Abstract
Over the past decade, the body of research linking energy balance to the incidence, development, progression and treatment of cancer has grown substantially. No prior NIH portfolio analyses have focused on energy balance within one institute. This portfolio analysis describes the growth of National Cancer Institute (NCI) grant research on energy balance–related conditions and behaviors from 2004 to 2010 following the release of an NCI research priority statement in 2003 on energy balance and cancer-related research. Energy-balance grants from fiscal years (FY) 2004 to 2010 were identified using multiple search terms and analyzed between calendar years 2008 and 2010. Study characteristics related to cancer site, design, population and energy-balance area (physical activity, diet, and weight) were abstracted.
From FY2004 to FY2010, the NCI awarded 269 energy balance–relevant grants totaling $518 million. In FY2010, 4.2% of NCI’s total research project grants budget was allocated to energy-balance research, compared to 2.1% in FY2004. The NCI more than doubled support for investigator-initiated research project grants (R01), and increased support for cooperative agreement (U01, U54) and exploratory research (R21) grants. In the portfolio, research examining energy-balance areas in combination accounted for 41.6%, and observational and interventional studies were equally represented (38.3% and 37.2%, respectively). Breast cancer was the most commonly studied cancer. Inclusion of minorities rose, and funding specific to cancer survivors more than doubled. From FY2004 to FY2010, NCI’s investment in energy-balance and related health behavior research showed growth in funding and diversity of mechanisms, topics and disciplines—growth that reflects new directions in this field.
Introduction
During the past decade, research linking energy balance to the initiation, development, progression and treatment of cancer has grown substantially. Energy balance–related conditions and health behaviors, including overweight, obesity, physical inactivity, and poor diet have been linked to increased incidence of many cancers.1–4 Several estimates of population-attributable risk suggest excess body fat may account for 3%–9% of all cancers and one fifth to one third of postmenopausal breast, colon, endometrial, kidney, and digestive cancers.5–8 Associations between energy balance and related health behaviors and poor quality of life, recurrence and mortality have also been identified in cancer survivors.9–13 Such evidence is particularly important given that approximately two thirds of U.S. adults are overweight or obese,14 and physical inactivity,15 sedentary behavior,16 and poor diet17 are common.
As the principal federal funding agency of biomedical research in the U.S., the NIH, housed in the DHHS, supports more than 90% of obesity research in the country through its 27 institutes and centers.18 In 2003, the National Cancer Institute (NCI) formally identified energy balance as a strategic research area.19 The priorities in the plan were informed by the NCI Energy Balance Working Group, which convened staff across programs and divisions with an expertise in research on diet/nutrition, physical activity, and weight across the range of research areas represented in NCI-funded grants, including behavioral science, epidemiology, genomics, surveillance, and applied research. In 2005, the NIH created an agency-wide task force to accelerate progress in obesity research: the NIH Obesity Research Task Force (ORTF), which published the NIH obesity research strategic plan21 that was updated in 2011.20,22
Together these plans and reports illustrated the growing consensus around the importance of energy balance and chronic disease, including cancer, and the need for coordinated research. In its 2003 research priority statement, NCI defined energy balance as:
“the integrated effects of diet, physical activity, and genetics on growth and body weight and cancer related research that encompasses research over the life course, across the cancer continuum and across stages and phases of cancer from the level of the cell to that of policy.”19 Energy balance was described in this strategic document as four primary goals: discovery, surveillance, measurement, and intervention delivery. This definition and these elements of energy balance served as the basis of the criteria used in this portfolio analysis.
The discovery goal sought to foster research that integrated weight, physical activity, and diet, along with genetic and environmental factors, and the cancer development process through investment in basic, clinical and transdisciplinary research. The second goal, surveillance, focused on monitoring trends and determinants related to diet, physical activity, weight and related factors through collaboration with surveillance efforts across federal agencies and development of new survey instruments. The third, measurement, aimed to expand validation research, the development of electronic monitoring and web-based instruments and the identification of novel biomarkers. The last, intervention delivery, encouraged research related to planning, implementing and evaluating dietary and physical activity interventions. NCI’s energy-balance initiative addressed the need for research to broaden from a focus on cellular- and individual-level research to research on how the individual responds to the diverse social, environmental and physical environments that may either hinder or facilitate the adoption of recommended health behaviors.
Since then, substantial investments have been made in advancing energy-balance and cancer research in scope and complexity to enhance understanding of the underlying biological mechanisms as well as the influence of social–environmental and policy forces at the population level. In 2007, the World Cancer Research Fund advocated for research designs that emphasized dietary and lifestyle patterns and habits over individual nutrients or nutrient classes, indicating a shift from traditional perspectives on nutrition and cancer.1
In addition, new research has emerged on the benefits of physical activity in reducing recurrence and mortality and improving quality of life in cancer survivors.23,24 The 2011 NIH ORTF’s revised plan for obesity research calls for transdisciplinary approaches that integrate research on biologic mechanisms regulating energy balance with focus on disseminating, implementing and evaluating multilevel energy-balance interventions.22 NCI strategic planning and initiatives are consistent with many components of this new plan.
Given the evolution of the field and the growing prevalence of energy balance–related conditions and health behaviors, a review of the extramural grant portfolio for NCI, one of the leading funders of research on the topic, is timely. Earlier portfolio analyses of obesity research across the NIH have been performed, and they reflect the specific aspects of obesity treatment and intervention approaches as related to chronic disease prevention, but do not reflect specific energy balance– and cancer-related challenges that have recently emerged. This NCI portfolio analysis describes the growth of investigator-initiated research supported by NCI on energy balance–related conditions and behaviors over the past 7 years.
Portfolio Analysis Methods
To identify and describe relevant grants, public-use and internal NIH and NCI extramural grant databases were searched for awards related to energy balance funded between FY2004 and FY2010. The publically available NIH Research Portfolio Online Reporting Tool: Expenditures and Results (RePORTER) was used to implement the search strategy, identify relevant grants and abstract key characteristics; additional attributes related to study design were identified through internal NCI grant records. The NCI component of the NIH obesity research portfolio was not used for this analysis as it is focused on obesity and not the broader field of energy balance– and cancer-related research.
Search Strategy and Inclusion Criteria
A text search strategy was used to identify NCI grants in this research area. The NCI’s 2003 definition of energy balance (quoted above) was used to guide the selection of search terms, which were reviewed by NCI subject matter experts. Abstracts and titles of grant applications were queried for multiple combinations of the following terms: energy balance, physical activity, fitness, exercise, obesity, body mass, energetics, diet, weight gain, loss and control, sex hormones, IGF factors, inflammation, oxidative stress, adipokines, behavioral interventions, policy, economics, genetics, surveillance, assessment, built environment, and animal models. The search included all components of energy balance, as described in the NCI definition. Grants examining a specific component of energy balance (i.e., diet, physical activity, or weight) were included and reported individually, as were studies examining energy balance in an integrated manner.
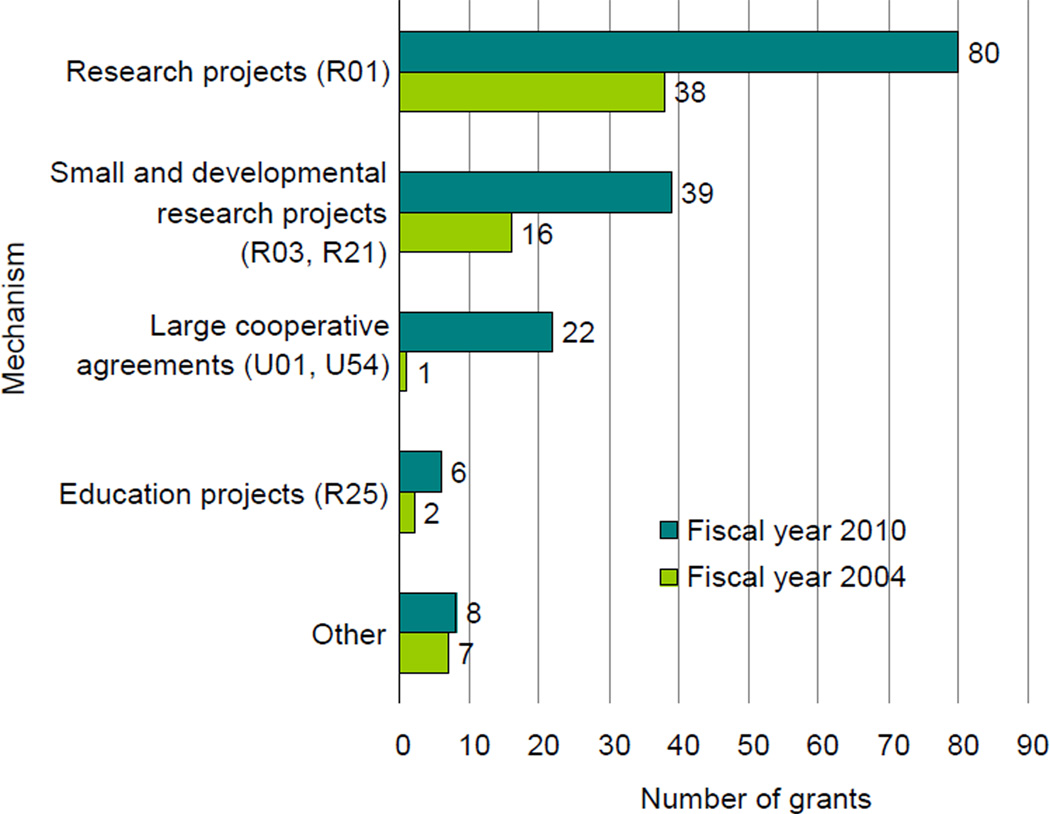
The search was limited to grants for which the NCI was the primary funder and those supported through research project, cooperative agreement, developmental, and small business mechanisms of varying dollar awards. The specific types of awards are listed in Figure 1. Excluded grants included those related to training, conferences, cancer centers, and grants focused on dietary supplements and micronutrients without any mention of energy balance in the application abstract.
Figure 1.
Number of energy-balance grants at the NCI by funding mechanism, FY2004 and FY2010
Note: Grants that accounted for less than 3% of the portfolio are not included in this figure.
FY, fiscal year; NCI, National Cancer Institute
Grants were included on the basis of their relevance to at least one of the four energy-balance goals in the NCI’s 2005 budget: discovery, surveillance, measurement, and intervention delivery. All study types were assessed, including basic and animal model, observational and descriptive, intervention, measurement and surveillance, and dissemination studies. Grants with titles that did not relate in any way to one of the four goals were excluded. The titles and abstracts for grants identified through the search strategy were reviewed to determine eligibility for inclusion. Discrepancies regarding coding by goal area were resolved through discussion.
Coding and Analysis
In addition to basic funding and administrative details, study characteristics related to cancer site, design, and study population were abstracted. Study location in the U.S. or abroad was not abstracted. The grants were categorized by topics (i.e., physical activity, diet, and weight), which were broadly defined as the primary measure of energy balance addressed in the grant application. Each topic spans multiple levels of research, including basic science, genetics, cellular mechanisms and animal models, epidemiologic and observational research, surveillance, measurement/validation, and intervention development and delivery. In abstracting information regarding study population, studies were categorized by their percentage share of minority participants, as described in the grant application (5%–24%, 25%–49%, 50%–75%, 76%–100%). The data were analyzed between 2008 and 2010.
Portfolio Analysis Results
Between FY2004 and 2010, the NCI awarded 269 research grants totaling approximately $518 million related to energy-balance conditions, mechanisms, markers and health behaviors, of a total of approximately $15 billion spent on research grants during that period. Over the 7 years, the NCI’s energy-balance grant-based research, including investigator-initiated and directed-funding research, doubled in terms of awards and funding. In FY2004, the NCI funded 5467 grants, of which 64 were energy-balance specific (1.2%); in FY2010, that number rose to 155 (3.1%), while the total number of grants declined to 5079.
The relative amount of funding also doubled, from 2.1% of the total research project grants budget in FY2004 (approximately $45.6 million of $2.1 billion) to 4.2% in FY2010 (approximately $90.8 million of $2.2 billion). A doubling occurred in the number of grants and amount of funding for investigator-initiated research project grants (R01), and increases occurred in cooperative agreement (U01, U54) and smaller exploratory research (R21) awards (Figure 1). R01 grants accounted for a smaller percentage of the overall energy-balance portfolio in FY2010 than in FY2004 in terms of number of grants (a change of −7.8%), whereas R21 and U54/U01 grants accounted for a larger percentage (changes of +8.0% and +12.6%, respectively). Grants responding to energy balance–specific program announcements and requests for applications accounted for just above one quarter (27.9%) of the portfolio.
Topic Areas, Research Themes, and Cancer Sites
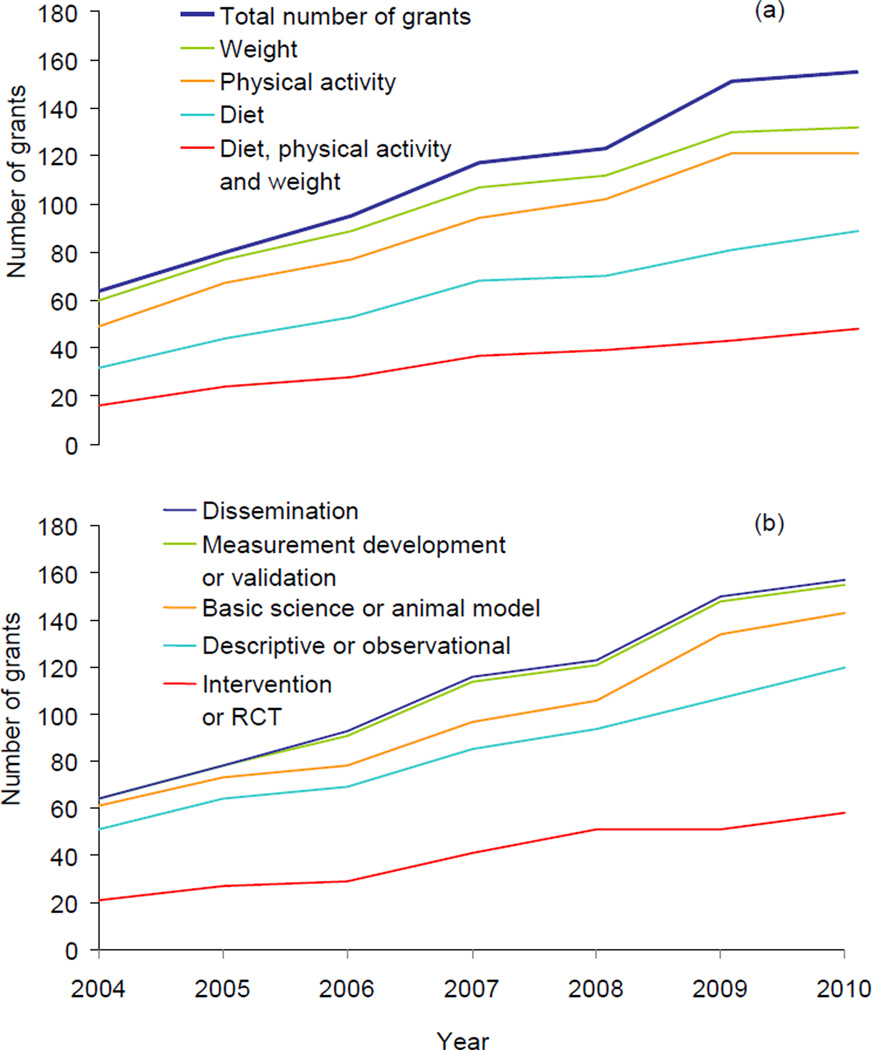
In terms of funding, research examining diet, physical activity, and weight together accounted for the largest proportion (41.6%) of the portfolio; diet alone accounted for about one third (35.4%), and physical activity alone accounted for about one sixth (16.2%). Table 1 provides a broad overview of the themes and some selected examples of topics addressed in the global areas of diet, physical activity, and weight by the four priority areas of the 2005 NCI budget. Research on diet and physical activity grew by approximately two thirds in terms of funding and +156.3% and +88.2%, respectively, in number of grants funded (Figure 2a).
Table 1.
Research themes and examples of selected topics in grants by NCI energy-balance goal area
| NCI Energy-Balance Goals | % of Grant Portfolio |
|---|---|
| Goal 1: Discover how body weight, physical activity, and diet, along with genetic and environmental factors, interact over a lifetime to influence the cancer process. | 37.8 |
| EXAMPLES OF TOPICS | |
| Animal model/basic science | |
| Molecular-nutrient interactions; fiber, gut microflora and epigenetic events; refined fructose; insulin and IGF-1 pathways; inflammation and obesity; Tsc-Mtor pathway in energy metabolism; metabolic syndrome and fatty acid synthesis; exercise mediated protection against brain metastases | |
| Descriptive/observational | |
| Dietary patterns and diet quality; foods ads and PSAs on obesity; genetic and endocrine pathways in obesity; IGF and IL-6 dysregulation; physical activity and smoking; effects of caffeine, exercise, and lipectomy; obesity and H. pylori; maternal obesity and intrauterine gene expression | |
| Intervention/RCTs | |
| Effects of exercise on melatonin and sleep; self-determination theory and lifestyle behaviors; body size and physical activity; adolescent diet and hormones; postprandial glycemic response by dietary glycemic load; effects of smart community growth on obesity prevention | |
| Goal 2: Monitor trends in and determinants of diet, weight, and physical activity and their cancer-related consequences across diverse populations by expanding nationwide research and health surveillance infrastructure. | 5.8 |
| Examples of topics (all are descriptive/observational) | |
| Neighborhood food availability, consumer economics and sentinel foods; trends in economic position and diet; diet, activity, obesity and built environment; multilevel exploration of obesity risk; weight gain in cancer survivors; lifecourse energy balance and cancer risk | |
| Goal 3: Develop improved measurement of body mass and composition, physical activity and fitness, and diet and bioactive food components through self-report measures and advances in technology for objective reference measures. | 11.6 |
| Examples of topics | |
| Survey to assess diet and activity environments in the home; validation of web-based dietary assessment tools; real-time recording of diet and physical activity; tool to develop food availability in the home; tool for geospatial analysis of physical activity; validation of preschool and high school diet recall | |
| Goal 4: Improve cancer-related health outcomes, especially in high-risk populations, by accelerating research in energy balance–related behaviors and developing interventions. | 44.8 |
| Examples of topics (most are intervention/RCT) | |
| Reducing cancer recurrence with weight loss; family eats, cancer prevention; diet composition and weight control; Mediterranean diet; supermarkets and diet behaviors; exercise for bone health in cancer survivors; physical activity and lymphedema; active video games and physical activity; worksite wellness for the web; school policy and youth obesity prevention; resistance training and smoking cessation | |
Note: Percentage of portfolio corresponds to the number of grants. The specific cancers addressed are not listed under topic areas.
NCI, National Cancer Institute
Figure 2.
Trends in the number of energy-balance research grants at the NCI by: (a) study topic area; and (b) design, both for FY2004–FY2010
Note: The solid line labeled “total number of grants” indicates all energy-balance research grants funded by NCI over the time period. Topics were broadly defined and categorized as the primary measure of energy balance addressed in the grant application. Each topic spans multiple levels of research, including basic science, genetics, cellular mechanisms and animal models, epidemiologic and observational research, surveillance, measurement/validation, and intervention development and delivery. Grants that examined energy balance more broadly or outside the context of diet, physical activity, or weight are not included in this figure.
FY, fiscal year; NCI, National Cancer Institute
Over the 7 years, the NCI nearly doubled investment in discovery, or research on how body weight, physical activity, and diet, along with genetic and environmental factors, interact over a lifetime to influence the cancer process (approximately $48 million in FY2010 versus $27 million in FY2004, a change of + 172.0% in number of grants. The NCI more than doubled its investment in accelerating and developing interventions related to energy-balance behaviors (approximately $24 million in FY2010 versus $8 million in FY2004, a change of +123.1% in terms of the number of grants). These two broad themes of the 2005 NCI budget accounted for more than three quarters (79.3%) of the NCI’s energy-balance grant funding.
In the area of discovery, the largest proportion of the funding (79.5%) supported large epidemiologic studies of cancer risk and prognosis. Funding for energy balance–related basic science research increased in the later years of FY2009 and FY2010 to about $7 million for each of those 2 years. Although support for developing and validating measures related to energy balance also increased substantially (from four grants in FY2004 to 13 in FY2010), it accounted for a relatively modest proportion of the overall portfolio (7.0%) in terms of funding. Whereas investment in extramural surveillance remained at a sustained level, such efforts are complemented by contracts and intra-agency agreements to enhance related surveillance and research.
Of grants specific to one type of cancer, the most common focus was breast cancer (39.5%), followed by colorectal/gastric (26.6%); prostate (11.0%); hematologic, (12.8%); and gynecologic (4.6%) cancers. Although support for breast cancer rose and remained high throughout the FY2004–FY2010 period, the most notable changes were in colorectal/gastric and prostate cancers (+20.8% and +9.4% of total grants specific to one type of cancer, respectively), particularly during the latter years of this period.
Study Design and Population
Interventions and RCTs accounted for 38.3% of all energy-balance grants, followed closely by descriptive and observational studies at 37.2%. Interventions and measurement development studies experienced the most substantial growth with respect to the number of awards funded, followed closely by basic science and observational studies (Figure 2b). In the basic sciences, grants were divided among cell cultures (n=11); animal models (n=20); and humans (n=11). Animal model research was limited to mouse and rat models.
The large majority of participants in studies with human subjects were adults. Funding for studies focusing on children or mixed-age populations remained substantially lower throughout the 7-year period. Research inclusive of minorities rose throughout the FY2004–FY2010 period; each category of minority representation rose substantially (5%–24%, 25%–49%, 50%–75%, 76%–100%). The amount of support for studies with 5%–24% minority participants more than quadrupled, and those with 25%–49% more than doubled. Funding for studies specific to cancer survivors more than doubled between FY2004 and FY2010 (+125.0 %).
Discussion
This portfolio analysis provides insight into NCI’s growing investment in research on energy balance–related health conditions and behaviors and highlights important changes in the research portfolio. Between FY2004 and FY2009, NCI and its NIH partners issued a number of funding opportunities relevant to energy balance, addressing issues related to improving exposure assessment, geographic and contextual influences, and economics. Recently released funding opportunities address issues in policy-relevant research, including enhancing environmental measures and examining school-based polices on energy balance–related behaviors. A complete list of available funding opportunities can be accessed at NCI’s website (cancercontrol.cancer.gov/energy_balance/funding.html). These findings indicate a strong response from extramural investigators, as NCI’s energy-balance portfolio has doubled in size, from 64 to 155 grants in FY2004 and FY2010, respectively, an increase from 2.1% to 4.2 % of NCI’s total research project grant portfolio.
The type of research being done has changed over the 7-year period. Whereas RCTs and interventions and descriptive and observational studies remained the most commonly utilized study designs, research on measurement and on basic science both doubled between FY2004 and FY2010. Additionally, the increased proportion of exploratory grants (R21s) and cooperative agreements (U54s and U01s) reflects greater use of exploratory and developmental research approaches and use of transdisciplinary research teams within targeted funding initiatives, such as the Transdisciplinary Research in Energetics and Cancer (TREC) (www.trecscience.org).
These findings also identify opportunities for additional research in basic science and implementation science. In the area of basic science, NCI’s Provocative Questions funding opportunity, issued in August 2011, included several questions related to the molecular mechanisms linking obesity, behaviors, and cancer risk. Further, NCI has supported workshops related to areas pertinent to energy balance and cancer; research gaps and opportunities from many of these have been summarized in publications.25–27 NIH obesity conferences have identified topics relevant to research on obesity and cancer. The limited number of NCI grants supporting implementation science reflects the state of cancer-related energy-balance research, which is focused on earlier phases of discovery research—rather than on implementation research designed to identify best approaches for widespread adoption in practice.
The increasingly interdisciplinary nature of the field is reflected by the high proportion (42%) of the portfolio examining physical activity, diet, and weight in combination. A leading example of such an activity is the TREC Initiative, which supports academic centers that integrate basic science and population-based research examining diet, weight, and physical activity and their effects on energy balance and cancer. The initiative also advances training in interdisciplinary approaches.
The analysis identified many studies examining the effects of energy balance on quality of life and biomarkers, but a limited number of RCTs on energy balance and cancer outcomes. A number of NIH trials have demonstrated the efficacy of weight loss in reducing risk for several chronic diseases. These trials and other research have demonstrated that it would not be feasible to conduct a weight loss trial of cancer prevention because the benefits for prevention of other chronic diseases would be demonstrated, and the trial consequently stopped, before the effect of weight loss on the prevention of cancer became evident. However, feasibility trials on weight loss or physical activity interventions in cancer patients and survivors are exploring the potential to test the effect of these interventions on disease outcomes.
Responsiveness to federal and scientific priorities is also illustrated by this analysis, as shown by: the increase in minority participants in many studies; inclusion of and focus on cancer survivors; and the rapidly increasing attention on colorectal/gastric, prostate, and hematologic cancers. In addition to research on the effect of energy balance with onset of cancer in adult life, research is expanding on the association of birth weight with both childhood and adult onset cancers. Because of the substantial amount of evidence that suggests it is difficult to reverse obesity once it occurs, a majority of research related to obesity prevention is focused on children and their early life experiences. In this area, NCI is supporting a modest, albeit growing, amount of research on children. These trends are consistent with strategic priorities developed and pursued by the NCI and NIH, as well as the overall evolution of the field.
Limitations
The limitations to this analysis should be considered, and caveats should be addressed regarding potential comparisons of this analysis to existing NIH summaries of nutrition- or obesity-related research. The definition of energy balance and related health behavior research used for this analysis may have resulted in omission of some relevant studies. However, for the purposes of tracking trends over time, it is unlikely that the analysis would have changed in the completeness of identification of relevant grants.
Among included studies, the multiple relevant topic areas or cancer sites may have been coded and characterized in a manner that does not fully reflect the multidimensional nature of a specific grant. Further, the comparability of the analysis to NIH reports of obesity-related grant funding is limited, as the search terms were different than those used in public NIH obesity research portfolios. This analysis is inclusive of energy-balance conditions and health behaviors, whereas the NIH portfolio specific to obesity is more restricted in focus. The coding categories used in the review were relevant to the NCI 2005 budget energy-balance research priorities and are not comparable to other NIH portfolio analyses. Additionally, given the nature of the text search strategy used in this analysis and study details not being reported in public and internal databases, grants may have been unintentionally omitted.
As always, the process by which grants were determined to be eligible for inclusion required interpretation and judgment. Although it was conducted with specific criteria, some grants may involve multiple research designs and might be categorized in several areas. However, the broad themes and patterns represented are likely reflective of trends in research support in the field. Lastly, no adjustments were made to account for either fluctuations in NCI funding levels due to federal budgetary issues during the FY2004–FY2010 period or economic inflation.
Conclusion
As the study of energy balance continues to grow in complexity, research opportunities spanning multiple conditions, levels and behaviors will become increasingly necessary. To meet this challenge, institutes across the NIH increasingly collaborate in the development and support of funding opportunities in this area, with coordination from the NIH-wide ORTF. Issued more frequently than previously, these co-funded opportunities represent a close scientific and programmatic partnership across disciplines and areas of expertise common to each institute and NCI’s active involvement. Trans-agency and public/private research coordination is furthered by the National Collaboration on Childhood Obesity Research (NCCOR), which is focused on research at the policy and environmental level relevant to children, families, and the communities in which they live, play, and work and reflects a partnership between NIH, the U.S. Department of Agriculture, the CDC, and Robert Wood Johnson Foundation (www.nccor.org).
A recent projection of the future health and economic burden of obesity from 2013 to 2030 in the United Kingdom and the U.S. estimated that continuation of existing trends in obesity will lead to between 405,000 and 539,000 additional cases of cancer in the U.S. by 2030.28 The attendant direct cost of combined medical costs for treatment of the multiple diseases related to obesity was estimated to increase by $48 to 66 billion per year in the U.S. In addition to medical costs, indirect costs of obesity include decreased years of disability-free life, increased early mortality, loss of years of productive work, higher disability costs, increased work absenteeism and reduced productivity.29 Physical inactivity, independent of obesity, also results in excessive direct medical costs.29
Such estimates indicate a need for an increased focus on obesity-prevention research in concert with research to gain a more in-depth understanding of the potential to prevent obesity as well as the link between energy balance and cancer risk and prognosis. NCI’s commitment to advancing research in this field is indicated by the expansion of investigator-initiated research as well as program-developed research initiatives, most recently in the 2011 NCI Provocative Questions Request for Applications that called for research on cellular and molecular mechanisms that underlie observed obesity and cancer risk associations.
Acknowledgements
The authors extend their appreciation to John Milner, Leah Sansbury, Audie Atienza, and Barbara Spalholz at the National Cancer Institute for their assistance in completing this analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.World Cancer Research Fund. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington DC: AICR; 2007. [Google Scholar]
- 2.Guh D, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis A. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health. 2009;9(1):88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedenreich CM, Neilson HK, Lynch BM. State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer. 2010;46(14):2593–2604. doi: 10.1016/j.ejca.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 4.Vainio H, Bianchini F. IARC Handbooks of Cancer Prevention, Vol. 6: Weight Control and Physical Activity. Lyon, France: IARC Press; 2002. [Google Scholar]
- 5.WHO. Diet, nutrition and the prevention of chronic diseases. Geneva: WHO; 2003. [Google Scholar]
- 6.Anthony P. Estimating the number of U.S. incident cancers attributable to obesity and the impact on temporal trends in incidence rates for obesity-related cancers. Cancer Detect Prev. 2008;32(3):190–199. doi: 10.1016/j.cdp.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Renehan AG, Soerjomataram I, Tyson M, et al. Incident cancer burden attributable to excess body mass index in 30 European countries. Int J Cancer. 2010;126(3):692–702. doi: 10.1002/ijc.24803. [DOI] [PubMed] [Google Scholar]
- 8.World Cancer Research Fund / American Institute for Cancer Research. Food, Nutrition, and Physical Activity: a Global Perspective. Washington DC: AICR; 2009. Policy and Action for Cancer Prevention. [Google Scholar]
- 9.Protani M, Coory M, Martin JH. Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat. 2010;123(3):627–635. doi: 10.1007/s10549-010-0990-0. [DOI] [PubMed] [Google Scholar]
- 10.Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM. Physical activity, biomarkers, and disease outcomes in cancer survivors: A systematic review. J Natl Cancer Inst. 2012;104(11):815–840. doi: 10.1093/jnci/djs207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siegel EM, Ulrich CM, Poole EM, Holmes RS, Jacobsen PB, Shibata D. The effects of obesity and obesity-related conditions on colorectal cancer prognosis. Cancer Control. 2010;17(1):52–57. doi: 10.1177/107327481001700107. [DOI] [PubMed] [Google Scholar]
- 12.Barbaric M, Brooks E, Moore L, Cheifetz O. Effects of physical activity on cancer survival: a systematic review. Physiother Can. 2010;62(1):25–34. doi: 10.3138/physio.62.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferrer RA, Huedo-Medina TB, Johnson BT, Ryan S, Pescatello LS. Exercise interventions for cancer survivors: a meta-analysis of quality of life outcomes. Ann Behav Med. 2011;41(1):32–47. doi: 10.1007/s12160-010-9225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among U.S. adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 15.Trends in leisure-time physical inactivity by age, sex, and race/ethnicity– U.S., 1994–2004. MMWR Surveill Summ. 2005;54:991–994. [PubMed] [Google Scholar]
- 16.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the U.S., 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010;140:1832–1838. doi: 10.3945/jn.110.124826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang T, Horlick MN. Trends in childhood obesity research: A brief analysis of NIH-supported efforts. J Law Med Ethics. 2007;35(1):148–153. doi: 10.1111/j.1748-720X.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- 19.National Cancer Institute. The Nation's Investment in Cancer Research: A Plan and Budget Proposal for Fiscal Year 2005. Washington DC: NIH; 2003. [Google Scholar]
- 20.NIH. New strategic plan for NIH obesity research seeks to curb epidemic. 3-31-2011. Bethesda MD: NIH; 2011. [Google Scholar]
- 21.Spiegel AM, Alving BM. Executive summary of the Strategic Plan for National Institutes of Health Obesity Research. Am J Clin Nutr. 2005;82(1):211S–214S. doi: 10.1093/ajcn/82.1.221S. [DOI] [PubMed] [Google Scholar]
- 22.NIH Obesity Research Task Force. Strategic Plan for NIH Obesity Research. Bethesda MD: NIH; 2011. [Google Scholar]
- 23.Schmitz KH, Courneya KS, Matthews C, et al. American College of Sports Medicine Roundtable on Exercise Guidelines for Cancer Survivors. Med Sci Sports Exerc. 2010;42(7) doi: 10.1249/MSS.0b013e3181e0c112. [DOI] [PubMed] [Google Scholar]
- 24.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Washington DC: DHHS; 2008. [Google Scholar]
- 25.Bouchard C, Agurs-Collins T. Studying Gene–Behavior Interactions and Obesity: Summary of Recommendations. Obesity (Silver Spring) 2008;16:S95–S96. doi: 10.1038/oby.2008.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKinnon RA, Reedy J, Handy SL, Rodgers AB. Measuring the food and physical activity environments: shaping the research agenda. Am J Prev Med. 2009;36:S81–S85. doi: 10.1016/j.amepre.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 27.Wong JB, Coates PM, Russell RM, et al. Economic analysis of nutrition interventions for chronic disease prevention: methods, research, and policy. Nutr Rev. 2011;69:533–549. doi: 10.1111/j.1753-4887.2011.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the U.K. Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 29.Colditz GA. Economic costs of obesity and inactivity. Med Sci Sports Exerc. 1999;31(11):S663–S667. doi: 10.1097/00005768-199911001-00026. [DOI] [PubMed] [Google Scholar]