Abstract
Precocious puberty in girls can be due to number of factors of which idiopathic central precocious puberty is the most common etiology. Here, we describe 3 cases of precocious puberty where the first case had premature thelarche in the background history of mother with Type 2 Diabetes Mellitus, cases 2 and 3 had ovarian tumours with heterogeneity in presentation.
Keywords: Precocious puberty, girls, ovarian tumours, idiopathic
INTRODUCTION
There are many genes and many pathways (excitatory and inhibitory) that control pubertal development.[1] The final event that initiates puberty is s sustained increase in the pulsatile release of gonadotrophin releasing hormone (GnRH) from GnRH neurons. In primates, these neurosecretory cells are located in the medial basal hypothalamus. The increase in GnRH pulses leads to activation of the pituitary ovarian axis which manifest clinically with the onset of secondary sexual characteristics. This usually happens after the age of 8 years in girls.[2] However, some recent studies have shown earlier onset of puberty in US girls. Majority of these girls who have breast development after 7 years reach a final height which is appropriate for their genetic potential without treatment.[3,4]
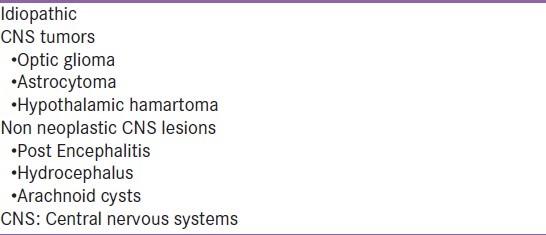
Precocious puberty is defined as development of pubertal changes before the age of 8 years in girls along with an increase in goandotropin and or sex steroid, accelerated somatic development and bone age. Precocious puberty is classified as gonadotropin dependent (central, true precocious puberty (PP)) or gonadotropin independent (peripheral, pseudo PP). Central precocious puberty (CPP) is due to early maturation of the hypothalamo pituitary gonadal (HPG) axis. The frequency of CPP is 1 in 5000-1 in 10,000. It is more common in girls, female:male ratio ranging from 3/1 to 23/1. However, CPP due to organic causes is more common among boys. Common causes for CPP are given in Table 1. Majority of CPP in girls is idiopathic. Environmental estrogen (cosmetic products, insecticides, bioengineered food products) can disturb the HPG axis. Childhood obesity, intra uterine growth retardation, parental obesity and diabetes are associated with early thelarche. Central nervous systems (CNS) pathology is observed in a small member of girls with CPP. These are hydrocephalus, meningo myelocele, neurofibromatosis, hypothalamic hamartomas, etc.[5–7] Hamartomas are non-neoplastic, congenital lesions, containing GnRH neurons. There are more frequent in children who manifest with puberty before 4 years. Children who have received cranial radiation for malignancy are at higher risk of CPP. CPP may be the first sign of optic glioma.
Table 1.
Causes for central precocious puberty in girls
Peripheral precocious puberty (PPP) or gonadotropin independent precocious puberty
Endogenous or exogenous estrogen excess leads to PPP in girls. Table 2 gives common causes of PPP. McCune–Albright syndrome manifests with Cafe’ au lait spots, poly ostotic fibrous dysplasia and PPP. It is due to mutations in the gene encoding the alpha subunit of the Gs protein. This should be considered in children who present with recurrent follicular cyst and irregular vaginal bleeding. Primary hypothyroid may manifest with thelarche in girls without accelerated growth. Some may have elevated Prolactin, Galactorrhora or ovarian cysts. Congenital adrenal hyperplasia manifests with hetero sexual pubertal development in girls. This may, following glucocorticoid therapy, manifest with CPP.
Table 2.
Causes of peripheral precocious puberty in girls

Premature thelarche
Starts before 2 years of age, may be unilateral. It is not associated with accelerated growth or bone maturation and regress with time. Follicle stimulating hormone (FSH) is increased and there is increased LH and FSH response to GnRH. Uterine and ovarian sizes are in the prepubertal range. Premature thelarche which starts after 2 years of age may progress to CPP.
Premature adrenarche
Increase in adrenal androgens. It may or may not be associated with premature pubarche (increase in pubic and axillary hair). It occurs as a result of increased secretion of androgens from the zona reticularis of the adrenal glands.
The pathologic conditions that need to be considered in children with premature adrenarche are adrenal tumors and congenital adrenal hyperplasia.
Premature adrenarche may be an early sign of metabolic syndrome or polycystic ovary syndrome. These may be associated hyperinsulinism and dyslipidemia. Some may have low birth weight, family members with obesity and T2DM.
DIAGNOSIS AND MANAGEMENT
Initial evaluation will include detailed medical history, including the onset of symptoms, rate of progression, growth and family history of PP and diabetes mellitus. Physical examination should include anthropometry and pubertal staging. Endocrine evaluation should include measurement of LH, FSH, E2 GnRH stimulation test,[8–10] and pelvic ultrasound for ovaries and uterus. Additional investigations may include measurement of 17 Hydroxyprogesterone (17OHP), DHEAS, Plasma Insulin, etc. In case of Premature thelarche, there is predominant FSH response while in CPP LH response is dominant. Both LH and FSH are suppressed or in the prepubertal range in PPP. Increase in ovarian volumes (bilateral) and uterus will indicate CPP. Ovaries are asymmetrically enlarged in PPP. Cranial magnetic resonance imaging (MRI) should be done in cases of CPP to exclude CNS pathology.
Treatment decisions are based on age at diagnosis, predicted height, anxiety about early menarche and psychological and behavior problems. Generally, children less than 7 years of age should be treated.
GnRH analogues have been used to treat children with CPP since early 80 s. They are considered safe.
Anti-estrogens or aromatase inhibitors may be used in case of McCune–Albright syndrome.
Girls with early puberty may be at greater risk for obesity, cardiovascular diseases and diabetes mellitus.[11]
CASE REPORTS
Case 1
Baby S C, presented with premature thelarche (B 3, tanner stage) at 19 months of age. Her birth weight was 9 pounds, mother had type 2 diabetes mellitus. There was no axillary or pubic hair, bone age was 2 years (Greulich Pyele). FSH 2.0 mIU/ml, LH 1.4 mIU ml Estradiol <10 pg/ml by chemiluminesence assay. On ultra sonography, uterus measured 23.4 × 15 × 8.7 mm. X-ray skull was normal. Subsequent follow-up did not reveal any progression in breast development or other pubertal development. Investigations at the age of 9 years for accelerated weight gain revealed subclinical hypothyroidism (TSH 10), she was initiated on eltroxin 50 mcg. She attained menarche at the age of 11 years. She had regular periods for first few months followed by excessive prolonged bleeding. For this she was started on an oral contraceptive pill. She continued to gain weight, now at age 16 years she is 82 kg and height 166 cms, BMI 29.8. Her present profile is FSH 4.5, LH 4.68, Prolactin 12.91, TSH 2.5, HbA1c 5.2, fasting insulin 11.3 and testosterone 0.133 (0.06-0.82).
Case 2
Baby R K, 3-year-old girl, presented with progressive bilateral breast enlargement over 1 year, irregular vaginal bleeding for 10 months and pubic hair development for 2 months. There was no clitoral enlargement, neck swelling, pigmented skin marks, bone pain/fractures. Parents could not comment on any recent height gain. She had no significant medical illness or radiation exposure in the past. Her birth and neonatal period were normal. Her milestones were normal for her age.
On examination, her vitals were normal. There was no thyroid swelling, café au lait spots or any bony abnormality. Tanners staging was B3P3. There was no axillary hair or genital ambiguity. Cardiac, thoracic and neurological examinations were normal. A solitary well defined pelvic mass firm to hard, mobile was palpable in right lower abdomen.
Her investigations showed normal hemogram, liver and renal functions. Her bone age, height age and chorological age were respectively 8 year, 10 months, 4 year (100 cm) and 3 year. Thyroid functions were normal. Her hormonal profile was as follows: LH <0.1 mIU/ml, FSH <0.1 mIU/ml, Testosterone 0.334 ng/ml, DHEAS 17.97 μg/dl, Estradiol >1000 pg/ml.
Computed Tomography (CT) pelvis showed a heterogeneously enhancing abdomino-pelvic mass.
She underwent resection of right tubo-ovarian mass, which was suggestive of juvenile granulose cell tumor. Post-operatively, child had withdrawal vaginal bleeding on day 2 of surgery lasting 48 h. Repeat hormonal profile done on 6th post-operative day showed markedly reduced Estradiol levels 17 pg/ml, LH <0.1 mIU/ml, FSH 0.1 mIU/ml, testosterone 0.025 ng/ml, DHEAS 0.947 μg/dl. She is now 6 months post-surgery. There was no vaginal bleeding so far.
Case 3
Baby S P, a 6-year-old girl, presented with progressive bilateral breast enlargement for 7 months, cyclical vaginal bleeding (3/25-30days) for 4 months and pubic hair development was noted for 2 months. There was no clitoral enlargement, neck swelling, pigmented skin marks, bone pain/fractures. There was h/o recent increase in height in the last 1 year. She had no significant medical illness or radiation exposure in the past. Her birth and neonatal period were normal. Her milestones were normal for her age.
On examination, her vitals were normal. There was no thyroid swelling, café au lait spots or any bony abnormality noted. Tanners staging was B3P3. There was no axillary hair or genital ambiguity. Cardiac, thoracic and neurological examinations were normal. Examination of the abdomen was normal.
Her investigations showed normal hemogram, liver and renal functions. Her bone age, height age and chorological age were respectively 7.8 year, 7 year (119 cm) and 6 year. Thyroid functions were normal. Her hormonal profile was as follows: LH < 0.1 mIU/ml, FSH < 0.1 mIU/ml, Testosterone 0.334 ng/ml, DHEAS 17.9 μg/dl, Estradiol > 162.8 pg/ml.
CT pelvis showed a bulky left ovary of size 5.4 cm predominantly solid with follicles seen at periphery and pubertal uterus.
She underwent laparascopic resection of right tuboovarian mass which on histopathology was mixed germ cell sex cord stromal tumor. Post-operatively, child had withdrawal vaginal bleeding on day 4 of surgery lasting 72 h. Repeat hormonal profile done on 6th post-operative day showed markedly reduced Estradiol levels 14.37 pg/ml, LH <0.184 mIU/ml, FSH 0.25 mIU/ml, testosterone 0.025 ng/ml, DHEAS 9.87 μg/dl. At 6 months follow-up, there was no vaginal bleeding so far.
COMMENTS
Case 1 presented with premature thelarche, subsequent follow-up showed no progression and good final height. Her birth weight was 9 pounds, and her mother had type 2 diabetes mellitus. We now know that children with type 2 diabetic parents tend to have premature thelarche, with high estradiol without an increase in LH, FSH. They are at higher risk for obesity and metabolic syndrome.
Cases 2 and 3, ovarian tumor presenting as sexual precocity gives an idea about the heterogeneity of presentation, biochemistry and histopathology. First child had an irregular vaginal bleeding with Estradiol levels of >1000 pg/ml due to a large juvenile granulosa cell tumor. Second had a fairly regular cyclical vaginal bleeding with Estradiol levels of 162.9 pg/ml due to mixed-sex cord stromal tumor. Both have successful outcome at 12 months and 6 months respectively of follow-up without recurrence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ojeda SR, Dubay C, Lomniczi A, Kaidar G, Matagne V, Sandau US, et al. Gene networks and the neuroendocrine regulation of puberty. Mol Cell Endocrinol. 2010;324:3–11. doi: 10.1016/j.mce.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herman-Giddens ME, Slora EJ, Wasserman RC, Bourdony CJ, Bhapkar MV, Koch GG, et al. Secondary sexual characteristics and menses in young girls seen in office practice: A study from the Pediatric Research in Office Settings network. Pediatrics. 1997;99:505–12. doi: 10.1542/peds.99.4.505. [DOI] [PubMed] [Google Scholar]
- 3.Tanner JM. Growth at Adolescence. Springfield, IL: Charles C. Thomas Publishers Ltd; 1962. [Google Scholar]
- 4.Susman EJ, Houts RM, Steinberg L, Belsky J, Cauffman E, Dehart G, et al. Longitudinal development of secondary sexual characteristics in girls and boys between ages 91/2 and 151/2 years. Arch Pediatr Adolesc Med. 2010;164:166–73. doi: 10.1001/archpediatrics.2009.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mogensen SS, Aksglaede L, Mouritsen A, Sørensen K, Main KM, Gideon P, et al. Pathological and incidental findings on brain MRI in a single center study of 229 consecutive girls with early or precocious puberty. PLOS One. 2012;7:e29829. doi: 10.1371/journal.pone.0029829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trivin C, Couto-Silva AC, Sainte-Rose C, Chemaitilly W, Kalifa C, Doz F, et al. Presentation and evolution of organic central precocious puberty according to the type of CNS lesion. Clin Endocrinol (Oxf) 2006;65:239–45. doi: 10.1111/j.1365-2265.2006.02582.x. [DOI] [PubMed] [Google Scholar]
- 7.Kotwal N, Yanamandra U, Menon AS, Nair V. Central precocious puberty due to hypothalamic hamartoma in a six-month-old infant girl. Indian J Endocrinol Metab. 2012;16:627–30. doi: 10.4103/2230-8210.98027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yazdani P, Lin Y, Raman V, Haymond M. A single sample GnRHa stimulation test in the diagnosis of precocious puberty. Int J Pediatr Endocrinol. 2012;2012:23. doi: 10.1186/1687-9856-2012-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee HS, Park HK, Ko JH, Kim YJ, Hwang JS. Utility of Basal luteinizing hormone levels for detecting central precocious puberty in girls. Horm Metab Res. 2012;44:851–4. doi: 10.1055/s-0032-1321905. [DOI] [PubMed] [Google Scholar]
- 10.Pasternak Y, Friger M, Loewenthal N, Haim A, Hershkovitz E. The utility of basal serum LH in prediction of central precocious puberty in girls. Eur J Endocrinol. 2012;166:295–9. doi: 10.1530/EJE-11-0720. [DOI] [PubMed] [Google Scholar]
- 11.Pierce MB, Kuh D, Hardy R. Role of lifetime body mass index in the association between age at puberty and adult lipids: Findings from men and women in a British birth cohort. Ann Epidemiol. 2010;20:6s76–82. doi: 10.1016/j.annepidem.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]


