Abstract
FRAX is an important web based tool to assess fragility fracture risk in osteoporosis. It has many important limitations too. Good clinical judgement is needed to interpret the results of FRAX. With increasing use we can improvise this tool further.
Keywords: Frax BMD osteoporosis
“If wishes were horses, beggars would ride. And then, fracture risk prediction would be even easier than adding 2+2!”
INTRODUCTION
Osteoporosis is by far the most common metabolic bone disease. An international Consensus Development Conference[1] more correctly labeled it as “a disease characterized by low bone mass and micro-architectural deterioration of bone tissue, leading to enhanced bone fragility and a consequent increase in fracture risk.”
While introduction of many anti-fracture medications since the early 1990s has revolutionized osteoporosis therapy, it is equally important to recognize the role of risk factors, both modifiable and non-modifiable. Understanding these risk factors and utilizing them to the fullest, in both fracture prediction and fracture prevention/management, would be like reinforcing our armamentarium to fight against this enemy “osteoporosis.”
fragility fractures of all kinds—vertebral, hip, forearm, and others—are a public health problem. With increasing longevity of the Indian population, this problem is going to reach epidemic proportions.[2] Despite the availability of diagnostic tools and clinical data supporting the importance of preventing and treating osteoporosis, many patients remain undiagnosed and untreated.[3]
Day in and day out, in our clinics, we come across patients with severe osteoporosis and no fractures and even patients with borderline osteopenia but multiple fragility fractures. The million-dollar question always remains; “Can we predict fragility fractures?” An ideal fracture prediction tool is equivalent to pursuit of the “holy grail.” Bone mineral density (BMD) assessment, although specific, may not be sensitive for predicting fracture risk. Adding clinical risk factors that are able to predict fracture independent of BMD may improve our ability to predict fracture risk.[4]
FRAX: FACTS
FRAX is a web-based algorithm (www.shef.ac.uk/FRAX) designed to calculate the 10-year probability of major osteoporosis-related fracture (clinical vertebral, hip, forearm, or humerus) and hip fractures in men and women based on easily obtained clinical risk factors and bone mineral density (BMD) [Figure 1].
Figure 1.
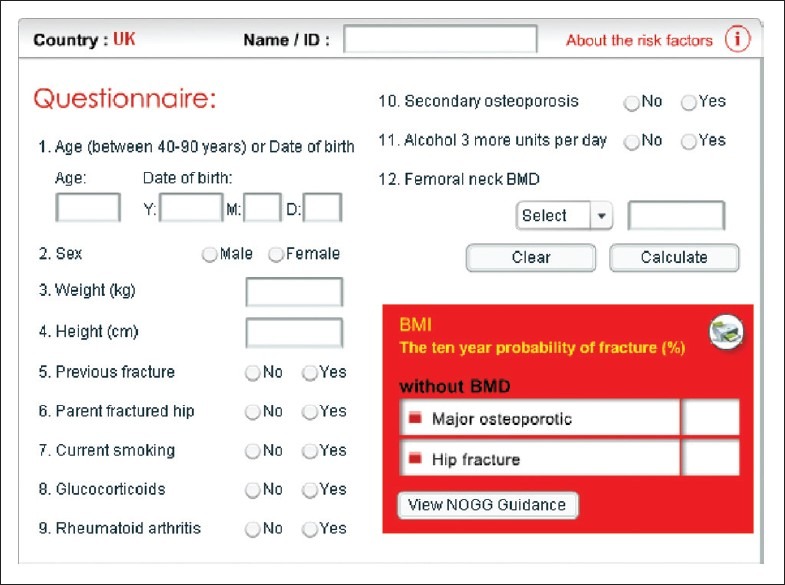
Showing FRAX calculation tool-web-based algorithm program
HOW WAS FRAX DEVELOPED?
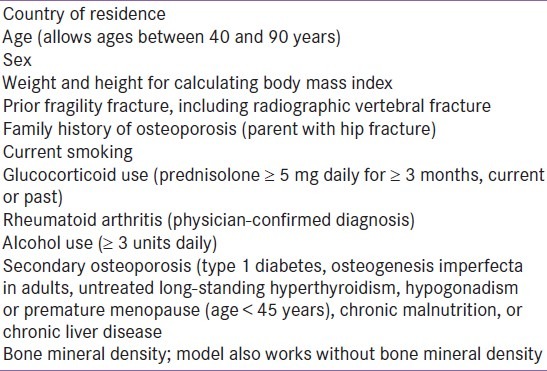
The WHO task force first reviewed the literature using mega-analysis to identify eight candidate risk factors for fracture, independent of BMD [Table 1]. For each country, they added country-specific fracture incidence rates to these clinical risk factors to yield a 10-year probability of fracture. In this model, we neither use relative risk, because relative risk decreases with age, nor do we use lifetime fracture risk as it begins to decline at 70 years of age because of competing risk of death.[4] This FRAX model has been validated in 11 cohorts across the globe.[5] Fracture risk prediction tools are designed to facilitate treatment of people at high absolute risk of fracture and re-assurance of those at low risk. Various guidelines based on these fracture prediction tools guide us in targeting the intervention. The National Osteoporosis Foundation (NOF)[6,7] intervention thresholds are based upon economic cost-effectiveness analyzes (10 year probability of major osteoporotic fracture ≥ 20% and hip fracture ≥ 3% is considered significant), whereas the National Osteoporosis Guideline Group (NOGG) guidelines recommend intervention if the probability of fracture exceeds that of a person of the same age, who has suffered a previous osteoporotic fracture.[8]
Table 1.
Clinical risk factors included in WHO Fracture Risk Assessment Tool
An important utility in fracture prediction using FRAX tool is its use of Body Mass Index (BMI) instead of BMD applicable as a simple screening test, thus avoiding unnecessary investigations in those with a very low probability of fracture. [Figure 2]
Figure 2.

Showing paper hand out that can be kept in OPD and also can calculate risk based on Body Mass Index (BMI), even if BMD not available
LEARNING BY EXAMPLE
A 50-year-old male with a BMI of 20 kg/m2 and having no risk factor can easily be re-assured, even without undergoing BMD testing (10 year probability of major osteoporosis related fracture is 1.5% and hip fracture is 0.2%).
FRAX: FANTASY
“Fantasy mirrors desire.” This is true even for FRAX prediction; it was devised with a desire to create a sure shot fracture prediction model, but it itself has its inherent flaws. Certain variables that would be difficult for a primary care practitioner—measurements of physical activity, vitamin D deficiency, bone turnover markers, despite them being independent risk factors, are excluded. FRAX does not take into account dose-response relationships.[4] For example, somebody on a higher dose of glucocorticoids has a greater risk as compared to somebody on a lower dose. FRAX also doesn’t take into account interaction of risk factors. FRAX may only be used in untreated patients. FRAX does not account for individuals who have low lumbar T-score but with normal femoral neck.[9] Composite strength indices of the femoral neck can predict fracture risk without race/ethnicity information as accurately as bone mineral density does in combination with race/ethnicity information, which is not incorporated in FRAX.[10] FRAX assumes that the relationship between BMI and mortality in all races and ethnic groups are similar, which is not so.[4] Subsequent fracture risk fluctuates over time and may be highest in the first 5 years after initial fracture.[5] The increased subsequent fracture risk after initial fracture is considered constant over time in FRAX.[4] The question always remains, should we deny an “established preventive strategy” to a person with borderline low risk just based on “health economics.” Communication about FRAX risk depends on the patient's understanding of the statistical concept of risk,[4] which is especially poor in our country.
LEARNING BY EXAMPLE
A 50-year-old male smoker, with chronic mal-absorption and hyperthyroidism and T score of -1.8, would be denied therapeutic intervention, if purely based on FRAX score (10 year probability of major osteoporotic fracture is 2% and hip fracture is 0.9%).
A 40-year-old female, with an autoimmune disease requiring treatment with multiple immune-modulators including glucocorticoids for a longer duration of time with a T score of -2.4, would be denied therapeutic intervention, if purely based on FRAX score (10 year probability of major osteoporotic fracture is 3% and hip fracture is 1.1%).
FRAX future
In the future, we can anticipate the incorporation of spinal BMD T-scores into the algorithm. Eventually, other bone measurements, biochemical tests, and risk factors may also be added. Meanwhile, the WHO Center is currently collaborating with organizations in many countries to adapt FRAX by incorporating their respective fracture and mortality rates into the algorithm. This will allow the use of FRAX to expand around the globe and enable those who are interested to develop region-specific treatment thresholds. The ultimate test of the validity of FRAX will come when its ability to predict fracture and to select patients for therapy is evaluated prospectively in large clinical trials.
FRAX: ALTERNATIVES
Several alternatives of FRAX exist such as the Canadian Osteoporosis Society,[11] the Nguyen algorithm,[12] and the Dutch algorithm.[13] These risk factor algorithms depend on a smaller number of clinical risk factors. They are often only valid and include other additional factors that may not be included in FRAX such as falls. They are often validated only in a given observational study or in given cohort and at this time, may not have generalized applicability. They need to be validated in different countries.[4]
CONCLUSION
FRAX is a major achievement in terms of our understanding of measuring fracture risk. But, FRAX does not replace good clinical judgment by the health care practitioner. It is likely that providing global risk information to patients at only one point in time may well be relatively ineffective.[4] We should thus consider repeating FRAX information over time, making it a dynamic tool. Perhaps the greatest current limitation of FRAX is that few use it.[5] Busy clinicians find it difficult to spend time on a web-based algorithm due to numerous reasons. But, more we use it, more we can improvise this tool.
“We become what we behold. We shape our tools, and thereafter our tools shape us.”
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Consensus development conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94:646–50. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 2.Malhotra N, Mithal A. Osteoporosis in Indians. Indian J Med Res. 2008;127:263–8. [PubMed] [Google Scholar]
- 3.Nguyen TV, Center JR, Eisman JA. Osteoporosis: Underrated, underdiagnosed and undertreated. Med J Aust. 2004;180:S18–22. doi: 10.5694/j.1326-5377.2004.tb05908.x. [DOI] [PubMed] [Google Scholar]
- 4.Silverman SL, Calderon AD. The Utility and Limitations of FRAX: A US Perspective. Curr Osteoporos Rep. 2010;8:192–7. doi: 10.1007/s11914-010-0032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watts NB, Ettinger B, LeBoff MS. FRAX facts. J Bone Miner Res. 2009;76:1–3. doi: 10.1359/jbmr.090402. [DOI] [PubMed] [Google Scholar]
- 6.Dawson-Hughes B, Tosteson AN, Melton LJ, 3rd, Baim S, Favus MJ, Khosla S, et al. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int. 2008;19:449–58. doi: 10.1007/s00198-008-0559-5. [DOI] [PubMed] [Google Scholar]
- 7.Tosteson AN, Melton LJ, 3rd, Dawson-Hughes B, Baim S, Favus MJ, Khosla S, et al. Cost-effective osteoporosis treatment thresholds: The United States perspective. Osteoporos Int. 2008;19:437–47. doi: 10.1007/s00198-007-0550-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A. Case finding for the management of osteoporosis with FRAX—assessment and intervention thresholds for the UK. Osteoporos Int. 2008;19:1395–408. doi: 10.1007/s00198-008-0712-1. [DOI] [PubMed] [Google Scholar]
- 9.National Osteoporosis Foundation: Clinician's Guide to Prevention and Treatment of Osteoporosis. [Last accessed on 2012 Nov 19]. Available from: http://www.nof.org/professionals/Clinicians_Guide.htm .
- 10.Ishii S, Greendale GA, Cauley JA, Crandall CJ, Huang MH, Danielson ME, et al. Fracture Risk Assessment without Race/Ethnicity Information. J Clin Endocrinol Metab. 2012;97:3593–602. doi: 10.1210/jc.2012-1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown JP, Josse RG. Scientific Advisory Council of the Osteoporosis Society of Canada.2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ. 2002;167:S1–34. [PMC free article] [PubMed] [Google Scholar]
- 12.Pluskiewicz W, Adamczy KP, Franek E, Leszczynski P, Sewerynek E, Wichrowska H, et al. Ten-year probability of osteoporotic fracture in 2012 Polish women assessed by FRAX and nomogram by Nguyen et al. Conformity between methods and their clinical utility. Bone. 2010;46:1661–7. doi: 10.1016/j.bone.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Plumijm S, Koes B, de Laet C, Van Schoor NM, Kuchuk NO, Rivadeneira F, et al. A simple risk score for the assessment of absolute fracture risk in general practice based on two longitudinal studies. J Bone Miner Res. 2009;24:768–74. doi: 10.1359/jbmr.081244. [DOI] [PubMed] [Google Scholar]


