Abstract
Introduction:
Empty sella is characterized by the herniation of the subarachnoid space within the sella, which is often associated with some degree of flattening of the pituitary gland. This study was undertaken to evaluate the clinical and hormonal profile in patients with empty sella.
Aims and Objectives:
To evaluate the clinical and hormonal profile of the patients with an empty sella.
Materials and Methods:
Patients undergoing a CT/MRI at our center, for various reasons but with the finding of the empty sella were included in this study. A detailed history and clinical examination was done. Apart from routine tests, hormonal evaluation included serum thyroid stimulating hormone, T4, cortisol (8 am), prolactin, total testosterone, follicle stimulating hormone, leutinizing hormone, and fasting Insulin like Growth factor 1 (IGF 1) were done.
Results:
A total of 34 patients, diagnosed radiologically to have empty sella, were evaluated and of them 24 had primary empty sella (PES) and 10 had secondary empty sella (SES). In subjects with PES, 12 out of 24 (50%) had endocrine dysfunction. The most common endocrine dysfunction noted was hyperprolactinemia, which was seen in 5 (20.8%) patients and the most common hormonal deficiency was isolated GH deficiency seen in four patients (12.5%).
Conclusion:
The high incidence of endocrine abnormalities in patients with PES mandates that these patients should routinely be subjected to endocrine evaluation to detect these deficiencies early, and appropriate replacement instituted where necessary, thus ensuring them of a better quality of life.
Keywords: Empty sella, isolated Growth Hormone Deficiency, Hyperprolactinemia
INTRODUCTION
Empty sella is characterized by the herniation of the subarachnoid space within the sella, which is often associated with some degree of flattening of the pituitary gland.[1,2] In primary empty sella (PES), several etiopathogeneic hypotheses have been proposed, including a congenital incomplete formation of the sellar diaphragm and suprasellar factors such as a stable or intermittent increase in intracranial pressure as well as volumetric changes in the pituitary (as observed in pregnancy).[1–3] On the other hand, secondary empty sella (SES) may be caused by pituitary adenomas undergoing spontaneous necrosis (ischemia or hemorrhage). Other causes known to cause SES are infective, autoimmune, traumatic, radiotherapy, drugs, and surgery. Numerous studies have shown that empty sella syndrome may be associated with pituitary dysfunction contrary to the notion of it being an incidental finding. Hence this study was undertaken to evaluate the clinical and hormonal profile in patients with empty sella.
AIMS AND OBJECTIVES
To evaluate the clinical and hormonal profile of patients with an empty sella.
MATERIALS AND METHODS
Inclusion criteria
Patients undergoing a CT/MRI at our center, for various reasons but with the finding of empty sella were included in this study.
Exclusion criteria
Patients having psychiatric disturbances, critical illness, pregnancy, lactation, or on drugs known to affect pituitary function were excluded from the study.
A detailed history and clinical examination was done. Apart from routine tests, hormonal evaluation included serum thyroid stimulating hormone, T4, cortisol (8 am), prolactin (PRL), total testosterone, follicle stimulating hormone, leuteinizing hormone and fasting IGF 1, all done by chemiluminescence. Stimulation tests were done where indicated.
Patients with history of pituitary apoplexy, head injury or surgery for pituitary adenoma were considered as SES and patients in whom an etiology was not discernible were considered as PES syndrome.
RESULTS
A total of 34 patients, diagnosed radiologically to have empty sella, were evaluated and of them 24 had PES and 10 had SES.
The mean age at diagnosis in subjects with PES was 40.6 ± 9.4 years and that in SES was 37 ± 9.6 years. In both PES and SES female predominance was observed, with the sex ratio being 3:1 and 2.3:1 respectively.
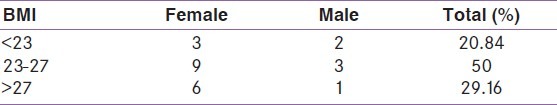
Etiology in the cases of SES was Sheehans syndrome in five, head trauma in three and post pituitary surgery in two. In the female patients with PES 83.3% (15/18) were multiparous and only 11% (2/18) were nulliparous, mean numbers of pregnancies in the multiparous women being 3.26 ± 0.79. The mean BMI in patients with PES was 26.4 ± 4.2 kg/m2 and that in SES was 24.3 ± 2.1 kg/m2 [Table 1].
Table 1.
Table showing patients with PES in different BMI groups
Most common presenting feature in PES was headache, present in 12 patients (50%). The headache was variable in localization, severity and duration, the most common pattern being diffuse with moderate intensity and a duration dating to few years. Three patients associated vomiting and evidence of papilledema suggestive of benign intracranial hypertension. However, cerebrospinal Fluid (CSF) pressures were not measured in these cases.
Endocrine function
All the patients of SES had panhypopituitarism, the most common presenting symptom being secondary amenorrhea in females and features of hypocortisolism in males.
In subjects with PES, 12 out of 24 (50 %) had endocrine dysfunction, though such dysfunction was clinically suspected in only eight of them. The most common endocrine dysfunction noted was hyperprolactinemia, which was seen in 5 (20.8%) patients. Four of these patients were females and none of the patients had serum PRL levels more than 100 μg/L (mean 61.96 ± 13.5 μg/L). Three of these five patients had isolated hyperprolactinemia while the other two had associated anterior pituitary hormonal deficiencies. In the PES subjects, 37.5% had at least one hormonal deficiency, the most common being isolated IGF 1 deficiency seen in four patients (12.5%). Other hormonal deficiencies that were seen in this group were isolated hypogonadotropic hypogonadism in two patients (8.3%), isolated central hypothyroidism in one patient (4.1%), isolated hypocortisolism in one patient (4.1%), and multiple pituitary hormone deficiency (hypocortisolism and hypogonadism) in one patient (4.1%). None of the patients had diabetes insipidus.
DISCUSSION
The reported prevalence of PES in general population is 8-35%.[4] In our study PES accounted for most cases of empty sella and it was more commonly noted in females with higher parity, as has been seen in earlier studies. Enlargement of the pituitary during pregnancy may lead to weaken of the sellar diaphragm, thus predisposing to herniation of cerebrospinal fluid into the sella.[4]
We also noted that obesity was more common among patients with PES. This is in accordance with the study De Marinis et al.[4] Obesity causes obstructive sleep apnea leading to hypercapnia and increased CSF pressure predisposing to empty sella.
There is a wide variation in the reported prevalence of endocrine abnormalities in PES. We noted endocrine dysfunction in 50% of PES patients while De Marinis et al. found endocrine abnormalities in 19%. Hyperprolactinemia was the most common endocrine abnormality observed in our study. In PES particularly, mild hyperprolactinemia has been frequently reported. This is thought to be due to pituitary stalk compression as a consequence of the remodeling of the hypothalamo-pituitary region and altered CSF dynamics. The most common hormonal deficiency was isolated growth hormone deficiency followed by isolated gonadotropin deficiency, which is compatible with previous studies. Somatotrophs are probably a more vulnerable component of the pituitary in PES, hence systematic GH testing and GH substitution considered in PES.
CONCLUSION
The high incidence of endocrine abnormalities in patients with PES, even when asymptomatic, mandates that these patients should routinely be subjected to endocrine evaluation to detect these deficiencies early, and appropriate replacement instituted where necessary, thus ensuring them of a better quality of life.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.McLachlan MS, Williams ED, Doyle FH. Applied anatomy of the pituitary gland and fossa: a radiological and histopathological study based on 50 necropsies. Br J Radiol. 1968;41:782–8. [Google Scholar]
- 2.Bergland RM, Ray BS, Torack RM. Anatomical variations in the pituitary gland and adjacent structures in 225 human autopsy cases. J Neurosurg. 1968;28:93–9. doi: 10.3171/jns.1968.28.2.0093. [DOI] [PubMed] [Google Scholar]
- 3.Jordan RM, Kendall JW, Kerber CW. The primary empty sella syndrome: analysis of the clinical characteristic, radiographic features, pituitary function and cerebral fluid adeno-hypophysial concentrations. Am J Med. 1977;62:569–80. doi: 10.1016/0002-9343(77)90420-x. [DOI] [PubMed] [Google Scholar]
- 4.De Marinis L, Bonadonna S, Bianchi A, Maira G, Giustina A. Primary empty sella. J Clin Endocrinol Metab. 2005;90:5471–7. doi: 10.1210/jc.2005-0288. [DOI] [PubMed] [Google Scholar]


