
RESULTS
Seventy nine of the 134 providers who were contacted completed the survey instrument (59% response rate). All respondents possessed either a doctor of medicine (MD) or osteopathic medicine (DO) degree. The majority of respondents were medical interns and residents (68%), with the remaining serving as attending physicians (32%). The reported breakdown of the medical residents by year of training was as follows: 32% were in their first postgraduate year, 22% in their second postgraduate year, and 15% in their third postgraduate year. All of the responding physicians reported having interacted with student pharmacists during their time on the inpatient medical team at each respective institution prior to the administration of this survey instrument, with 22% reporting having worked with 7 or more students, 19% with 5 to 6 students, 34% with 3 to 4 students, and 25% with 1 or 2 students.
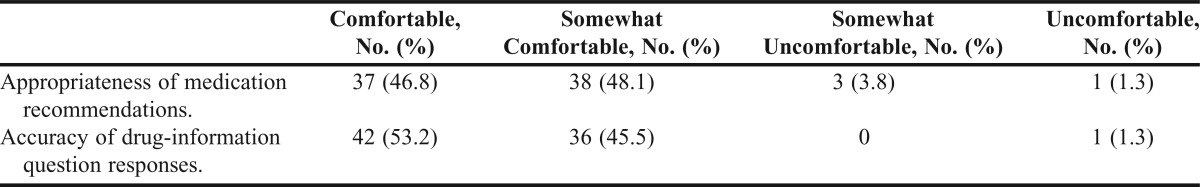
Nearly all providers (≥95%) agreed or strongly agreed that students: were prepared for rounds; possessed necessary patient-specific information; and responded to drug information questions in a reasonable timeframe (Table 1). Eighty-seven percent of providers agreed or strongly agreed that student pharmacists were actively involved in patient care. Furthermore, 95% of respondents were either comfortable (46.8%) or somewhat comfortable (48.1%) with the appropriateness of medication recommendations, and 98% were either comfortable (53.2%) or somewhat comfortable (45.5%) with the accuracy of drug information responses (Table 2).
Table 1.
Provider Perception of Student Pharmacists’ Preparation for and Participation in Daily Rounds in an Inpatient General Medicine Setting
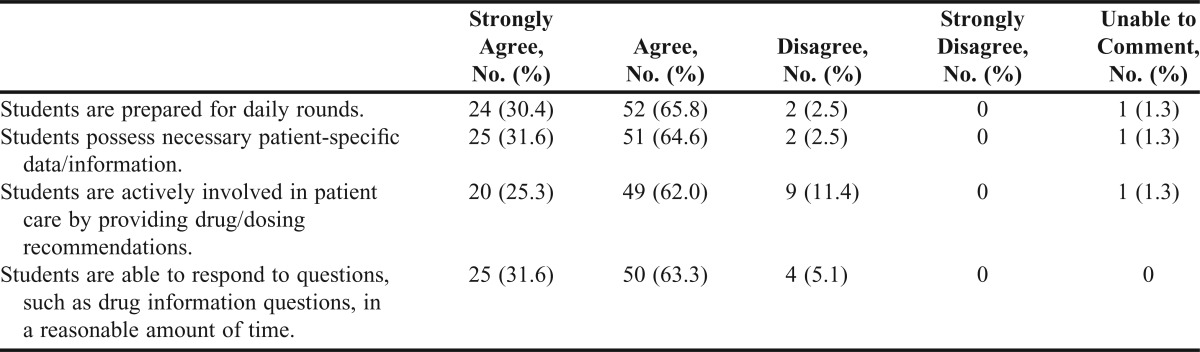
Table 2.
Provider Perception of Appropriateness and Accuracy of Student Pharmacists’ Recommendations and Responses as Part of a Healthcare Team in an Inpatient General Medicine Setting
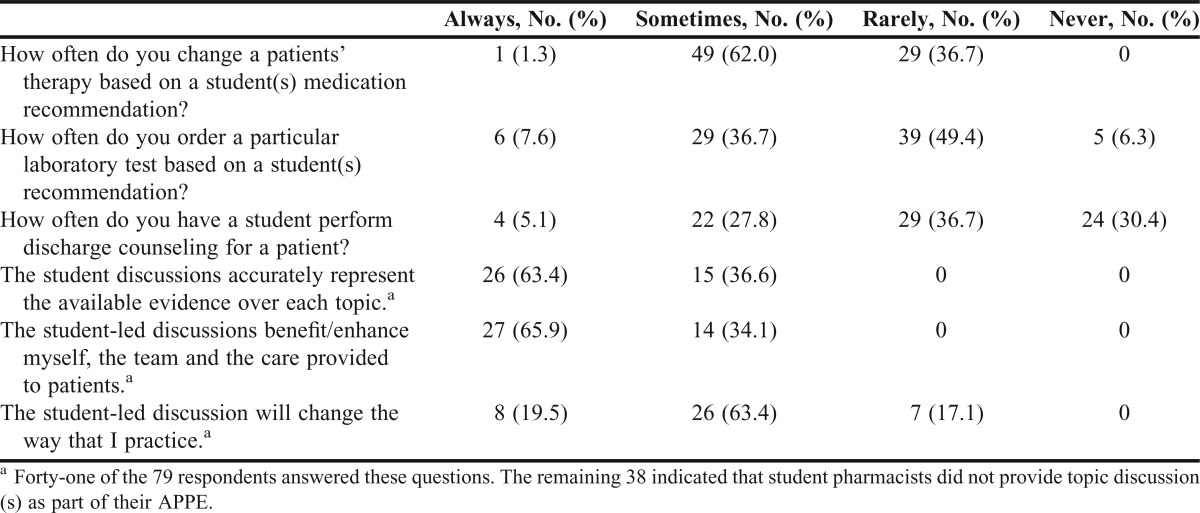
Providers also agreed with, and implemented, student medication therapy recommendations, with 62% responding that they “frequently” modify patients’ therapy based on student pharmacist suggestions. Additionally, 37% of the providers reported that they “frequently” ordered laboratory tests based on student pharmacists’ recommendations; although the exact nature and type of laboratory testing was not ascertained as part of this survey. Physicians reported not consistently asking student pharmacists to perform discharge counseling, with 30% reporting never having asked a student to complete this task, and 37% reported asking a student to complete this task “infrequently.” Furthermore, 52% of the responding providers indicated that the student pharmacists led at least 1 drug therapy education presentation with the medical team. Sixty-three percent of those providers who indicated that students led clinical discussions with the medical team stated that the student-led discussions “always” accurately represented the available evidence, and 65.9% of these respondents said the discussions “always” had a positive impact on the medical team and patient care. While 19.5% of the responding providers stated that they “always” changed their practice based on student recommendations, 63.4% stated that they “sometimes” and 17.1% stated that they “rarely” changed their practice (Table 3). However, the specific types of practice changes the providers made based on student pharmacist recommendations were not captured as part of this survey. Sixty-two percent of the responding providers perceived student pharmacists participation within the medical team to be “very beneficial” to the health care provided at their institution, and another 29% ranked it as “somewhat beneficial.”
Table 3.
Provider Use of Student Pharmacists’ Information and Abilities Within Daily Medical Rounds in an Inpatient General Medicine Setting
DISCUSSION
The value of the pharmacist’s role in improving patient outcomes in several types of practice settings has been well documented.3-5 However, there is a paucity of literature describing prescriber perceptions of the benefit of a pharmacist or student pharmacist in similar practice environments.6 Of those published reports that have attempted to capture the role and contribution of pharmacists or student pharmacists, most have been conducted outside of the United States, potentially limiting the transferability of their results to the US health care system; were not conducted in the internal medicine setting; and/or had small sample sizes.7-12 Despite these limitations, the results of this study are similar to those reported in the literature for practicing pharmacists. As can be seen from this study, and others, health care providers respond positively regarding the impact pharmacists have on patient care and their value to the medical team. Additionally, providers may not be aware of the role and skills of pharmacists or student pharmacists in the management of patient-care--related activities, as was seen within our study related to discharge medication counseling.9
As providers have become more comfortable with the expanding role and responsibility of pharmacists in the medication use process, their perceptions and subsequent expectations have evolved.7 Positive perceptions of pharmacy practitioners by medical and nursing staff members have been previously evaluated and published in the medical literature, but no evaluation of student pharmacists previously existed.11 Also, important pharmacy functions such as providing patient counseling are more likely to occur if the pharmacist is working directly in the patient care area and not at a remote location. Furthermore, general medicine practitioners in Australia expect and value communication from their pharmacy colleagues related to information about the patient as part of providing complete medical care.12 These findings highlight the need for student pharmacists and pharmacists to communicate directly with prescribers during patient rounds, to be immersed in the patient care setting, and to maintain positive relationships and accessibility.
Provider perception of student pharmacists is likely to improve over time as providers gain a better understanding of student pharmacists’ abilities and scope of practice, and develop a positive working relationship with them. However, this improvement may be hampered by the rapid turnover associated with student APPEs. In contrast, when a dedicated pharmacist is permanently assigned to a healthcare team, long-term relationships can be built with other providers.
Overall, a positive perception of the contributions of student pharmacists was observed in this study. While the reported prescriber level of comfort with the appropriateness of student recommendations was positive, the data revealed a wide range of comfort among institutions (18.2% to 61.5%). Notably, the providers from the institution with the lowest reported level of comfort regarding student recommendations were also more likely than providers at any other institution surveyed to change therapy based on student recommendations. This may have been a result of the scope and nature of the recommendations provided.
The variations in perceptions among providers from different medical centers may be explained in a number of ways. Differences in the level of training of respondents, as well as the number of student pharmacists with whom providers had interacted likely impacted the responses to some of the items in the questionnaire. Previous provider experience with student pharmacists varied greatly, with approximately 25% of respondents having previously worked with 1 or 2 student pharmacists, and approximately 20% having worked with 7 or more student pharmacists. The variation between providers and their previous experience with student pharmacists may have led to confusion regarding the role of the student pharmacist within the medical team and may have impacted the results of our survey as some respondents stated they were unsure if it was appropriate to ask questions of the students or to assign them specific tasks. These findings may have negatively impacted the prescribers’ willingness to routinely accept student pharmacists’ therapy and laboratory testing recommendations, or have the students perform discharge counseling and provide in-service topic discussions. Furthermore, we did not accurately quantify the number of times providers accepted student recommendations, nor did we capture the extent to which providers may have altered a patients therapy, ordered laboratory tests, or any of the specific questions addressed in Table 3, which obfuscates the provider’s use of student pharmacists in these roles. Additionally, the extent of these interactions varied between institutions, and in some cases, the interactions may have been as brief as 1 week. This limited duration of interaction may have affected the results of the survey. This may particularly be true as providers who did not respond to the survey may have done so because they felt unable to comment on the quality of student pharmacists’ contribution to the team.
Another aspect not captured as part of this study was the variability in individual student’s effort, initiative, enthusiasm, and confidence, as well as the timeliness and accuracy of their responses to provider questions. Each of these factors may have had a significant impact on the providers’ overall perceptions of the student pharmacist, and as such, may have increased, or decreased, the likelihood that a provider would act upon any recommendations or suggestions made by the student pharmacist.
Furthermore, every institution has a culture that is based on its vision and mission, and this extends to interprofessional medical teams. Even slight variations in institutional culture among institutions may have impacted our findings. For example, responsibilities such as medication reconciliation and discharge counseling may routinely be performed by nonpharmacy health care professions. Lastly, the overall response rate for this study was just under 60%, and consisted solely of physicians. These factors present additional limitations as they mean we were not able to capture all health providers’ perceptions regarding student pharmacists, and we were not able to demonstrate any differences in perception based on health care provider type (eg, physician vs nurse). The missing responses may have increased or decreased the perceived benefits of the student pharmacists within this setting, as well as provided differences in perception based on health care provider role.
These findings provide colleges and schools of pharmacy with information that can be readily applied in their classroom and experiential curriculum. Specifically, colleges and schools of pharmacy can focus educational efforts for their students around the provision of high-quality medication reconciliation, prospective medication review, discharge counseling, and response to drug information requests from providers and patients. These efforts can be implemented throughout the curriculum within many different courses including therapeutics-based coursework, practice-laboratory work, and/or within focused elective courses. Additionally, these data can be used to engage and educate healthcare providers about the range of patient-care contributions that can be made by student pharmacists. Colleges and schools of pharmacy should reach out directly to the healthcare providers with whom their students interact in all patient-care experiences, and begin, or continue, a dialogue regarding the expectations and opportunities for student pharmacists. Without adequate education and promotion of the range of services that student pharmacists can provide within the health care team, their services may continue to be underused, to the ultimate detriment of the patients for whom they care. With this in mind, the preceptors at each of the aforementioned sites are actively engaging health care providers, to a higher degree than was previously done, to promote the broad-reaching service that student pharmacists and pharmacists can provide as part of an interdisciplinary health care team. Our findings suggest that if a more active role for student pharmacists is desired within the health care team, acknowledgement, support, and “buy-in” from other health care professionals is imperative. These factors have broad implications in the training of student pharmacists in preparation for medical team rounding experiences on APPEs. The interprofessional medical team is more likely to use student pharmacists when providers have a thorough understanding of their capabilities.
CONCLUSIONS
This study adds to the understanding of the perceptions and the nature of interactions between physicians and student pharmacists in an inpatient general medicine team setting. The majority of the findings of this study confirmed what is found in the literature regarding physicians’ positive perception pharmacists also holds true for student pharmacists. Especially the belief that student pharmacists make a positive contribution to the healthcare team in a number of areas. However, it was found that physicians did not rely on student pharmacists to perform a variety of medication-related services, including discharge counseling. This study highlights the overall positive perception that healthcare providers have of student pharmacists working within an inpatient medical setting, but also the continued need to establish a formal role for student pharmacists in patient care.
REFERENCES
- 1.Mersfelder TL, Bouthillier MJ. Value of the student pharmacist to experiential practice sites: a review of the literature. Ann Pharmacother. 2012;46(4):541–548. doi: 10.1345/aph.1Q544. [DOI] [PubMed] [Google Scholar]
- 2.Ray MD, Helms RA. Assessing the value of services provided by pharmacy faculty on a contractual basis. Am J Health-Syst Pharm. 2010;67(17):1463–1466. doi: 10.2146/ajhp100089. [DOI] [PubMed] [Google Scholar]
- 3.Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med. 2006;166(9):955–964. doi: 10.1001/archinte.166.9.955. [DOI] [PubMed] [Google Scholar]
- 4.Chisholm-Burns MA, Lee JK, Spivey CA, et al. US pharmacists effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- 5.Chisholm-Burns MA, Graff Zivin JS, Lee JK, et al. Economic effects of pharmacists on health outcomes in the United States: a systematic review. Am J Health-Syst Pharm. 2010;67(19):1624–1634. doi: 10.2146/ajhp100077. [DOI] [PubMed] [Google Scholar]
- 6.Makowsky MJ, Schndel TJ, Rosenthal M, Campbell K, Tsuyuki RT, Madill HM. Collaboration between pharmacists, physicians and nurse practitioners: a qualitative investigation of working relationships in the inpatient medical setting. J Interprof Care. 2009;23(2):169–184. doi: 10.1080/13561820802602552. [DOI] [PubMed] [Google Scholar]
- 7.Farrell B, Pottie K, Woodend K, et al. Shifts in expectations: evaluating physicians’ perceptions as pharmacists become integrated into family practice. J Interprof Care. 2010;24(1):80–89. doi: 10.3109/13561820903011968. [DOI] [PubMed] [Google Scholar]
- 8.Blake EW, Blair MM, Couchenour RL. Perceptions of pharmacists as providers of immunizations for adult patients. Pharmacotherapy. 2003;23(2):248–254. doi: 10.1592/phco.23.2.248.32083. [DOI] [PubMed] [Google Scholar]
- 9.Côté L, Légaré F, Richer M. Development of the pharmacist-physician relationship: perceptions of program directors and trainees in the faculties of pharmacy and medicine in Quebec, Canada. Am J Pharm Educ. 2001;67(2):Article 43. [Google Scholar]
- 10.Lalonde L, Hudon E, Goudreau J, et al. Physician-pharmacist collaborative care in dyslipidemia management: the perception of clinicians and patients. Res Soc Admin Pharm. 2011;7(3):233–245. doi: 10.1016/j.sapharm.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Fairbanks RJ, Hildebrand JM, Kolstee KE, Schneider SM, Shah MN. Medical and nursing staff highly value clinical pharmacists in the emergency department. Emerg Med J. 2007;24(10):716–719. doi: 10.1136/emj.2006.044313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dey RM, de Vries JW, Bosnic-Anticevicha S. Collaboration in chronic care: unpacking the relationship of pharmacists and general medical practitioners in primary care. Int J Pharm Pract. 2011;19(1):21–29. doi: 10.1111/j.2042-7174.2010.00070.x. [DOI] [PubMed] [Google Scholar]


