Abstract
Objective. To implement an introductory pharmacy practice experience (IPPE) involving discharge counseling on postpartum pertussis immunization recommendations and evaluate its impact on student learning and patient immunization rates.
Design. Seventeen pharmacy students provided verbal and written information based on Centers for Disease Control and Prevention (CDC) recommendations regarding pertussis immunization for mothers and caregivers of newborns.
Assessment. Educational and clinical outcomes were evaluated using student documentation and pharmacy records. Students completed 615 IPPE hours and provided 1,263 consultations. Students reported that 52% of mothers requested immunization, 27% were undecided, 11% had previously been immunized, and 10% declined. Following counseling, immunization rates, as a percentage of total births, significantly increased by 18.5%. Learning objectives of enhanced counseling and documentation skills were achieved.
Conclusions. IPPE students provided patient counseling in an institutional setting that contributed to healthcare team efforts to increase pertussis immunization rates in mothers of newborns. This IPPE may serve as a potential model for additional student involvement in discharge counseling.
Keywords: pertussis, immunization, discharge counseling, introductory pharmacy practice experience (IPPE)
INTRODUCTION
In 2007, the Accreditation Council for Pharmacy Education increased the requirements for introductory pharmacy practice experiences (IPPE) for doctor of pharmacy (PharmD) programs.1 The 2011 updated version of the accreditation standards provided increased direction regarding the structure of IPPEs. The minimum number of required IPPE hours was specified as not less than 300. Further, the majority of students’ time (minimum of 150 hours) had to be balanced between community pharmacy and institutional health-system settings. As colleges and schools of pharmacy have implemented these standards, concerns related to capacity and learning objectives have been noted.2-4
As colleges and schools of pharmacy continue to refine their IPPE programs within the limited capacity of their partnering organizations, benefit of the IPPE to the partnering organization must be evaluated along with educational outcomes.5,6 This paper describes the implementation of an IPPE in an institutional setting and evaluates its impact on the goals of the partnering healthcare organization as well as the educational goals for student learning.
In September 2009, an IPPE for second-year pharmacy students enrolled in a 4-year PharmD program was established wherein students provided discharge counseling regarding Centers for Disease Control and Prevention (CDC) recommendations for postpartum pertussis immunization. At the time, the CDC's Advisory Committee on Immunization Practices (ACIP) recommended that pregnant women who had not been previously immunized with the tetanus toxoid, diphtheria toxoid, and acellular pertussis (Tdap) vaccine receive it in the immediate postpartum period before hospital discharge. The recommendation also stated that Tdap immunization could be received at an interval as short as 2 years after the most recent tetanus and diphtheria (Td) immunization.7 (These recommendations have since changed, as noted in the Discussion).
This IPPE was designed in response to an area hospital’s infection control committee’s discussion on potential strategies to employ in response to increased rates of pertussis infection in the community. A college of pharmacy faculty member serving on this committee suggested the possibility of using IPPE students to provide discharge counseling on pertussis immunization to newborns’ mothers and other close contacts on the hospital’s postpartum unit. The committee endorsed this strategy and developed recommendations for student training. The committee recognized that although nursing staff members already included pertussis immunization information as part of the unit’s standardized discharge counseling protocol, the breadth of topics included in the nurses’ discharge counseling protocol and the limited time nurses had to deliver this information did not allow for emphasis of this particular immunization. This study was designed to analyze the effectiveness of this IPPE through 3 primary objectives: (1) evaluate achievement of student learning objectives for the IPPE; (2) document student-perceived immunization decisions of mothers who received consultations from students; and (3) measure changes in pertussis immunization rates on this hospital unit.
DESIGN
Students assigned to the IPPE were trained at the beginning of each semester to perform this targeted intervention. The 3-hour instructional portion of the training included a live presentation on CDC recommendations related to Tdap immunization presented by an infectious disease specialist who served on the hospital’s infection control committee. Instructions on hospital procedures and documentation processes were provided by the unit’s nurse manager. Following this training component, students completed 4 to 6 hours of training with a peer mentor who had successfully completed this IPPE. Schedules were overlapped so that the student completing the IPPE could mentor the incoming student for at least 2 days.
After training, students provided mothers on the hospital's postpartum unit verbal and written information about the benefits and risks of Tdap immunization, based on CDC recommendations. Written materials were provided by the manufacturer of the vaccine used by the hospital. These materials were approved by the required committees of the hospital.
All mothers on the postpartum unit were eligible for postpartum counseling related to Tdap immunization, according to the unit’s standard discharge counseling protocol. The Tdap consultation was provided by either a student or nursing staff member, depending on the availability of students in relation to the patient’s anticipated discharge. Neither the nursing staff nor students provided Tdap counseling to patients if the infant would not be moving to the mother’s home (eg, in cases of adoption, infant death, etc) or if the chart contained documentation that the mother had already received the Tdap immunization as an adult. Only nursing staff members provided counseling to patients younger than 18 years of age.
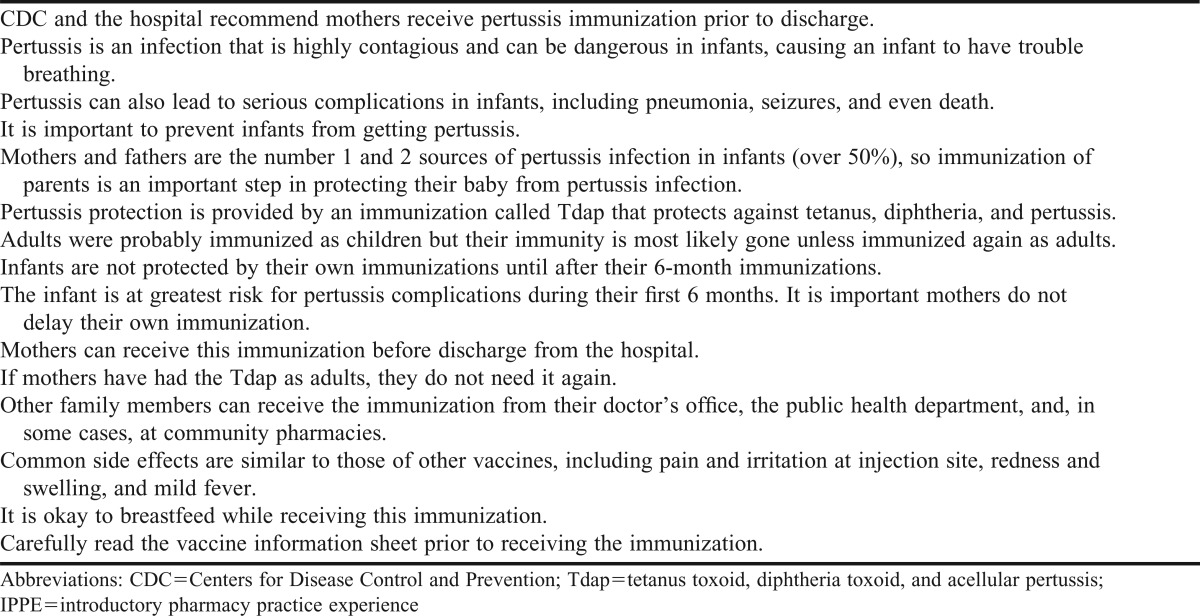
On each day of the IPPE, students received a list of all patients on the postpartum unit. If a given patient was eligible for counseling, a student determined if discharge was approaching. If discharge was not likely in the next 24 hours, counseling was deferred to either the nursing staff or a student providing counseling on a subsequent day. If discharge was likely in the next 24 hours, the student approached the mother and asked her permission to provide important information on immunizations. Once verbal permission was received, counseling was provided. If the mother was occupied (eg, sleeping, had guests, etc), counseling was deferred to either the nursing staff or a student providing counseling on a subsequent day. Appendix 1 outlines the counseling points generally included in a consultation. Students answered questions from the mother if they had received training to provide the requested answers. All other questions were referred to the preceptor or nursing staff.
After each consultation, the student determined his/her perception of the mother’s decision whether to receive the immunization prior to discharge. Students classified the mothers’ decisions in 1 of the following categories: patient requests immunization; patient is considering immunization; immunization is not indicated; or patient refuses immunization. These categories were listed in a standardized progress note that the student completed and added to the patient chart along with any supporting documentation.
For patients who were considering but not committed to immunization, students noted any concerns or questions in the progress note so that other healthcare providers could further address issues. Students were instructed not to pressure mothers to request immunization but to professionally provide information and lay a foundation of knowledge so other healthcare providers could continue to encourage immunization with mothers who were resistant. Mothers who were unsure of their current immunization status but interested in immunization were placed in this category. If the patient refused immunization, the student documented any reasons stated by the patient in the progress note so that other healthcare providers could address these specific concerns.
During some consultations, students determined that immunization was not indicated for the particular patient. There were 2 main reasons for this categorization. In some cases, the patient had been previously immunized as an adult, but this information had not been documented in the chart. These findings were subsequently documented in the progress note and the medical chart. The second reason for noting that immunization was not indicated was if the mother had received a Td immunization in the last 2 years, as CDC recommendations at the time of the consultation were for such patients to delay Tdap immunization. (CDC recommendations for Tdap immunization were updated in 2011, as explained in the Discussion section).
At the end of each day’s IPPE hours, students reported immunization requests to the nurse leader who activated standard orders. Students provided consultations for 2 hours each day of the workweek. Student hours were scheduled to avoid conflict with other discharge counseling, lactation consultations, and various educational programs provided on the postpartum unit. The nursing team leader in charge of immunizations served as the primary preceptor for the students. A pharmacy faculty member was also available for consultation if the students had any additional questions during this experience.
Students also provided recommendations for immunization to other close contacts of the infant (eg, fathers, other parental figures, grandparents, siblings), per CDC guidelines. As the hospital offered immunizations only to admitted patients, close contacts who required immunization were referred to other sources, such as local public health departments, pharmacist immunizers, and medical clinics.
EVALUATION AND ASSESSMENT
Achievement of learning objectives was measured by student self-assessment of improvement in counseling and documentation skills over the course of the IPPE, based on students’ documentation of the experience in the college’s experiential education database. The learning objectives for this IPPE were to interview patients and provide information; collect subjective information and use charts and/or electronic records to collect objective information; and understand and implement the process used to document interventions and the method used to request changes in drug therapy.
Clinical outcomes were measured by student perceptions of immunization decisions made by the mothers receiving counseling and by changes in immunization dispensing rates on the postpartum unit of the hospital relative to the number of births at the hospital during the same period. Students used the same categories as those used in the progress notes to document their perceptions of the mothers’ decisions to immunize following the consultation. Each day, the aggregate number of recommendations for each category was entered in the experiential education documentation system. Immunization rate was defined as the number of doses of Tdap vaccine that were dispensed to patients on the postpartum unit divided by the total number of births during the defined time period. Total birth data are collected by the hospital for reporting to public agencies.
Evaluation of achievement of learning objectives was conducted over the first 16 months (September 2009-December 2010) of the IPPE. An analysis of number of students, IPPE hours, and consultations is presented in Table 1. Students were asked to evaluate the IPPE by ranking their agreement with evaluation statements on a scale of 1 (strongly disagree) to 5 (strongly agree). Select responses contributing to these learning objectives are listed in Table 2. Students were also asked to evaluate the overall experience as excellent, good, fair, or poor.
Table 1.
Patient Consultations in an IPPE to Increase the Rate of Postpartum Tdap Immunization
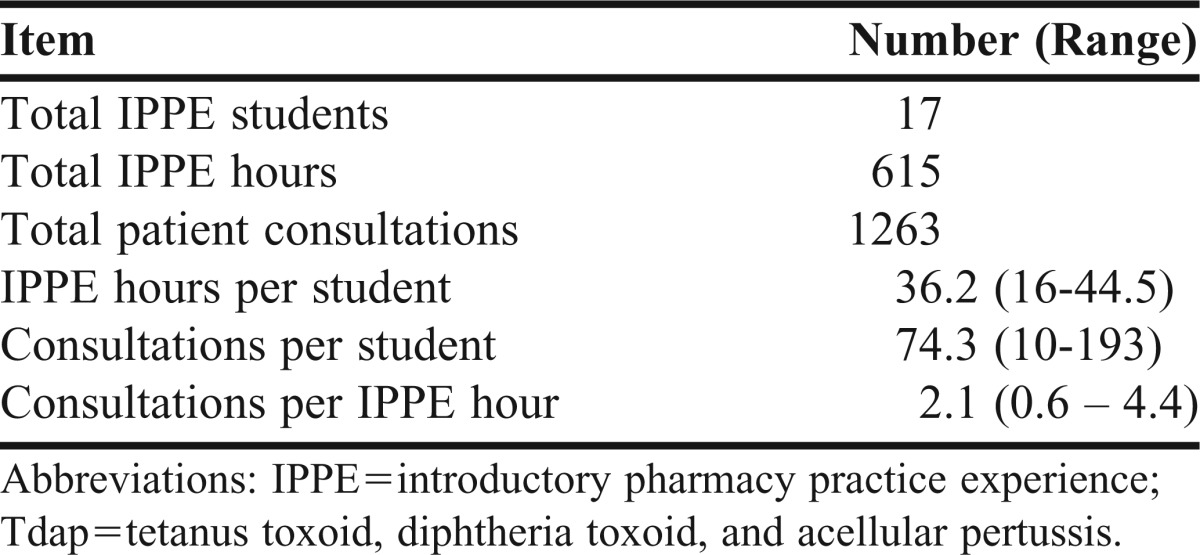
Table 2.
Student Self-Assessment Following Completion of an IPPE to Increase the Rate of Postpartum Tdap Immunization (n = 17)
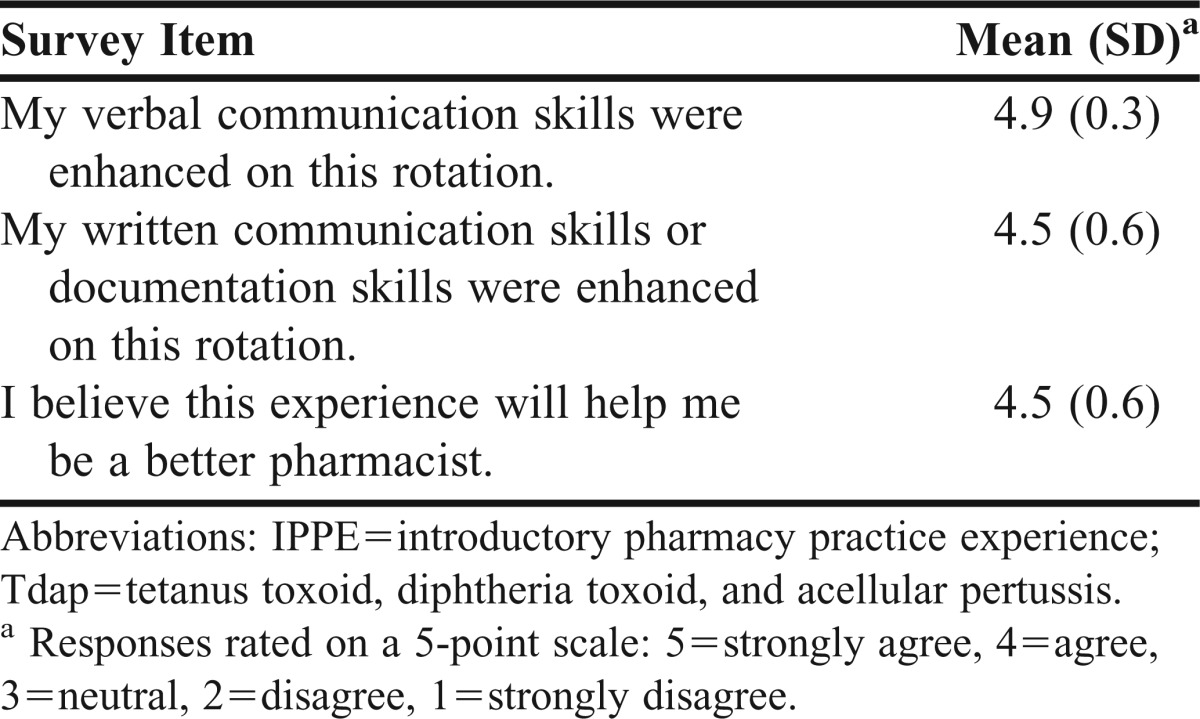
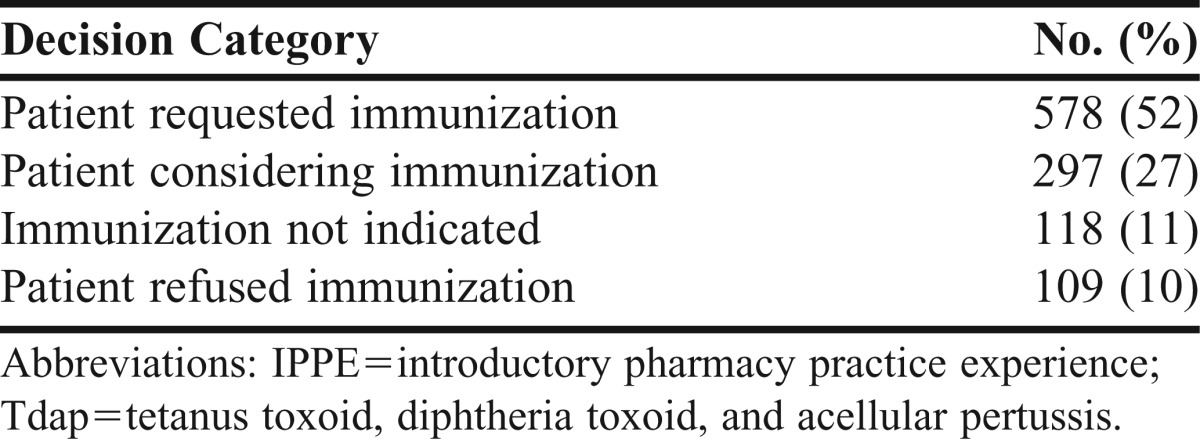
All students rated the experience as excellent (n = 11) or good (n = 6), except for 1 student who did not complete the IPPE. Students were also given the opportunity to provide free text comments as part of the IPPE evaluation. Common themes in these comments related to improved counseling and documentation skills. Documentation of student-perceived immunization decisions of the mothers receiving consultations began following the first 2 IPPE students. Table 3 documents student-perceived immunization decisions for 1,102 consultations performed by 15 students. Immunization rate data compared the time period of December 2008 through August 2009, which immediately preceded IPPE implementation, to the equivalent time period of December 2009 through August 2010 during the first year of the IPPE.
Table 3.
Student-Perceived Immunization Decisions During an IPPE to Increase the Rate of Postpartum Tdap Immunization (n=15)
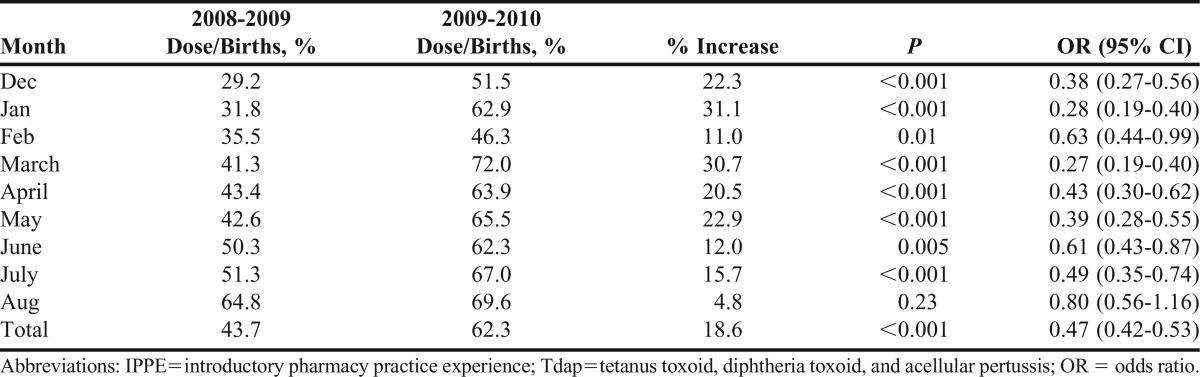
During the preintervention time period, there were 2,667 births, and 1,166 Tdap immunizations were dispensed to mothers on the postpartum unit, resulting in an overall immunization rate of 43.7%. During the intervention period, there were 2,411 births, and 1,503 immunizations were dispensed, for an overall immunization rate of 62.3%. The 18.6% increase in immunization rate was highly significant (p< 0.001; Table 4). The increase in immunization rate was significant for all months except August. A Spearman correlation test, conducted to determine how the change correlated over time, demonstrated a significant trend (r=0.6).
Table 4.
Analysis of Immunization Rates Prior to and Following an IPPE to Increase Rate of Postpartum Tdap Immunization
DISCUSSION
This IPPE to improve pertussis immunization rates in mothers of newborns met learning and clinical objectives. As colleges and schools of pharmacy continue to refine their IPPE programs, this IPPE could serve as a model for successful implementation. Several factors contributed to the success of this IPPE: site support, including student training; team ownership of the intervention; purpose of the intervention; and targeting of the intervention.
The IPPE students contributed to the healthcare team’s efforts to increase the Tdap immunization rate on the postpartum unit of this hospital. The infection control committee authorized the students’ role on this unit in response to an identified need, and several of the committee members assisted in training the students. Endorsement by this committee enhanced the credibility of the students on the unit, and the support and cooperation of nursing supervisors and staff members were critical to the success of this IPPE. By contributing to the team’s effort, which resulted in the improved immunization rate, student activity was viewed by the IPPE site as an asset.
Likewise, students were viewed as a part of but not the sole solution to the identified need. Students did not assume full responsibility for this intervention, and we do not assert that the students’ work alone increased the immunization rate. Given the students’ limited time on the unit, nurses still provided counseling in their absence. If a student reported that a patient had not agreed to the recommended immunization, other healthcare professionals continued to encourage immunization. However, students became part of the healthcare team serving a distinct purpose of increasing the Tdap immunization rate.
The targeting of this intervention allowed students to focus on the process of providing patient education rather than on information alone. As IPPE students have significant classroom coursework remaining, skills that were emphasized included communicating effectively with patients and obtaining necessary information from the medical chart. Although the information provided was fairly standard for most patients, as noted in the student evaluation comments, the delivery of the information had to be personalized to meet individual patient needs. Also, a targeted intervention such as this 1 allows chart review skills to be gradually introduced to students without becoming the predominant activity of the IPPE.
This IPPE has the potential to serve as a model for additional student involvement in discharge counseling. Although we evaluated an intervention related to immunization, the model is transferable to other topics based on the needs of partnering institutions. This analysis shows that students can provide targeted patient care in this setting at a relatively early stage of their education. This type of IPPE would be particularly helpful in creating experiences to obtain required institutional health system IPPE hours earlier in the degree program.
In January 2011, approximately 4 months after the data analysis for this study was completed, the CDC's ACIP updated its recommendations on the Tdap vaccine for the general public. These recommendations included providing Tdap immunization regardless of the interval since the most recent Td vaccine administration and providing Tdap immunization to adults 65 years or older who anticipate close contact with an infant less than 12 months of age.8 In June 2011, ACIP further updated the recommendations that were in place at the time of this writing to recommend that pregnant women not previously immunized be administered the Tdap vaccine during the third or late-second trimester of pregnancy (after 20 weeks’ gestation).9
CONCLUSION
In this IPPE involving discharge counseling regarding CDC recommendations for postpartum pertussis immunization, educational and clinical outcomes were evaluated, demonstrating positive results. Evaluations supported that students increased their skills in counseling and documentation. Student participation on the healthcare team contributed to a significant increase in the pertussis immunization rate among mothers of newborns. This IPPE may serve as a model for a discharge counseling IPPE.
ACKNOWLEDGEMENTS
The authors acknowledge and thank Stephen Elliott, DO, PhD, for his role in student training; Kim Wente, Peggy Black, Shellee Burkhart, and other nursing staff involved in precepting our students; Michelle Kraber for her assistance in obtaining pharmacy dispensing data; Mark Kennedy of Sanofi Pasteur for supplying patient education materials and training support; and Amy Munemoto, PharmD, for her assistance with data collection while a student pharmacist at Drake University.
Appendix 1.
Tdap Immunization Counseling Points Provided by IPPE Students
REFERENCES
- 1.Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Accreditation Council for Pharmacy Education Web site. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed July 23, 2012. [Google Scholar]
- 2.Capacity of hospitals to partner with academia to meet experiential education requirements for pharmacy students. Am J Pharm Educ. 2008;72(5):Article 117. doi: 10.5688/aj7205117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith KM, Phelps PK, Mazur JE, May JR. Relationships between colleges of pharmacy and academic medical centers. Am J Health-Syst Pharm. 2008;65(18):1750–1754. doi: 10.2146/ajhp080145. [DOI] [PubMed] [Google Scholar]
- 4.Traynor K. Experiential education requirements squeeze schools, rotation sites. Am J Health-Syst Pharm. 2004;61(15):1537–1538. doi: 10.1093/ajhp/61.15.1537. [DOI] [PubMed] [Google Scholar]
- 5.Flynn AA, MacKinnon GE., III Assessing capacity of hospitals to partner with academic programs for experiential education. Am J Pharm Educ. 2008;72(5):Article 116. doi: 10.5688/aj7205116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chase P. Rethinking experiential education (or does anyone want a pharmacy student?) Am J Pharm Educ. 2007;72(2):Article 27. doi: 10.5688/aj710227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prevention of pertussis, tetanus, and diphtheria among pregnant and postpartum women and their infants: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2008;57(4):1–47. 51. [PubMed] [Google Scholar]
- 8.Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine. Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60(01):13–15. [PubMed] [Google Scholar]
- 9.Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months. Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60(41):1424–1426. [PubMed] [Google Scholar]


